Hypoestrogenic conditions in women of reproductive, pre- and menopausal ages
Hypoestrogenic conditions include changes in the body of women against the background of a decrease or cessation of estrogen production by the ovaries.
First of all, a complex of vegetative-vascular, neuroendocrine and neuropsychic symptoms arises (early temporary disorders). Then urogenital and sexual disorders and changes in appearance appear (medium-term disorders). Late metabolic disorders occur last: osteoporosis, coronary heart disease, Alzheimer's disease [1].
These numerous symptoms of hypoestrogenism are associated with the presence of a huge number of estrogen receptors in various organs and systems of a woman: genitals, hypothalamus and pituitary gland, cardiovascular system, urethra and bladder, skin and hair, large intestine, liver [2].
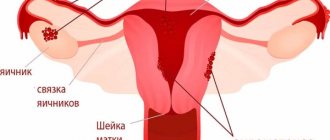
The above changes can occur not only naturally during menopause, but also when a woman’s body is exposed to other factors: after surgical operations (removal or resection of the ovaries due to cysts and apoplexy, amputation of the uterus); with depletion of the follicular apparatus (ovarian depletion syndrome) [3, 4]; with a perverted reaction of estrogen receptors (resistant ovarian syndrome); against the background of the use of certain medications, in particular hormone-releasing hormone agonists (AH-RG); in the treatment of estrogen-dependent diseases of the female reproductive system, as well as in long protocols for stimulating superovulation in the in vitro fertilization (IVF) program for the treatment of infertility (requires add-back therapy to relieve neurovegetative symptoms) [5, 6].
Hypoestrogenic conditions associated with a slight decrease in estrogen production (with sparing resection of the ovaries, cauterization of not polycystic, but multifollicular ovaries, etc.) have their own special clinical manifestations, most often leading to impaired reproductive function (anovulation, luteal phase deficiency; reduced ovarian reserve , leading to a poor ovarian response in IVF programs) [7]. According to our data, such patients occur in IVF programs in 22.3% of cases.
Hypoestrogenism in the menopausal period can serve as a model for studying the classical clinical manifestations of this condition, since menopause is a natural rather long biological process of transition from the reproductive period to old age, which is based on the gradual decline of ovarian function and a decrease in estrogen production. Early-time disorders manifest themselves most clearly [1]. The complex of symptoms of early-term disorders with a certain degree of severity is usually called climacteric syndrome (CS). According to our data obtained together with I.V. Besman [8], CS in perimenopause occurs in 57.6% of cases, while in 65% it occurs in a complicated form (i.e., against the background of extragenital pathology). The complicated form of CS causes the maximum severity of CS symptoms. Currently, early symptoms of hypoestrogenism are associated with disorganization of the function of the limbicoreticular complex. Impaired hypothalamic function is associated with manifestations of early-onset disorders such as hot flashes, hyperhidrosis, palpitations, and hypertension. Depression, sleep disturbances, headaches, and memory loss are associated with dysfunction of the limbic system. All early-term disorders reduce a woman’s quality of life, but this is especially true for hot flashes and sleep disorders. Hot flashes can bother a woman 5–10–20 or more times a day. Sleep disorders: prolongation of the period of falling asleep, frequent awakenings at night, shallow sleep - do not give the feeling of proper rest. Undoubtedly, all these disorders require a differentiated approach to treatment depending on the cause of hypoestrogenism and the age at which they occur.
Today, hormone replacement therapy (HRT) is considered a non-alternative pathogenetic therapy for early symptoms of hypoestrogenism [1, 6]. In women of reproductive age after surgical removal or resection of the ovaries, with resistant and exhausted ovarian syndromes, treatment can begin with combined estrogen-progestogen drugs [1]. These can be modern three-phase drugs, for example Qlaira. In women after hysterectomy, therapy is carried out using natural estrogens followed by the addition of gestagens [6]. If oral drugs are poorly tolerated, they can be recommended in the form of a gel or patch for percutaneous administration (Estrogel, Divigel, Klimara) with periodic administration of gestagens vaginally (for example, Utrozhestan). The duration of HRT is determined by the condition and well-being of the patient.
During menopause, when treating early-onset disorders, it is important to adhere to the position of the International Menopause Society (2007):
- HRT is prescribed for clear indications, primarily for the relief of menopausal symptoms;
- the need for continued treatment and the presence of indications for HRT should be reviewed regularly, especially with long-term use.
In addition, modern principles for prescribing HRT should be taken into account:
- only natural estrogens are used (17β-estadiol, estradiol valerate);
- minimally effective doses of hormones are used;
- the drug is selected individually;
- before therapy, a special examination is carried out, during therapy - daily monitoring;
- the start of HRT should not be later than 5 years from the onset of menopause;
- HRT should not be prescribed if there are contraindications.
