The female hormone estrogen is a substance that determines a woman’s health. There are more than 30 estrogen-like substances, but the most significant are estradiol, estrone and estriol. The mechanism of action of these fractions is to support the reproductive, cardiovascular, nervous systems and musculoskeletal system.
What is the hormone estrogen responsible for?
Estrogen in women is produced from androgen as a result of enzymatic reactions.
The role of estrogens in the functioning of the female body is as follows:
- building a silhouette according to the female type, a special accumulation of fat in the lower part of the body;
- growth of the uterus, tubes, ovaries;
- breast growth in teenagers;
- female-pattern hair growth, pigmentation of nipples and external genitalia;
- uterine tone during ovulation, contractile movements of the tubes to promote sperm;
- regular menstrual cycle, possibility of conception;
- inhibition of the growth of cholesterol plaques, timely removal of “bad” cholesterol (maintaining normal lipid metabolism);
- reducing the risk of osteoporosis;
- maintaining the balance of ferrates and copper in the blood;
- normalization of cognitive abilities - memorization, concentration;
- ensuring an adequate course of pregnancy;
- maintaining healthy nails, hair and skin.
Estrogens, derivatives of progesterone, have a complex effect on a woman’s body. They take part in the work of the heart muscle, support the body’s thermoregulation and the process of calcium absorption. It is under their influence that secondary sexual characteristics are formed in teenage girls - a feminine voice, figure.
Just as estrogen is responsible for femininity, testosterone (a steroid hormone) is responsible for masculinity. If a man has more estrogen than testosterone, he will exhibit feminine characteristics.
ESTROGEN METABOLISM IN WOMEN
(general concepts and clinical practice)
PART II
ESTROGEN METABOLISM IN WOMEN (GENERAL VIEWS AND CLINICAL PRACTICE).
PART 2. TREATMENT OF HYPERESTROGENEMIA
Estrogen dominance is a fairly common disorder of the metabolism of female sex hormones and is manifested by the development of the following diseases in women: endometriosis, endometrial polyps, cervical dysplasia, fibrocystic mastopathy, uterine fibroids, etc. The presence of the listed diseases in the patient indicates a violation of estrogen metabolism, and the degree of metabolic imbalance is beyond the compensatory capabilities of the body. These diseases cannot be tolerated, since aggravation of estrogen metabolism disorders can lead to the development of malignant neoplasms of the uterus and mammary gland. In our opinion, it is undesirable to use synthetic hormones to treat these diseases. This is due to the fact that the metabolism of synthetic hormones mainly occurs through the genotoxic pathway and, in addition, they can block key enzymes that detoxify female sex hormones. Thus, according to research, the metabolites of the synthetic hormones equilin and equivelin are converted in the liver into 4-hydroxy-o-quinone-glutathione conjugates. The saturated beta ring of these hormones switches the synthesis of 2-hydroxy metabolites of female sex hormones to the 4-hydroxy pathway. [1]. In addition, endogenous 4-hydroxyestrone has a weaker effect on inducing DNA damage and apoptosis in breast cancer cell cultures compared to 4-hydroxyequilenine [2]. The influence of metabolites of synthetic hormones on the activity of key detoxification enzymes is evidenced by the following data. Thus, 4-hydroxyequilenine is an irreversible inhibitor of COMT, which catalyzes the methylation of 4-hydroxyestradiol [3]. 4-hydroxy-equilenin, as well as 4,17-hydroxyequilenin. significantly reduces the activity of glutathione-S-transferase literally a few MINUTES after administration into the body [4].
1 CAUSES OF DISEASES
The primary task of the doctor before starting treatment is to try to find the reasons that led to the development of these diseases.
Here is a far from complete list: smoking, taking hormonal drugs, chronic stress, poor-quality and unbalanced nutrition, exposure to toxic substances at work and at home (phthalates, pesticides, heavy metals, etc.), excessive physical activity, insufficient intake of vitamins , minerals, essential fatty acids, antioxidants, associated diseases, in particular diseases of the digestive system, endocrine organs, obesity, etc.
I would like to pay special attention to the constant or periodic use of pharmaceuticals. It turns out that a number of medications have a rather negative effect on the exchange of female sex hormones. So. a drug that is widely used to treat peptic ulcers and diseases associated with high acidity - omeprazole. is a powerful stimulator of cytochrome P-450 1B1, the activation of which leads to the formation of more converging estrogen metabolite - 4-hydroxy-estrone - in a woman’s body. Phenobarbital and other barbitols:. hypoglycemic drugs (troglitaeon, pioglitazone), anti-tuberculosis drugs (rifampicin) strongly activate the work of another enzyme - cytochrome ZA4, which converts estrone into 16-hydroxyestrone. The latter is a very active metabolite of female sex hormones, increased concentrations of which are associated with long-term risk of uterine and breast cancer.
2 TREATMENT. MAIN DIRECTIONS FOR CORRECTION OF ESTROGEN METABOLISM
The main target of treatment in the case of estrogen dominance is the correction of the metabolism of female sex hormones. Such tactics will not only successfully cure the disease, but also eliminate the possibility of relapse of the disease.
1. Stimulation of the preferential (2-hydroxy-) detoxification pathway of female sex hormones
Very often, patients with hyperestrogenemia have low levels of 2-hydroxyestrone, a “good” metabolite of female sex hormones, which indicates a reduced activity of this hormone conversion pathway. To stimulate it, first of all, it is necessary: to halve the number of cigarettes smoked (benzopyrene, a toxin that is formed as a result of smoking, is destroyed along the same path). In the diet, it is necessary to increase the consumption of raw cruciferous vegetables (cabbage, Brussels sprouts, broccoli, watercress, cauliflower), and also prescribe the following drugs: indole-3-carbinol (I3C), soy isoflavones, omega-3 fatty acids.
