Metformin Long Ozone TB prolongir released 500 mg N 60
Active substance:
Metformin*
Indications
Type 2 diabetes mellitus in adults, especially in obese patients, with ineffective diet therapy and exercise:
as monotherapy;
in combination with other oral hypoglycemic agents or insulin.
Directions for use and doses
Inside. The tablets are swallowed whole, without chewing, with a sufficient amount of liquid, 1 time per day during or after dinner.
The dose of the drug is set by the doctor individually for each patient based on the results of measuring the concentration of glucose in the blood.
Monotherapy and combination therapy in combination with other hypoglycemic agents
Recommended dose:
for tablets with a dosage of 1000 mg - 1 tablet (1000 mg) 1 time per day during or after dinner.
For tablets with a dosage of 850 mg - 2 tablets (1700 mg) 1 time per day.
If adequate glycemic control cannot be achieved while taking the recommended dose, the dose may be increased to the maximum.
Maximum recommended dose:
for tablets with a dosage of 850 mg - 3 tablets 1 time per day (2550 mg);
for tablets with a dosage of 1000 mg - 2 tablets 1 time per day (2000 mg).
If adequate glycemic control is not achieved when taking the maximum recommended dose once daily, the maximum dose (for Metformin Long 1000 mg) may be divided into two doses: one 1000 mg tablet with breakfast and one 1000 mg tablet at breakfast. dinner time. If adequate glycemic control is not achieved in this case, a switch to regular-release metformin with a maximum daily dose of 3000 mg is possible.
For patients not taking metformin, the recommended starting dose of metformin extended-release is 500 mg (similar drugs are available in the indicated dosage) or 850 mg of Metformin Long once daily with dinner. Every 10-15 days it is recommended to adjust the dose based on the results of measuring blood glucose concentrations. Slowly increasing the dose promotes better gastrointestinal tolerability.
In case of switching from another hypoglycemic agent, dose selection is carried out as described above, starting with the administration of extended-release metformin at a dose of 500 mg (similar drugs are available in the indicated dosage) or 850 mg of Metformin Long with a possible subsequent transition to Metformin Long at a dosage of 1000 mg .
Metformin Long is prescribed as maintenance therapy to patients taking metformin in the form of regular-release tablets at a dose of 1000 mg or 2000 mg. To switch to an extended-release formulation, the daily dose should be equivalent to the daily dose of regular-release metformin. Patients taking metformin in the form of regular-release tablets at a dose exceeding 2000 mg are not recommended to switch to Metformin Long.
Combination with insulin
To achieve better glycemic control, metformin and insulin can be used in combination therapy. The usual starting dose of metformin extended-release is 500 mg (similar drugs are available in the indicated dosage) or 850 mg of Metformin long once a day with dinner, while the dose of insulin is adjusted based on the results of measuring blood glucose concentrations. Next, it is possible to switch to the drug Metformin Long at a dosage of 1000 mg.
Patients with kidney failure
Metformin can be used in patients with moderate renal failure (creatinine clearance 45 - 59 ml/min) only in the absence of standing, which may increase the risk of developing lactic acidosis.
The initial dose of extended-release metformin is 500 mg (similar drugs are available in the indicated dosage) or 850 mg of Metformin Long once a day. The maximum dose is 1000 mg per day.
Renal function should be carefully monitored every 3-6 months.
If creatinine clearance is below 45 ml/min, the drug should be discontinued immediately.
Elderly patients
For elderly patients, the dose is adjusted based on assessment of renal function, which should be performed regularly (see "Special Instructions").
Duration of treatment
Metformin Long should be taken daily, without interruption. If treatment is stopped, the patient must inform the doctor.
Missing a dose
If a dose is missed, the patient should take the next dose at the usual time. You should not take a double dose of Metformin Long.
Before use, consultation with a specialist is required.
The method of administration and dosage regimen of a particular drug depend on its release form and other factors. The optimal dosage regimen is determined by the doctor.
