Editor: Andriyanov G.Yu., general practitioner, Ph.D. April, 2019.
Synonyms: hematocrit, hematocrit number, hematocrit value, Ht, Hct, Hematocrit.
The hematocrit number is the ratio of the red blood cell volume to the liquid amount of blood (i.e., the ratio of the volume of red blood cells to plasma). The determination of this indicator is included in the mandatory list for determining other indicators in a general blood test (CBC). Hematocrit measurement is not performed separately.
The hematocrit value is used to judge the thickness of the blood and its ability to transport oxygen.
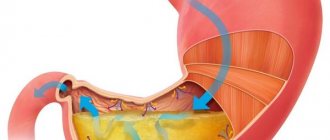
Photo: with a decrease in hematocrit value, the ratio of red blood cells to plasma volume decreases
Hematocrit - what is it, what does it depend on
Hematocrit analysis provides data on the ratio of the volume of red blood cells to the total volume of blood; sometimes this indicator refers to the ratio of the volume of all formed elements to the total volume. There is no particular difference between the interpretations; 99% of the blood cell volume is made up of red cells. More often, hematocrit is recorded as a percentage of the total volume, less often as a ratio of cell volume to total blood volume.
This indicator is determined as part of a general blood test complex. It is classified as secondary and is calculated based on data on the number of red blood cells. Occasionally, direct measurement of hematocrit is performed by centrifuging the sample. This procedure allows you to separate plasma from formed elements and directly measure this indicator.
Reasons for decreased hematocrit
Gestational period. Starting from the second trimester, the volume of circulating blood increases, but the number of red blood cells does not change.
Overhydration. Intravenous massive infusions lead to an increase in the volume of circulating blood, that is, to dilution of the blood, while the number of red blood cells remains the same.
Anemia of various origins. The lack of red blood cells naturally affects hematocrit values.
Intensive destruction of red blood cells. Occurs in the presence of hemolytic anemia of hereditary or acquired origin, in case of poisoning with hemolytic toxins (salts of heavy metals, consumption of toadstool) or serious infectious diseases (malaria, typhoid fever).
Blood loss (internal or external bleeding). Replenishment of circulating blood volume can be done quickly with crystalline or colloidal solutions. Restoration of lost red blood cells occurs only after a certain time or through blood transfusion.
Hyperproteinemia (increased total protein in the blood). This condition is observed in myeloma, lymphogranulomatosis, paraprotienemic hematoblastoses, diarrhea and vomiting. Excess protein in the blood draws fluids from the body into the bloodstream, increasing the volume of circulating blood while maintaining the same number of red blood cells.
A disorder of the formation of new red blood cells in the bone marrow. May be caused by blood diseases (anemia, leukemia), taking cytostatics and antitumor drugs, and renal paresis.
Tactics depending on the degree of reduction in the indicator:
- A decrease in hematocrit in the range of 35-30% requires outpatient observation by a doctor and changes in diet (increase consumption of meat, leafy greens, liver).
- When the hematocrit value decreases to 29-24%, iron supplements, B vitamins and folic acid are prescribed.
- If the rate drops to 13% or less, the condition is considered extremely serious and requires emergency hospitalization.
When the hematocrit decreases and anemia is detected in people over 65 years of age, the examination should be more thorough, since anemia in old age often accompanies serious diseases, for example, renal failure, hypo- or hyperthyroidism.
Indications and preparation for analysis
Indications for hematocrit analysis are symptoms indicating the development of anemia or other diseases of the blood or hematopoietic system. These include:
- Pale or jaundiced skin
- Enlarged spleen, liver
- Changes in the size of lymph nodes
- Digestive disorders
- Skin and hair problems (rashes, ulcers on mucous membranes, hair loss or brittleness)
In addition to identifying anemia, the analysis allows us to identify other diseases, for example, polycythemia (a chronic disease in which the bone marrow produces an excess amount of red blood cells) of various origins. This study is also used when it is necessary to assess the need for blood transfusion and calculate the required volume of transfusion.
