Neupomax®
Neupomax® can be administered by daily subcutaneous (SC) injection or daily short (30-minute) intravenous (IV) infusion. The drug can also be administered as a 24-hour intravenous or subcutaneous infusion.
The choice of route of administration should depend on the specific clinical situation, but in most cases the subcutaneous route of administration is preferred.
To avoid pain during injection, it is best to change the injection site daily.
Standard cytotoxic chemotherapy regimens
5 mcg/kg body weight 1 time per day daily subcutaneously or intravenously for 30 minutes until, after the expected maximum decrease in the level of neutrophils, their number is restored to normal, upon reaching which the drug can be discontinued .
The first dose of Neipomax® should be administered no earlier than 24 hours after the end of the course of cytotoxic chemotherapy. Duration of therapy is up to 14 days. After induction and consolidation therapy for acute myeloid leukemia, the duration of use of Neipomax® may increase to 38 days, depending on the type, dose and chemotherapy regimen used.
Typically, a transient increase in the number of neutrophils is observed 1-2 days after the start of treatment with filgrastim. To achieve a stable therapeutic effect, interrupting treatment until normal neutrophil values are achieved after the expected maximum decrease in their level is not recommended. If the absolute number of neutrophils exceeds 10,000/μl, treatment with Neypomax® is stopped.
Myeloablative therapy followed by autologous or allogeneic bone marrow transplantation
The initial dose is 10 mcg/kg per day intravenously drip over 30 minutes or 24 hours, or as a 24-hour subcutaneous infusion.
The first dose of Neipomax® should be administered no earlier than 24 hours after cytotoxic chemotherapy, and in case of bone marrow transplantation - no later than 24 hours.
The duration of therapy is no more than 28 days. The daily dose of the drug is adjusted depending on the dynamics of neutrophil content. If the absolute neutrophil count is more than 1000/μl for three consecutive days, the dose of Neipomax® is reduced to 5 μg/kg/day. If, when using this dose for another 3 days in a row, the absolute number of neutrophils exceeds 1000/μl, the administration of Neipomax® is stopped. If during treatment the absolute number of neutrophils decreases to a level of less than 1000/μl, the dose of Neipomax® is increased again in accordance with the above scheme.
Mobilization of peripheral blood stem cells in patients with tumor diseases
10 mcg/kg 1 time per day subcutaneously or by continuous 24-hour subcutaneous infusion for 6 consecutive days. In this case, 2 leukapheresis are usually performed in a row, on the 5th and 6th days. In case of additional leukapheresis, the administration of Neipomax should be continued until the last leukapheresis.
Mobilization of PSCC after myelosuppressive chemotherapy
5 mcg/kg per day by daily subcutaneous injection, starting from the first day after completion of chemotherapy until the number of neutrophils reaches normal values.
Leukapheresis should only be performed when the absolute neutrophil count exceeds normal values (> 2000/µl).
Mobilization of PSCCs from healthy donors for allogeneic transplantation
10 mcg/kg/day subcutaneously for 4-5 days and 1 or 2 leukapheresis usually allows to obtain more than 4x106CD34+ cells/kg body weight of the recipient.
There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 and over 60 years of age.
Severe chronic neutropenia (SCN)
Neipomax® is prescribed at an initial dose of 12 mcg/kg/day for congenital neutropenia and 5 mcg/kg/day for idiopathic or periodic neutropenia, subcutaneously once or by multiple injections daily until the neutrophil count consistently exceeds 1500/mcL. After achieving a therapeutic effect, the minimum effective dose is determined to maintain this level. After 1-2 weeks of treatment, the initial dose can be doubled or halved, depending on the patient's response to therapy. Subsequently, individual dose adjustments can be made every 1-2 weeks to maintain the average neutrophil count in the range of 1500-10000/μl. In patients with severe infections, a more rapid dose escalation regimen may be used. The safety of filgrastim in long-term treatment of patients with SCN with doses greater than 24 mcg per day has not been established.
Neutropenia in HIV infection
The initial dose is 1-4 mcg (0.1-0.4 million IU)/kg subcutaneously 1 time per day until the number of neutrophils normalizes. The maximum daily dose should not exceed 10 mcg/kg. After achieving a therapeutic effect, it is recommended to use Neipomax® in a maintenance dose: 300 mcg subcutaneously every other day. Subsequently, doses are adjusted on a case-by-case basis to maintain an average neutrophil count greater than 2000/µl.
Application in pediatric practice
Dosing recommendations for pediatric patients are the same as for adults.
