pharmachologic effect
An antifungal drug for external use with a wide spectrum of antifungal activity. In small concentrations, terbinafine has a fungicidal effect against dermatophytes (Trychophyton rubrum, Trychophyton mentagrophytes, Trychophyton verrucosum, Trychophyton violaceum, Trychophyton tonsurans, Microsporum canis, Epidermophyton floccosum), yeast fungi (mainly Candida albicans) and certain dimorphic fungi (Pityrosporum orbiculare).
Activity against yeast-like fungi, depending on their type, can be fungicidal or fungistatic.
Terbinafine does not affect the metabolism of hormones or other drugs.
The minimum inhibitory concentration for Trychophyton rubrum is 0.001-0.06 μg/ml. For onychomycosis of the hands, the effectiveness of treatment is 95%, for onychomycosis of the feet - more than 90%. With chronic dermatophytosis of smooth skin, remission is achieved in 75-95% of patients. Subjective improvement in the treatment of progressive candidiasis of smooth skin and lesions of large and interdigital folds, paronychia, caused by Candida albicans and resistant to therapy with nystatin, levorin in combination with clotrimazole and miconazole, occurs within 3-4 days, and complete resolution of the process occurs after 3-5 weeks
Terbinafine ointment
Registration number: R No. LSR-008761/09
Trade name of the drug: Terbinafine-MFF.
International nonproprietary name: Terbinafine.
Dosage form: Ointment for external use.
Composition per 100 g of ointment: Active substance:
- Terbinafine hydrochloride - 1.00 g
- Excipients: - up to 100 g
- Methyl parahydroxybenzoate (methylparaben) - 0.10 g
- Carbomer (rarely cross-linked polyacrylic acid mAPS-06) - 1.50 g
- Polysorbate - 80 (Tween - 80) - 1.00 g
- Vaseline oil - 5.00 g
- Propylene glycol - 10.00 g
- Sodium hydroxide (sodium hydroxide) - 0.40 g
- Purified water - 81.00 g
Description: White ointment with a characteristic odor.
Pharmacotherapeutic group: Antifungal agent.
ATX code: D01AE15
Pharmacological properties: Antifungal drug for topical use with a wide spectrum of antifungal activity. In small concentrations, terbinafine has a fungicidal effect against dermatophytes (Trichophyton rubrum, T.mentagrophytes, T.verrucosum, T.violaceum, T.tonsurans, Microsporum canis, Epidermophyton floccosum), molds (mainly Candida albicans and certain dimorphic fungi (Pityrosporum orbiculare Activity against yeast fungi, depending on their type, can be fungicidal or fungistatic. Terbinafine specifically changes the early stage of sterol biosynthesis occurring in fungi. This leads to ergosterol deficiency and intracellular accumulation of squalene, which causes fungal cell death. Terbinafine acts by inhibiting the enzyme squalene epoxidase located on the cell membrane of the fungus.Terbinafine does not affect the cytochrome P450 system in humans and, accordingly, the metabolism of hormones or other drugs.
Pharmacokinetics: When applied topically, absorption is less than 5% and has a slight systemic effect.
Indications for use: Prevention and treatment of fungal skin infections, including mycoses of the feet (“fungus” of the foot), inguinal athlete’s foot (tinea cruris), fungal infections of the smooth skin of the body (tinea corporis), caused by dermatophytes such as Trichophyton (including , T.rubrum, T.mentagrophytes, T.verruco-sum, T.violaceum), Microsporum canis and Epidermophyton floccosum. Yeast infections of the skin, mainly those caused by the Candida genus (eg, Candida albicans), particularly diaper rash. Versicolor (Pityriasis versicolor), caused by Pityrosporum orbiculare (also known as Malassezia furfur).
Contraindications: Hypersensitivity to terbinafine or to any of the inactive ingredients included in the drug. Chronic or active liver diseases, chronic renal failure (creatinine clearance 50 ml/min), children under 12 years of age (lack of sufficient clinical experience).
With caution: Hepatic and/or renal failure, alcoholism, suppression of bone marrow hematopoiesis, tumors, metabolic diseases, occlusive vascular diseases of the extremities.
Pregnancy and lactation: In experimental studies, teratogenic properties of terbinafine were not identified. The use of the drug during pregnancy is possible in cases where the expected benefit to the mother outweighs the possible risk to the fetus. Terbinafine is excreted in breast milk. If it is necessary to use the drug during lactation, the issue of stopping breastfeeding should be decided.
Directions for use and dosage: Externally. Adults and children over 12 years of age: Before applying the ointment, clean and dry the affected areas. The ointment is applied once or twice a day in a thin layer to the affected skin and surrounding areas and rubbed in lightly. For infections accompanied by diaper rash (under the mammary glands, in the spaces between the fingers, between the buttocks, in the groin area), the places where the ointment is applied can be covered with gauze, especially at night.
Average duration of treatment:
- Dermatomycosis of the trunk, legs: 1 week 1 time per day
- Ringworm of the feet: 1 week 1 time per day Candidiasis of the skin: 1-2 weeks 1 or 2 times per day
- Tinea versicolor: 2 weeks 1 or 2 times a day.
A decrease in the severity of clinical manifestations is usually observed in the first days of treatment. If treatment is not regular or is stopped prematurely, there is a risk of the infection returning. If after one to two weeks of treatment there are no signs of improvement, the diagnosis should be verified.
