- home
- general surgery
- Adrenal tumor
- Pheochromocytoma - hormonally active adrenal tumor
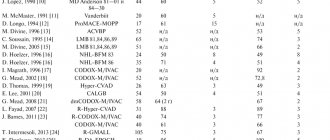
Pheochromocytoma accounts for about 5-7% of adrenal tumors. At the present stage of development of diagnostic methods, at least 50% of pheochromocytomas are initially detected as incidentalomas (accidentally detected), and only about half of these observations are accompanied by arterial hypertension. Despite certain advances in the interpretation of the radiological semiotics of pheochromocytoma, laboratory tests are fundamental in confirming the diagnosis.
Malignant pheochromocytomas (pheochromoblastomas) are often found. This group of pheochromocytomas also includes catecholamine-producing tumors with distant metastases. They are usually fused with surrounding organs. The tumor on the section is variegated due to the alternation of dark red areas and grayish fields of necrosis; the capsule is sharply worn out in places or even absent.
1.General information
In order not to overload the text with complex terminology from the very beginning, let’s try to figure it out in order. The title ends in "-oma", so it's definitely about a tumor.
Chromaffin cells (literally “related to chromium”) are a type of endocrine cells. Consequently, they are capable and obligated to produce hormones at the command of the nervous system, i.e. biochemical regulators of physiological and mental processes in the body.
The synonymous names for these cells are pheochromocytes; from here the “origin” of the tumor to which this article is devoted becomes clear. By the way, the prefix “feo-” indicates a dark color. Dissected chromocytes are stained with chromic acid salts and are visualized under a microscope as yellow-brown.
These cells produce catecholamines (“fear and battle hormones”), i.e. adrenaline, norepinephrine and dopamine. The history of scientific research into tumors developing from such tissue dates back to the 80s of the nineteenth century. Today, medicine knows a lot about pheochromocytoma, but not everything: a number of key points need further study.
It is known, in particular, that pheochromocytes are found in a variety of structures and systems of the body, but their greatest concentration is in the adrenal medulla.
Accordingly, pheochromocytoma in the vast majority of cases (approx. 90%) is found there. It is also known that this tumor is quite rare: statistical estimates vary slightly around the frequency of 1:200,000 (it should be noted that some sources consider this estimate to be underestimated), and the frequency of new confirmed cases of the disease is approximately 1 case per one and a half to two million people in the world. year. It has finally been established that pheochromocytoma is a classic hormone-producing tumor, i.e. its growth and activity cause increased levels of associated hormones.
Considering which hormones are secreted in chromaffin cells, it is not difficult to understand the patterns of the clinical picture of the disease.
A must read! Help with treatment and hospitalization!
Classification
The formation of the adrenal glands is distinguished, i.e. pheochromocytoma itself. In addition to the adrenal glands, a small number of chromaffin cells in the form of small clusters can be found in the heart, head, neck, bladder, and along the spine. Tumors in these cells are called paragangliomas. They have a similar effect on the body as pheochromocytomas, as the same hormones are released.
Classification of pheochromocytoma according to ICD-10
The disease is placed in section D35.0 - “Benign neoplasm of other and unspecified endocrine glands.”
2. Reasons
The etiopathogenetic mechanism of the triggering and development of pheochromocytoma is one of those moments that modern science cannot yet explain reliably and unambiguously. Diseases of this kind are usually called sporadic: in their rare occurrences, it is impossible to trace any logic and system, a statistically stable and repeated influence of any factors. Attempts to prove the hereditary nature have not yet been crowned with convincing success, although it has long been known that pheochromocytoma is one of a number of purely genetic syndromes (Sipple, Hippel-Lindau, etc.) - but precisely as one of many manifestations of a more general anomaly, and not as an axial, syndrome-forming one phenomenon. In general, one or another connection with heredity is found in no more than every tenth case.
Visit our Oncology page
Pathogenesis
The clinical symptoms of pheochromocytoma are associated with the effect on the body of catecholamines excessively produced by the tumor. In addition to catecholamines (norepinephrine, adrenaline, dopamine), pheochromocytoma can secrete ACTH, calcitonin, serotonin, somatostatin, vasoactive intestinal polypeptide, the strongest vasoconstrictor - neuropeptide Y and other active substances that cause diverse effects.
Pheochromocytoma is an encapsulated tumor with good vascularization, about 5 cm in size and an average weight of up to 70 g. Pheochromocytomas are found in both large and smaller sizes; Moreover, the degree of hormonal activity does not depend on the size of the tumor.
3. Symptoms and diagnosis
Pheochromocytoma can be either malignant (in which case it is called pheochromoblastoma) or benign. Malignant ones are several times less common (and, as a rule, are localized outside the adrenal glands), but there is also no consensus in this regard. The fact is that pheochromocytoma more often meets some criteria for malignancy, but almost never meets others. Thus, more than 60% of such tumors grow due to atypical cells and become overgrown with their own vascular network of blood supply, but no more than 5% of pheochromocytomas metastasize and grow into adjacent structures.