Contraindications to HRT:
- skin lesions;
- estrogen-dependent tumors of the genital organs;
- suspected presence or presence of breast cancer;
- venous thromboembolism;
- severe liver and kidney diseases;
- bleeding from the genital tract of unknown origin.
HRT modes:
- In perimenopause - cyclic drugs that imitate the normal menstrual cycle (Klimonorm, Cyclo-Proginova, Estrogel, Divigel + Utrozhestan, Duphaston, Klimen, Femoston 1/10, 2/10, etc.).
- In postmenopause - continuous therapy that does not cause bleeding: Angelique (1 mg 17β-estadiol + 2 mg drosperinone), Mirena + Klimara, Klimadien (estradiol valerate + dienogest), Estrogel + Utrozhestan, Livial (tibolone), Femoston 1/5.
- In the absence of a uterus, monotherapy with estrogens (Klimara, Proginova, Estrogel, Divigel).
- For obesity, metabolic syndrome, increased risk of vascular episodes, phase therapy with transdermal and vaginal forms (Estrogel, Divigel, Utrozhestan).
- If the patient refuses HRT or there are contraindications, decide on the use of herbal medicine in the form of homeopathic medicines and dietary supplements, which include estrogen-like substances. These drugs have virtually no contraindications and contain cohosh extract, soy, vitamins, minerals, etc. Among them are Remens, Klimaxan, Klimaktoplan, Klimadinon, QI-CLIM, Menopace Plus, Estrovel, Menoril, Soifem, etc.
The drug Menopace Plus is interesting in its composition, which includes capsules with vitamins and minerals (21 components), as well as herbal tablets containing soy isoflavones, flax seed lignans, sage and green tea. The components of the herbal tablet are converted into phytoestrogens in the intestines, have a beneficial effect on the nervous system, reduce hot flashes, and are sources of antioxidants. The cycle of taking this drug, one capsule and one herbal tablet per day, is 28 days.
We, together with I.V. Besman [9], have experience in the use of alternative herbal remedies to HRT in the treatment of a complicated form of CS in cases where HRT was contraindicated. Our studies have shown that the quality of life of these patients, determined by a special scale, is somewhat worse than that of those who took HRT; but significantly better than those who did not take any drugs at all. In addition, these drugs give a good effect in relieving vasomotor symptoms in long protocols with AG-RG IVF programs.
All of the above once again confirms the opinion of experts that a differentiated approach to the treatment of early-term disorders in hypoestrogenic conditions using HRT of various regimens or alternative herbal remedies gives a good effect and significantly improves the quality of life of women.
Literature
- Medicine of menopause / Ed. V. P. Smetnik. Yaroslavl: Litera Publishing House LLC, 2006. 848 p.
- Kulakov V.I., Prilepskaya V.N. Practical gynecology. Clinical lectures. 3rd ed., add. M.: MEDPress-inform, 2006. 720 p.
- Dobrokhotova Yu. E. Hysterectomy in reproductive age (systemic changes in a woman’s body and methods of their correction). Author's abstract. dis. Dr. med. Sci. M., 2000. 36 p.
- Zaidieva Ya. Z. Hormone replacement therapy. Pharmacology and clinical application. M.: 2001. 50 p.
- Infertile marriage. Modern approaches to diagnosis and treatment: a guide / Ed. G. T. Sukhikh, T. A. Nazarenko. 2nd ed., rev. and additional M.: GEOTAR-Media, 2010. 784.: ill.
- Guide to outpatient care in obstetrics and gynecology / Ed. V. I. Kulakov, V. N. Prilepskoy, V. E. Radzinsky. M.: GEOTAR-Media, 2006. 1056 p.
- Nazarenko T. A. Stimulation of ovarian function. 3rd ed., add. M.: MEDPress-inform, 2011. 272 p.: ill.
- Besman I.V., Rudakova E.B. Medical tactics for complicated forms of menopausal syndrome in perimenopausal women // Omsk Scientific Bulletin. 2010. No. 1 (94). pp. 10–13.
- Rudakova E. B., Besman I. V. Quality of life as a criterion for the effectiveness of treatment of menopausal syndrome // Omsk Scientific Bulletin. 2008. No. 1 (65). pp. 81–84.
E. B. Rudakova1, Doctor of Medical Sciences, Professor T. V. Strizhova, Candidate of Medical Sciences L. Yu. Zamakhovskaya
GBUZ MO MOPC, Balashikha
1 Contact information
Abstract. Pathogenetic therapy treatment of early symptoms of hypoestrogenism consists of hormone replacement therapy (HRT). In the case of contraindications to the HRT medication or refusal of a woman, alternative herbal medication is effective less than HRT, but however improves the quality of life.