The dosage regimen for terbinafine ointment in the elderly does not differ from that described above.
Use of the drug in children: The use of this drug in children under 12 years of age is not recommended.
Side effects: Redness, itching or burning sensation may appear at the sites where the drug is applied. Allergic reactions.
Overdose: No cases of drug overdose have been reported. If terbinafine ointment is accidentally taken orally, you can expect the same side effects to develop as with an overdose of terbinafine tablets (headache, nausea, epigastric pain and dizziness).
Treatment: Activated carbon, if necessary, symptomatic maintenance therapy.
Interactions: There are no known drug interactions for terbinafine ointment.
Special instructions: A decrease in the severity of clinical manifestations is usually observed in the first days of treatment. In case of irregular treatment or its premature termination, there is a risk of recurrence of infection. Terbinafine ointment is for external use only. Avoid contact with eyes as it may cause irritation. If the drug accidentally gets into your eyes, they should be immediately rinsed with running water, and if persistent irritation develops, you should consult a doctor. If allergic reactions develop, the drug must be discontinued.
Release form: Ointment for external use 1%. 10 g or 15 g in aluminum tubes with bouchons made of polymer materials. The tube with instructions for use is packed in a cardboard box.
Shelf life: 2 years. Do not use after expiration date.
Storage conditions: Store at a temperature not exceeding + 25°C. Keep out of the reach of children.
Conditions for dispensing from pharmacies: Without a doctor's prescription.
Contraindications
Hypersensitivity to terbinafine or to any of the inactive ingredients included in the drug.
Carefully
Renal/liver failure, alcoholism, suppression of bone marrow hematopoiesis, tumors, metabolic diseases, occlusive vascular diseases of the extremities, pregnancy, breastfeeding, children under 12 years of age (lack of sufficient clinical experience of use).
Use during pregnancy and breastfeeding
In experimental studies, teratogenic properties of terbinafine were not identified. To date, no malformations have been reported with the use of Terbinafine cream. However, since clinical experience with the use of Terbinafine cream in pregnant women is very limited, it should be used only for strict indications.
Terbinafine is excreted in breast milk. However, if a nursing mother uses Terbinafine cream, a small amount of the active substance is absorbed through the skin, so adverse effects on the baby are unlikely.
The cream should not be applied to the mammary glands during breastfeeding.
During pregnancy and breastfeeding, use only if the expected benefit to the mother outweighs the potential risk to the fetus or child.
Composition of Terbinafine ointment
The main component is terbinafine hydrochloride. In one tube it is contained in the amount of 1g per 100g of composition. As additional substances, it contains rare cross-linked polyacrylic acid in the amount of 1.5 g, as well as 10 g of propylene glycol, 5 g of petroleum jelly, 0.4 g of sodium hydroxide. A large share of the volume is purified water - here it is 81g.
Terbinafine is available both as an ointment and as a gel or cream. The product for topical use is packaged in aluminum tubes, which are placed in cardboard packages, 1 piece each.
special instructions
Irregular use or early termination of treatment increases the risk of relapse. If after 2 weeks of treatment there is no improvement in the condition, it is necessary to re-determine the causative agent of the disease and its sensitivity to the drug. During the treatment process, it is necessary to follow general hygiene rules to prevent reinfection (through underwear, shoes). Avoid contact with the mucous membrane of the eyes, nose, and mouth.
Impact on the ability to drive vehicles and operate machinery
During the period of treatment with the drug, it is possible to drive vehicles and engage in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Modern possibilities of using terbinafine for the treatment of fungal diseases
The incidence rate increases significantly in patients in older age groups, regardless of gender. According to foreign researchers, onychomycosis affects from 2 to 18.5% of the total population of the planet, and in the age group of 70 years and older, 50% of the world’s population is affected by this disease [1,8]. According to various authors, fungal infections of the feet are observed in a third of all European residents [18,20]. As a rule, the development of onychomycosis is preceded by mycosis of the feet - according to our data, only 30% of patients had isolated onychomycosis, in the remaining 70% of patients it was combined with mycosis, which began before the fungal infection of the nails [2]. Thus, treatment of mycosis of the feet is the prevention of the development of onychomycosis. Very often, dermatologists are faced with insufficient awareness of patients - the latter do not know about the presence of a fungal infection, even seeing manifestations on the skin in the form of peeling, intertrigo, hyperkeratosis, and attribute this to physiological characteristics or age-related changes. On the other hand, some patients, seeing changes in the nail plates, regard this as onychomycosis and begin to treat it themselves with all available means. In the presence of mycosis of smooth skin without affecting the nails and involving the hair in the process, a cure can be achieved using only topical antimycotics. One of the most