A. Indole-3-carbinol (I3C)
Indole-3-carbinol (I3C) is a powerful activator of cytochrome P450 1A1, which converts estrogens into 2-hydroxy metabolites. This substance is obtained from cruciferous vegetables and is very unstable. Therefore, high-quality drugs always have a capsule form, to which an antioxidant is added for stabilization, and usually their shelf life does not exceed 1 year from the date of production. The dose of I3C should be 300-450 mg per day. The duration of treatment is at least 3 months and is determined based on repeated laboratory tests. Restoration of normal concentrations of 2-hydroxyestrogens and the ratio of 2-hydroxy- to 16-hydroxyestrogens is grounds for discontinuation of therapy or transfer to a maintenance dose.
Due to the powerful activation of cytochrome P450 1A1 in a woman’s body, the concentration of 2-hydroxyestrogens, the most preferred metabolites in the period before menopause, increases [5].
In addition to stimulating 2-hydroxylation, I3C has many different effects on cells in the body. Thus, I3C was found to stimulate apoptosis of precancerous and cancerous breast cells, and this effect is associated with the fact that I3C blocked the activation of NF-kappa-B caused by transfection of the Akt gene. Thanks to this effect, the authors of the article concluded that I3C has a preventive effect against certain forms of breast cancer [6]. The data obtained are consistent with the results of other studies that showed that I3C induces apoptosis of breast cancer cells independently of the p53 and Bax genes [7]. Similar data were obtained in studies of prostate cancer cells. I3C stimulated apoptosis of these cells by reducing NF-kappa-B activation and inhibited their growth by inhibiting the GT phase of the cell cycle [8]. A study of the effect of I3C on cervical cells showed that it inhibited the anti-apoptotic effect of estradiol on epithelial cells exposed to potential mutagenic substances [9].
A study of the effect of I3C on human colon epithelial cell lines showed that this substance has an anticancer effect due to STIMULATION of apoptosis and enhancing the detoxification capabilities of cells in response to exposure to potential mutagenic substances [10]. These data are consistent with studies showing that I3C reduces the risk of colon cancer and polyps in animal models [11].
The anticancer effect of I3C is not only due to its effect on estrogen metabolism. Thus, it was found that I3C blocks angiogenesis in tumor tissue [12]. influences carcinogenesis due to the binding of free radicals [13]. I3C also increases the activity of glutathione D-transferase and quinone reductase. This leads to a decrease in the concentration of quinones and semiquinones, carcinogenic metabolites of female sex hormones [14]. Induction of detoxification enzymes of the second phase of detoxification, such as glutathione-B-transferase, increases the protection of body cells from compounds that have a mutagenic effect. Thus, it was found that I3C induces the activity of at least 11 different enzymes of the second phase of detoxification [15].
Thus, analyzing the above scientific data, it can be argued that I3C stimulates the 2-hydroxy pathway - the preferred pathway for detoxification of female sex hormones, has a modulating effect on estrogen receptors, stimulates the apoptosis of cancer cells, has antioxidant properties and stimulates enzymes of both the former and the second phase of detoxification in the body.
B. Soy isoflavones
In the case of hyperestrogenemia, we obtained a positive effect from the use of soy isoflavones. There are several mechanisms of their therapeutic action. First of all, soy isoflavones stimulate the 2-hydroxylation of estrogens and thus increase the ratio of 2- to 16-hydroxyestrogens. Some authors consider this effect of soy isoflavones in the context of their anticancer effects [16]. Consumption of soy isoflavones at a dose of 65–132 mg per day reduced the excretion of 4-hydroxyestrone, a potentially carcinogenic estrogen metabolite in menopausal women [17]. Similar data were obtained when studying the effect of soy isoflavones on the metabolism of female sex hormones in the period before menopause [18]. Another beneficial effect of soy isoflavones is their ability to induce the synthesis of sex hormone binding protein in the blood serum. Increasing its concentration reduces the bioavailability of estradiol for estrogen-sensitive tissues [19].
The therapeutic dose of soy isoflavones should be 90-180 mg per day for several months. Discontinuation or transfer to a maintenance dose of 45-90 mg is carried out only after achieving normal levels of estrogens and their metabolites and subject to clinical regression of the diseases.
It should be remembered that soy protein may not be a good source of isoflavones, as they are lost during industrial processing of soybeans.
B. Other factors affecting estrogen metabolism
It turned out that consumption of omega-3 fatty acids stimulates the 2-hydroxylation of estrogens. However, the mechanism of action of omega-3 fats remains unknown.
A study of the level of physical activity in women showed that dosed physical activity increases the ratio of 2- to 16-hydroxyestrogens [20].
2. Inhibition of undesirable (16-hydroxy- and 4-hydroxy-) metabolic pathways of female sex hormones
As mentioned earlier, the 16- and 4-hydroxy pathways of female sex hormone metabolism are less desirable in premenopausal women. Therefore, reducing the activity of enzymes that are involved in the metabolism of estrogens along these pathways is a fairly important therapeutic goal.
A decrease in the activity of cytochrome P450 3A4 will lead to a decrease in the formation of 16-hydroxyestrone, a metabolite that is 8 times more active than estradiol and thus significantly weakens its effect on estrogen receptors. The most powerful inhibitor of cytochrome P450 3A4 activity is naringenin, a flavonoid found in grapefruits. According to some studies, one glass of grapefruit juice reduces the activity of cytochrome P450 3A4 by 30% within 12 hours [21]. Other natural inhibitors of this enzyme activity include licorice root, garlic and St. John's wort.
Reducing the activity of cytochrome P450 1B1 is possible with the help of isoflavones found in the kyuju plant (Pueraria lobata). The most active isoflavone of this plant is puerarin, which has the ability to inhibit the activity of some cytochrome P450s. It was found that it inhibits the activity of cytochromes 3A, 2E1 and 2B1, and therefore can reduce the formation of 4-hydroxyestrogens. In addition, it stimulates the activity of cytochrome 1A2, which causes an increase in the production of 2-hydroxyestrogens [22].