Storage mode, interactions and side effects are indicated in the instructions
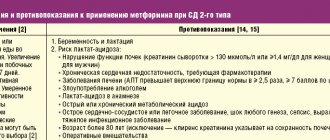
Contraindications
hypersensitivity to metformin or to any excipient;
diabetic ketoacidosis, diabetic precoma, coma;
renal failure (creatinine clearance less than 45 ml/min);
acute conditions with a risk of developing renal dysfunction: dehydration (with chronic or severe diarrhea, repeated bouts of vomiting), severe infectious diseases (for example, respiratory tract infections, urinary tract infections), shock;
clinically pronounced manifestations of acute or chronic diseases that can lead to the development of tissue hypoxia (including cardiac or respiratory failure, acute myocardial infarction);
extensive surgical operations and injuries, when insulin therapy is indicated (see section “Special Instructions”);
liver failure, liver dysfunction;
chronic alcoholism, acute alcohol poisoning;
pregnancy;
lactic acidosis (including history);
use within less than 48 hours before and within 48 hours after radioisotope or x-ray studies with the introduction of iodine-containing contrast agent (for example, intravenous urography, angiography) (see section “Interaction with other drugs”);
following a hypocaloric diet (less than 1000 kcal/day);
lactose intolerance, lactase deficiency, glucose-galactose malabsorption;
children under 18 years of age due to the lack of clinical data on use.
Carefully
Use the drug:
the risk of developing lactic acidosis;
in patients with renal failure (creatinine clearance 45 - 59 ml/min);
during breastfeeding.
Metformin long, 30 pcs., 750 mg, extended-release film-coated tablets
Lactic acidosis
Lactic acidosis is a rare but serious complication (high mortality if not treated promptly) that may occur due to accumulation of metformin. Cases of lactic acidosis when taking metformin occurred mainly in patients with diabetes mellitus with severe renal failure.
Other associated risk factors, such as decompensated diabetes mellitus, ketosis, prolonged fasting, alcoholism, liver failure and any condition associated with severe hypoxia, should be considered, which may help reduce the incidence of lactic acidosis.
The risk of developing lactic acidosis should be taken into account when nonspecific signs appear, such as muscle cramps accompanied by dyspeptic disorders, abdominal pain and severe asthenia. Lactic acidosis is characterized by severe malaise with general weakness, acidotic shortness of breath, vomiting, abdominal pain, muscle cramps and hypothermia followed by coma. Diagnostic laboratory parameters are a decrease in blood pH (less than 7.25), lactate content in the blood plasma over 5 mmol/l, increased anion gap and lactate/pyruvate ratio. If lactic acidosis is suspected, stop taking the drug and consult a doctor immediately.
The use of iodine-containing radiocontrast agents
Intravascular administration of iodinated radiocontrast agents can lead to the development of renal failure and accumulation of metformin, which increases the risk of developing lactic acidosis. Metformin should be discontinued, depending on renal function, 48 hours before or during an X-ray examination using iodinated contrast agents, and not resumed until 48 hours after it, provided that during the examination, renal function was found to be normal.
Surgical operations
The use of metformin should be discontinued 48 hours before elective surgery and can be continued no earlier than 48 hours after, provided that renal function has been found to be normal during the examination.
Kidney function
Since metformin is excreted by the kidneys, before starting treatment and regularly thereafter, it is necessary to determine QC:
- at least once a year in patients with normal renal function;
- at least 2-4 times a year in elderly patients, as well as in patients with CC at the lower limit of normal.
In the case of CC less than 45 ml/min, the use of the drug is contraindicated.
Particular caution should be exercised in case of possible impairment of renal function in elderly patients, with simultaneous use of antihypertensive drugs, diuretics or non-steroidal anti-inflammatory drugs.
Heart failure
Patients with heart failure have a higher risk of developing hypoxia and renal failure. Patients with chronic heart failure should have cardiac and renal function monitored regularly while taking metformin. Taking metformin in heart failure with unstable hemodynamic parameters is contraindicated.
Other Precautions
Patients are advised to continue to follow a diet with even carbohydrate intake throughout the day. Overweight patients are advised to continue to follow a low-calorie diet (but not less than 1000 kcal/day). Patients should also exercise regularly.
Patients should inform their physician about any treatment they are undergoing and any infectious diseases such as colds, respiratory tract infections, or urinary tract infections.
It is recommended that routine laboratory tests be performed regularly to monitor diabetes mellitus.