active antimycotics is terbinafine. It belongs to allylamine derivatives. In terms of the breadth of the spectrum of antifungal action, this drug surpasses all other antifungal drugs: polyene antibiotics, azoles (imidazole derivatives - clotrimazole, ketoconazole, etc., as well as first generation triazoles - itraconazole, fluconazole, etc.) and echinocandins. In recent years, many studies have been conducted confirming the high effectiveness and safety of terbinafine (Lamisil) in the treatment of fungal infections. The undoubted advantages of this drug include a large number of its forms for external use - cream, dermgel, spray and film-forming solution for the treatment of types of mycosis. Terbinafine in the form of a cream is ideal for squamous and squamous-hyperkeratotic forms. In the first case, it is enough to apply the cream to the affected area once a day. within 7 days [15]. For the treatment of hyperkeratotic forms of mycosis, use the drug 2 times a day. within 2 weeks. makes it possible to achieve clinical and mycological cure. In a study conducted by Yu.N. Perlamutrov and K.B. Olkhovskaya, it has been shown that complete mycological cure is achieved with the use of terbinafine 1 time per day. within 2 weeks. occurred in 80% of patients, and 2 times a day. – in 93%. At the same time, by the end of the course of treatment, the disappearance of peeling, itching and healing of deep and superficial cracks was observed in patients in both groups, but when using the cream 2 times a day. these symptoms resolved more quickly [4]. For intertriginous and dyshidrotic forms, it is appropriate to prescribe dermgel or spray - they have a pronounced antipruritic and drying effect. It is also convenient to prescribe the spray in the presence of lesions on smooth skin (lichen versicolor, microsporia) in the folds and on the scalp. So, according to A.A. Haldina et al., when applying both spray and dermgel to lesions in large folds, etiological cure was observed in 100% of cases, regardless of the nature of mycosis (Tr. rubrum, Ep. floccosum, C. albicans). When analyzing the dynamics of regression of skin symptoms, it was revealed that when using the spray, the regression of clinical symptoms is somewhat ahead of that when using dermgel, this is especially noticeable with the regression of itching and maceration [7]. There is a high effectiveness of using spray and dermgel for the treatment of patients with pityriasis versicolor. According to L.P. Kotrekhova et al., the effectiveness of dermgel and spray therapy was 94.8 and 93.8%, respectively. At the same time, patients note the ease of use and good organoleptic properties of the drug, such as the absence of greasiness and oily sheen of the skin. The hygroscopic properties of the drug made it possible to apply it to skin folds even in obese patients [3]. A new, and certainly promising form is a film-forming solution, which is applied to the skin of the feet once. N.N. Potekaev et al. treated 20 patients with various forms of mycosis of the feet with Lamisil Uno. Clinical and mycological cure occurred in 80% of patients by the 10th day of observation. The drug was ineffective in the squamous-hyperkeratotic form. For erased, squamous and intertriginous forms, the effectiveness is 100%. I would especially like to note that single use of the drug is very convenient for patients [5]. A randomized, double-blind, placebo-controlled study was conducted on the effectiveness of a single application of a 1% film-forming solution of terbinafine in 324 patients with mycosis of the feet. The result was assessed after 6 weeks. after using the drug. The study found negative culture, microscopy, and mycological cure rates of 91%, 81%, and 78%, respectively, while the placebo response rate was 17% [11]. Another very important point is the possibility of curing mycosis in a short time - with squamous and intertriginous forms of the lesion, the disease is cured in 1 week, while azole drugs must be used for 4 weeks. [17,18]. A longer course of therapy often leads to non-compliance with the treatment regimen; patients stop using the drug after visible improvements and are not treated further, which leads to relapse of the disease. In some cases (with damage to the nail plates, a common skin process, hair involvement), local antifungal therapy is not effective enough, and there is a need to prescribe a systemic drug, the most effective and safe of which is terbinafine [19]. Terbinafine has a fungicidal effect on dermatophytes, molds and some dimorphic fungi; on yeast fungi, depending on their type, it has a fungistatic or fungicidal effect [13,16]. The pronounced antimycotic effect of terbinafine also manifests itself in vivo, which is facilitated by its pharmacokinetics. After oral administration, the maximum concentration of terbinafine in the blood is reached within 2 hours, the drug is almost completely bound to plasma proteins. Due to its lipophilicity, terbinafine quickly diffuses through the dermis and accumulates in the stratum corneum and nail plates, and is also excreted with sebum, resulting in high concentrations of the drug in hair follicles and hair. Stable concentrations of terbinafine in tissues are achieved 10–14 days after the start of oral administration, the half-life of its elimination varies from 24 to 156 days, as a result of which the drug remains in the nail plates for a long time after stopping its use [8,10]. It is known that fungal infections of the scalp can be successfully treated with terbinafine. To confirm this, 3 groups of children aged 2 to 14 years with a confirmed diagnosis of trichophytosis