3. Modulation of the function of female sex hormone receptors
A. Soy isoflavones
Soy isoflavones have the ability to modulate estrogen receptors.
In vitro and in vivo studies have shown that estrogens have a weak estrogenic effect, which is approximately 1000 times weaker than the effect of estradiol [23]. Another study showed that isoflavones, by binding to estrogen receptors, can compete with estradiol for the receptor or even block receptor function [24].
B. Indole-3-carbinol (I3C)
It has been shown that a product of I3C metabolism in the body can act as a ligand for estrogen receptors and exhibit tamoxifen-like effects on estrogen-responsive tissues [25].
Other studies have shown that 13C is an antagonist of o-estrogen receptors. In addition, this substance, on the one hand, suppresses the estrogen-sensitive genes pS2 and cathepsin-D, and on the other, increases the activity of the BRCA1 gene, which, in turn, blocks the transcriptional activity of estrogen receptor alpha [26].
B. Naringenin and resveratrol
Naringenin, a flavonoid found in grapefruits, and the antioxidant resveratrol, found in red grapes, influence estrogen signaling through direct and indirect blocking effects on estrogen receptor α [27]. Moreover, the mechanism of action of these nutrients is different [28].
D. Vitamin B6
Pyridoxine (vitamin B6) affects the transmission of signals of steroid hormones, including estrogens. Studies have shown that vitamin B6 interacts with the hormone-receptor complex and reduces its binding to DNA and thus disrupts the transmission of the hormonal signal to cell DNA [29]. Based on this, patients with high estrogen levels should receive fairly high doses of vitamin B6 (30-50 mg per day).
4. Combat oxidative stress
Oxidative stress leads to the formation of semiquinones and quinones - metabolites of female sex hormones that cause irreversible damage to cell DNA. To combat oxidative stress, you need to do two things. First, provide the necessary nutrients to your own antioxidant system. So. Copper and zinc are required for superoxide dismllase. selenium and acetylcysteine - for glutathione peroxidase. vitamin B3 - for glutathione reductase. iron - for catalase. Secondly, prescribe plant antioxidants, such as green tea catechins, lycopene, turmeric, limonene, vitamins C and E, and β-carotene, which can inactivate reactive oxygen species.
5. Maintenance of enzymes of the second phase of detoxification, which take part in the final inactivation of female sex hormones
Treatment measures to maintain the final elimination of female sex hormones should cover 3 main pathways of the second phase of detoxification.
A). An important condition for the normal functioning of methylation processes in the body is the consumption of sufficient amounts of protein. This is due to the fact that the universal donor of methyl groups in the body is s-adenosine-methionine, which, in turn, is formed from the amino acid methionine, consumed mainly with animal protein. Therefore, it is necessary to conduct a comprehensive assessment of a woman’s nutrition and, in case of insufficient protein intake, introduce protein foods into the diet. To accurately assess protein needs, it is better to use special computer programs that allow not only to correctly assess the quality of a woman’s diet, but also to restore the detected imbalance. These programs can be found on the website www.anti-aging.kiev.ua.
In addition to protein, methylation processes require micronutrients, which are cofactors of enzymatic methylation systems.' Therefore, the treatment plan should include the following vitamins and minerals:
- folic acid in a dose of 400-1000 mg per day;
- vitamin B6 in a dose of 10-40 mg per day;
- vitamin B2 in a dose of 15-30 mg per day;
- vitamin B12 at a dose of 250-500 mcg per day;
- magnesium in a dose of 400-800 mg per day.
However, the above therapy may not be effective in all patients. This is due to the fact that approximately 25% of Europeans have a genetic polymorphism in MTHFR, a key enzyme in methylation processes in the body. In these patients, methylation processes can be restored either using the methylated form of folic acid (5-methyl-tetrahydrofolate), or using betaine hydrochloride, which acts as a donor of methyl groups, regardless of 5-methyl-tetrahydrofolate. Thus, if the genetic characteristics of the patient are not known, it is better to prescribe a B vitamin complex containing the methylated form of folic acid and betaine hydrochloride.
B). Conjugation with glutathione is involved in the inactivation of quinones, genotoxic metabolites of female sex hormones. For the normal occurrence of this reaction, N-acetylcysteine is necessary, an amino acid that limits the synthesis of glutathione. It has been shown that the administration of this amino acid leads to a significant increase in the concentration of reduced glutathione in tissues and acceleration of conjugating reactions with glutathione [30]. Silymarin also stimulates endogenous glutathione synthesis [31].
IN). To maintain sulfitation activity, molybdenum and inorganic sulfates should be prescribed.
G). Glucose is required to activate glucuronidation processes. Therefore, absolute insulin deficiency or insulin resistance, which are accompanied by a decrease in glucose concentration inside insulin-dependent cells, are always accompanied to some extent by disturbances in glucuronidation. In addition to carbohydrate metabolism, the activity of glucuronidation processes is actively influenced by triiodothyronine, the most active hormone of the thyroid gland. T3 stimulates the expression of UDP-glucuronosyltransferase genes, and this activation depends on the body’s supply of vitamin A [32]. Along with T3, glucosonilates, present in watercress and other cruciferous vegetables, are powerful inducers of the key glucuronidation enzyme, UDP-glucoronosyltransferase [33]. Artichoke extract also has a similar effect [34].
6. Prevention of enterohepatic recirculation of female sex hormones
To prevent the absorption of female sex hormones in the intestines, first of all, it is necessary to consume a sufficient amount of fiber. Women who follow this recommendation have lower levels of estrogen in their blood [35]. Soy fiber and flax seed fiber absorb estrogens most actively. A major role in the recycling of estrogens from the intestine is played by 3-glucuronidase, a bacterial enzyme that cleaves glucuronic acid from detoxified compounds (estrogens). The most powerful inhibitor of the activity of this enzyme is calcium glucarate, a nutrient present in some vegetables [36]. In addition, Silymarin and licorice root also reduce its activity [37].
