Iron and iron health: what role does the microelement play in our body?
Iron is part of hemoglobin. In turn, the protein hemoglobin is a building material for erythrocytes - red blood cells that carry oxygen from the lungs to the organs, and on the way back rid them of carbon dioxide. Actually, this process is called cellular respiration. Without iron it is impossible. And since every cell in our body needs oxygen, iron can be called one of the most important elements.
The synthesis of hemoglobin takes 60–70% of all iron entering the body. The remaining 30–40% is deposited in tissues and spent on solving other problems - metabolic processes, regulation of the thyroid gland, maintaining the body's defense system and connective tissue synthesis.
As you can see, the functions of iron are varied and numerous, but oxygen transport is the most important of them.
Iron is poorly absorbed even with ideal health and proper diet - the human body is able to absorb up to 10% of the iron supplied with food.
Its manifestations:
- Pale, slight yellowness of the hands and nasolabial triangle;
- Shortness of breath, increased heart rate, fainting (especially with a rapid transition from a horizontal to a vertical position);
- Palpitations, chest pain;
- Increased fatigue;
- Weakness, dizziness, flashing “spots” before the eyes, drowsiness during the day and insomnia at night, impaired concentration, decreased memory, performance, irritability, tearfulness;
- Loss of appetite, nausea, flatulence;
- Swelling of the face in the morning.
Patients often get used to their condition, regarding it as overwork, stress, etc.
Daily iron requirement in healthy people
Iron requirements vary depending on age and health status.
Infants under six months of age have little need for iron, since they are born with a fair supply of this element. Newborns only need 0.27 mg of iron per day. Children from six months to a year require 11 mg, children from 1-3 years old - 7 mg, children aged 4-8 years - 10 mg, 9-13 years old - 8 mg.
Adolescents 14–18 years old should receive 11–15 mg daily, with girls having a higher need for iron due to monthly blood loss during menstruation.
Men require about 10 mg of iron per day, women - 15-18 mg. During pregnancy, the norm increases to 25–35 mg, and during breastfeeding - to 25 mg.
After about 50 years, the iron requirement for men and women becomes the same - about 10 mg per day.
These are average figures, but in some cases the need for iron may be slightly higher than the statistical average. Athletes and people engaged in heavy physical labor require more iron. The need for iron also increases during recovery from operations and injuries (especially if they were accompanied by blood loss), infectious diseases, as well as for those who suffer from constant bleeding (hemorrhoids, stomach ulcers, nosebleeds, heavy menstruation, etc.).
Complications of pregnancy with iron deficiency anemia
Anemia in pregnant women is a pathological background that contributes to the development of a number of complications of pregnancy and childbirth.
- Premature abruption of a normally located placenta, anomalies of labor.
- Increased blood loss during childbirth and bleeding - in 10% of women.
- In 8–12% of cases, the postpartum period is complicated by purulent-septic diseases and uterine subinvolution.
- A lactation disorder was detected, and both quantitative and qualitative changes in breast milk were observed.
- Adverse effects on the condition of the fetus: contributes to the development of fetal growth retardation syndrome, chronic fetal hypoxia.
- A decrease in adaptation of newborns in the early neonatal period is recorded in half of the cases.
Foods High in Iron
Our body cannot synthesize iron; it only processes this element, extracting it from worn-out red blood cells. “Fresh” iron comes from food. However, even if you eat foods containing iron, this does not mean that you have enough. The thing is that there are two types of iron.
Iron can be heme (divalent) or non-heme (trivalent). The first is found in products of animal origin and is easily digestible (about 25%), the second is part of plants and is absorbed by only 8–10% maximum[3]. This is why vegans and vegetarians often lack this element, even if they eat foods rich in iron.
And yet, it is the right diet that is considered the main way to prevent iron deficiency. Iron is found in significant doses in the following foods:
Animal products:
- pork liver - 29 mg (hereinafter the figure is given per 100 g of product);
- hard cheese - 19 mg;
- beef liver - 9 mg;
- egg yolk - 6 mg;
- beef tongue - 5 mg;
- turkey - 4 mg;
- beef - 2.8 mg;
- chicken - 2.5 mg;
- mackerel - 2.5 mg;
- pork - 1.6 mg;
- herring - 1 mg;
- cottage cheese - 0.4 mg.
Products of plant origin:
- beans - 72 mg;
- hazelnuts - 51 mg;
- oat flakes - 45 mg;
- fresh forest mushrooms - 35 mg;
- millet - 31 mg;
- peas - 20 mg;
- seaweed - 16 mg;
- prunes - 13 mg;
- dried apricots - 12 mg;
- buckwheat - 8 mg;
- tofu - 5.5 mg;
- peaches - 4.1 mg.