were treated with griseofulvin for a month and terbinafine for 2 weeks. and 1 month It was shown that the effectiveness of therapy was approximately the same and amounted to 100% with griseofulvin, 95% with a 2-week course of terbinafine and 94.1% with a monthly dose [12]. A study was conducted on the effectiveness of oral terbinafine for the treatment of a hyperkeratotic form of mycosis of the feet with a torpid course. The drug at a dose of 125 mg was prescribed daily for 1 month. It was found that the maximum concentration of the drug (247.8 ng) in the stratum corneum of the epidermis was determined by the end of 1 week. treatment, which is 50 times the minimum inhibitory concentration for dermatophytes. After 6 weeks the concentration of the drug decreased to 50.73 ng, and after 8 weeks. terbinafine was no longer detectable in the skin. The effectiveness of therapy was 95% [14]. The low potential for drug interactions with other drugs is also important, because Onychomycosis often affects older people who are forced to take a large number of different medications for other diseases [13]. Thus, based on the analysis of literature data, we can conclude that terbinafine (Lamisil) is a highly effective drug for the treatment of fungal infections, has a large number of different forms, which significantly expand the possibilities of antifungal therapy. Literature 1. Malcolm B. Athlete's foot // Attending physician. 1998. No. 6. 2. Vasenova V.Yu. Immunopathogenesis, morphofunctional characteristics, clinical picture, complex therapy and prevention of onychomycosis: Abstract of thesis. ... doc. honey. Sci. M., 2008. 3. Kotrekhova L.P., Vasilyeva N.V., Raznatovsky K.I., Piotrovskaya I.V. Clinical efficacy and safety of terbinafine (Lamisil spray, Lamisil dermgel) in the treatment of pityriasis versicolor // Clinical dermatology and venereology. 2007. No. 3. P. 35–38. 4. Perlamutrov Yu.N., Olkhovskaya K.B. Optimization of therapy for mycoses of the feet in women using 1% Lamisil cream // Clinical dermatology and venereology. 2006. No. 2. P. 78–80. 5. Potekaev N.N., Serov D.G., Dvoryankova E.V., Zhukovsky R.O. Effective therapy of mycoses of the feet with a single use of a new external form of terbinafine - a film-forming solution of Lamisil Uno // Clinical Dermatology and Venereology. 2008. No. 4. pp. 85–88. 6. Sergeev A.Yu., Ivanov O.L., Sergeev A.Yu. and others. Study of modern epidemiology of onychomycosis // Bulletin of Dermatology and Venereology. 2002. No. 3. P. 31–35. 7. Khaldin A.A., Tsykin A.A., Izyumova I.M. Clinical and etiological effectiveness of 1% Lamisil® spray in the treatment of fungal infections of large skin folds // Russian Journal of Skin and Venereal Diseases. 2007. No. 1. P. 56. 8. Baran R. Onychomycosis: the current approach to diagnosis and therapy. London: Malden MA, 1999. 9. Chen SCA, Sorrell TC New Drugs, Old Drugs. Antifungal agents // Med. J. Austral. 2007. Vol. 187. No. 7. R. 404–409. 10. Cribier BJ, Bakshi R. Terbinafin in the treatment of onychomycosis: a review of its efficacy in high-risk populations and in patients with nondermatophyte infections // BJ Dermatol. 2004. Vol.150. R. 414–420. 11. De Chauvin MF, Viguie-Vallanet C., Kienzler JL, Larnier C. Novel, single-dose, topical treatment of tinea pedis using terbinafine: results of a dose-finding clinical trial. Mycoses. 2008 Jan. Vol. 51(1). R. 1–6. 12. Deng S., Hu H., Abliz P., Wan Z., Wang A., Cheng W., Li R. A random comparative study of terbinafine versus griseofulvin in patients with tinea capitis in Western China. Mycopathologia. 2011 Nov. Vol. 172(5). R. 365–372. 13. Gianni C. Update on antifungal therapy with terbinafine // G Ital Dermatol Venereol. 2010 Jun. Vol. 145(3). R. 415–424. 14. Kikuchi I., Tanuma H., Morimoto K., Kawana S. Usefulness and pharmacokinetic study of oral terbinafine for hyperkeratotic-type tinea pedis // Mycoses. 2008 Nov. Vol. 51(6). R. 523–531. 15. Korting HC, Kiencke P., Nelles S., Rychlik R. Comparable efficacy and safety of various topical formulations of terbinafine in tinea pedis irrespective of the treatment regimen: results of a meta-analysis // Am J Clin Dermatol. 2007. Vol. 8 (6). R. 357–364. 16. Revankar SG, Nailor MD, Sobel JD Use of terbinafine in rare and refractory mycoses // Future Microbiol. 2008 Feb. Vol. 3(1). R. 9–17. 17. Schafer–Korting M., Schoellmann C., Korting HC Fungicidal activity plus reservoir effect allow short treatment courses with terbinafine in tinea pedis // Skin Pharmacol Physiol. 2008. Vol. 21(4). R. 203–210. 18. Schmid–Wendtner MH, Korting H. Topical terbinafine. Reduction of duration of therapy for tinea pedis // Hautarzt. 2008 Dec. Vol. 59 (12). R. 986–991. 19. Singal A., Khanna D. Onychomycosis: Diagnosis and management // Indian J Dermatol Venereol Leprol. 2011 Nov–Dec. Vol. 77(6). R. 659–672. 20. Stock I. Antimycotic therapy of Tinea pedis and other foot mycoses // Med Monatsschr Pharm. 2008 Jul. Vol. 31(7). R. 247–258. Van Duyn Graham L., Elewski BE. Recent updates in oral terbinafine: its use in onychomycosis and tinea capitis in the US // Mycoses. 2011 Nov. Vol. 54 (6). R. 679–685.
Directions for use and doses
Externally.
Adults and children over 12 years of age: apply the cream to the affected skin and adjacent areas in a thin layer, lightly rubbing, 1 or 2 times a day. The duration of treatment depends on the indication and severity of the disease. The course of treatment is on average 2-4 weeks. Duration and frequency of use: dermatomycosis of the trunk, legs, feet - 1 time per day for 1 week; skin candidiasis - 1-2 times a day for 1-2 weeks; lichen versicolor - 1-2 times a day for 2 weeks.