7. Reduced aromatase activity
As mentioned earlier, aromatase is an enzyme that converts andorostenedione to estrone and testosterone to estradiol. However, in some cases (obesity, exposure to herbicides [38], exposure to pesticides [39, 40], excessive alcohol consumption [42]) the activity of this enzyme increases significantly, which leads to the formation of large amounts of estrogens. High enzyme activity is indicated by normal or decreasing levels of androstenedione and testosterone in the peripheral blood, accompanied by high concentrations of estradiol and estrone. Today there are a fairly large number of aromatase inhibitors used to treat breast cancer. Among these drugs are Anastrasol and Arimidex. In addition, there are a number of natural compounds that have the ability to reduce enzyme activity. Among them, chrysin, apigenin, and naringenin can be distinguished [41]. However, aromatase inhibitors must be used with caution, as their use may cause relative or absolute androgen dominance. This will lead to acne, especially just before or during menstruation, ovarian cysts, and other symptoms of androgen dominance.
3 CONCLUSION
Thus, in the treatment of diseases associated with estrogen dominance, a safe and highly effective alternative to hormone therapy and therapy aimed at inhibiting the secretion of gonadotropins has emerged, which has a fairly stable positive effect on the course of the disease. The good clinical results of this approach are due to the impact of treatment on the causes that led to estrogen dominance, an understanding of the entire complex chain of estrogen metabolism, an integrated approach to the correction of hormonal imbalances, and the use of safe natural compounds that have a powerful modulating effect on estrogen metabolism.
BIBLIOGRAPHY
- Zhang F, Chen Y, Pis ha E, Shen L, Xiong Y, van Breemen KB, Bolton JL. The major metabolite of equilin, 4-hydroxyequilin, autoxidizes to an o-quinone which isomerizes to the potent cytotoxin 4-hydroxyequiknin-o-quinone. Zhang E, Chem Res Toxicol 1999 12(2):204-213.
- Chen Y, Liu X, Pisha E, Constantinou AI, Hua Y, Shen L, van Breemen RB, Elguindi EC, Blond SY, Zhang F, Bolton JL. A metabolite of equine estrogens, 4-hydroxyequilenin, induces DNA damage and apoptosis in breast cancer cell lines. Chem Res Toxicol (United States) May 2000, 13(5):342-350.
- Yao J, Li Y, Chang M, Wu H, Yang X Goodman JE, Liu X Liu H Mesecar AD, Van Breemen RB, Yager JD, Bolton JL. Catechol estrogen 4-hydroxyequilenin is a substrate and an inhibitor of catechol-O-methyltransferase. Chem Res Toxicol (United States) May 2003;16(5):668-675.
- Yao J, Chang M, Li Y, Pisha E, LiuX, Yao D, Elguindi EC, Blond SY, Bolton JL. Inhibition of cellular enzymes by equine catechol estrogens in human breast cancer cells: specificity for glutathioneS-transferase Pl-1. Chem Res Toxicol (United States) Jul 2002;15(7):935-942.
- Michnovicz JJ, Adlercreutz H, Bradlow HL. Changes in levels of urinary estrogen metabolites after oral indole-3-carbinol treatment in humans. J Natl Cancer Inst May 21 1997;89(10):718-723.
- Rahman KM, Li Y, Sarhar FH. Inactivation of akt and NF-kappaB play important roles during indole-3-carbinol-induced apoptosis in breast cancer cells. Nutr Cancer 2004;48(l):84-94.
- Ge X Fares FA, Yannai S. Induction of apoptosis in MCF-7 cells by indole-3-carbinol is independent of p53 and bax. Anticancer Res, Jul-Aug 1999; 19(4B):3199-3203.
- Chinni SR, Li Y, Upadhyay S, Koppolu PK, Sarhar FH. Indole-3-carbinol (I3C) induced cell growth inhibition, Gl cell cycle arrest and apoptosis in prostate cancer cells. Oncogene May 24 2001;20(23):2927-2936.
- Chen D, Carter TH, Auborn KJ. Apoptosis in cervical cancer cells: implications for adjunct anti-estrogen therapy for cervical cancer. Anticancer Res Sep-Oct 2004;24(5A):2649-2656.
- Bonnesen C, Eggleston IM, Hayes JD. Dietary indoles and isothiocyanates that are generated from cruciferous vegetables can both stimulate apoptosis and confer protection against DNA damage in human colon cell lines. Cancer Res (United States) Aug 15 2001;61(16):6120-6130.
- Kim DJ Shin DH, Ahn B, KangJS, Nam KT, Park CB, Kim CK, HongJT, Kim YB, Yun YWJangDD, YangKH. Chemoprevention of colon cancer by Korean food plant components. Mutat Res Feb-Mar 2003;523-524:99-107.
- Chang X, Toi JC, Hong C, Kim HA, Riby JE, Firestone GL, Bjeldanes LF. 3,3′-Diindolylmethane inhibits angiogenesis and the growth of transplantable human breast carcinoma in athymic mice. Carcinogenesis Apr 2005;26(4):771-778.
- ArnaoMB, Sanchez-Bravo J, Acosta M. Indole-3-carbinol as a scavenger of free radicals. Biochem Mol Biol Int (Australia) Aug 1996;39(6): 1125-1134.
- Staack R,Kingston S] Wallig MA, Jeffery EH. A comparison of the individual and collective effects of four glucosinolate breakdown products from Brussels sprouts on induction of detoxification enzymes. Toxicol Appl Pharmacol Mar 1998;149(l):17-23.
- Wallig MA, Kingston S, Staack R, Jefferey EH. Induction of rat pancreatic glutathione S-transferase and quinone reductase activities by a mixture of glucosinolate breakdown derivatives found in Brussels sprouts. Food Chem Toxicol (England) May 1998;36(5):365-373.
