The disease is treated by: Pediatric gastroenterologist
- Gastritis in a child: symptoms and treatment
- Causes of the disease
- Diagnosis of acute and chronic forms of the disease in children
- Features of acute gastritis
- Features of the chronic form of the disease
- How to treat gastritis in children?
- Diet features
Gastritis is a disease characterized by various inflammations of the gastric mucosa. Each type of disease has its own symptoms, therefore, knowing them, you can even externally determine the type of gastritis - chronic or acute.
Gastritis in a child: symptoms and treatment
Common symptoms include:
- heaviness and discomfort in the stomach, combined with or without pain;
- pain in the upper abdomen, which can be mild or very severe - this parameter depends on the child’s pain threshold and the intensity of inflammation;
- decreased appetite or complete refusal to eat;
- heartburn, which worsens with exercise and bending over and can spread through the esophagus;
- belching of food or air, which may be accompanied by an unpleasant odor;
- bloating, constipation, hypovitaminosis and other digestive disorders;
- nausea;
- vomit;
- pain when palpating the stomach area;
- pale skin, white or gray coating on the tongue (indirect signs).
Signs of chronic atrophic gastritis in children:
- heaviness in the stomach;
- digestive dysfunction;
- anemia;
- deficiency of vitamins in the body.
Symptoms of acute gastritis in children:
- vomiting (if it lasts for a very long time, lethargy occurs);
- constant pain;
- poor general health.
Hyperacid chronic gastritis manifests itself:
- pain;
- sour belching;
- heartburn;
- pain in the stomach;
- stomach upsets.
Development mechanisms
Causes of acute gastritis in children:
- Foodborne illness (a gastrointestinal disease that occurs after eating food containing bacteria and their toxins. Often occurs due to the consumption of rotten foods, unwashed fruits or dirty water);
- Long-term use of certain medications (salicylates, sulfonamides, glucocorticoids, digitalis preparations, etc.);
- Poisoning with household poisons;
- Allergy.
When a large number of bacteria enter the gastrointestinal tract, inflammation occurs. Excess fatty, spicy and poorly chewed food slows down the evacuation (removal) of stomach contents and worsens the secretory function of the organ (the secretion of digestive juice for digesting food). The food lump lingers in the stomach, it is saturated with enzymes, after which it disintegrates due to the action of bacteria, and the fermentation process begins.
Which leads to aggravation of the course and chronicity of the process.
Causes of chronic gastritis in children:
- The presence of the bacterial flora Helicobacter pylori (the same bacterium leads to ulcers). In 80-85% of cases it is what causes gastritis;
- Poor nutrition (eating rough, too hot or cold, fatty, spicy or poorly chewed food);
- Dry food;
- Eating 1-2 times a day or less often;
- Lack of vitamins, complete proteins and fats in the diet;
- Endocrine diseases;
- Kidney damage;
- Diseases of the cardiovascular system;
- Long-term use of medications (salicylates, sulfonamides);
- The source of infection in the oral cavity (disease of teeth and gums);
- Burdened heredity;
- Allergies.
The factors that cause acute and chronic gastritis are similar or even coincide. The main difference is the duration of their effect on the body. In acute gastritis, one contact with an irritant (expired cottage cheese or a large portion of fast food) is enough for an attack. In chronic gastritis, an irritating factor acts on the gastric mucosa for a long time and repeatedly, gradually leading to a decrease in the activity of the digestive glands.
Causes of the disease
Most often , gastritis of any form occurs in schoolchildren . The age from 6 to 17 years is a period of active development and growth, which creates favorable factors for damage to the body. Reasons include:
- unhealthy diet (chips, fast food, carbonated drinks, fatty and spicy foods, smoked foods). This is the most common cause of gastritis;
- eating spoiled food containing harmful microorganisms;
- lack of system in eating - irregular meals with long intervals and excessively large portions;
- excessive physical activity;
- lack of physical activity;
- psycho-mental excessive stress at school, lack of rest, leading to impaired production of gastric juice, poor appetite;
- damage by infections and/or toxins;
- general allergic reactions.
What kind of disease is this and why does it occur?
Despite the fact that our stomach is a “tough nut” that can withstand hydrochloric acid, certain types of food, drinks and medications can greatly impair its health. If a person regularly eats spicy food or drinks a lot of alcohol, then damage and inflammation form on the mucous membrane of the organ, which is called gastritis.
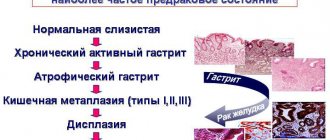
The disease has different forms, which differ in their origin and symptoms. Some types are easy to treat without leading to dire consequences, while others provoke the development of polyps and malignant tumors in the stomach. However, this can be avoided if you contact a competent specialist in time and start treatment.
If we talk about children, there can be several causes of gastritis:
- unhealthy diet - fast food, chips, sweet carbonated water, fatty foods;
- severe stress while studying;
- excessive physical activity;
- sedentary lifestyle;
- allergy;
- entry of the virus into the body;
- bacterium Helicobacter pylori.