Returning to the main clinical picture, it should be noted that most often the hormonal activity of pheochromocytoma manifests itself in crisis attacks: very high blood pressure (up to 300 mm Hg or more) is accompanied by a feeling of fear, tachycardia, pallor, nausea and/or vomiting, frequent and profuse urination, increased body temperature, increased heart rate, hyperhidrosis (forced sweating) and severe headache. The combination of the last three symptoms forms the so-called. Carney's triad and is observed in almost all patients with crisis-type pheochromocytoma. With a smoother type of course, blood pressure is increased almost constantly; with mixed forms, persistent hypertension alternates with even more dangerous crises; the most aggressive form of pheochromocytoma symptoms can result in life-threatening catecholamine shock.
Equally serious are other possible complications associated with hypersecretion of catecholamines and severe persistent arterial hypertension: various types of heart failure, stroke (acute cerebrovascular accidents, strokes), pathology of the gastrointestinal tract, kidneys, blood vessels, etc. The most dramatic outcome is sudden death from vascular collapse; This was precisely the first described clinical case associated with a bilateral adrenal tumor.
Diagnosis is extremely difficult, firstly, by the rarity of the pathology (in a doctor’s practice, pheochromocytoma may occur only once in a lifetime or not at all), and secondly, by the absence of pathognomonic or at least highly specific symptoms. Often, identifying the true cause of hypertension takes a lot of time and requires consistent exclusion of a number of symptomatically similar diseases. It is not for nothing that this tumor is called the “great imitator” - from one to two thirds of correct diagnoses are postmortem.
Adequate intravital diagnosis is based on anamnestic and clinical data, monitoring of blood pressure dynamics, laboratory tests of hormone levels in the blood, as well as imaging methods (ultrasound and tomography), which make it possible to clarify the size and localization of pheochromocytoma.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnosis of pheochromocytoma.
Fractionated determination of metanephrines (that is, separate determination of metanephrine and normetanephrine, if indicated - methoxytyramine) in urine or plasma has the greatest diagnostic sensitivity in relation to the initial (i.e., truly tumor) amount of catecholamines. This test is recommended as a first-line diagnostic test. The sensitivity of the method for determining methylated catecholamine derivatives in urine is 99%, the specificity is 91. Plasma methylated catecholamines have a sensitivity of almost 99%, and a specificity of 85% - 89%.
Reference values for plasma and urinary fractionated metanephrines should primarily ensure optimal diagnostic sensitivity. The specificity of this test is assessed secondarily. This is due to the potential consequences of a missed diagnosis.
A decrease in specificity significantly increases the number of false-positive results; therefore, serious treatment decisions should be based on the degree to which the upper limit of reference values is exceeded. A slight excess of the upper limit of both plasma and urinary fractionated metanephrines is associated with a slight likelihood of pheochromocytoma, while a fourfold excess is associated with an almost 100% likelihood of this type of tumor.
If the results of hormonal studies are questionable, scintigraphy with MIBG-I123, determination of chromogranin A and/or a test with clonidine are used to increase the specificity of the test and verify the diagnosis of pheochromocytoma. With adrenal tumors with low native density of the tissue component (less than 10 H units), the likelihood of pheochromocytoma is extremely low, which can be used as a differential method in the “gray” zone of the level of fractionated metanephrines.
It should be noted that the study of fractionated metanephrines for the diagnosis of pheochromocytoma is a primary task that precedes the assessment of the malignant potential of the tumor.
4.Treatment
The method of choice is adrenalectomy - unilateral or total surgical removal of the adrenal glands (in the latter case, lifelong hormone replacement therapy will be required). Organ-preserving intervention is also practiced, but the risk of relapse is unreasonably high. Minimally invasive (endoscopic, without open cavity intervention) removal methods require further technical development. If there are contraindications, radiation therapy may be prescribed.
Conservative treatment, the essence of which is to inhibit the secretion of catecholamines by the tumor, is much less effective.
The prognosis depends on a number of clinical, morphological and individual factors. Thus, with timely surgical intervention for benign pheochromocytoma, the five-year survival rate (the main indicator for oncology) approaches 100% with a low percentage of relapses, but with a malignant course it does not reach even half (the remaining cases of pheochromoblastoma are characterized by sluggish progression and approximately 20-year survival).
Forecast
With timely and high-quality treatment, hypertension in most cases goes away without a trace. Sometimes it remains, but becomes less aggressive and responds better to conventional medications. In 10% of cases, relapses are possible due to the fact that the tumor can be located in other places besides the adrenal glands. This requires additional treatment and possibly surgery.
Pheochromocytoma is a fairly serious disease. Find out more on our clinic’s website Dobrodut.com. Our specialists categorically do not recommend self-medication. Contact a good endocrinologist who can correctly prescribe treatment and resolve the issue of surgical removal of the tumor.
Related services: Surgical operations Laparoscopy
Complications
The most severe complication of the clinical course of pheochromocytoma is catecholamine shock, manifested by uncontrolled hemodynamics - a chaotic change of episodes of hyper- and hypotension that cannot be corrected. In pregnant women, pheochromocytoma disguises itself as toxicosis of pregnancy, preeclampsia and eclampsia and often leads to an unfavorable outcome of childbirth.
The stable form of pheochromocytoma is characterized by persistently high blood pressure with the gradual development of changes in the kidneys, myocardium and fundus, mood variability, increased excitability, fatigue, and headaches. Metabolic disorders (hyperglycemia) lead to the development of diabetes mellitus in 10% of patients. Diseases that often accompany pheochromocytoma are cholelithiasis, Recklinghausen's disease (neurofibromatosis), Cushing's syndrome, Raynaud's syndrome, etc.