- Kishida T, Beppu M, Nashiki K Izumi T, Ebihara K Effect of dietary soy isoflavone aglycones on the urinary 16alpha-to-2-hydroxyestrone ratio in SZN/HeJ mice. Nutr Cancer (United States) 2000;38(2):209-214.
- Xu X, Duncan AM, Wangen KE, Kurzer MS. Soy consumption alters endogenous estrogen metabolism in postmenopausal women. Cancer Epidemiol Biomarkers Prev Aug 2000;9(8):781-786.
- XuX Duncan AM, Merz BE, Kurzer MS. Effects of soy iwflavones on estrogen and phytoestrogen metabolism in premenopausal women. Effects of soy isoflavones cm estrogen and phytoestrogen metabolism in premenopausal women. Cancer Epidemiol Biomarkers Prev Dec 1998;7(12):1101-1108.
- Adlercreutz H, Hockerstend K, Bannwart, et al. Effect of dietary components, including lignans and phytoestrogens, on enterohepatic circulation and liver metabolism of estrogens and on sex hormone-binding globulin (SHBG). J Steroid Biochem 1987;2 7(4-6):1135-1144.
- Matthews CE, Fowke JH, Dai Q, Leon Bradlow H, Jin F, Shu XO, Gao YT, Longcope C, Hebert JR Zheng W. Physical activity, body size, and estrogen metabolism in women. Cancer Causes Control (Netherlands) Jun 2004;15(5):473-481.
- Yee GC, Stanley DL, Pessa LJ, et al. Effect of grapefruit juice on blood cyclosporine concentration. Lancet 1995;345:955-956.
- Guerra MC, Speroni E, Brocolli M, et al. Companion between Chinese medical herb Pueraria lobata crude extract and its main isoflavone puerarin. Antioxidant properties and effects on rat liver CYP-catalysed drug metabolism. Life Set 2000;67:2997-3006.
- Miksicek RJ. Commonly occurring plant flavonoids have estrogenic activity. Mol Pharmacol 1993;44:37-43.
- Pollard JW. Modifiers of estrogen action. Sci Med Jul/Aug 1999:38-47.
- Riby JE, Feng C, Chang YC, Schaldach CM, Firestone GL, Bjeldanes LF. The major cyclic trimeric product of indole-3-carbinol is a strong agonist of the estrogen receptor signaling pathway. Biochemistry (United States) Feb 8 2000;39(5):910-918.
- Meng Qj Yuan F, Goldberg ID, Rosen EM, Aubom K, Fan S. Indole-3-carbinol is a negative regulator of estrogen receptor-alpha signaling in human tumor cells. J Nutr Dec 2000;130(12):292 7-2931.
- Yoon K, Pellaroni L, StonerM, Gaido K, Safe S. Differential activation of wild-type and variant forms of estrogen receptor a by synthetic and natural estrogenic compounds using a promoter containing three estrogen-responsive elements. J Steroid Biochem Mol Biol 2001;78:25-32.
- Yoon K, Pellaroni L, Ramamoorthy K, Gaido K, Safe S. Ligand structure-dependent differences in activation of estrogen receptor alfa in human HepG2 liver and U2 osteogenic cancer cell lines. Mol. Cell Endocrinol 2000;162:211-220.
- Bender DA. Novel function of vitamin B6. Proceedings Nutr Soc 1994;53:625-630.
- DeFlora S, Benniceli C, Camoiriano A et al. In vivo effects of N-acetylcysteine on glutatione metabolism and on biotransformation of carcinogen and/or mutagenic compounds. Carcinogenesis. 1985;6:1735-1745.
- Wellington K, Jarvis B. Silymarin: a review of its clinical properties in the management of hepatic disordes. BioDrugs 20()1;15(7): 465-489.
- Haberkorn V, HeydelJM, MounieJ, Artur Y, Gaudonnet H. Influence of vitamin A status on the regulation of uridine (5~~-) diphosphate-glucuronosyltransferase (UGT) 1A1 and UGT1A6 expression by L-triiodthyronine. British J Nutr 2001;85:289-297.
- Kassie F, Robot S, Uhl M et al. Chemoprotective effects of garden cress (Lepidium sativum) and its constituents towards 2-amino-3-methyl-imidazol[4,5-f]quinolin (IQJ-induced genotoxic effects and colonic preneoplastic lesions. Carcinogenesis 2002;23(7):1155 -1161.
- KirchhoffR Beckers CH, KirchhoffGM, Trinczek-Gartner H. Petrowicz O, Reimann HJ. Increase in choleresis by means of artichoke extract. Phytomed 1994;1:107-115.
- Goldin BR Adlercreutz H, Gorbach SL. et al. Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. New Engl J Med 1982;307:1542-1547.
- Dwivedi C, Heck Wf, Downie AA, Larroya S, Webb TE. Effect of calcium glucarate on fl-glucoronidase activity and glucarate content of certain vegetables and fruits. Biochem Med Metab Biol 1990;43:83-92.
- KumagaiA, Nishino K, Shimomura A, Kin T, Yamamura. Effect of glycyrrhizin on estrogen action. Endocrinol Japan 1967;14(l):34-38.
- HeckerM, Park JW, Murphy MB, Jones PD, Solomon KR, Van DerKraak G, CanJ A, Smith EE, du Preez L, Kendall RJ, Giesy JP. Effects of atrazine on CYP19 gene expression and aromatase activity in tests and on plasma sex steroid concentrations of male African clawed frogs (Xenopus laevis). Toxicol Sci (United States) Aug 2005;86(2):273-280.
- Holloway AC, Stys KA, Foster. DDE-induced changes in aromatase activity in endometrial stromal cells in culture. Endocrine (United States) Jun 2005;27(1):45-50.
- Sanderson JT, Boerma J, Lansbergen GW, van den Berg M, Induction and inhibition of aromatase (CYP19) activity by various classes of pesticides in H295R human adrenocortical carcinoma cells. Toxicol Appl Pharmacol (United States) Jul 1 2002;182(l):44-54.