Elderly patients, patients with impaired renal or hepatic function
No dose adjustment of Neypomax® is required.
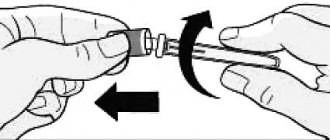
Breeding instructions
When administered subcutaneously
The drug should not be further diluted.
When preparing a solution for infusion
Neipomax® is diluted with only 5% dextrose solution. Dilution with 0.9% sodium chloride solution is not allowed (pharmaceutical incompatibility).
Neipomax® in diluted form at a concentration of 2 to 15 μg/ml can be adsorbed by glass and plastics. In this case, to prevent absorption, it is necessary to add human serum albumin to the solution in the required amount to achieve its concentration in the final solution of 2 mg/ml. For a diluted solution of Neipomax® at a concentration of more than 15 mcg/ml, the addition of albumin is not required.
Neipomax® cannot be diluted to a concentration of less than 2 mcg/ml.
Content
- Characteristics of Neipomax (vial 30mln/ml 1ml No. 5)
Composition: Bottle 1 ml Filgrastim 30 million.
ED (300 mcg).
Excipients: glacial acetic acid, sodium hydroxide, sorbitol, polysorbate 80, water for injection.
Solution for intravenous and subcutaneous administration in the form of a clear or slightly opalescent, colorless or slightly colored liquid.
Pharmacological Action: Filgrastim is a recombinant human granulocyte colony-stimulating factor (G-CSF).
It has biological activity similar to endogenous human G-CSF, differing from the latter in that it is a non-glycosylated protein with an additional N-terminal methionine residue.
Filgrastim, produced using recombinant DNA technology, is isolated from the cells of the bacterium Escherichia coli, into the genetic apparatus of which the gene encoding the G-CSF protein has been introduced.
Filgrastim stimulates the formation of functionally active neutrophils, their release into the peripheral blood from the bone marrow and is used in the treatment of patients with neutropenia of various origins.
Method of Administration: Neipomax® can be administered by daily subcutaneous injections or daily short 30-minute IV infusions.
The drug can also be administered as an intravenous or subcutaneous 24-hour infusion.
The choice of route of administration should depend on the specific clinical situation, however, in most cases, subcutaneous administration of the drug is preferable.
To avoid pain during injection, you should change the injection site daily.
Standard regimens of cytotoxic chemotherapy The drug should be prescribed at a dose of 5 mcg/kg 1 time/day daily subcutaneously or intravenously for 30 minutes until, after the expected maximum decrease in the level of neutrophils, their number is restored to normal.
When the norm is reached, the drug can be discontinued.
The first dose of Neipomax should be administered no earlier than 24 hours after the end of the course of cytotoxic chemotherapy.
The duration of therapy is no more than 14 days.
After induction and consolidation therapy for acute myeloid leukemia, the duration of use of Neipomax can be increased to 38 days, depending on the type, dose and chemotherapy regimen used.
A transient increase in the number of neutrophils is usually observed 1-2 days after the start of treatment with filgrastim.
To achieve a stable therapeutic effect, it is not recommended to interrupt treatment until normal neutrophil values are achieved after the expected maximum decrease in their level.
When the absolute number of neutrophils is >10,000/μl, treatment with Neypomax is stopped.
Myeloablative therapy followed by autologous or allogeneic bone marrow transplantation The initial dose of the drug is 10 mcg/kg/day intravenously over 30 minutes or 24 hours, or by 24-hour subcutaneous infusion.
The first dose of Neipomax should be administered no earlier than 24 hours after cytotoxic chemotherapy, and in case of bone marrow transplantation - no later than 24 hours.
The duration of therapy is no more than 28 days.
The daily dose of the drug is adjusted depending on the dynamics of neutrophil content.
If the absolute neutrophil count exceeds 1000/μl for 3 consecutive days, the Neipomax dose is reduced to 5 mcg/kg/day; if, when using this dose over the next 3 days, the absolute neutrophil count continues to exceed 1000/μl, the administration of Neipomax should be discontinued.
If during treatment the absolute number of neutrophils decreases to a level of less than 1000/μl, the dose of Neipomax should be increased again, in accordance with the above scheme.
Mobilization of peripheral blood stem cells in patients with tumor diseases The drug should be used at a dose of 10 mcg/kg 1 time/day subcutaneously or administered by continuous 24-hour subcutaneous infusion for 6 consecutive days.
In this case, 2 leukapheresis are usually performed in a row, on the 5th and 6th days.
In case of additional leukapheresis, the administration of Neipomax should be continued until the last leukapheresis.
