PIRIBEDIL
pharmachologic effect
Antiparkinsonian drug. The mechanism of action is associated with stimulation of dopamine receptors mainly in the nuclei of the extrapyramidal system. Increases blood supply to tissues and stimulates the transmission of nerve impulses, which helps improve brain metabolism.
It has a vasodilating effect due to its effect on dopamine receptors located in the smooth muscles of peripheral vessels.
Pharmacokinetics
After oral administration, piribedil is rapidly absorbed from the gastrointestinal tract, Cmax is reached after 1 hour. Plasma protein binding is low. It is characterized by a high degree of metabolism with the formation of 2 main metabolites - hydroxylated and dehydroxylated. The concentration of piribedil in the blood plasma decreases in two phases - T1/2 from 1.7 hours to 6.9 hours. It is excreted mainly in the form of metabolites in the urine: by the kidneys - 68%, with bile - 25%.
PIRIBEDIL (PIRIBEDIL) - Indications
Parkinson's disease (both as monotherapy and in combination with levodopa), chronic cognitive impairment and neurosensory deficits (including attention and memory disorders) in senile dementia (as an additional symptomatic therapy), intermittent claudication due to obliterative diseases arteries of the lower extremities (as an additional therapy), ischemic circulatory disorders of the eye.
Dosage regimen
When taken orally, the daily dose is 50-250 mg. The frequency and duration of use depend on the indications, the patient's response to treatment, and the components of combination therapy.
Side effect
From the digestive system:
rarely - nausea, vomiting, flatulence.
From the side of the central nervous system:
rarely - anxiety, agitation.
From the cardiovascular system:
in some cases - orthostatic hypotension.
Contraindications
Acute myocardial infarction, acute vascular insufficiency, hypersensitivity to piribedil.
Use during pregnancy and breastfeeding
There have been no adequate and well-controlled studies of the safety of piribedil during pregnancy.
In experimental studies
The teratogenic effect of piribedil has not been established.
special instructions
When used in patients with arterial hypertension, simultaneous antihypertensive therapy is necessary.
Should not be used concomitantly with dopamine receptor antagonists.
Drug interactions
When used simultaneously with dopamine receptor antagonists, a mutual decrease in effectiveness is possible.
Possibilities of using piribedil from the point of view of evidence-based medicine
The first non-ergoline dopamine receptor agonist (DRA), piribedil, was developed in the 1970s for the adjunctive treatment of Parkinson's disease (PD). Today, the delayed-release tablet form of piribedil is widely used throughout the world. Indications for the use of piribedil ( Pronoran
) have expanded during this time and now look like this: Parkinson’s disease (PD) (monotherapy for early stages, complex therapy for advanced stages); cognitive impairment and sensorineural deficits; intermittent claudication due to obliterating diseases of the arteries of the lower extremities; ophthalmological diseases of ischemic origin (decreased visual acuity, narrowing of the visual field, decreased color contrast, etc.). Such diverse use of the drug in diseases in the pathogenesis of which dopamine plays an important role (Fig. 1) is due to unique mechanisms of action that distinguish it from other ADRs: partial agonism to dopamine D2 and D3 receptors; antagonism to α2A- and α2C-adrenergic receptors; low affinity for serotonin 5-HT receptors (low risk of developing psychotic disorders); slight affinity for histaminergic and cholinergic receptors.
The use of piribedil in Parkinson's disease
The main directions of pharmacotherapy for PD can be considered: neuroprotective treatment (preventing cell death and slowing the rate of neurodegeneration) and symptomatic therapy (correction of motor and non-motor manifestations of PD). Symptomatic therapy for PD
is currently leading and is based on compensation of dopaminergic deficiency and correction of motor symptoms of parkinsonism (hypokinesia, resting tremor, rigidity).
Attempts are also being made to influence other parts of the pathogenesis of PD (adrenergic, cholinergic, serotonergic imbalance) that cause dopamine-resistant symptoms of PD [1, 2]. Levodopa drugs remain the most effective symptomatic treatment for PD, but due to a number of side effects in most cases (exceptions are old age, severe motor deficits, intolerance, contraindications or ineffectiveness of other antiparkinsonian drugs), it is not recommended to start therapy for PD directly with levodopa drugs. Preference is given to ADRs, MAO-B inhibitors, amantadine [3], which are expected to have a neuroprotective effect [4]. As PD progresses, the prescription of levodopa becomes inevitable, but its combination with other antiparkinsonian drugs makes it possible to take small doses of levodopa for a long time, thereby reducing the risk of adverse events [5]. The effectiveness of piribedil against motor symptoms of PD
(hypokinesia, rigidity, tremors, postural disorders) has been proven in a large series of observations [6–8].