- Sanderson JT, HordijkJ, Denison MS, Springs teel MF, Nantz MH, van den Berg M. Induction and inhibition of aromatase (CYP19) activity by natural and synthetic flavonoid compounds in H295R human adrenocortical carcinoma cells. Toxicol Sci (United Stales) Nov 2004;82(l):70-79.
- Etique N, Chardard D, Chesnel A, Merlin JE, Flament S, Grillier-Vuissoz I. Ethanol stimulates proliferation, ERalpha and aromatase expression in MCF-7 human breast cancer cells. Int J Mol Med (Greece) Jan 2004;13(l):149-55.
Types of female hormone
Three basic factions:
- Estradiol is the most important hormone. Before the onset of puberty in boys and girls, its concentration in the blood is the same; the content changes at approximately 12–13 years. Participates in the accumulation of fatty tissue on the chest, hips, development of the mammary glands, and maintains skin tone. In the pubertal phase, it forms sexual characteristics, in adult women it maintains the health of the skin and hair, slows down cellular aging, participates in the construction of bone tissue, utilizes harmful cholesterol, and affects emotional stability. During the gestational period, it helps to increase the size of the uterus along with the growth of the fetus, increases the metabolic rate, forms the bone tissue of the fetus and provides it with nutrients and oxygen.
- Estrone. Synthesized by the adrenal cortex, ovaries and fat cells. It is an “intermediate” hormone, used by the body as a raw material for the production of estradiol.
- Estriol. It has virtually no effect on hormone levels in women, is inactive in the body, and is found in small quantities. But immediately after conception, its level increases under the influence of gonadotropin to prepare the uterus for growth with an enlarged fetus. It also forms ducts in the breast for lactation, reduces the risk of uterine tone, prevents spasms, and increases blood flow in the uterine cavity. Produced by placental tissue.
Progesterone
Since there is a close relationship between estrogen and progesterone, it is worth mentioning that estrogen dominance can also be caused by low progesterone levels. What this means is that even if you have enough estrogen in your body, you can still suffer from estrogen dominance if your progesterone levels are very low.
Low progesterone levels typically occur in women who experience chronic stress, chronic exposure to estrogen, and a diet that lacks essential nutrients.
Estrogen norm
Normal hormone levels are determined by periods of the menstrual cycle:
| Type of estrogen | 1 phase | 2 phase | Pregnancy | Climax |
| Estradiol | 15-60 ng/l | 27-246 ng/l | 17-18 thousand ng/l | 5-30 ng/l |
| Estrone | 5-9 ng% | 3-25 ng% | 1500-3000 ng% | — |
| Estriol | — | — | 0.7-110 nmol/l | — |
Estriol is produced only by the placenta, from the moment of conception to 40 weeks. It is first synthesized from maternal cholesterol by the adrenal glands, then by the fetal liver.
During the gestational period, important values are not only the content of estriol in the mother, but also in the fetus. In the amniotic fluid in the 2nd trimester it should be in the range of 3.5–27.1 nmol/l, in the 3rd trimester – 7.3–69 nmol/l.
The main reasons for the increase in estrogen in the blood
- Increased load on the liver. Excess hormone is excreted by this organ; if the liver is overloaded with toxins, it will not be able to cope with this task in a timely manner. The accumulation of negative forms of estrogen can lead to endometriosis and breast cancer.
- Long-term constipation. The longer the time toxins in the form of negative forms of estrogen remain in the intestines, the more likely they are to get back into the blood and cause hormonal imbalance.
- Lack of sleep or insomnia. With prolonged sleep disturbances, stress levels increase, which is associated with the release of cortisol. Cortisol destroys progesterone and hormonal imbalance progresses.
- Problems with excess weight. Fatty tissue helps toxins accumulate and re-enter the bloodstream, overloading the liver. This load provokes the accumulation of excess estrogen.
- Xenoestrogens. These are hormones that do not belong to the human body, but imitate the action of estrogen and block the work of the real hormone. They come from the environment - these are synthetic substances contained in products, cosmetics, and household items.
To identify hormonal imbalances, you need to contact a gynecologist-endocrinologist. Self-medication never leads to positive results.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Symptoms of Imbalance
Estrogens actively influence the female body from the first menstruation to the development of menopause. Both an increase and a decrease in their volume inhibit reproductive function, spoil a woman’s appearance, the condition of the cardiovascular system, and the structure of bones and cartilage.
Signs of hormone excess in women
Normally, estrogen synthesis increases during puberty and during pregnancy, if it occurs without pathologies. In other periods, an increase in concentration is often caused by improper functioning of the body or the intake of the hormone from food and the environment.
Reasons for estrogen dominance:
- consumption of foods high in phytoestrogens;
- incorrectly selected hormone replacement therapy;
- frequent drinking of alcohol;
- excess weight;
- vascular diseases, heart disease, diabetes, hypertension;
- uncontrolled use of OK (oral contraceptives).
Symptoms of excess estrogen are:
- Excessive weight gain
. With increased levels of female hormones, adipose tissue accumulates mainly in the waist, buttocks, and thighs. - Irregular cycle
- scanty or, conversely, heavy discharge, breakthrough bleeding, hyperpolymenorrhea, amenorrhea and other disorders. - Breast tenderness and swelling
. Normally, this condition is observed a few days before the onset of menstruation and during pregnancy. If the mammary glands hurt in the middle of the cycle, this may indicate an increase in estrogen levels. - Increased emotionality
. PMS, sudden mood swings, depression, anxiety, panic attacks, and insomnia may develop. - Regular headaches
. Most often they are associated with approaching menstruation. - Hair loss
, baldness, deterioration of nails and hair. - Memory impairment
. Some scientists associate Alzheimer's disease with low levels of female estrogen. - Chronic fatigue
.
Important!