Menopause (menopause) and hormone replacement therapy
Belarusian Medical Academy of Postgraduate Education
Menopause is a natural period during which a woman’s reproductive function declines. Its onset is genetically determined and, as a rule, ends with menopause - the cessation of ovulation, menstruation and the ability to bear children. In women of the European population, this period occurs at the age of 45-55 years with the peak of menopause at the age of about 50 years. The process of aging of the ovaries with a decrease in inhibin levels and the appearance of anovulatory cycles begins quite early, after 35 years, and accelerates after 40 years. The period of a woman’s life from 2 to 6 years before menopause is called premenopause, the period from the onset of menopause for 1-2 years before and after menopause is called perimenopause, and the subsequent years of life are called postmenopause. Some clinicians divide postmenopause into early (first 2-6 years) and late (subsequent years of life). Menopause that occurs before the age of 40 is considered pathological, and its cause should be clarified. Late menopause (after 55 years) is often caused by tumors that produce estrogen.
Until the 20th century, women, as a rule, did not live to see menopause, dying from various causes during their childbearing years. With the development of civilization, women's life expectancy has increased. According to WHO experts, by 2025 the number of women aged 60 years and over will exceed 1 billion. By 2015, the proportion of women over 45 years of age in all countries of the world will reach 46% of their total number.
The onset of menopause is genetically very stable and has not changed over the past 100 years, although some environmental and social factors can accelerate it, for example smoking (by 1.5 years) [8].
Pathophysiology of menopause and problems associated with it
For many years, the prevailing hypothesis was that the onset of menopause is caused by primary changes in the hypothalamic centers with a decrease in their sensitivity to estrogens and an inadequate increase in pituitary gonadotropins (FSH and LH). Currently, the dominant hypothesis is that there is a primary failure of inhibin production by aging ovaries. This process is likely controlled by the aging gene. A decrease in the level of inhibin causes a constant increase in the level of FSH, and then LH. This leads to the appearance of anovulatory cycles and subsequently to complete atresia of the follicles. The cessation of ovulation disrupts the cyclic secretion of estradiol and progesterone, ovarian sclerosis occurs and fertility is irreversibly impaired. With the advent of anovulatory cycles, the number of which progressively increases, the menstrual cycle gradually lengthens. At the same time, during each cycle the number of growing follicles decreases until their reserves are completely depleted. This process takes from 2 to 8 years. During premenopause, estradiol and LH levels remain normal. Estradiol usually remains at normal levels until the growth and development of follicles completely ceases. The duration of the follicular phase is the main determinant of the length of the menstrual cycle. FSH and inhibin levels are inversely proportional. Despite the fact that inhibin is a more sensitive marker of ovarian follicular function, it is not possible to determine it in clinical practice, so the level of inhibin can be judged by the FSH level. Estrogen saturation during hormone replacement therapy (HRT) only slightly reduces FSH, since it responds exclusively to inhibin. Therefore, FSH indicators cannot serve as markers of estrogen saturation during HRT. Against the background of an increase in FSH (10-20 times higher than normal), LH levels can remain normal, normal ovulatory cycles are observed, and even premenopausal women are not immune from accidental pregnancy, at least until an increase in the level of not only FSH, but also LH. In this regard, in the medical literature there are reports of cases of pregnancy in women aged 60 years and older. These women were likely premenopausal.
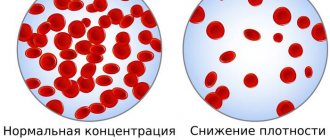
Only 10% of women stop menstruation immediately, but for the majority, menopause is preceded by a period of prolonged irregularity of menstruation [8]. During this period, bleeding appeared at the end of the period of inadequate luteal phase or at the peak of estradiol release, which was not accompanied by adequate ovulation or the formation of the corpus luteum. After menopause, the supply of follicles disappears quite quickly, which leads to a 10-20-fold increase in FSH and an approximately 3-fold increase in LH, reaching its maximum values in the first 1-3 years after menopause. After menopause, the main estrogen in a woman’s body becomes estrone, which is formed as a result of aromatization of androstenedione in peripheral tissues (fat, muscle, etc.). The level of androstenedione in the blood after menopause is 50% of that before menopause. Most androstenedione is produced in the adrenal cortex, and only a small amount is secreted by the ovarian stroma. The level of testosterone in the blood decreases in most women during menopause, but in some the secretion of testosterone by the ovaries even increases. This is due to the effect of high levels of gonadotropins on ovarian stromal tissue in the absence of follicles and when estrogen levels decrease. However, the total amount of testosterone secreted in postmenopausal women decreases due to a decrease in the primary sources of peripheral conversion of androstenedione. In postmenopause, estradiol is formed in small quantities (10-20 pg/ml) as a result of tissue conversion of estrone. Circulating levels of estrone are higher than estradiol, 30-70 pg/ml. The total amount of estrogens is 45 ng/24 hours. Almost all of them are of tissue origin as a result of peripheral conversion of androstenedione [9]. The ratio of androgens and estrogens changes sharply in the direction of androgens, so moderate manifestations of hirsutism are often observed in postmenopause. With age, the content of DHEA and DHEA-S decreases, while the levels of androstenedione, testosterone and estrogens circulating in the blood of postmenopausal women remain relatively stable.