Terbinafine cream - instructions
Unlike ointment, cream does not penetrate so deeply into the skin. Part of the applied layer is often rubbed off on clothing and surfaces with which the affected area of the body comes into contact. Therefore, the use of cream can be increased up to 3 times a day.
The advantage of the cream is its effectiveness even on moderately wet surfaces, which is especially important for fungal skin infections. If it is not possible to dry the surface due to the constant release of liquid, it is better to buy a cream, since the ointment in this case will be ineffective.
Terbinafine – experience of 20 years of use
Terbinafine hydrochloride (hereinafter referred to as terbinafine), 1% cream, is marketed under the trade name Lamisil®.
The drug was first registered in the EU in the UK in October 1990 and went on sale as a prescription drug in 1992. Currently, Lamisil® cream is registered in 101 countries and is on the market in 92 countries, including all European countries. In 44 countries (Australia, Denmark, Finland, France, Germany, Norway, Sweden, USA, Great Britain, in some countries of Eastern Europe, Asia and Latin America) it has over-the-counter status.
Terbinafine cream (Lamisil®) is used to treat various fungal skin diseases caused by dermatophytes (tinea glabrous, athlete's foot, athlete's foot), fungal infections (cutaneous candidiasis), and tinea versicolor.
Dermatophytosis is basically a superficial infection of the skin, hair and nails. With these infections, lesions can occur anywhere on the body and are characterized by erythema, small papules, vesicles, fissures and desquamation. They usually occur in a mild or moderate form, but many patients complain of pain, swelling, itching and burning. In addition to discomfort, patients may experience distress.
Cutaneous candidiasis is caused by Candida yeast, the most common of which is Candida albicans. The disease resembles dermatophytosis with skin redness, itching and peeling; in more severe cases, pustules and exudation appear. This disease can develop against the background of other skin infections, including dermatophytosis. Specific diagnostics consists of identifying the pathogen in a specific culture.
Tinea versicolor is caused by the yeast Pityrosporum orbiculare (their saprophytic form in human skin is called Malassezia furfur). It is a recurrent skin disease with areas of depigmentation, peeling and redness. After the doctor has made the diagnosis for the first time (it should be differentiated from other depigmentation and/or skin diseases accompanied by peeling, i.e., vitiligo and eczema), the patient can easily determine the relapse in the future.
This article presents the results of studies on the clinical pharmacology, effectiveness and safety of the drug terbinafine.
Terbinafine hydrochloride is a new class of antifungal agents, allylamines. The fungicidal effect of terbinafine is the inhibition of squalene epoxidase, an enzyme in the biosynthesis of ergosterol, which in turn disrupts biosynthesis in the membrane of fungal cells and causes their death. In comparison, rat liver squalene epoxidase is almost 2000 times less sensitive to terbinafine compared to the fungal enzyme. This selectivity and specificity of action gives reason to believe that people will not experience adverse events due to the mechanism of action of the active substance.
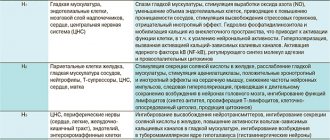
The ability of Lamisil® cream to cause local irritation and sensitization has been sufficiently studied in healthy volunteers. The results are presented in the table.
The data obtained indicate that Lamisil® cream, when applied to intact or scarified skin, extremely rarely causes adverse reactions due to irritation, contact sensitization, phototoxicity or photosensitization. The drug is no different from placebo or other known topical antifungals.
The effectiveness of Lamisil® cream has been well studied in clinical studies, on the basis of which the drug is approved for the treatment of fungal skin infections caused by dermatophytes (athlete's foot, athlete's foot inguinal and ringworm of smooth skin), fungal infections caused by Candida species (C. albicans), and lichen versicolor .
Only the main results of clinical studies are presented here.
Effective against athlete's foot (use once a day for one week)
In 135 patients with athlete's foot (athlete's foot), it was shown that Lamisil® cream with this regimen of use provided a mycological cure in 90% of cases and the effectiveness of treatment (mycological + clinical effect in eliminating all minor signs and symptoms) was 74–92%. These figures are significantly higher than in the placebo (vehicle) group. They correspond to the indicators with more frequent or prolonged use of the drug, i.e. there is no need to increase the duration of therapy [1].
Five clinical studies were conducted in 248 patients to evaluate the effectiveness and tolerability of Lamisil® cream in this treatment regimen. It was found that the drug provided mycological cure in 84–100% of cases and the effectiveness of treatment (mycological + clinical effect) was also 96–100%. These figures are significantly higher than in the placebo group [2–6]. They correspond to indicators with more frequent or prolonged use of the drug, as well as the results of treatment with terbinafine in other dosage forms.
Relapses after treatment regimen 1 time per day for one week
Two studies were conducted in which patients with athlete's foot received Lamisil® cream in this regimen or for 1-5 days. The rate of relapse or reinfection at 8 and 12 weeks was 3% (3 out of 98 people) [7]. In two other studies of 63 patients with tinea glabrous/tinea groin, the rate of relapse or reinfection was 3.2% (2 patients). In these cases, it is more correct to talk about reinfections rather than relapses.