The MDS-EBM (International Society for the Study of PD and Movement Disorders) Working Group assessed piribedil as “effective” and “clinically useful” for the symptomatic treatment of patients in the early stages of PD, either as monotherapy or in combination with levodopa. Due to the lack of results from randomized placebo-controlled trials, “the available evidence is insufficient” to conclude that piribedil is effective in treating and preventing motor fluctuations [9]. The effectiveness of piribedil monotherapy
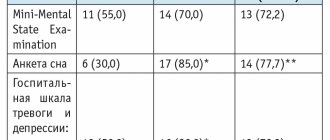
has been demonstrated in two large studies. In the placebo-controlled REGAIN trial [10], untreated patients with early-stage PD were treated for 7 months. received therapy with piribedil (up to 300 mg/day) or placebo, an improvement was achieved in the form of a decrease in the total score by 4.9 (versus a deterioration in the placebo group by 2.6 points) on the Unified Parkinson's Disease Rating Scale (UPDRS) III subscale of physical activity (Table 1) [10] and improvement in the UPDRS II subscale of daily activities. Another open-label study of 113 treatment-naïve patients with PD confirmed the beneficial effects of piribedil monotherapy on major motor symptoms and mood [11].
The effectiveness of piribedil
in combination with levodopa
was assessed in 4 placebo-controlled [12–15] and a number of open studies [16–20].
The results of all studies showed a significant reduction in motor symptoms of PD when piribedil was added to levodopa therapy. Using an average dose of piribedil 150 mg/day for 6 months. all main motor symptoms decreased: tremor - by 72.2%, rigidity - by 66.6%, hypokinesia - by 72.1% [13]. A number of authors emphasize the predominant effect of the drug on tremor [9, 16], however, most studies show effectiveness against all motor symptoms [21]. The effectiveness of piribedil (150 mg/day) was compared with bromocriptine (25 mg/day), as a result, the same effectiveness of these drugs was shown (after 12 months of therapy there was an improvement in UPDRS III: -7.9 ± 9.7 and -8, 0±9.5, respectively) [22]. The effect of piribedil on motor fluctuations
has not been sufficiently studied.
It has been shown that the administration of piribedil less often leads to the development of dyskinesias in animals, and their intensity is significantly lower than with the administration of levodopa [23]. According to a placebo-controlled study [24], a single intravenous infusion of piribedil after 15 minutes effectively reduced movement disorders on the UPDRS III scale and stopped the “off” state in 7 out of 10 patients. In another placebo-controlled crossover study of 30 patients, piribedil was significantly superior to placebo in interrupting OFF episodes with an orodispersible sublingual formula (-13 vs. -7) [25]. These results indicate the effectiveness of piribedil in patients with late stages of PD and fluctuations, but require further testing in larger samples. The effect of piribedil on non-motor symptoms of PD
was studied in studies [22, 26, 27], which determined a positive effect on emotional, motivational and cognitive impairment. The authors emphasize the duration of the effect throughout the year [22]. Similar results were obtained in a domestic study of the effectiveness of piribedil (150–250 mg/day) in 60 patients with PD, in whom, for 6 months. therapy, there was an improvement in neurodynamic characteristics, memory and regulatory functions [4]. When comparing piribedil with other ADRs, its superiority in terms of its effect on cognitive functions is revealed. For example, in a comparative study of piribedil with bromocriptine, a significant improvement in the Wisconsin Card Sorting Test (an assessment of executive function) was shown with piribedil, but not with bromocriptine [22]. The authors explained the additional benefits of piribedil in relation to cognitive functions by its effect on corticolimbic adrenergic and cholinergic transmission [16]. A reduction in depression in patients with PD while taking piribedil was obtained in a number of studies [11, 28]. The antidepressant effect of the drug in this case is very useful, since approximately a third of patients with PD suffer from anxiety and depressive disorders [29]. The frequent occurrence of depression in PD is largely explained by neurochemical disorders, mainly the deficiency of norepinephrine and serotonin that occurs with degeneration of the raphe nuclei, as well as a lack of dopaminergic excitation of the orbitofrontal cortex [30]. The moderate antidepressant effect of piribedil is associated with a dopaminergic effect on the mesolimbic system, as well as with noradrenergic effects (see Fig. 1). Many patients with PD also have motivational disorders and suffer from the symptom complex “anergy, anhedonia, apathy.” This complex is isolated separately from depression; most likely it has a different nature: such patients do not have the features characteristic of depression (feelings of sadness, guilt, hopelessness, pessimism) and respond poorly to therapy with traditional antidepressants. Apathy is observed on average in 40–45% of patients with PD and can occur regardless of depression and cognitive impairment. This symptom is very difficult to treat, and the discovery of piribedil's ability to reduce its severity was an unexpected and useful finding. The positive effect of piribedil (300 mg/day) on apathy and mood disorders was shown in a 12-week placebo-controlled study of 37 patients with PD and apathy [26]: the apathy score improved by 34.6% (in the placebo group - by 3. 