Diagnosis of acute and chronic forms of the disease in children
The reason for the need for examination is the child’s complaints and external manifestations of the disease. The diagnosis can be confirmed or refuted by fibrogastroduodenoscopy. It is important to remember that the symptoms of gastritis are similar to other diseases that can be more dangerous.
During an examination using endoscopic technology, the doctor examines the gastric mucosa. Based on this, a conclusion is made about the child’s condition and treatment is prescribed. Source: L. N. Tsvetkova [et al.] Gastroenterological pathology in children: pathomorphosis of diseases and improvement of diagnostic methods at the present stage // Materials of the XVIII Congress of Pediatric Gastroenterologists, 2011, p. 5-8
This study presents challenges with young children. Therefore, fibrogastroduodenoscopy is not indicated for everyone. Children most often undergo general preventive treatment, based on the effectiveness of which a conclusion is made about the presence of the disease. If the symptoms do not go away during treatment, an endoscopic examination is performed, as there are direct indications for it - the possible presence of a more serious illness.
To exclude other digestive diseases, an ultrasound is also prescribed.
To determine the degree of gastritis and the presence of complications, laboratory diagnostics are performed:
- clinical blood test;
- general urine analysis;
- identifying the level of diastase;
- liver tests;
- fecal analysis for helminths.
Treatment of gastritis
Gastritis is a gastrointestinal disease, the key aspect of treatment of which remains diet.
The child should eat often, but in fractional portions. Fried, fatty foods, smoked foods, spicy seasonings, and marinades are temporarily excluded. All food must be boiled or steamed. It is recommended to feed the child pureed foods to minimize mechanical irritation of the gastric mucosa. Medication correction of the baby’s well-being is achieved using the following groups of drugs:
- proton pump inhibitors (Pantoprazole, Omeprazole), which reduce acidity;
- enveloping drugs - Almagel, Gaviscon;
- antibiotics (Metronidazole, Clarithromycin) are used to identify H. Pylori or other pathogenic bacteria.
In case of serious complications (bleeding, perforation, etc.), surgical intervention may be required.
Prevention of gastritis of any etiology involves eating well-heat-treated food in fractional portions. It is recommended not to abuse fast food. But the main thing is regular, nutritious meals. Gastritis is often also called “students’ disease” due to constant dry snacks. “SM-Doctor” is an advanced medical center that provides a full package of diagnostic and therapeutic services to patients with various forms of gastritis. The sooner the child begins to receive adequate treatment, the faster he will recover.
Features of acute gastritis
Inflammation of the mucous membrane appears due to negative external factors: poor nutrition, infections, consumption of expired products. Children can swallow substances containing toxins and poisons: household chemicals, drugs for adults, etc. They provoke irritation or burns of the mucous membrane, as a result, acute inflammation occurs.
Depending on the degree of damage to the mucous membrane, gastritis has varying degrees of severity and symptoms:
- with superficial inflammation, one-time vomiting and stomach pain occur;
- with deep inflammation, prolonged vomiting and stomach pain appear;
- when superficial erosions form due to inflammation, severe pain, prolonged vomiting, and general weakness appear;
- deep destruction and inflammation provoke similar, but very severe symptoms with dehydration against the background of incessant vomiting.
The first degree of the disease does not pose a threat and goes away without a trace with proper treatment. The second to fourth require specialized help because they can provoke gastric bleeding, dehydration, and intoxication.
Chronic gastritis
According to the causes of chronic gastritis, there are:
- Primary (exogenous). As an independent disease.
- Secondary (endogenous). As one of the manifestations of other somatic pathologies.
By localization:
- Focal (fundal). When it affects the bottom of the stomach;
- Common. Affects several sections, most or all of the stomach (pangastritis);
- Combined (gastroduodenitis). It causes inflammation of the stomach and duodenum.
With the flow:
- Latent (hidden, asymptomatic);
- Monotonous (symptoms are always present);
- Recurrent (alternate periods of exacerbations and remissions).
By stages (phases) of the process:
- Exacerbation (severe symptoms);
- Incomplete clinical remission (unexpressed symptoms, inflammation of the stomach is visible during FGDS);
- Clinical remission (there are no symptoms, but during FGDS inflammation of the mucous membrane is detected);
- Clinical and endoscopic remission (no symptoms, no traces of inflammation during instrumental examination).
According to changes in the mucous membrane:
- Superficial (without atrophy);
- Hypertrophic (with the growth of the mucous membrane, the formation of cysts and polyps);
- Hemorrhagic (tendency to bleeding from the walls of the stomach);
- Erosive (with the formation of stomach ulcers);
- Subatrophic (slow small-focal atrophy);
- Atrophic;
- Mixed.
Features of the chronic form of the disease
This type of disease lasts a long time , the symptoms are mild, and exacerbations occur periodically. It occurs due to disturbances in the activity and properties of the gastric mucosa: a lot of gastric juice is produced, which subsequently stagnates. As a result, the mucous membrane digests itself, and irritation occurs.