With other treatment regimens, the rate of relapse/reinfection was 2/46 8 weeks after treatment twice daily for 4 weeks and 5/42 12 weeks after treatment for one week also twice daily. Thus, a treatment regimen of once a day for one week is quite adequate for the effective treatment of athlete's foot or ringworm of smooth skin/tinea groin [8].
In general, a treatment regimen with the application of Lamisil® cream once a day for one week is as effective as regimens with more frequent or longer use of the drug.
The effectiveness and safety of Lamisil® cream in adults is well documented, as evidenced by its registration in almost 100 countries, in a third of which it has over-the-counter status. The drug has been studied to a lesser extent in children.
Lamisil® cream was evaluated in 12 clinical studies in children under 15 years of age with athlete's foot, ringworm of the smooth skin/tinea groin, scalp, cutaneous candidiasis, and external auditory canal. The smallest age is 2 years. A total of 223 patients were assessed. The drug was shown to be effective and well tolerated in most cases. Thus, in one study of 97 children, adverse events occurred in only 5 people, were mild and quickly disappeared after discontinuation of the drug. No differences were found in comparison with adult patients [11–14].
A total of 19 studies were conducted comparing with other drugs (clotrimazole, econazole, ketoconazole and bifonazole), which included a total of 2095 patients, with 1054 receiving Lamisil cream. 33 adverse events (3.13%) were recorded. Their frequency turned out to be very low. With the exception of one case of eye irritation and one case of metallic taste in the mouth, all other manifestations were limited to the application site and included itching, dryness, irritation and a burning sensation. When comparing the results of treatment with terbinafine and other drugs, the nature and frequency of adverse events were practically no different. Thus, the safety of terbinafine does not differ from the safety of various other topical drugs used in various countries for the treatment of fungal infections [16].
In some studies, the cream was used for more than one week, sometimes up to four weeks [15, 17]. However, this was not accompanied by an increase in the incidence of side effects. Therefore, in cases where patients themselves use the cream beyond the recommended period, there is no danger of an increase in adverse events.
Thus, Lamisil® cream is a widely known antifungal agent with fungicidal activity and proven effectiveness. Its safety has been studied both in clinical studies and as a result of long-term post-marketing surveillance.
Of course, the clinical effectiveness and safety in the treatment of dermatomycosis of smooth skin, groin and feet, cutaneous candidiasis and lichen versicolor exceeds the minimal risk of side effects.
Literature
- Alexander BD, Perfect JR Antifungal resistance trends towards the year 2000, Implications for therapy and new approaches // Drugs. 1997; 54:657–678.
- Balfour JA, Faulds D. Terbinafine. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic potential in superficial mycoses // Drugs. 1992; 43(2):259–284.
- Evans EGV The clinical efficacy of terbinafine in the treatment of fungal infections of the skin // Rev Contemp Pharmacother. 1997; 8:325–341.
- Favre B., Leidich SD, Ghannoum MA, Ryder NS Biochemical mechanism of resistance to terbinafine in clinical isolates of the dermatophyte Trichophyton rubrum (abstract). 41st Interscience Conference on Antimicrob Agents and Chemother, Chicago, American Society for Microbiology, Washington DC, 2001.
- Hofbauer B., Leitner I., Ryder NS In vitro susceptibility of Microsporum canis and other dermatophyte isolates from veterinary infections during therapy with terbinafine or griseofulvin // Med Mycol. 2002; 40:1–5.
- Jungnickel PW, Hunnicutt DM Alcohol Abuse. In: Young LY, Koda-Kimble MA (eds). Applied Therapeutics - The Clinical Use of Drugs (6th Edition). Applied Therapeutic Inc Vancouver, 1995, p. 82–91.
- Leidich SD, Isham N., Leitner I., Ryder NS, Ghannoum MA Primary resistance to terbinafine in a clinical isolate of the dermatophyte Trichophyton rubrum (abstract). 41st Interscience Conference on Antimicrob Agents and Chemother, Chicago, American Society for Microbiology, Washington DC, 2001.
- Osborne CS, Favre B. Identification of Amino Acid Substitution(s) in the Squalene Epoxidase Sequence from Trichophyton rubrum Isolates Resistant to Terbinafine (abstract). 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, American Society for Microbiology, Washington DC, 2002.
- Osborne CS, Favre B, Ryder NS Investigation of Terbinafine Resistance Frequency and Development in Trichophyton rubrum [abstract]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, American Society for Microbiology, Washington DC, 2002.
- Reed BR Dermatologic drugs, Pregnancy and Lactation // Arch Dermatol. 1997; 133:894–98.
- Rex JH, Rinaldi MG, Pfaller MA Resistance of Candida species to fluconazole // Antimicrob Agents Chemother. 1995; 39:1–8.
- Ryder NS, Favre B. Antifungal activity and mechanism of action of terbinafine // Rev Contemp Pharmacother. 1997; 8:275–287.
- Ryder NS, Leitner I. In vitro activity of terbinafine (Lamisil): an update // Journal of Dermatological Treatment. 1998; 9 (Suppl), 23 S-28 S.
- Suhonen R., Neuvonen PJ The tolerability profile of terbinafine // Rev Comtemp Pharmacother. 1997; 8:373–386.
- Waller P., Coulson RA, Wood S. Regulatory pharmacovigilance in the United Kingdom: Current principles and practice // Pharmacoepidemiology and Drug Safety. 1996; 5:363–375.