2%) on the Starkstein apathy scale and by 46.6% (in the placebo group worsened by 2.3%) on the Robert Inventory apathy score; the Beck depression score improved by 19.8% (in the placebo group it worsened by 1.4%); the Beck anxiety score improved by 22.8% (in the placebo group - by 8.3%); the Beck anhedonia score improved by 49% (in the placebo group - by 5.6%). It is assumed that apathy in PD develops under the influence of mesolimbic dopaminergic deficit. Thus, the effect of piribedil is pathogenetically justified and most likely associated with the effect on dopamine D3 receptors [23]. It should be emphasized that very few drugs have been shown to be effective against apathy [31], and it is important that the effectiveness of piribedil was proven in a randomized, double-blind, placebo-controlled trial.
The use of piribedil for mild and moderate cognitive disorders of various origins
Piribedil (Pronoran) compares favorably with many other drugs due to its large evidence base in terms of the treatment of moderate cognitive impairment (MCI). Its action is due to insufficiency of dopaminergic and adrenergic mediation, which develops in the brain during normal and pathological aging [32, 33]. Even a slight “age-related” dopamine deficiency plays a significant role in the decline of cognitive functions in older people. Naturally, in neurodegenerative and cerebrovascular diseases, neuronal death and neurotransmitter dysfunction increase manyfold, so replenishment of dopaminergic deficiency is useful for any variants of MCI [34]. Since piribedil combines dopaminergic and adrenergic properties, it accordingly improves not only dopaminergic, but also noradrenergic transmission, which is no less important for cognitive activity (maintaining active wakefulness, an adequate level of attention, memory processes). This combined effect enhances the nootropic effect. In addition, it has been shown that the use of Pronoran increases cerebral and peripheral blood supply, which is important for the treatment of patients with cognitive impairment in cerebrovascular diseases [35]. The positive effect of piribedil in MCI of various origins has been shown in more than 10 foreign clinical studies involving about 7000 patients and in a significant number of domestic works, of which the most famous: a study of the effectiveness of Pronoran in mild and moderate cognitive impairment of a vascular nature involving 29 patients - demonstrated a significant decrease in the severity of memory impairment, abstraction and praxis disorders [36]; the Prometheus study involving more than 2000 patients with discirculatory encephalopathy and MCI - after 12 weeks. therapy with Pronoran showed “moderate” or “significant” improvement in cognitive function in 67% of patients [37]; The FUETE study involving 189 patients with MCI on the background of arterial hypertension and cerebral atherosclerosis found a regression of objective cognitive disorders and subjective complaints in all 4 compared therapeutic groups (Pronoran, piracetam, ginkgo biloba extract, vinpocetine), but the severity of the improvement was significantly higher in the Pronoran group [38]; a study of the effectiveness of Pronoran in 55 patients with MCI of various etiologies - showed moderate/marked improvement in patients with both the dysregulatory (vascular) type of MCI (36 and 43% of patients) and the amnestic (Alzheimer's) type of MCI (44 and 36% of patients) [39]; a comparative study of the effectiveness of Pronoran with ginkgo biloba (35 patients with MCI secondary to dyscirculatory encephalopathy in 3 therapeutic groups (Pronoran, Pronoran + ginkgo biloba, ginkgo biloba) - showed significant improvement in the Pronoran group, significantly superior to the improvement in the monotherapy group with ginkgo biloba [40].A number of multicenter randomized placebo-controlled studies of the effectiveness and safety of piribedil have been conducted abroad.In particular, a 90-day double-blind study found an improvement in cognitive scores on the Mini-Mental State Examination (MMSE) [41, 42], a positive effect on thinking (comprehension, reasoning, developing strategies and problem solving) [43].In a study by S. Corradino [44], it was shown that therapy with Pronoran 50 mg for 3 months leads to an improvement in cognitive functions by 33% (especially memory ) and an increase in the level of wakefulness by 34%. With the use of a dose of 50 mg, there is an improvement not only in cognitive functions, but also in a number of sensory indicators of an asthenic-depressive nature, there is a significant decrease in visual, auditory disorders and dizziness (in 41, 71 and 84% of patients respectively) [45, 46], depressive and anxiety symptoms, patients complain less of forgetfulness, headaches, fatigue, and noise in the head. Thus, for the treatment of cognitive disorders, high doses of the drug are not required; a dose of 50 mg (1 tablet) per day is sufficient. This dosage is considered effective and safe, well tolerated by patients and does not cause serious adverse reactions.