Rarely in children there is a form in which the cells of the mucous membrane are destroyed, the function of producing gastric juice, on the contrary, is reduced.
About the disease
Gastritis is one of the most common diseases of the gastrointestinal tract (GIT), which occurs more often in children, starting from school age.
The disease is characterized by the formation of a focus of inflammation in the gastric mucosa. This is how characteristic clinical symptoms appear, which can be provoked by both external and internal causes. The pathology can be acute or chronic. The danger of the disease lies in the disruption of digestive function and the possible development of serious complications that worsen the patient’s quality of life. If left untreated, gastritis progresses from childhood into adulthood.
How to treat gastritis in children?
The treatment methodology depends on the form of gastritis in children: chronic or acute.
Treatment of acute gastritis:
- gastric lavage;
- taking sorbents or gastrocytoprotective drugs;
- taking enzymes;
- taking medications to reduce the production of gastric secretions (if the disease lasts);
- diet;
- taking antispasmodics for severe pain.
Treatment of chronic gastritis:
- in case of excessive production of gastric juice, antisecretory therapy is carried out;
- if Helicobacter pylori is detected, antibacterial drugs are prescribed;
- taking antacids;
- taking antispasmodics for severe pain;
- taking medications to normalize intestinal and gastric motility;
- taking enzymes;
- for atrophy, vitamins and iron supplements are prescribed;
- treatment with mineral waters;
- Spa treatment.
Diagnosis of childhood gastritis
Diagnostics must be comprehensive. The patient's complaints and clinical picture allow a preliminary diagnosis of gastritis to be made. If this disease is suspected, a number of laboratory and instrumental studies are carried out:
- Fibrogastroduodenoscopy is the most informative research method, technically difficult, especially in children. An endoscope is inserted into the stomach cavity - a flexible instrument with fiber optics, with which the mucous membrane is visualized. This makes it possible to fully evaluate its structure. At the same time, a biopsy is performed - taking a sample of stomach tissue for further histological examination.
- Fractional sensing . It is used to study gastric contents, which are aspirated using a special probe. The level of hydrochloric acid secretion is determined, which makes it possible to differentiate between hyperacid and hypoacid gastritis.
- pH-metry is used for the same purpose, but the analysis of secretory activity is carried out directly inside the organ. To do this, a probe with a sensor is inserted, which remains in the stomach for some time. To obtain objective data, a histamine test is used to assess stimulated secretion.
- Ultrasound (ultrasound) is performed to exclude other pathologies (pancreatitis, hepatitis, biliary dyskinesia, etc.).
- A stool test is performed to identify helminthic infestations or occult blood.
- Blood and urine analysis . The blood is examined to rule out anemia and possible bleeding in the child. The main criteria here will be the level of red blood cells and hemoglobin.
Diet features
Proper nutrition is the key to minimizing relapses of gastritis.
- Regular fractional meals in equal portions.
- Only high-quality food, freshly prepared.
- Lack of fatty, spicy, smoked, fried foods containing a lot of spices and additives, raw vegetables, buns, legumes.
- Eating steamed or boiled foods.
- The presence in the menu of cereals, mashed potatoes, chicken, lean meat and fish, weak tea, cocoa with milk, honey, crackers, etc. on the recommendation of a doctor.
Advantages of SM-Clinic
In our medical center you will find some of the best gastroenterologists in the city for the diagnosis and treatment of childhood gastritis of all forms. We will quickly diagnose a child of any age, prescribe effective therapy, and provide the necessary consultations on nutrition and relapse prevention.
You can make an appointment by phone.
Sources:
- E. V. Savitskaya. Features of gastroduodenal pathology in children of preschool and primary school age // Suchasna gastroenterology, 2008, No. 3, p. 35-37.
- Yu.V. Belousov. Chronic atrophic gastritis in children // Clinical Pediatrics, 2011, 5 (32).
- L. N. Tsvetkova [and others]. Gastroenterological pathology in children: pathomorphosis of diseases and improvement of diagnostic methods at the present stage // Materials of the XVIII Congress of Children's Gastroenterologists, 2011, p. 5-8.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a gastroenterologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Ultrasound of the abdominal organs (comprehensive) | 2900 rub. |
| Ultrasound of the retroperitoneal space (and retroperitoneal lymph nodes) | 1400 rub. |
| Ultrasound of the gallbladder | 1400 rub. |
| Ultrasound of the abdominal organs (comprehensive) | 2900 rub. |
| Ultrasound of the liver | 1600 rub. |
| Ultrasound of the spleen | 1600 rub. |
| Diagnosis of Helicobacter pylori infection (HELPIL test) | 1200 rub. |
| Colonoscopy | 5050 rub. |
| Biopsy during endoscopic examination (1 biopsy) | 1000 rub. |
| Body composition assessment - bioimpedance analysis | 2150 rub. |
| Body composition assessment - repeated (bioimpedance analysis) | 1750 rub. |
| Esophagogastroduodenoscopy (EFGDS) | 3050 rub. |