Complications of hyperestrogenism - endometrial hyperplasia, increased risk of bleeding, fibroids, endometriosis, cycle disorders. There are relative and absolute forms:
- relative hyperestrogenism
- a decrease in progesterone levels with the same amount of estrogen; - absolute hyperestrogenism
- an increase in estrogen with the same concentration of progesterone.
In adult women, hyperestrogenism can cause a condition similar to the manifestations of menopause - sweating, hot flashes, irritability, frequent headaches.
Symptoms of hormone deficiency
Estrogen deficiency can be caused by the following factors: taking hormonal drugs, thyroid pathologies, therapy for estrogen-dependent tumors in women, taking nootropics or antidepressants, sudden weight loss, pituitary gland diseases, unbalanced nutrition.
Estrogen deficiency can be determined by the following symptoms:
- During puberty, there may be a delay in the formation of secondary sexual characteristics - absence of menarche until 15–16 years of age, irregular periods, formation of a male-type figure in girls with a narrow pelvis, broad shoulders and developed muscles. The imbalance is also manifested by a decrease in the size of the uterus, underdevelopment of both external and internal reproductive organs.
- During menopause, a decrease in estrogen is normal. If the concentration of hormones falls at the age of 40–45 and earlier, the symptoms of menopause appear more clearly - rapid heartbeat, profuse sweating, hot flashes, dizziness, migraines.
- After the age of 35–40, the main symptoms are weight gain, disruption of the gastrointestinal tract, the appearance of wrinkles, cellulite, stretch marks, moles and papillomas in large numbers, decreased libido, high heart rate, and impaired blood circulation in the brain.
- In young women, estrogen deficiency leads to frequent colpitis, vaginitis, cycle disruptions, pronounced PMS, decreased performance, joint pain, changes in blood pressure, and lack of lubrication in the vagina.
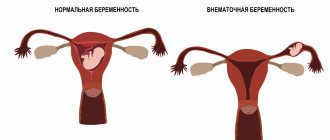
During pregnancy, such a pathology is fraught with disruptions in the development of the placenta, abruption, miscarriage, abnormalities in the formation of the child’s nervous and cardiac systems, and uterine bleeding. The risk of genetic abnormalities in the fetus, in particular Down syndrome, also increases.
Increased hormone levels
Among women
Some of the most important hormones in a woman’s body are estrogen and progesterone. Both are produced in the ovaries. These hormones are released at different phases of the menstrual cycle.
On the first day of menstruation, the pituitary gland releases follicle-stimulating hormone (FSH). Under its influence, the follicle begins to develop on the ovary and estrogens are released. As soon as their level rises to a certain point, they block the release of FSH. This occurs approximately on the 12th–15th day of the cycle.
At this time, the pituitary gland begins to secrete another hormone - luteinizing hormone (LH). When its level rises, ovulation occurs - the follicle bursts and an egg ready for fertilization emerges. After ovulation, estrogen levels decrease and progesterone begins to be produced in the ovaries.
Schematically, the production of hormones during the menstrual cycle can be represented as follows:
follicle-stimulating hormone (pituitary gland) → estrogens (ovaries) → luteinizing hormone (pituitary gland) → progesterone (ovaries)
Oral contraceptives operate on this principle: they regulate the amount of female hormones in the body. At the same time, they reduce the level of FSH to such an amount that luteinizing hormone does not begin to be produced. No luteinizing hormone - no ovulation.
In men
Normally, in men, the amount of estradiol should fluctuate between 50–130 pmol/l. Increased hormone levels in men may indicate a tumor in the testicles.
How to check your estrogen levels?
A basic estrogen test is a blood test.
It contains all 3 fractions of the hormone, the ratio of each type is determined in accordance with the following factors:
- age;
- presence or absence of pregnancy;
- taking medications containing any hormones;
- weight.
It is important to take the test in accordance with the duration of the cycle:
- if the cycle is 20–21, blood is taken 2–3 days from the start of the first bleeding;
- with a cycle of 28 days – 3–5 days;
- more than 28 days – in the range of 5–7 days from the start of menstruation.
If the cycle is irregular, an ovulation test is first performed.
Within 24 hours of its onset, the concentration of estrogen reaches its peak. Before taking tests, a woman is recommended to limit her intake of hormone-containing drugs, exclude sexual activity, and physical activity.
The last meal is possible no later than 10 hours. You can find out the answer in 20–30 minutes.
Treatment of hormonal imbalance
The main goal of therapy is to normalize the stages of estrogen production, increase or decrease concentrations to normal.
During the pubertal phase, menopause and or pregnancy, treatment with hormones (gestagens and estrogens) is not carried out.
Medicines
If, in case of hormone deficiency, it is necessary to take drugs that can restore estrogen, then in case of its excess it is strictly forbidden to be treated with such drugs.
To increase estrogen levels
If estrogen is synthesized in a woman in small quantities, the following drugs are prescribed:
| Name | Action |
| Premarin | Conjugated estrogen. Contains natural estrogens. Used for estrogen deficiency, after surgery on the uterus, ovaries, to prevent osteoporosis during the menopause phase. |
| Proginova | Contains estradiol valerate, restores the volume of steroid hormones, improves the condition of cartilage and bone tissue, removes symptoms of menopause, improves skin condition, and slows down aging. |
| Veroshpiron | Includes spironolactone, which has an estrogen-like effect. It has a diuretic effect, reduces testosterone concentrations, and is used in the treatment of polycystic ovary syndrome and menstrual disorders. Reduces the manifestations of female alopecia, skin problems, male pattern hair growth. |
| Hemafemin | Contains deer pantohematogen, increases the concentration of estrogen in the female body, additionally includes vitamins C, E. Affects the functioning of the ovaries, eliminates hot flashes and pressure surges. Not used during pregnancy, with caution - in case of impaired blood clotting or thrombosis. |
| Stella | Stimulates the production of estrogen, reduces the activity of papillomavirus, reduces the risk of developing tumors that produce estrogen. Contains broccoli extract, silicon dioxide, green tea, lactose, soy extract. |
| Ovestin | Contains estriol. Used to reduce the brightness of menopause, in the treatment of infertility, after surgical extirpation of the uterus, ovaries, and tubes. |
| OK (Estrogenolite, Janine, Aktivel, Lindinet, Femoden) | Monophasic contraceptives contain synthetic estrogens in small doses. They enhance the natural process of hormone production and stop ovulation. |
Remedies of this type are often produced in tablets, replenishing the lack of estrogen. Hormone replacement therapy drugs are used for menopause, estrogen deficiency, and infertility. Oral contraceptives are often prescribed to normalize the cycle, for endometriosis, and breakthrough bleeding.