During menopause, estrogen production in the ovaries ceases, however, in some postmenopausal women, estrogen levels due to tissue conversion of androstenedione and testosterone to estrone can be significant. The clinical manifestations of estrogen excess can vary and greatly depend on the degree of extraglandular formation. The conversion of androstenedione to estrone directly correlates with the amount of fatty tissue that can contribute to this conversion. In combination with a decrease in the level of sex hormone binding globulins, this can lead to endometrial and breast cancer. Thus, body weight is positively correlated with estrone and estradiol levels. The aromatization of androgens to estrone is especially pronounced in adipose tissue, although it also occurs in other tissues (to a lesser extent). With age, in late postmenopause, the ovarian stroma is completely depleted, however, despite continued intense stimulation by very high levels of FSH and LH, steroidogenesis in the ovary ceases.
At the same time, the contribution of adrenal precursors to the formation of estrogens in tissues becomes insufficient to maintain estrogen-dependent organs and tissues. As a result, underweight women especially suffer from a lack of estrogen. Menopause may begin earlier in women following a vegetarian diet, and, conversely, obese women often suffer from excess estrogen. What all menopausal women have in common is that they are deprived of progesterone.
For many years, clinical situations associated with changes in the production of estrogen and progesterone during menopause were considered only from the standpoint of loss of reproductive ability. Over the past 40 years, the understanding of the participation of sex steroids in physiological processes has expanded significantly. Receptors for estrogen have been found not only in the tissues of target organs (uterus, ovary, mammary gland), but also in other tissues: urethra, bladder, pelvic floor muscles, brain cells, myocardium, arterial walls, bone tissue, skin, mucous membranes mouth, larynx, conjunctiva, etc. It is logical to assume that almost all steroid hormones, both sex and adrenal, somatotropin and thyroid hormones have receptors in all tissues of the body, without exception, and differ only in quantity and sensitivity. They are actively involved in maintaining the normal functioning of many important systems (nervous, cardiovascular, immune, etc.), determining the cellular synthesis of protein, lipids, energy complexes, the activity of enzyme systems, the balance of basic electrolytes, as well as the activity of life processes in cells and, as an outcome, their aging and death (meaning what is usually called the general biological effect of certain hormones, most often against the background of their deficiency).
Consequently, against the background of estrogen deficiency in menopause, and sometimes in premenopause, various clinical manifestations of this deficiency in the form of painful conditions can develop. Quite often they are of a pronounced nature, which served as the basis for distinguishing them into a separate nosological form - menopausal syndrome (CS). However, even if the clinical manifestations do not assume the character of CS, many clinicians call them a decrease in quality of life. This concept includes changes in the perception of ordinary life situations, suspiciousness, anxiety, sleep and memory disorders, vegetative disorders, etc. In recent years, scientific data have appeared that to some extent explain disturbances in higher nervous activity in menopausal women by estrogen deficiency, in particularly estradiol. During menopause, the secretion of neuropeptides in the central nervous system and hypothalamus is disrupted, and this is logical, because it has been proven that the only representative of estrogens in the central nervous system (regardless of gender) is estradiol. Estrogens enhance the serotonergic and cholinergic systems and increase the sensitivity of dopaminergic receptors. Moreover, the greatest changes during estrogen deficiency are observed in the hippocampus and frontal lobe of the cerebral cortex [5]. Disruption of the interaction of neurotransmitters, as it turns out, determines the psychological characteristics of a woman’s behavior as she ages [3].
Menopause is not always accompanied by severe depressive states, but there is always a decrease in mood or some degree of depression. Loss of progesterone is fraught with the clinical picture of relative hyperestrogenism with an increased risk of target organ cancer or bleeding in premenopause. Estrogen deficiency is directly related to dyslipidemia and the progression of atherosclerosis, changes in the state of the immune system - a surge in a whole complex of autoimmune diseases (thyroid gland, connective tissue, joints, etc.). Aging of cartilage tissue, together with the loss of calcium, first in spongy and then in tubular bones, leads to the development of osteoporosis, osteoarthropathy of the spine with irreversible deformation or fractures of the limbs with the slightest trauma. The incidence of spontaneous fractures in late postmenopausal women increases to 40%. Another problem - arterial hypertension, insulin resistance with the development of type 2 diabetes mellitus with obesity, dyslipidemia (metabolic syndrome, resulting in a sharp increase in the number of vascular accidents - myocardial infarction, strokes) - is also directly related to menopause. There is evidence of an increase in the incidence of Alzheimer's disease in menopausal women and a noticeable decrease in its detection in women receiving HRT.