No special preparation is required for the hematocrit test. It is necessary to follow the standard rules for conducting a general blood test:
- Blood is drawn early in the morning.
- You should not eat food 6-10 hours before the test.
- Avoid alcohol 2-3 days before the procedure.
Patients who smoke are advised to abstain from smoking for at least 2-3 hours before blood collection. If these recommendations are not followed, the analysis may give unreliable results. This is due to the fact that the composition of the blood is subject to strong fluctuations depending on the action of various environmental factors.
Indications
The appointment of an OAC, which includes a hematocrit study, is included in the standard patient examination plan and is mandatory:
- when undergoing a medical examination and/or medical examination;
- if any disease is detected or suspected by a clinic doctor;
- in preparation for planned surgery;
- during hospitalization (on the day of admission and on the eve of discharge).
Calculation of the hematocrit number is required for certain indications;
- blood clotting disorder;
- dehydration (dehydration);
- assessment of the degree of anemia (anemia), polycythemia (increase in blood cells);
- bleeding.
Blood test for hematocrit
The manipulation is performed in the morning, blood is taken from a vein or from a finger. At the Medart clinic, the most modern equipment is used for analysis, so the sampling is most often done from a vein.
To obtain the material, special vacuum containers (vacutainers) are used. This is a modern syringe replacement that provides a number of benefits for the patient:
- Virtually painless procedure.
- Minimum time to obtain the required amount of blood.
- Accurate calculation of the amount of reagent and blood.
- Minimum time for conducting the study and issuing results to the patient.
Modern technologies allow the procedure to be carried out as quickly as possible, without consequences for health.
Reasons for increasing hematocrit
Dehydration (dehydration). Loss of fluid due to repeated vomiting and/or diarrhea, sunstroke, burn disease, pathology of the digestive tract, intestinal obstruction, hyperhidrosis (excessive sweating), peritonitis leads to blood thickening due to an unchanged number of red blood cells.
Hypoxia. People suffering from diabetes, smokers, people located high in the mountains or in unventilated areas experience a lack of oxygen, which leads to the release of red blood cells into the bloodstream.
Cardiovascular pathology. Heart defects, coronary disease, and cardiovascular failure are accompanied by a lack of oxygen in the blood.
Bronchopulmonary pathology. Chronic hypoxia leads to: bronchial asthma, emphysema, obstructive bronchitis and other pulmonary diseases.
Neoplasms in the kidneys. Any kidney tumor provokes increased production of erythropoietin, which increases the formation of red blood cells.
Erythrocytosis. The pathology is characterized by increased production of red cells (true erythrocytosis) or redistribution of formed blood elements in some diseases (redistribution).
Erythremia. Refers to true erythrocytosis, synonymous with Vaquez-Osler disease. It is one of the variants of chronic leukemia.
Leukemia. Accompanied by an increase in white blood cells and a decrease in its liquid part.
Norms
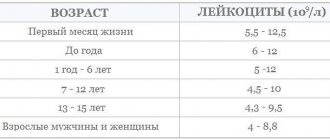
The normal hematocrit level depends on the age and gender of the person. For a mature woman it is 37-50%, for a man 34-45%. For newborns, this figure may be higher and ranges from 35 to 65%. As people grow older, the hematocrit decreases, reaching minimal levels in the elderly. This is the result of decreased bone marrow activity and decreased production of blood cellular elements.
A decrease in normal hematocrit in women is associated with regular blood loss during menstruation. High values in children are a manifestation of active processes in the development of red bone marrow and other hematopoietic organs.
It is important to consider that after massive blood losses and blood transfusions, determining the hematocrit level will give results with a large error. To reliably assess this indicator in such cases, it is necessary to wait a certain time.
It may take up to 3 months for complete physiological restoration of red blood cell levels to normal levels. This period is the life cycle of red blood cells, during which the cellular composition of the blood is renewed.