Side effects of piribedil
Side effects (AEs) of piribedil are comparable in spectrum and frequency of occurrence to those of other non-ergoline ADRs [11]. Most AEs are dose-dependent and decrease or disappear when the dose of the drug taken is reduced. The most common gastrointestinal symptoms, according to clinical studies, are nausea/vomiting (0–33% of cases, according to various sources) and hypotension/dizziness (3–30%). The strategy to combat these PEs includes taking the drug after meals and taking the peripheral dopamine receptor blocker domperidone, which eliminates the dopaminergic effects of levodopa and ADR outside the central nervous system. There is evidence that domperidone enhances the effect of piribedil, causing a more intense and prolonged increase in motor activity and a decrease in cognitive deficits [47]. A fairly common AE during ADR therapy are attacks of daytime sleepiness (2–30%), but a number of studies did not find any differences between piribedil and placebo [48]. Additionally, a randomized, blinded trial showed that switching to piribedil in PD patients experiencing sudden daytime sleepiness while on pramipexole or ropinirole resulted in a significant reduction in sleepiness, improvements in Epworth Sleepiness Scale scores, and overall treatment experience, with no changes in motor function. characteristics [26]. These results suggest a lower risk of drowsiness with piribedil, which is explained by the additional adrenergic properties that increase wakefulness and alertness. Psychiatric disorders are another type of AE expected when ADR is prescribed, especially in older patients and in the presence of cognitive deficits. In this case, a longer titration and lower therapeutic doses of ADR are recommended. During piribedil therapy, psychotic disorders were observed with varying frequencies (4–23%), but it should be noted that in a number of studies their rates were comparable to those taking placebo. For example, in a study by O. Rascol et al. [25] psychiatric disorders were reported in 2.3% of cases with piribedil and 1.8% with placebo. In another comparative study of piribedil (150 mg/day) and bromocriptine (25 mg/day) with levodopa in patients with early stages of PD, the frequency of hallucinations on piribedil was 8.1%, on bromocriptine - 2.8%, withdrew from the study due to with this PE, 2.9% and 1.4% of patients, respectively [20].
Conclusion
To summarize, it should be noted that the use of piribedil in the treatment of PD is effective as monotherapy in the early stages and in combination with levodopa in advanced stages. There is no doubt about its beneficial effect on the motor manifestations of PD, as well as on a number of non-motor disorders, and its neuroprotective effect is assumed. Piribedil is not inferior in effectiveness and tolerability to other non-ergoline ADRs, in addition, it has adrenergic properties, suggesting additional potential for influencing non-motor symptoms of PD, such as depression, apathy and cognitive deficits. The effectiveness and safety of the use of piribedil in patients with mild and moderate cognitive deficits has now been confirmed by multiple clinical studies. The drug has a positive effect on cognitive functions in most patients, improving thinking, memory and attention, and also has a positive effect on neurosensory deficits in the elderly. It is recommended to start treatment as early as possible, since piribedil therapy is effective in pre-dementia stages of cognitive impairment.
Parkinson's disease (PD) is a chronic, progressive brain disease associated with the degeneration of dopaminergic neurons in the substantia nigra and the formation of intracellular Lewy bodies. PD is manifested by a combination of hypokinesia with rigidity, resting tremor and postural instability, as well as a wide range of non-motor manifestations (mental, autonomic, sensory, etc.).