These general biological problems should not be associated with the severity of the manifestations of menopausal syndrome. The problem of hormonal correction of menopause is broader. Most clinicians view it as an opportunity to slow down the aging process and improve the quality of life of women after 46 years, given that the average life expectancy at menopause is 30 years. In this regard, three problematic questions arise, to which there are currently no clear answers:
- Do not interfere during menopause, believing that everything that happens during this period is physiological and should be.
- Menopause and menopause are genetically inevitable processes, but, taking into account the existing medical knowledge about them, they are subject to correction, like any other condition accompanied by hormonal deficiency.
- It is necessary to intervene, but only when menopause is accompanied by menopausal syndrome.
Attitudes towards menopause vary among clinicians and depend on knowledge about the pathophysiology of menopause and menopause. Perhaps, opinions agree on one thing: CS should be corrected, since this condition causes health problems and is regarded as a disease. Hormonal replacement should be carried out, and you should not wait for the consequences of a deficiency of estrogen and progesterone and other hormones to appear. Replacement or corrective (premenopausal) hormonal therapy is carried out (of course, with the woman’s consent) exclusively individually, taking into account several factors:
- Hormonal status of the woman (hypoestrogenic, euestrogenic, hyperestrogenic), absence or presence of manifestations of CS.
- Features of the physiological course of menopause: what “falls out”, what dominates in the late fertile period, premenopause, perimenopause, menopause, postmenopause and late postmenopause.
- Hormonal correction and replacement must correspond to the pathophysiological ones, and the doses of hormones must be minimally sufficient for the metabolic correction of their deficiency.
- In case of CS, regardless of the degree of its manifestations and the phase of menopause, hormone replacement therapy is the main and pathogenetic treatment. All other methods should be considered as auxiliary (auxiliary), contributing to the rapid achievement of the goal - restoration of metabolic disorders as a consequence of estrogen and progesterone deficiency.
- HRT is a method of “preventing” diseases of aging (arterial hypertension and vascular accidents, osteoporosis, osteoarthropathy, Alzheimer’s disease, metabolic syndrome and type 2 diabetes).
- HRT is a method of truly improving the quality of life of women after 45 years of age, and perhaps one of the ways to suppress the aging gene.
- The HRT complex should include thyroid hormones, growth hormone, DHEA and melanotonin.
Menopausal syndrome is a complex of pathological symptoms caused by a deficiency of estrogen and progesterone, which often accompanies a woman during menopause. According to V.P. Smetnik [2], the frequency of CS ranges from 40 to 60% and its manifestations can be of any severity - from mild to severe. The degree of severity is judged either by the number of “hot flashes” (up to 10 per day - mild, 20 - moderate, more than 20 - severe CS) or by the Kupperman index, where each symptom is assessed in points (up to 20 points - mild, up to 35 - moderate , more than 35 - severe CS).
The most common symptoms of CS:
1. Menstrual cycle disorders: anovulatory cycles, decreased fertility, decreased menstrual blood loss, dysfunctional uterine bleeding, irregular menstrual cycle.
2. Vasomotor symptoms: hot flashes, sweating, chills, palpitations, dizziness, pressure changes, skin hyperemia, paresthesia. “Hot flashes” - an almost obligatory symptom of CS - are often accompanied by erythrophobia (redness of the face, neck, upper half of the body), combined with chills, dizziness, and hypertension. Their duration is no more than 1-2 minutes, rarely (in persons with concomitant vegetative-vascular dystonia) - up to 20-30 minutes. There is no dependence on any factors; they can be provoked by psycho-emotional stress. Profuse sweating, as in hypoglycemia. In patients with diabetes mellitus, it is necessary to differentiate from hypoglycemia by determining blood glucose. It can be combined or replaced by “tides”, but it can also be without them. It is more often observed at night, wakes women up, and deprives them of sleep. Less of a concern in the cold season. Paresthesia - a feeling of "crawling" or numbness of the limbs - is often combined with "hot flashes". Attacks of pain can be of any nature, of varying duration, in the form of spasms for up to 30 minutes, of any localization (in the heart, right hypochondrium, etc.). They can be treated with sedatives, β-blockers, and antispasmodics. Arterial hypertension is often combined with “hot flashes”, pain, and is easily relieved with antihypertensive drugs (blood pressure often drops sharply, even to the point of hypotension, from the usual intake of dibazole, when therapeutic doses are mistakenly administered, as in hypertension). Attacks of tachycardia and increased blood pressure can be relieved with psychotropic and sedative drugs (Elenium, Seduxen 1-2 ml IM).
3. Neuropsychic symptoms: irritability, tearfulness, insomnia, decreased mood, persistent migraine-like headaches, sometimes depressive states, conflict at home, at work, short temper, intolerance, memory impairment (due to decreased concentration), suspiciousness. These phenomena are relieved by sedatives and psychotropic drugs, but only for the period of their effect. They finally disappear no earlier than after 2-3 months with the use of HRT.