Hematocrit norms
| The newborn's hematocrit is increased | 50 ÷ 70%(0,5-0,7) |
| Newborn at one week old | 37 ÷ 49%(0,37-0,49) |
| In a baby at three months it decreases | 30 ÷ 36%(0,3-0,36) |
| In a child aged one year | 28÷ 45%(0,28-0,45) |
| In ten years | 36 ÷ 40% (0,36-0,4) |
| In adult women | 36 ÷ 46%(0,36-0,46) |
| In adult men | 38-50%(0,38-0,5) |
How is this indicator determined?
Hematocrit is determined simply: blood is drawn into a special test tube (its inner walls are treated with a substance that prevents clotting). The test tube is placed in a centrifuge, where red blood cells settle under the influence of centrifugal force. The blood is divided into two layers. A simple measurement of the lower column determines the hematocrit value.
The measurement of this indicator is included in the programs of all hematological analyzers produced by various companies. In such an analysis it will be designated NCT or PCV.
Hematocrit increased
An increase in the level of red blood cells detected in a hematocrit analysis may indicate various pathological conditions. The most common:
- Primary erythrocytosis. It occurs as a result of overactive production of red blood cells, including immature forms. May indicate the development of tumors in the bone marrow.
- Secondary erythrocytosis. Develops as a consequence of pathologies of the respiratory and cardiovascular systems (heart defects, respiratory failure).
- Reduced plasma volume. May indicate the development of peritonitis, leukemia, kidney disease. Often occurs with extensive burns, when blood plasma sweats through the damaged dermis.
- Dehydration. Observed in uncompensated diabetes mellitus, it can result from diarrhea, vomiting, excessive sweating and lack of fluid in the diet.
Erythrocytosis can develop in heavy smokers, especially if smoking has led to secondary damage to the respiratory system and heart. In this case, the body turns on mechanisms to compensate for insufficient oxygenation due to a significant increase in the number of red cells.
An increase in hematocrit is not always a consequence of disease. An increase in the number of red blood cells is considered normal for residents of mountainous areas and professional climbers. When exposed to high altitude conditions for a sufficiently long time, the body compensates for the lack of oxygen and atmospheric pressure by increasing the production of red blood cells.
Erythrocytosis is often asymptomatic and is discovered by chance during a blood test for other reasons. Only with a significant increase in hematocrit are the following observed:
- Pain in joints, muscles.
- Dyspnea.
- High blood pressure.
- Ringing in the ears and dizziness.
- Increased sweating, sleep disturbances.
These symptoms are not specific, so if such ailments occur, you should consult a doctor for further diagnosis.
To restore the physiological level of hematocrit, it is necessary to find out the reason that led to an increase in the amount of blood cells and eliminate it. For example, if erythrocytosis was caused by dehydration (lack of water in the body - dehydration), it is enough to restore the normal amount of fluid to normalize this indicator.
There is no need to self-medicate; only a specialist can accurately determine the cause of the increase in hematocrit and prescribe the correct diagnosis and treatment. Therefore, if there are any changes in the blood test, you should consult a specialist and strictly follow the recommendations received.
How does increased hematocrit manifest?
An increase in the specific gravity of red blood cells may not manifest itself in any way, or there may be individual, completely nonspecific symptoms:
- headache;
- dizziness;
- feeling of pressure in the head;
- dyspnea;
- fast fatiguability;
- skin itching;
- redness of the skin.
With such symptoms, a person may not see a doctor for a long time, but the problem may grow and lead to serious consequences.
See: Thick blood, Why I'm always cold, Complete blood count.
Reasons for the increase in children
The main ones are pediatric diseases. Whether it's scarlet fever, measles, rubella or chicken pox. The child’s body responds to all infectious processes by increasing the hematocrit level. This is normal, although this phenomenon does not always occur.
Correction is carried out by eliminating the underlying disease. Special measures are not needed.
An increase in hematocrit in a child means that septic processes may develop. Also, do not forget about the list presented above. Such diseases are possible not only in adults. Sometimes they occur in children.
How to measure
To measure hematocrit, a special graduated glass tube is used. To do this, it is filled with blood and centrifuged for an hour to separate plasma and cells. At the same time, red blood cells begin to settle to the bottom to a certain level, which is the result. Today, hardware methods are used for calculations - a hemolytic analyzer. When calculating Ht, RBC (absolute number of red blood cells) and MCV (average red cell volume) are taken as a basis. Even with minor blood loss, for example, during menstruation, it is not recommended to take the test, since Ht will be underestimated due to a compensatory increase in the amount of plasma.