According to various researchers, the average prevalence of PD is 100 cases per 100,000 population. Incidence of B.P. increases with age and reaches 55 people per 100,000 in 70-year-olds and 220 per 100,000 in people over 85 years of age [1, 2].
In recent years, dopamine receptor agonists (DRAs), which, due to their chemical properties, directly stimulate dopamine receptors, reproducing the effect of dopamine, have been increasingly used to treat PD at different stages. Since 1971, they were first prescribed to patients with PD as an addition to levodopa, but it was subsequently found that in the early stages of PD, ADRs have an effect comparable in effectiveness to levodopa. In addition, their early administration reduces the risk of motor fluctuations and drug-induced dyskinesias. With their help, they effectively control the main symptoms of PD, including tremor, and reduce the severity of depression and anxiety.
ADR does not interact with food proteins during transport through the gastrointestinal tract and blood-brain barrier, unlike levodopa drugs. In addition, ADR has a longer plasma half-life. This class of drugs provides longer-lasting, physiological-like, selective stimulation of dopamine receptors. The metabolism of ADR does not produce free radicals, which can accelerate neuronal apoptosis in PD [3, 4].
In recent years, the possibility of a neuroprotective effect of ADR in PD and its influence on the rate of disease progression has been actively studied. The possible neuroprotective effect of ADR is associated with a decrease in dopamine synthesis, an antioxidant effect, and stimulation of the autotrophic function of neurons [5, 6].
ADRs are used both in the early stages of PD as monotherapy or in combination with amantadines, MAO type B inhibitors, anticholinergics, and in advanced stages of the disease as an addition to levodopa.
The article presents 2 clinical observations of patients with PD at the early and advanced stages of the disease.
Observation 1.
Patient
V.
, 46 years old, complained of trembling at rest and awkwardness in her right hand. The symptoms first appeared 6 months ago, when the patient noticed that it became difficult for her to write, her handwriting changed, she began to perform slower and worse small movements with her right hand, then a tremor appeared in this hand, occurring at rest.
In the clinical picture: hypomimia, rare blinking, bradyllalia, hypokinesia, increased tone of the extrapyramidal type, pronounced resting tremor in the right limbs, acheirokinesis on the right. There is no postural instability.
During the examination, symptoms of anxiety and depression were noted in the form of depression, decreased range of interests, apathy, increased fatigue, decreased ability to concentrate, and sleep disturbances. Mild cognitive impairment of a subcortical nature was revealed in the form of a decrease in the speed of performing neuropsychological tests. When examining cognitive function using the Mini Mental State Examination (MMSE), a score of 27 was obtained.
A diagnosis of PD, mixed form, stage 1 according to Hoehn and Yahr was made. Mild cognitive impairment. Affective disorders (depressive syndrome).” Therapy was prescribed: piribedil (pronoran) 50 mg with a gradual increase in dose once a week to 150 mg/day. When re-examined after 3 months, the patient noted positive dynamics in her condition, the severity of tremor, hypokinesia and rigidity in the right extremities decreased, and her gait improved. The patient began to perform daily work better, her handwriting improved, and her performance was restored. In addition, mood and concentration improved significantly, and sleep normalized. The repeated assessment on the MMSE scale was 30 points.
Observation 2.
Patient
I.
, 63 years old, complained of slowness of movements, general stiffness, trembling in the hands, more on the left, instability when walking, frequent falls and freezing, violent movements in the limbs. Symptoms first appeared 12 years ago, when tremors appeared at rest in the left arm, then awkwardness and slowness of movements in the left arm and leg. After 2 years, trembling and awkwardness in the right limbs began. At the clinic, a diagnosis of PD was made and amantadine 300 mg/day was prescribed. During therapy, the patient did not notice any changes in her well-being.
A few months later, instability appeared when walking, and therefore levodopa/benserazide 300 mg/day was prescribed. The patient noted a short-term improvement, she began to maintain balance better, stiffness, slowness of movements and tremors, and walking disturbances decreased. However, the disease continued to progress steadily, and the symptoms began to increase. The dose of levodopa was increased to 900 mg/day over 10 years. In the last 3 years, I began to notice a reduction in the duration of action of a single dose of levodopa to 2 hours and the appearance of violent movements in the limbs 1 hour after taking a single dose of levodopa. In the clinical picture: hypomimia, rare blinking, hypophonia, bradyllalia, axial rigidity, hypokinesia on both sides, more on the left, increased tone of the extrapyramidal type on both sides, more on the left, pronounced rest tremor on both sides, more on the left, drug-induced dyskinesia of peak dose in the form of generalized choreoathetosis, pronounced postural instability, microbasia with frequent freezing. A diagnosis was made of “mixed form of PD, stage 4 according to Hoehn and Yahr. The phenomenon of single-dose levodopa depletion. Drug-induced peak dose dyskinesias."