Mobilization of PSCC after myelosuppressive chemotherapy The drug should be used at a dose of 5 mcg/kg per day by daily subcutaneous injections, starting from the first day after completion of chemotherapy until the number of neutrophils reaches normal values.
Leukapheresis should only be performed when the absolute neutrophil count exceeds the normal value (>2000/µl).
Mobilization of PSCC in healthy donors for allogeneic transplantation. Using the drug at 10 mcg/kg/day subcutaneously for 4-5 days and performing 1-2 leukapheresis usually allows one to obtain CD34+>4x106 cells/kg body weight of the recipient.
Severe chronic neutropenia (SCN)Neipomax® should be used at an initial dose of 12 mcg/kg/day for congenital neutropenia and 5 mcg/kg/day for idiopathic or intermittent neutropenia subcutaneously once or by several injections daily until the number of neutrophils will not consistently exceed 1500/µl.
After achieving a therapeutic effect, the minimum effective dose is determined to maintain this level.
After 1-2 weeks of treatment, the initial dose can be doubled or halved, depending on the patient's response to therapy.
Subsequently, individual dose adjustments can be made every 1-2 weeks to maintain the average neutrophil count in the range of 1500-10,000/μl.
In patients with severe infections, a more rapid dose escalation regimen may be used.
The safety of filgrastim in long-term treatment of patients with SCN with doses greater than 24 mcg/kg/day has not been established.
Neutropenia in HIV infection The initial dose of the drug is 1-4 mcg (0.
1-0.
4 million
U)/kg s.c. 1 time/day until the number of neutrophils normalizes.
The maximum daily dose should not exceed 10 mcg/kg.
After achieving a therapeutic effect, it is recommended to use Neipomax® in a maintenance dose - 300 mcg subcutaneously every other day.
Further dosing regimen is adjusted in each individual case separately to maintain the average neutrophil count >2000/μl.
Recommendations for dosage regimens for children correspond to those for adults.
There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 years of age.
Patients with impaired renal and/or liver function, as well as elderly patients, do not require adjustment of the Neipomax dosage regimen.
There are no data on the safety and effectiveness of filgrastim in healthy donors over 60 years of age.
Rules for preparing solutions When administered subcutaneously, the drug should not be further diluted.
When preparing a solution for infusion, it is recommended to use only 5% dextrose solution as a solvent.
Dilution 0.
9% sodium chloride solution is not allowed due to pharmaceutical incompatibility.
Neipomax® in diluted form at a concentration of 2 to 15 μg/ml can be adsorbed by glass and plastic materials.
In this case, to prevent absorption, it is necessary to add human serum albumin in the required amount to the drug solution to achieve its concentration in the final solution of 2 mg/ml.
For a diluted solution of Neipomax at a concentration of more than 15 μg/ml, the addition of albumin is not required.
Neipomax® should not be diluted to a concentration of less than 2 mcg/ml.
Interaction: The safety and effectiveness of administering filgrastim on the same day as myelosuppressive anticancer drugs has not been established.
There are isolated reports of increased neutropenia with simultaneous administration of filgrastim and 5-fluorouracil.
There is currently no data on possible interactions with other hematopoietic growth factors and cytokines.
Lithium, which stimulates the release of neutrophils, may enhance the effect of filgrastim.
Pharmaceutical interactionsDilution 0.
9% sodium chloride solution is not allowed due to pharmaceutical incompatibility.
Side Effects: From the musculoskeletal system: pain in bones, muscles and joints, osteoporosis.
From the digestive system: anorexia, diarrhea, hepatomegaly, nausea, vomiting.
From the hematopoietic system: neutrophilia, leukocytosis (as a consequence of the pharmacological action of filgrastim), anemia, thrombocytopenia, enlargement and rupture of the spleen.
From the respiratory system: adult respiratory distress syndrome, infiltrates in the lungs.
From the cardiovascular system: decrease or increase in blood pressure, skin vasculitis, tachycardia.
From laboratory parameters: reversible increase in the content of LDH, alkaline phosphatase, GGT, uric acid, transient hypoglycemia after meals; very rarely - proteinuria, hematuria.
Allergic reactions: skin rash, urticaria, facial swelling, wheezing, shortness of breath.
Other: headache, fatigue, general weakness, nosebleeds, petechiae, erythema nodosum.
Filgrastim does not increase the incidence of adverse reactions to cytotoxic therapy.