- Watson A., Marley J., Ellis D. et al. Terbinafine in onychomycosis of the toenail: A novel treatment protocol // J Am Acad Dermatol. 1995; 33: 775–779.
- White TC, Marr KA, Bowden RA Clinical, cellular and molecular factors that contribute to antifungal drug resistance // Clin Microbiol Rev. 1998; 11 (2): 382–402.
Dr. Thomas Jones
Antwerp Hospital, Belgium
Contact information about the author for correspondence
Comparative pharmacoeconomic assessment of the use of antimycotics of the terbinafine group
It is known that most of the drugs sold in the Russian Federation are not original drugs, but their generic analogues. An increase in the share of generic drugs is a clear trend in the development of pharmaceutical markets in all developed countries. This area is supported by WHO within the framework of the Essential Medicines program. After the expiration of the patent, any pharmaceutical company can acquire the right to produce its own version of the original drug - a reproduced drug, or generic (from the English generic - general, group, generic). The advantage of generics is their relatively low cost, which is explained by the fact that the creation and registration of a generic does not require the same costs as the creation and testing of the original product. First of all, long-term clinical trials are not conducted, and the similarity of the properties and therapeutic effects of generic and original drugs is determined in pharmaceutical and biological equivalence studies.
Preparations are equivalent from a pharmaceutical point of view if they contain the same amount of active substance and comply with current international production standards, as determined by special pharmacopoeial tests. The requirements for the production of generics and original drugs are the same and comply with the rules of Good Manufacturing Practice (GMP). Bioequivalence (pharmacokinetic equivalence) is defined as the identity of two pharmaceutically equivalent drugs according to the main pharmacokinetic parameters (the degree and rate of absorption of the drug, the time to reach and the value of maximum concentration in the blood, the nature of distribution in tissues and body fluids, the type and rate of excretion) in studies involving healthy volunteers. An important feature of real clinical practice is the differences in the preferences of doctors when prescribing medications and patients when purchasing specific drugs in the pharmacy chain. Thus, some doctors, guided by “concern” for the patient’s financial well-being, prescribe cheap drugs that often do not comply with GCP and GMP standards, while others are inclined to use expensive original drugs, which often do not have real clinical advantages over cheaper generics . A scientifically based, rather than intuitive or empirical, choice of drug is required, which is possible by conducting clinical and economic studies based on the foundations of evidence-based medicine and the results of comparative clinical trials. The results obtained will make it possible to assess the real significance for practice of the drugs being studied, as well as to determine the cost of additional benefits that certain drugs have.
Due to the significant increase in the incidence of mycotic infections caused by dermatophytes, adequate selection of antifungal agents for empirical therapy is becoming increasingly important. The appearance on the domestic market of a number of antimycotics of the terbinafine group expands the choice of options for practitioners.
Considering the socio-economic situation in the country, the assessment of the minimum cost of treatment and the cost/effectiveness ratio are of particular importance. Rational use of antimycotic therapy from the standpoint of both clinical and economic efficiency can lead to significant cost savings, which is especially important when domestic healthcare resources are limited.
The purpose of this study is to conduct a comparative pharmacoeconomic analysis of the use of antimycotics of the terbinafine group, available on the domestic drug market, in various clinical situations: 1) in patients with onychomycosis of the hands and feet, 2) in patients with mycosis of smooth skin, and 3) in patients with trichomycosis.
For comparison, we selected the main drugs of this group available on the pharmacy market: Lamisil, Terbizil, Binafin, Exifin, Fungoterbin, Terbinox.
Pharmacoeconomic analysis was carried out in 2 stages:
- Development of a treatment model in accordance with industry standards.
- Estimating the cost of treating the disease.
When calculating the cost of treatment, we took into account the following characteristics:
- Cost of the drug.
- Cost of treatment.
Data on the cost of medicines and medical products, the website “Medicines in Moscow Pharmacies”. All cost indicators are presented in rubles.
To estimate the cost of therapy for onychomycosis, we considered two- and three-month courses of taking the drug at a daily dose of 250 mg.
The results of the study are presented in table. 1.
As can be seen from the table, the most expensive course of treatment is Lamisil, and the most affordable are courses conducted by Terbinox and Binafin.
To estimate the cost of therapy for microsporia and trichophytosis, we considered six- and five-week courses of therapy of 250 mg of the drug per day.
The results are presented in table. 2.
For the treatment of microsporia and trichophytosis, the most affordable course was Binafin and Terbinox. The most expensive course was Lamisil.
The evaluation of ointment forms of terbinafine encountered some difficulties, since various drugs are packaged in tubes of 10 g and 15 g. For ease of calculation, we estimated the cost of 15 g of the drug. The results are presented in table. 3.
The most expensive cream is Lamisil, the most affordable is Terbinox.
The data obtained indicate that therapy with the original drug Lamisil is the most expensive, while generic tablets Terbinox and Binafin, as well as Terbinox cream, significantly save the patient’s money.
Terbinafine cream for external use, 1% tube 30 g (Vertex)
Registration Certificate Holder
VERTEX (Russia)
Dosage form
Medicine - Terbinafine
Description
Cream for external use 1%
white, homogeneous, with a weak characteristic odor.