Piribedil was added to the therapy at a dose of 50 mg with a gradual increase to 150 mg/day; in parallel, the dose of levodopa was gradually reduced to 650 mg/day. As a result of correction of therapy, freezing and falling became less common, and the severity of violent movements decreased; the duration of the switching period has increased.
In the 1st clinical observation, a relatively young patient with an early stage of PD, affective and mild cognitive disorders was prescribed piribedil (pronoran) as monotherapy, which ensured good control of motor disorders, regression of mild cognitive and depressive disorders.
In the 2nd observation, piribedil (pronoran) was prescribed in combination with levodopa, which made it possible to gradually reduce the daily dose of levodopa and reduce the severity of levodopa-induced dyskinesias. In addition, motor fluctuations also decreased (the “dose depletion” phenomenon).
Piribedil (pronoran) is a non-ergoline dopamine receptor agonist. It is the only agonist that increases the activity of both dopaminergic and noradrenergic systems.
Piribedil (pronoran) stimulates the D3 subtype of D2 receptors and also blocks presynaptic α2 adrenergic receptors, thereby enhancing noradrenergic transmission. Provides a therapeutic effect approaching the effect of levodopa and tonic stimulation of dopamine receptors in the striatum, which is associated with a low risk of developing fluctuations and dyskinesias. In addition, piribedil (pronoran) blocks alpha-2-noradrenergic receptors, eliminating symptoms of PD that are insensitive to levodopa - disturbances in posture, gait, and postural instability. Motor freezing is a special type of gait disturbance in PD; they are associated with the loss of postural reflexes, as well as activation of antagonist muscles. This phenomenon may be a kind of equivalent to specific action dystonia that occurs when walking. It is believed that freezing develops as a result of impaired release of norepinephrine in the frontal cortex [7–9]. In addition to the nigrostriatal dopaminergic pathway, which is associated with the regulation of movements, there are mesolimbic and mesocortical dopaminergic pathways. The mesolimbic pathway is associated with the functions of mood, emotions and motivation, while the mesocortical pathway provides the processes of attention, concentration and memory. Stimulation of the D3 type of D2 receptors in the limbic system is associated with the antidepressant effect of ADR. Since piribedil is an α2-adrenergic receptor antagonist, it improves noradrenergic transmission in the cortex, limbic system and locus coeruleus. The key source of ascending noradrenergic mediation is the locus coeruleus of the brainstem. Axons of noradrenergic neurons of the locus coeruleus project to all parts of the cerebral cortex. By increasing the activity of the noradrenergic system, piribedil stimulates cholinergic transmission in the cerebral cortex, which improves posture and gait in patients with PD, as well as cognitive function and attention. The role of noradrenergic mediation in cognitive processes is due to ensuring concentration of attention and mnestic processes, processing of sensory information. Insufficiency of the noradrenergic system is associated with slow mental processes, decreased attention, depression, and walking disorders in patients with PD. [10, 11]. Also, the noradrenergic activity of piribedil (pronoran) helps prevent autonomic disorders, primarily orthostatic hypotension, characteristic of patients with PD [7].
Thus, 2 clinical observations demonstrate the advisability of prescribing piribedil (pronoran) in the early and advanced stages of PD in order to correct motor, affective and mild cognitive disorders, as well as correct motor fluctuations. Prescribing pronoran to patients with late stages of PD leads to an increase in the duration of the “on” period, a decrease in the duration of the “off” period, and an increase in the duration and effectiveness of a single dose of dopamine-containing drugs.
Monotherapy with piribedil (pronoran) can delay the administration of levodopa and prevent motor fluctuations and dyskinesias. In addition, it may prevent the death of dopaminergic neurons caused by the action of levodopa. According to various data, ADRs can delay the need to prescribe levodopa for 3-5 years.
Piribedil (pronoran) occupies a special place among other ADRs due to its effect on adrenergic and noradrenergic neurotransmission, which makes it possible to influence affective, cognitive disorders and a number of non-motor symptoms of PD.