To reduce estrogen levels
In this case, antiestrogenic drugs are used.
Prescribed depending on the cause of low levels of female hormones:
- Antitumor drugs: Arimidex, Femara.
- For uterine, ovarian and anovulatory infertility: Tamoxifen.
- For breast cancer: Letrozole.
Review of tablets containing estrogen →
Estrogen in food
{banner_banstat9}
The effect of drug treatment can be improved with the help of properly selected nutrition.
To increase performance
The activity of estrogen production can be increased by including foods that are rich in hormone-like substances in the menu:
- vegetables
- eggplants, tomatoes, carrots, pumpkin, beets; - greens, herbs
- celery, parsley, asparagus, spinach, basil; - fruits and berries
- pomegranates, dates, cherries, melons, apricots, papaya, grapes, raspberries; - dairy products
- cheese, butter, sour cream, cottage cheese, kefir; - sunflower seeds
, flax seeds, pumpkin seeds, peanuts, sesame seeds; - garlic
, mustard.
To preserve the maximum benefits of products, subject them to minimal heat treatment, include them in the menu every day, choose only fresh vegetables and fruits, and cook them once.
To reduce performance
{banner_banstat10}
The purpose of the diet: weight loss, normalization of the digestive tract:
- exclude canned food, fatty meats, sausage, coffee, beer and alcohol in general;
- consume more: mushrooms, citrus fruits, green tea;
- Replace cow's milk with coconut or rice milk.
Folk remedies that increase estrogen
Estrogen metabolism, as well as hormone concentrations, can be normalized using folk remedies:
- Take 20 fresh raspberry leaves and pour 200 ml of boiling water for one hour. Drink instead of regular tea 2 times a day, first strain and cool. Start taking it in the middle of your menstrual cycle.
- Pour 100 ml of boiling water over 5 hop cones, simmer for 5 minutes, then add 5 mint leaves, leave for 40 minutes. Drink half a glass three times a day for 1 month.
- Pour 100 g of plantain seeds with 50 ml of fresh flaxseed oil. Leave it for a day. Then take one teaspoon before meals three times a day.
- Grind 100 g of fresh nettle leaves, squeeze the juice from half a lemon, grate the peel, mix everything. Boil with 300 ml of water over low heat for 10 minutes, leave under a closed lid for half an hour. Then strain, take up to 3 glasses a day instead of tea.
- Take equal amounts of dried lemon balm and rose hips, add water so that it covers the dry ingredients. Boil for about half an hour, cool, strain and drink 1 glass in the morning and before bed instead of tea.
You can increase the synthesis of natural hormones in the female body using aromatherapy. Use oil of cypress, rose, lavender, mint, bergamot, orange, birch buds. They can also be used for bathing and massage.
Hormone levels in the body after menstruation
After menstruation, estrogen levels gradually increase, which helps the endometrium grow in the uterus. The woman’s general condition is gradually normalizing.
The main symptoms characterizing a woman’s condition after menstruation:
- normalization of mood - the correct balance of hormones is established;
- improvement of skin condition - progesterone is not produced as actively;
- the appearance of energy and increased performance is a consequence of an increase in estrogen.
Interesting! Estrogen is considered the hormone of female beauty. It makes a woman a woman and stimulates her sexuality.
Note that during this period a woman looks most attractive.
Possible consequences and complications
If estrogens are secreted in insufficient quantities, there is no therapy, and pathological conditions develop:
- obesity;
- bone destruction;
- thrombosis;
- infertility;
- mastopathy;
- breast tumors;
- metabolic disorders;
- thyroid pathology;
- mental and nervous disorders;
- ovarian cysts;
- menstrual cycle disorders.
With excess estrogen, weight also increases, skin condition worsens, breast sensitivity increases, and blood pressure rises. Sleep, gastrointestinal function, and psycho-emotional background suffer.
The main task of estrogen is to provide a woman with the opportunity to become pregnant and bear a fetus. It is also thanks to this hormone that girls develop a typically female figure, thinner and more elastic skin than men, and no hair in the chest and abdomen. With an excess or deficiency of all fractions of estrogen, hormonal levels are disrupted, which is fraught with health complications and difficulties in conceiving and bearing a fetus.
What can a lack or excess of estrogen lead to?
As is already clear, the physical and psychological state of a woman directly depends on the level of estrogen in the blood, so it is very important to monitor this indicator and take action in case of any imbalance.
Consequences of falling estrogen levels:
- various pains, mainly headaches and heart pain, as well as pain in the lower back, back;
- deterioration of thermoregulation, in particular hot flashes;
- bone fragility;
- vasoconstriction;
- memory impairment;
- the appearance of wrinkles;
- fluctuations in the emotional background.
With an excess of estrogen, women experience:
- various inflammations;
- bloating;
- increased blood pressure;
- aggression, irritability and sleep problems;
- all kinds of pain.
There are several reasons for the decrease and increase in estrogen in a woman’s body. It could be
- dysfunction of the pituitary gland,
- unbalanced diet,
- too much physical activity,
- menopause and the period preceding it.
Excess estrogen is rare; usually it is the lack of this hormone that has to be corrected. Its most common cause is age-related changes in the female body, which begin after 40 years. Unfortunately, it is impossible to avoid them and ensure eternal youth, but there are ways to slow down such processes.