4. Vestibular disorders: dizziness can be of the nature of a Meniere-like syndrome, with nausea, tinnitus, loss of balance, and falls. May be accompanied by short-term loss of consciousness with falls, bruises and other injuries. Diagnosis is quite difficult. Attacks are relieved with sedatives and antispasmodics. They finally go away with the use of HRT.
5. Diencephalic symptoms, simulating diencephalic, sympathoadrenal crises, begin more often at night or in the evening with palpitations (before embryocardia), increased blood pressure, changes in skin color (pallor of the skin of the face and limbs), severe weakness, a feeling of fading and cardiac arrest, fear of death. Often accompanied by chills, tremors, dizziness, and sweating. Less common are adynamia, motor aphasia, and short-term loss of consciousness. The attack lasts for several minutes (5-10, up to 20 minutes), passes on its own, and is replaced by polyuria and chills. Can be treated with sedatives (seduxen). The symptoms disappear completely with the use of HRT.
6. Cardiovascular disorders (dishormonal cardiopathy) most often manifest themselves as pain in the heart area. The pain is intense, prolonged, aching or stabbing. They are not provoked by physical activity and are not aggravated by it. Bed rest only focuses a woman's attention on pain. Sedatives help, nitroglycerin is ineffective. Rhythm disturbances are often paroxysmal in nature, do not depend on physical activity, and occur at any time; more often these are extrasystoles. Complaints of shortness of breath are nothing more than a feeling of lack of air, which a woman compensates by taking deep breaths. This feeling of lack of air can appear at any time, does not depend on physical activity and goes away when the patient’s attention is diverted. ECG changes may mimic small focal myocardial infarction or ischemic heart disease. A test with β-blockers (Inderal, Obzidan) 60-80 mg helps in diagnosis. Obzidan is taken orally on an empty stomach. An ECG is recorded before and after the test 1.5 hours later. With menopausal cardiopathy, noticeable positive ECG dynamics are observed, in contrast to coronary artery disease.
7. Genitourinary symptoms: itching, dyspareunia, atrophic colpitis, cystitis, bladder atony, distress, urinary incontinence. Symptoms of CS associated with urogenital atrophic processes continue for years, disabling patients due to the addition of urogenital infections. According to V.E. Balan [1], about 70% of women over 60 years old have urogenital symptoms. To eliminate it, long-term HRT (6-12 months) is required. Sexual desire in most women decreases with the onset of menopause, but for some it does not change and even increases. Very rarely hypersexuality develops, reaching the point of nymphomania. A combination of HRT and psychotropic medications helps treat this condition.
8. Changes in the skin and appendages: aging and dry skin, wrinkles, loss of elasticity, dryness and hair loss, brittle nails. The skin suffers from collagen loss, and for most women, these changes begin in the perimenopause and increase sharply during menopause. There is evidence that three years after the onset of menopause, a woman loses up to 30% of collagen and calcium in bone tissue. HRT restores calcium and collagen loss, which takes 3 to 5 years.
9. Metabolic disorders: progression of atherosclerosis, ischemic heart disease, frequent vascular accidents, myocardial infarction, stroke, osteoporosis (menopausal, senile). The process of resorption in trabecular bone tissue begins in women aged about 40 years, exceeding bone tissue formation by 0.5% per year, and accelerates 10 times with the onset of menopause, reaching 1-1.5% loss of total bone mass per year . Over 20 years of postmenopause, losses reach 50% for trabecular bone tissue and 30% for cortical bone. The positive effect of HRT on bone tissue was noted even when it was prescribed late (in persons over 65 years of age) [7]. A calcium-retaining effect is observed when using 0.5 mg of estradiol. In addition to HRT, the treatment complex should include vitamin D preparations (400-800 IU daily) and increase the daily calcium intake to 1200-1500 mg, especially for people over 70 years of age and those who spend little time in the sun. Physical activity and daily walks of 1.5-2 km also contribute to the deposition of calcium in bones, while smoking and alcohol aggravate osteoporosis. To prevent osteoporosis, hormone therapy should be started as early as possible and continued throughout life. There is convincing evidence of a 20-50% reduction in the incidence of strokes and myocardial infarction in those receiving HRT [4, 11]. The beneficial effect of estrogens on the lipid spectrum has been proven (increasing HDL and VLDL, decreasing LDL and VLDL). The permeability of arteries to lipid complexes decreases. Numerous studies have demonstrated the antioxidant effect of estrogens and their modulating effect on the immune system. There is evidence of the stabilizing effect of estrogens in arterial hypertension [6]. Many studies emphasize the vasodilatory and thrombolytic effects of estrogens. There are several dozen studies that have proven the beneficial effect of HRT on the cardiovascular system, and HRT is promising for the prevention of vascular accidents in women after 45 years of age [11]. However, hormone therapy cannot stop the progression of atherosclerosis and, according to available literature data, is not used for the primary prevention of coronary artery disease.