Contraindications: - severe congenital neutropenia (Kostmann syndrome) with cytogenetic disorders; - use of the drug to increase doses of cytotoxic chemotherapeutic drugs in excess of the recommended doses; - hypersensitivity to filgrastim or other components of the drug.
The drug should be used with caution in case of malignant and precancerous diseases of a myeloid nature (incl.
h.
acute myeloid leukemia), sickle cell anemia.
Use during pregnancy and breastfeeding Category C drug.
The safety of filgrastim during pregnancy has not been established, therefore, when prescribing the drug to pregnant women, the expected benefit to the mother should be weighed against the potential risk to the fetus.
It is not known whether filgrastim is excreted in breast milk.
The use of filgrastim during breastfeeding is not recommended.
Use in children: Recommendations for dosage regimens for children correspond to those for adults.
There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 years of age. The safety and effectiveness of the drug in newborns have not been established.
Overdose: The consequences of an overdose of Neipomax are unknown.
1-2 days after discontinuation of the drug, the number of circulating neutrophils usually decreases by 50%, with a return to normal after 1-7 days.
Special Instructions: Treatment with Neypomax should only be carried out under the supervision of a physician experienced in the use of CSF and with the necessary diagnostic capabilities.
Cell mobilization and apheresis procedures should be performed in specialized medical institutions.
The safety and effectiveness of filgrastim in patients with myelodysplastic syndrome and chronic myeloid leukemia have not been established, and therefore the use of filgrastim in these diseases is not recommended.
Particular attention should be paid to the differential diagnosis between acute myeloid leukemia and blast crisis of chronic myeloid leukemia.
Before prescribing Neipomax to patients with SCN, differential diagnosis should be carefully carried out to exclude other hematological diseases, such as aplastic anemia, myelodysplasia and chronic myeloid leukemia (morphological and cytogenetic analysis of the bone marrow should be performed before starting therapy).
When filgrastim was used in patients with SCN, cases of myelodysplastic syndrome and acute myeloid leukemia were observed.
Despite the fact that the connection between the occurrence of these diseases and the use of filgrastim has not been established, the drug should be used with caution in SCN under the supervision of morphological and cytogenetic analysis of the bone marrow (once every 12 months).
If cytogenetic abnormalities appear in the bone marrow, the risk-benefit ratio of further filgrastim therapy should be carefully assessed.
If myelodysplastic syndrome or leukemia develops, Neipomax should be discontinued.
Treatment with Neypomax should be carried out under regular monitoring of a complete blood count with counting the leukocyte formula and platelet count (before starting therapy and then 2 times a week with standard chemotherapy and at least 3 times a week with mobilization of PSCC with or without subsequent bone marrow transplantation).
When using Neipomax to mobilize PSCC, the drug is discontinued if the number of leukocytes exceeds 1x105/μl.
If the platelet count is stable and does not exceed 1x105/μl, it is recommended to temporarily discontinue filgrastim therapy or reduce the dose of the drug.
Filgrastim does not prevent thrombocytopenia and anemia caused by myelosuppressive chemotherapy.
During treatment with Neypomax, urine tests should be performed regularly (to exclude hematuria and proteinuria) and the size of the spleen should be monitored.
Filgrastim should be used with caution in patients with sickle cell disease due to the potential for a significant increase in the number of sickle cells.
The safety and effectiveness of the drug in patients with autoimmune neutropenia have not been established.
Patients with bone pathology and osteoporosis receiving continuous treatment with Neypomax for more than 6 months require monitoring of bone density.
The effect of filgrastim on graft-versus-host disease has not been established.
Use in pediatrics Recommendations for dosage regimens for children correspond to those for adults.
There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 years of age.
The safety and effectiveness of the drug in newborns have not been established.
Storage conditions: Cold +5
NEUPOMAX RR D/V/V AND S/C INTRODUCTION. 30 MILLION UNITS/ML 480 MCG/1.6 ML No. 5
Directions for use and doses
Neupomax can be administered by daily subcutaneous (SC) injections or daily short (30-minute) intravenous (IV) infusions.
The drug can also be administered as a 24-hour intravenous or subcutaneous infusion. The choice of route of administration should depend on the specific clinical situation, but in most cases the subcutaneous route of administration is preferred.
To avoid pain during injection, it is best to change the injection site daily.
Standard cytotoxic chemotherapy regimens
5 mcg/kg body weight 1 time per day daily subcutaneously or intravenously for 30 minutes until, after the expected maximum decrease in the level of neutrophils, their number is restored to normal, upon reaching which the drug can be discontinued .