Metformin does not cause hypoglycemia when used alone, but caution is recommended when used in combination with insulin or other hypoglycemic agents (for example, sulfonylurea derivatives or repaglinide, etc.). Symptoms of hypoglycemia include weakness, headache, dizziness, increased sweating, rapid heartbeat, blurred vision, or difficulty concentrating.
Questions about the use of the drug for various diseases and conditions
In recent years, clinicians have been talking a lot about the possibilities of using metformin for patients suffering from NAFLD. In addition, it has been successfully prescribed to women with polycystic ovary syndrome for the purpose of ovulation induction. In this case, it is used as an independent remedy or combined with clomiphene.
If we compare the effect of metformin with the effect of other drugs that lower sugar levels, it has a much stronger anti-cancer potential, inhibiting the proliferation of pathological cells that form in the mammary glands in women and in the prostate in men. In order to evaluate this effect of metformin more objectively, further research is necessary.
Metformin as an effective drug of the biguanide class
Biguanides have been used in medicine for a long time - at least 50 years. They effectively fight insulin resistance, which is the main pathogenetic mechanism in the development of diabetes. The drug metformin has established itself as the safest medicine, which is recommended by almost all the world's leading experts.
If a patient is diagnosed with new-onset type 2 diabetes, prescribing metformin is the first step the clinician should take when prescribing treatment. It is a first-line drug.
The mechanism of action of metformin is to reduce the body's resistance to insulin. Since the post-receptor mechanisms of insulin function are disrupted as a result of the pathological process, the task of the drug is to restore this function with the implementation of important therapeutic effects:
- liver cells begin to absorb glucose more intensively, as do muscle and fat cells. Thanks to this, the number and activity of glucose transporters (1,3 and 4) are restored;
- the liver does not produce glucose as quickly, since the process of gluconeogenesis itself is reduced. This is due to inhibition of lipid oxidation;
- the intestinal mucosa begins to utilize glucose more intensively;
- in the portal vein there is a decrease in the level of glucose concentration.
As a result, fasting glucose also becomes lower, with a decrease in the need for insulin secretion.
Metformin has not only antihyperglycemic properties. Numerous studies have revealed a number of its beneficial therapeutic properties:
- reducing the risk of overall deaths;
- reducing the risk of cardiovascular complications;
- beneficial effect on fat metabolism with a decrease in VLDL and triglycerides in the blood plasma;
- decreased platelet aggregation (sticking together);
- antiatherosclerotic effect.
An anorexigenic effect has also been identified, promoting weight loss.
The problem of insulin resistance in T2DM
The main pathogenetic link of T2DM is the body's resistance to insulin. This means a violation of the biological response of peripheral tissue to the action of insulin, which “works” in both an endogenous and exogenous manner. Now there is such a thing as genetic determination of insulin resistance. For example, patients suffering from T2DM are carriers of point genetic mutations. Places of their origin:
- leptin receptor gene;
- SIR-1 gene (insulin receptor substrate);
- PPAR-gamma.
Secondary insulin resistance is caused by intoxication of the body with glucose, that is, a situation when a person is in a hyperglycemic state that lasts for a long time. Since modern man, unfortunately, consumes much more energy than he spends, it is insulin resistance that takes one of the leading places among the factors due to which:
- abdominal obesity occurs;
- free fatty acids accumulate in the body;
- as a result: a person gets sick with diabetes mellitus-2.
As already noted, the risk of heart and vascular diseases in diabetes is very high, which often leads to premature deaths among such patients.
Clinical symptoms of insulin resistance
Liver tissue, as well as muscle and fat tissue, lose sensitivity to the drug. Myocytes (muscle cells) suffer from a lack of glucose, as there are serious problems with its entry into the muscles from the bloodstream. In turn, adipocytes (fat cells) do not respond to the antilipolytic effect exerted by insulin. As a result, the following accumulate in the body:
- free fatty acids (abbreviated FFA);
- glycerol.
It is due to the action of FFA that low-density atherogenic lipoproteins (or VLDL) are formed.
Due to insulin resistance in the liver tissue, glycogenesis becomes lower, and glycogenolysis and gluconeogenesis, on the contrary, increase, which causes the development of hyperglycemia.