Gynecologists divide the clinical manifestations of CS into early (vasomotor, emotional and mental), mid-term (changes in the skin and appendages, urogenital) and late-term (osteoporosis, cardiovascular). CS can occur in any phase of the menopause. According to V.P. Smetnik [2], CS is observed in 37% of premenopausal women, 40% of menopausal women and 21% of postmenopausal women (after 1.5-2 years, and in 2% - after 3-5 years). Cases of symptoms of CS occurring 10 years after the onset of menopause have been described. The duration of CS is usually 1-2 years, but in 20-50% of women it lasts more than 5 years. Very rarely, CS bothers a woman for many years, sometimes weakening, sometimes intensifying, and rarely goes away without HRT. It largely depends on the personality type, social factors, family relationships and the woman’s attitude towards herself. There is no direct relationship between the severity of CS and the level of estrogen deficiency. Combinations of vegetative and cardiac, psychoemotional and other symptoms are possible. This chaos mimics other diseases and often contributes to misdiagnosis.
Differential diagnosis of CS
CS is often regarded as coronary artery disease with systolic arterial hypertension, diencephalic pathology, osteochondrosis of the thoracic and cervical spine with vertebrobasilar insufficiency syndrome. Menopausal cardiopathy is often mistaken for angina pectoris, and cardiac arrhythmias for ischemic heart disease and myocardial infarction. Myasthenic syndrome with insomnia is often mistaken for asthenoneurotic syndrome. Migraine-like headaches, when half of the head hurts for a week, are very difficult to diagnose.
Differential diagnosis is based on accurate knowledge of the clinical symptoms of CS, their characteristics in comparison with the patient’s age. Laboratory data are of great importance (FSH level, obzidan test, ECG dynamics, trial use of antipsychotics and sedatives). In some cases, the diagnosis of CS is quite complex and requires a careful history taking. The presence of symptoms in combination with “hot flashes”, the short duration of symptoms, and the frequent change of all possible combinations of them help in the diagnosis; in doubtful cases - a high level of FSH, 10-20 times higher than normal, in comparison with age, as well as relief of symptoms with sedative therapy.
In the treatment of CS, the only pathogenetic method of therapy is hormone replacement therapy with estrogen-gestagen drugs. All other methods are not pathogenetic and can only be used as auxiliary ones.
Today, despite the widespread use of HRT in the USA, Europe, and Southeast Asia, there is no convincing evidence that HRT using an estrogen-progestogen combination increases the risk of endometrial and breast cancer even after 20 years of its use [12]. At the same time, we can confidently state that hormone replacement therapy with estrogen-gestagen combinations without any particular risk of carcinogenesis for target organs can be used in the case of menopausal syndrome, as well as for the prevention of osteoporosis, vascular accidents and Alzheimer's disease. HRT provides an improvement in the quality of life of women during menopause and postmenopause, preventing the inevitable costs of atrophy of the genitourinary system, helping to maintain mental and intellectual integrity.
Contraindications for HRT:
- Malignant neoplasms of target organs (uterus, ovary, mammary gland).
- Uterine bleeding of unknown origin.
- Liver cirrhosis and other diseases accompanied by liver or kidney failure.
- Acute thrombosis and thrombophlebitis.
- Acute thromboembolic conditions and blood diseases.
- Diabetes mellitus with pronounced micro- and macroangiopathies.
Before carrying out HRT, a thorough examination of women is required to exclude oncological pathologies of the ovaries, uterus and mammary glands. A sonographic examination of the uterus, ovaries, and mammary glands is performed; blood pressure control, determination of body mass index, lipid profile, FSH level, preferably oncocytological examination of cervical mucus. Subsequently, every 6-12 months the examination is repeated with a mandatory consultation with a gynecologist. The thickness of the endometrium is determined. An endometrial thickness of up to 5 mm, as a rule, guarantees against dysfunctional uterine bleeding as a result of an overdose of estrogens, despite their combined use with gestagens. Pure estrogens without progestogen cover can only be used in women with a removed uterus.