How to increase and decrease Ht?
A decreased hematocrit is less common than an increased one. Treatment will depend on the causes of the decrease. That is, drugs are needed to eliminate the primary disease. If this is due to iron deficiency anemia, you should change your diet and include more foods containing iron in your menu. In addition, iron supplements are prescribed. All this will help increase the level of this indicator.
If both red blood cells and hematocrit are elevated, the question arises of lowering it. To do this, you can use the following tips:
- eat fewer foods that contain iron;
- drink more fluids, as dehydration increases this indicator;
- you should avoid alcohol and coffee, which have a diuretic effect and therefore lead to dehydration;
- eat grapefruit every day, which contains a flavonoid that leads to the natural disposal of red blood cells;
- There are foods rich in antioxidants, these include beans, prunes, and various berries.
Ht during pregnancy
During gestation, the hematocrit is usually low. The normal blood level in women is from 40 to 46%, while during pregnancy it decreases quite significantly - to 34%. There is no need to worry about this as it is considered normal in this condition. But if during pregnancy the hematocrit is even more reduced (up to 20-25%), anemia may develop, which means your health will worsen, weakness and malaise will appear. You cannot self-medicate; you must consult your doctor who will monitor the condition.
Increase factors in women
Growth is possible for several other specific reasons.
Menstrual cycle
Especially in the initial stage. When the hormonal background is not yet stable. The disorder develops spontaneously and disappears just as quickly.
We can say that the deviation is physiological and does not require special drug correction or other intervention.
In some cases - pregnancy in the initial phase
In the later stages of gestation, the opposite is true. And that's okay. As for the first trimester, there are options.
As with the menstrual cycle, no special measures are needed. Everything will recover on its own. Provided that the patient is relatively healthy and does not have the disorders described earlier.
Climax
Menopause is a hormonal imbalance caused by age. Hematocrit increases in women after 50 years of age due to the natural decline of reproductive function. Accompanied by pressure surges and changes in the blood picture.
If necessary, medications are prescribed to correct hormonal levels. Estrogens, taken orally.
What is hidden behind vegetative-vascular dystonia?
Iron deficiency
Diarrhea
Vomit
Thyrotoxicosis
22182 November 26
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vegetative-vascular dystonia: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
The term “vegetative-vascular dystonia” (VSD) is used by doctors to describe a number of symptoms indicating an imbalance of the autonomic nervous system, which can be observed in various diseases.
The autonomic nervous system is that part of the nervous system that regulates the functioning of internal organs, endocrine and exocrine glands, blood and lymphatic vessels. It maintains blood pressure, heart contractility, kidney function, is responsible for body temperature, regulates metabolic processes, etc.
The autonomic nervous system consists of the sympathetic and parasympathetic divisions, whose functions are mostly opposite. Thus, the influence of the sympathetic department of the autonomic nervous system leads to increased heart rate during physical exercise or emotional stress. Activation of the parasympathetic department occurs when a person is resting - blood pressure decreases and the pulse becomes slower.
In addition to the term “vegetative-vascular dystonia”, others are used that describe the same conditions - “neurocirculatory asthenia” or “neurocirculatory dystonia” (NCD).
In fact, VSD is not a disease, but a syndrome in which there is no organic pathology of a specific organ or system, and the disorders are functional in nature.
In our country, VSD remains one of the most popular diagnoses, while in 80% of cases there are serious pathologies behind it, the identification of which should be the attention of specialists. Note that abroad the diagnosis of “vegetative-vascular dystonia” is practically not heard.
The International Classification of Diseases, 10th revision (ICD-10) does not include such diagnoses as “VSD” and “NCD” and they are not assigned a separate code, and the ICD 11th revision proposes the term “Disorders of the autonomic nervous system” to designate functional disorders of the nervous system unspecified."