The first dose of Neipomax should be administered no earlier than 24 hours after the end of the course of cytotoxic chemotherapy. Duration of therapy is up to 14 days. After induction and consolidation therapy for acute myeloid leukemia, the duration of use of Neipomax may increase to 38 days, depending on the type, dose and chemotherapy regimen used.
Typically, a transient increase in the number of neutrophils is observed 1-2 days after the start of treatment with filgrastim. To achieve a stable therapeutic effect, interrupting treatment until normal neutrophil values are achieved after the expected maximum decrease in their level is not recommended. When the absolute number of neutrophils exceeds l0000/μl, treatment with Neypomax is stopped.
Myeloablative therapy followed by autologous or allogeneic bone marrow transplantation
The initial dose is 10 mcg/kg per day intravenously drip over 30 minutes or 24 hours, or as a 24-hour subcutaneous infusion.
The first dose of Neipomax should be administered no earlier than 24 hours after cytotoxic chemotherapy, and in case of bone marrow transplantation - no later than 24 hours.
The duration of therapy is no more than 28 days. The daily dose of the drug is adjusted depending on the dynamics of neutrophil content. If the absolute neutrophil count is more than 1000/μl for three consecutive days, the dose of Neipomax is reduced to 5 μg/kg/day. If, when using this dose for another 3 days in a row, the absolute number of neutrophils exceeds 1000/μl, the administration of Neipomax is stopped. If during treatment the absolute number of neutrophils decreases to a level of less than 1000/μl, the dose of Neipomax is increased again, in accordance with the above scheme.
Mobilization of peripheral blood stem cells in patients with tumor diseases
10 mcg/kg 1 time per day subcutaneously or by continuous 24-hour subcutaneous infusion for 6 consecutive days. In this case, 2 leukapheresis are usually performed in a row, on the 5th and 6th days. In case of additional leukapheresis, the administration of Neipomax should be continued until the last leukapheresis.
Mobilization of PSCC after myelosuppressive chemotherapy
5 mcg/kg per day by daily subcutaneous injection, starting from the first day after completion of chemotherapy until the number of neutrophils reaches normal values.
Leukapheresis should only be performed when the absolute neutrophil count exceeds normal values (> 2000/µl).
Mobilization of PSCCs from healthy donors for allogeneic transplantation
10 mcg/kg/day subcutaneously for 4-5 days and 1 or 2 leukapheresis usually allows one to obtain more than 4x106 CD34+ cells/kg body weight of the recipient. There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 and over 60 years of age.
Severe chronic neutronenia (SCN)
Neipomax is prescribed at an initial dose of 12 mcg/kg/day for congenital neutropenia and 5 mcg/kg/day for idiopathic or periodic neutropenia, subcutaneously once or by multiple injections daily until the neutrophil count consistently exceeds 1500/mcL. After achieving a therapeutic effect, the minimum effective dose is determined to maintain this level. After 1-2 weeks of treatment, the initial dose can be doubled or halved, depending on the patient's response to therapy. Subsequently, individual dose adjustments can be made every 1-2 weeks to maintain the average neutrophil count in the range of 1500-10000/μl. In patients with severe infections, a more rapid dose escalation regimen may be used. The safety of filgrastim in long-term treatment of patients with SCN with doses greater than 24 mcg per day has not been established.
Neutronia in HIV infection
The initial dose is 1-4 mcg (0.1 - 0.4 million units)/kg subcutaneously 1 time per day until the number of neutrophils normalizes. The maximum daily dose should not exceed 10 mcg/kg. After achieving a therapeutic effect, it is recommended to use Neipomax in a maintenance dose: 300 mcg subcutaneously every other day. Subsequently, doses are adjusted on a case-by-case basis to maintain an average neutrophil count greater than 2000/µl.
Application in pediatric practice
Dosing recommendations for pediatric patients are the same as for adults.
Elderly patients, patients with impaired renal or hepatic function
No dose adjustment of Neypomax is required.
Breeding instructions
When administered subcutaneously, the drug should not be further diluted.
When preparing a solution for infusion, Neipomax is diluted with only 5% dextrose solution. Dilution with 0.9% sodium chloride solution is not allowed (pharmaceutical incompatibility).
Neipomax in diluted form at a concentration of 2 to 15 mcg/ml can be adsorbed by glass and plastics. In this case, to prevent absorption, it is necessary to add human serum albumin to the solution in the required amount to achieve its concentration in the final solution of 2 mg/ml. For a diluted solution of Neipomax at a concentration of more than 15 μg/ml, the addition of albumin is not required.
Neipomax cannot be diluted to a concentration of less than 2 mcg/ml.