Principles of HRT
For continuous hormone replacement therapy, only natural estrogens are used: estradiol, estrone and estriol. Of the estradiol preparations in European countries, the most commonly used is estradiol valerate (E2V) in doses of 1-2 mg/day or 17b-estradiol in a dose of 1 mg/day. Estrone is used in the form of conjugated estrogens in the form of the drug Premarin, where it is the main component along with equilin and 17-dihydroequilin (recommended dose - 0.625 mg / day). This drug is widely used in the United States, Latin America and Southeast Asia. Estriol for oral use is available in tablets of 1-2 mg, as well as in the form of creams and vaginal balls for topical use. Since the main goal of HRT is to obtain metabolic effects, and not endometrial proliferation, the principle of reducing the dose of both estrogenic components and gestagens should be adhered to. Recently, transdermal forms of administration of estrogens and gestagens have become popular. This excludes hepatic metabolism. The therapeutic dose was reduced to 0.05-0.1 mg/day. Transdermal administration in the form of patches and gels is convenient to use, estradiol is released more evenly, and its effect on coagulation is practically eliminated. However, there is an opinion that the oral route of estrogen administration is more effective for correcting the lipid spectrum. In the treatment of urogenital disorders, a local effect is easily achieved with the vaginal administration of suppositories with estriol.
Gestagens should be used in minimal doses to ensure secretory transformation of the endometrium. They are added to estrogens for 10-12 days to prevent estrogen-induced endometrial hyperplasia and the possible risk of its degeneration. Along with progesterone, its derivatives are used as gestagens: 20α- and 20β-dihydrosterone, 17α-hydroxyprogesterone, 19-nortestosterone derivatives (norethisterone acetate, levonorgestrel, gestodene). Orally administered gestagens, depending on the dose and structure, can interfere with the positive effect of estradiol on liver cells due to a partial androgenic effect. Natural progesterone has the least hepatocellular effect, and 19-nortestosterone derivatives have the greatest. Transdermal administration ensures minimal effects on liver cells.
In premenopause, therapy with only gestagens or estrogen-gestagen combinations in a cyclic mode can be used, in menopause (up to 55 years) - estrogen-gestagen combinations (in the same mode). However, clinicians do not have a consensus regarding treatment regimens. Preference is given to estrogen-gestagen combinations in menopause on a constant basis, eliminating the occurrence of menstrual-like reactions. In late postmenopause, estrogen-gestagen combinations are prescribed only on a continuous basis. Complex therapy for CS includes a diet that prevents the development of osteopenia (with Ca content up to 1200-1500 mg/day). Be sure to maintain sufficient physical activity for the same purposes. To more quickly normalize mental status, HRT is combined with the prescription of tranquilizers, sleeping pills or psychotropic drugs, depending on the severity of depression. Xanax (0.25 mg) is very effective, starting with two tablets in the morning and evening, increasing the dose every 2-3 days to 2 mg/day, course - 2-3 weeks; for sleep disturbances - chalcion 0.25-0.5 mg at night, course - 7-14 days; for anxiety conditions - fevarin (100 mg), starting with 1/4 tablet. per day, increasing the dose every 2-3 days to 100 mg/day, long-term, course - at least 6 weeks. The antidepressant lerivon (30 mg) is also effective long-term, 1/2 tablet. at night, course - 4-6 weeks.
Hormonal therapy for menopausal syndrome must continue for at least a year, otherwise its symptoms may return. For other purposes - prevention of osteoporosis, slowing down the aging process - the duration of HRT should be at least 5-7 years. Since the effect of not only sex hormones weakens with age, complex treatment should include thyroid hormones (50-100 mcg L-thyroxine, 8-16 units of growth hormone 1-2 times a week), melanotonin, DHEA, androgens (individually in each specific case). But such therapy is currently being developed. In the future, oral HRT preparations will most likely be replaced by transdermal forms (in the form of gels and creams). In the longer term, HRT will be combined with drugs that suppress the aging gene, which will allow women to maintain physical and mental activity into old age.
Literature
- Balan V.E., Smetnik V.P. Urogenital disorders in menopause. - M., 1998.
- Smetnik V.P., Kulakov V.I. Menopause Guide. - M., 2001.
- Amelsvoort T., Murphy D. // Gynecology Forum. - 1999. - V.4, N 2. - P.25-29.
- Falkeborn M. et al.// Arch. Intern. Med. - 1993.- V. 153. - P.1201.
- Gould E., Woolley CS, Frankfurt M., McEwen BS // J. Neurosci. - 1990. - V.10. — P.1286—1291.
- Hassager C., Christiansen C. // Maturitas. - 1988. - V. 9. - P.315.
- Lindsay R. // Lancet. - 1993. - N 341. - P.801.
- McKinlay SM et al. // Maturitas. - 1992. - V. 14. - P.103.
- Meldrun DR, Davidson BJ, Tarun IV, Judd HI // Obstet. Gynecol. - 1981. - V. 57. - P.626.
- Stampher MJ, Colditz GA // Prev. Med. - 1991. - V. 20. - P.47.
- Thompson SG, Meadle TV, Greenberg G. // J. Epidemiol. Comm. Health. - 1989. - V. 43. - P.173.
- Wingo PA, Layde PM, Zec NC et al. // JAMA. - 1987. - V.257. — P.209.
G.V. Kozyuk
Medical news. - 2004. - No. 7. — P. 48-54.