Symptoms of vegetative-vascular dystonia
Patients diagnosed with VSD, NCD, or somatoform dysfunction of the autonomic nervous system usually present with a wide range of complaints. They consult a doctor with symptoms such as a feeling of weakness, fatigue, rapid heartbeat or interruptions in heart function, increased or decreased blood pressure, periods of shortness of breath, increased anxiety, irritability, fearfulness, and may even experience fainting, pain or discomfort in the heart area , abdominal discomfort, dyspeptic disorders.
These complaints may hide a number of serious diseases (anemia, thyroid disease, arterial hypertension, coronary heart disease, panic attacks, depressive or anxiety disorder, etc.), which are easy to miss, explaining the patient’s symptoms by the fact that he has a disorder of the autonomic system. nervous system.
What diseases cause vegetative-vascular dystonia?
Iron-deficiency anemia
Iron deficiency anemia (IDA) is a disease characterized by a decrease in iron content in the blood serum, bone marrow and tissues and leading to disruption of the synthesis of hemoglobin and red blood cells, and the development of trophic disorders.
Latent iron deficiency is characterized by depletion of iron reserves in the body with normal blood hemoglobin levels. Symptoms of latent deficiency or anemia are weakness, increased fatigue, decreased performance, pale skin, headache, rapid heartbeat, low blood pressure, dry skin, brittle hair and nails, and abdominal discomfort.
Iron deficiency in anemia can be caused by a lack of iron intake, impaired absorption, or increased loss.
The main causes of IDA in women: heavy menstrual bleeding, pregnancy, childbirth (especially repeated ones) and lactation. For postmenopausal women and men, the main cause is bleeding in the gastrointestinal tract. Iron deficiency can develop during periods of intensive growth in children, when following a plant-based diet, after resection of the stomach or intestines, and also as a result of impaired iron absorption in people with inflammatory diseases of the gastrointestinal tract.
Thyroid diseases
Impaired production of thyroid hormones (thyroid hormones) can lead to their excess (hyperthyroidism) or deficiency (hypothyroidism) in the blood. With hypothyroidism, the patient feels apathy and drowsiness, fatigue, memory loss, has difficulty concentrating, depression, chilliness, does not tolerate cold well, has intense hair loss, brittle nails, swelling, muscle pain, weight gain with decreased appetite , constipation. With excessive production of hormones, patients complain of rapid heartbeat, tremors of the limbs, sweating, a feeling of heat and poor heat tolerance, tearfulness, fussiness and irritability, weight loss with increased appetite, insomnia.
Thyroid diseases can have a blurred clinical picture and occur under the masks of other diseases.
In some patients, neurological symptoms predominate, in others, blood pressure increases, in others, the leading symptoms are gastrointestinal disorders - nausea, flatulence, constipation.
A number of other somatic diseases, for example, arterial hypertension
or
coronary heart disease
, may also underlie complaints that the doctor regards as dysfunction of the autonomic nervous system (especially if the patient is young). When the examination does not reveal any organic abnormalities, and laboratory tests are within or borderline the norm, this does not mean that the patient is “inventing” his poor state of health.
Functional disorders of the nervous system can accompany such mental disorders as panic attacks, anxiety or depressive disorders, etc.
Panic disorder
Panic disorder is a common disease that tends to be protracted. It is 2-3 times more common in women and usually begins at a young age. The main manifestation of panic disorder is repeated attacks of anxiety, which are called panic attacks. A panic attack is an inexplicable, painful attack of poor health, which is accompanied by various vegetative symptoms, fear and anxiety. Previously, such patients were often diagnosed with “VSD with a crisis course” or “sympathoadrenal crisis.”
The presence of at least four of the following symptoms in patients should lead the doctor to think about a possible panic disorder (and in some cases, two are enough):
- pulsation, palpitations, rapid pulse;
- sweating;
- chills, tremors, feeling of internal trembling;
- feeling of lack of air, shortness of breath;
- choking or difficulty breathing;
- pain or discomfort in the left side of the chest;
- nausea or abdominal discomfort;
- feeling dizzy, unsteady, lightheaded, or lightheaded;
- a feeling of depersonalization and lack of understanding of the reality of what is happening;
- fear of going crazy or committing an uncontrollable act;
- fear of death;
- numbness or tingling sensation (paresthesia) in the limbs;
- sensation of waves of heat or cold passing through the body.