1 g
terbinafine hydrochloride 10 mg
Excipients
: benzyl alcohol, polysorbate 60 (Tween 60), sorbitan monostearate, cetyl alcohol, isopropyl myristate, cetyl palmitate, sodium hydroxide, purified water.
15 g - aluminum tubes (1) - cardboard packs. 30 g - aluminum tubes (1) - cardboard packs.
Indications
- prevention and treatment of fungus, fungal infections of the skin, including mycoses of the feet (“fungus” of the foot), inguinal athlete’s foot (tinea cruris), fungal infections of the smooth skin of the body (tinea corporis), caused by dermatophytes such as Trichophyton (incl. T. rubrum, T. mentagrophytes, T. verrucosum, T. violaceum), Microsporum canis and Epidermophyton floccosum;
- yeast infections of the skin, mainly those caused by the genus Candida (for example, Candida albicans), in particular diaper rash;
- Versicolor versicolor (Pityriasis versicolor), caused by Pityrosporum orbiculare (also known as Malassezia furfur).
Contraindications for use
- hypersensitivity to terbinafine or to any of the inactive ingredients included in the drug. With caution
: liver and/or renal failure, alcoholism, suppression of bone marrow hematopoiesis, tumors, metabolic diseases, occlusive vascular diseases of the extremities, children under 12 years of age (lack of sufficient clinical experience).
pharmachologic effect
An antifungal drug for topical use with a wide spectrum of antifungal activity. Even in small concentrations, terbinafine has a fungicidal effect against dermatophytes (Trychophyton rubrum, T.mentagrophytes, T.verrucosum, T.violaceum, T.tonsurans, Microsporum canis, Epidermophyton floccosum), molds (mainly C.albicans) and certain dimorphic fungi (Pityrosporum orbiculare). Activity against yeast fungi, depending on their type, can be fungicidal or fungistatic.
Terbinafine specifically alters the early stage of sterol biosynthesis occurring in fungi. This leads to ergosterol deficiency and intracellular accumulation of squalene, which causes the death of the fungal cell. Terbinafine acts by inhibiting the enzyme squalene epoxidase located on the cell membrane of the fungus.
Terbinafine does not affect the cytochrome P450 system in humans and, accordingly, the metabolism of hormones or other drugs.
Drug interactions
There are no known drug interactions for Terbinafine Cream.
Dosage regimen
Externally.
Adults and children from 12 years old
Before applying the cream, it is necessary to clean and dry the affected areas. The cream is applied once or twice a day in a thin layer to the affected skin and surrounding areas and rubbed in lightly. For infections accompanied by diaper rash (under the mammary glands, in the spaces between the fingers, between the buttocks, in the groin area), the places where the cream is applied can be covered with gauze, especially at night. For extensive fungal infections of the body, it is recommended to use the cream in 30 g tubes. Average duration of treatment:
dermatomycosis of the trunk, legs - 1 week, 1 time per day; dermatomycosis of the feet - 1 week, 1 time per day; skin candidiasis - 1-2 weeks 1 or 2 times a day; tinea versicolor: 2 weeks 1 or 2 times a day.
A decrease in the severity of clinical manifestations is usually observed in the first days of treatment. If treatment is not regular or is stopped prematurely, there is a risk of the infection returning. If after one to two weeks of treatment there are no signs of improvement, the diagnosis should be verified.
The dosage regimen for the drug in
elderly people
does not differ from that described above.
The use of this drug in children under 12 years of age
.
Overdose
No cases of drug overdose have been reported. If terbinafine cream is accidentally taken orally, you can expect the same side effects as with an overdose of tablets (headache, nausea, epigastric pain and dizziness).
Treatment:
activated carbon, if necessary - symptomatic maintenance therapy.
Side effect
Redness, itching or burning sensation may appear at the sites where the drug is applied. Allergic reactions.
special instructions
A decrease in the severity of clinical manifestations is usually observed in the first days of treatment. In case of irregular treatment or its premature termination, there is a risk of recurrence of infection.
Terbinafine cream is for external use only. Avoid contact with eyes as it may cause irritation. If the drug accidentally gets into your eyes, they should be immediately rinsed with running water, and if persistent irritation develops, you should consult a doctor.
If allergic reactions develop, the drug must be discontinued.
Storage conditions
In a dry place, protected from light, out of reach of children, at a temperature not exceeding 25°C.
Use during pregnancy and breastfeeding
Restrictions during pregnancy - With caution. Restrictions when breastfeeding - With caution.
In experimental studies
No teratogenic properties of terbinafine were identified.
To date, no malformations have been reported with the use of Terbinafine. However, since clinical experience with the use of Terbinafine in pregnant women is very limited, it should be used only when strictly indicated. Terbinafine is excreted in breast milk.
However, if a nursing mother uses Terbinafine cream, a small amount of the active substance is absorbed through the skin, so adverse effects on the baby are unlikely. Use in elderly patients
Restrictions for elderly patients - No restrictions. Dosage regimen for the elderly
no different from the above.
Use in children
Restrictions for children - Contraindicated. Use of this drug in children under 12 years of age
.
Terms of sale
The drug is approved for use as a means of OTC.
Contacts for inquiries
VERTEX JSC (Russia)
199106 St. Petersburg Vasilyevsky Island, 24-liniya, no. 27, lit. A Tel/fax