Although the iron content of some plant foods is high, the non-heme form of iron is poorly absorbed. Therefore, it is important for those following a plant-based diet to check their iron levels and, if necessary, take dietary supplements that contain this element.
Our body perceives iron best from meat (on average 20% is absorbed), a little worse from fish and seafood (about 11%), legumes (7%) and nuts (6%). Only 1-3% of iron is absorbed from fruits, vegetables and cereals.
To improve the absorption of iron, it is also important to receive the right amounts of vitamins and minerals, which play the role of catalysts and help this element to be absorbed. These include:
- Vitamin C. Iron is almost not absorbed without ascorbic acid, so the menu must include foods rich in ascorbic acid - berries, oranges and grapefruits, cabbage, red peppers.
- Vitamin A. If a person lacks vitamin A, then iron will not be absorbed and used to “build” new red blood cells. Many orange and yellow fruits and vegetables are rich in vitamin A - it is this substance that gives them their cheerful colors. To replenish vitamin A reserves, you need to eat more dried apricots, carrots and pumpkin. However, it's important to know that fats are needed for this vitamin to be absorbed, so don't ignore sources of retinol like butter, fish oil, and egg yolks.
- Folic acid (vitamin B9). It helps absorb iron and normalizes the digestive tract, and healthy digestion is extremely important for the absorption of this element. Sources of folic acid are eggs, soybeans, yeast, green leafy vegetables, dill, eggplant, tomatoes, chicken liver.
- Copper. Sources of copper are offal, fish and seafood (shrimp, oysters, etc.), cabbage.
Principles of therapy
The primary goal of treatment is to prevent complications. For this:
1. Aspiration and gastric emptying are performed. Vomiting is induced if <1 hour has passed since taking the tablet. This will remove iron from the digestive tract before it is absorbed. Radiologically proven Fe tablets in the stomach are indicative of lavage. Please note that the procedure is contraindicated if the patient is vomiting blood.
2. Patients who are asymptomatic when taken within 6 hours and who show no signs of clinical toxicity do not require treatment.
3. Patients with rare symptoms require only symptomatic treatment.
4. Intravenous hydration for all patients with significant symptoms. Treatment with intravenous fluid to maintain fluid balance is important because hypovolemic shock is a leading cause of premature death from toxicity.
5. Check your blood pressure and heart rate regularly, and control your breathing.
6. The antidote for poisoning is Deferoxamine. This drug increases iron excretion (Fe-binding antidote) and is indicated for severe iron poisoning.
7. If the patient is unaffected after several hours of observation and serum Fe remains low, he is discharged.
Rules for rational nutrition
The more variety of products you use in cooking, the less likely you are to become deficient in iron or any other trace element or vitamin. However, the diet for iron deficiency also contains some restrictions. The fact is that some elements can impair the absorption of this mineral. This does not mean that you need to completely abandon them. But it is better not to eat foods containing iron at the same time as:
- tea and coffee, red wine. These drinks reduce the body's ability to absorb iron by about a third, by the way, like chocolate;
- milk and dairy products. They are rich in calcium, and calcium is not friendly with iron;
- sesame seeds and seeds, bran, sprouted wheat, nuts. All of these foods are valuable sources of magnesium. But magnesium, like calcium, interferes with the absorption of iron.
If your goal is to increase your blood iron levels, eat all of the above foods only 3-4 hours after foods high in iron. But you should avoid fatty and fried foods, ready-made oil sauces such as mayonnaise, hot spices and marinades - all this irritates the mucous membranes of the gastrointestinal tract and interferes with the absorption of iron.
Etiology and pathogenesis
· Free, unbound iron is toxic to living tissue and can locally destroy the intestinal mucosa.
· 10% of ingested iron (Fe 2+) is actively absorbed as ions in the small intestine. After absorption, iron accumulates as Fe3+ in the mucosal storage protein ferritin. From there, iron is transported to the liver, spleen and bone marrow for further storage in ferritin or for inclusion in the heme molecule.
· Iron is transported bound to the transport protein transferrin.
· When the blood's ability to bind iron is exceeded (serum iron > 90 µmol/L), free ions lead to tissue damage in most organs, including the liver and heart.
An example of a daily diet: today is my “iron” day...