Other signs may include abdominal pain, upset bowel movements, frequent urination, a feeling of a lump in the throat, gait disturbance, visual or hearing impairment, cramps in the arms or legs, and motor dysfunction.
Anxiety during a panic attack can be both pronounced and barely noticeable - in this case, vegetative symptoms come to the fore. The duration of the attack is 15-30 minutes.
Panic disorder is characterized by the recurrence of panic attacks, it is not caused by the action of any substances or somatic disease (heart rhythm disturbance, thyrotoxicosis, hypertensive crisis), it is characterized by a person’s constant concern about the recurrence of attacks. Usually the first attack makes a painful impression on the patient, leading to constant anxiety and anticipation of repetitions. The more catastrophic a person assesses the first episode (for example, he believes that he is developing a heart attack or stroke), the more severe the panic disorder is and the faster concomitant diseases can join (depression, agoraphobia, alcoholism, etc.).
Generalized anxiety disorder
Generalized anxiety disorder (GAD) is widespread and persistent anxiety and tension that is not caused or limited by any environmental circumstances - so-called “free-floating anxiety.” Among the adult population, about 5% suffer from this disorder, most often women are patients. The disease usually appears between the ages of 20-35 years.
GAD can have a chronic course with periods of exacerbations and remissions. The anxiety state with GAD lasts at least 6 months, is not amenable to conscious control (the patient is not able to suppress anxiety through willpower or rational beliefs), and the intensity of the experience is disproportionate to the reality of life circumstances.
The main symptom of generalized anxiety disorder is diffuse anxiety that is not associated with specific situations, that is, the patient is constantly tense in anticipation of something bad, restless, and preoccupied for various reasons.
Other symptoms include irritability, increased vigilance, difficulty concentrating, and sensitivity to noise. The disease is characterized by muscle tension, which is accompanied by tremors of the limbs, inability to relax, increased muscle tone, headache, and aching muscle pain.
In generalized anxiety disorder, symptoms associated with increased activity of the autonomic nervous system are very common: dry mouth, difficulty swallowing food and water, abdominal discomfort, flatulence, diarrhea, nausea. Patients complain that it is difficult for them to breathe, they feel discomfort in the heart area, interruptions in its work, and pulsation of the neck vessels. In addition, a case of erectile dysfunction, decreased libido, delayed menstruation, and frequent urination has been described.
Depressive disorder
Depression is one of the most common mental disorders. Episodes of depression are characterized by daily low mood and last at least 2 weeks. The patient experiences decreased interest in work, family, and increased fatigue. A person in a depressive episode has difficulty concentrating, has low self-esteem, is pessimistic, and has problems with appetite and sleep.
Depression can occur in the so-called hidden form, when it is not a low mood that comes to the fore, but a feeling of physical ill health.
Patients complain of lack of strength, weakness, malaise, note the appearance of unpleasant sensations or pain in the body, rapid heartbeat, nausea, and increased sweating. In such cases, doctors prescribe a series of examinations and consultations, and if even minor deviations from the norm are detected, which are in no way related to the patient’s current condition, they begin to treat him. Incorrectly prescribed treatment does not lead to relief of the patient's condition, but can cause side effects and increase anxiety. It is these patients who are often diagnosed with “vegetative-vascular dystonia”, “spinal osteochondrosis”, “cardioneurosis”, etc. But if these patients come to see a psychiatrist, then usually the doctor immediately understands that he is a person with a depressive disorder and prescribes psychopharmacological treatment.
Diagnosis of vegetative-vascular dystonia
If you suspect a disorder of iron metabolism in the body, the following examinations must be carried out:
- general blood test with determination of hematocrit, level of red blood cells in the blood, study of the level of reticulocytes in the blood with determination of the average content and average concentration of hemoglobin in red blood cells, determination of the size of red blood cells;