How to create a menu that will help cope with iron deficiency? It's actually not difficult. Foods rich in iron and the vitamins necessary for its absorption are neither rare nor particularly expensive. Here is an example of an “iron” diet for one day:
Breakfast: 2 soft-boiled eggs or scrambled eggs, fresh cabbage salad, a slice of black bread with butter and hard cheese, orange juice:
Second breakfast: curd mousse with dried apricots and prunes or oatmeal with dried fruits, rosehip infusion. :
Lunch: chicken soup or borscht with mushrooms, stewed liver with onions or baked turkey with vegetable stew, fruit salad and dried fruit compote. :
Dinner: steamed beef patties or mackerel baked in foil, pea puree or stewed carrots, soothing herbal tea:
This menu is not only rich in iron, vitamins C, B9 and copper, it also fits the definition of dietary, contains a sufficient amount of fiber and will not harm your figure.
Helpful information
Find out more about poisonings, their symptoms, treatment regimens, antidotes and consequences:
- Acetylsalicylic acid.
- Carbon monoxide: signs, symptoms, treatment.
- Benzodiazepines.
- Benzodiazepine-like hypnotics.
- Beta blockers.
- Lead, fluorine.
- Calcium antagonist.
- Cardiac glycosides.
- Ethanol.
- Ethylene glycol.
- Histamine
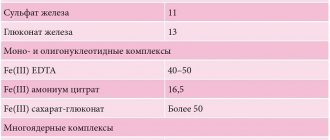
Iron intake standards for patients with anemia
Sometimes tests reveal not just a lack of iron, but a more serious situation - iron deficiency anemia. Typically, this condition develops against the background of gastrointestinal diseases, tumor processes, helminthic infestations, and constant bleeding. It is often diagnosed in people who have experienced significant blood loss during injury or surgery.
Iron deficiency anemia is diagnosed if the hemoglobin level drops to 100–70 g/l and serum ferritin drops to 15 ng/ml.
If iron deficiency anemia is diagnosed, you cannot prescribe treatment yourself. The doctor selects the therapy. Perhaps he will prescribe multivitamin complexes and dietary supplements with iron, and in the most severe cases, he may even prescribe iron supplements - quite strong drugs with numerous side effects. You can take such medications only under the supervision of your doctor.
Stages and characteristic symptoms
The manifestations of iron toxicity are usually described as five, often overlapping, phases:
- Gastrointestinal phase: from 30 minutes to 6 hours after oral administration. Symptoms: abdominal pain, vomiting, diarrhea, hematemesis, exhaustion, shock and metabolic acidosis. Vomiting is the most obvious indicator of severe poisoning at this stage. It occurs due to hypovolemic shock. Most patients with mild to moderate iron toxicity do not progress and symptoms resolve within 4 to 6 hours.
- Latent or relatively stable phase: 6 to 24 hours after administration. The latent phase gives the impression of improvement. It is short-lived or absent in people with severe poisoning.
- Shock and metabolic acidosis: 6 to 72 hours after ingestion. Shock, pallor, tachycardia, hypotension, coagulopathy may occur, and hepatotoxicity may further develop.
- Hepatotoxicity/liver necrosis: 12 to 96 hours after administration. Due to liver necrosis, intestinal obstruction occurs.
- Intestinal obstruction: 2-8 weeks after ingestion of Fe. Due to scarring of the gastrointestinal tract, especially at the exit from the stomach.
Clinical data
List of signs and symptoms
Stage 1 (1/2 to 1 hour after administration):
· Stomach ache.
· Vomiting and diarrhea, and bloody vomiting is not uncommon.
· Weakness, shock and metabolic acidosis may develop.
Stage 2 (6-12 hours after administration):
· Not everyone goes through this stage.
· Gastrointestinal symptoms may stop.
· This apparent recovery may provide false security.
Stage 3 (12-48 hours after administration):
· May occur early in case of serious poisoning or after the quiet phase of the 2nd course.
Metabolic acidosis and shock.
· Anemia.
· Necrosis.
· Kidney, liver and heart failure.
· Possibly fatal within 1-3 days.
Stage 4 (days to weeks after recovery):
· Obstruction of the gastrointestinal tract due to injury due to poisoning.
Additional Research
1. Determination of Fe concentration in the blood. Serum iron - useful to confirm Fe intake and to determine severity. High concentrations are not always associated with danger because they measure free circulating Fe while intracellular Fe causes systemic toxicity.
2. If serum Fe concentration is not readily available, the following may indicate serious toxicity:
Leukocytosis > 15 x 109.
· Hyperglycemia > 8.3 mmol/l.
· Diarrhea/vomiting.
· Detection of tablet residues using abdominal x-ray.
· Serum electrolytes, blood urea and serum creatinine.
· Glucose level.
3. Coagulation parameters (INR, prothrombin), determination of leukocyte formula. Blood gases should be obtained from a patient with severe symptoms.
4. Other studies. X-ray of the abdomen. The tablets are often X-ray resistant.
List of sources
- Smirnov O.A. Frequency and morphological characteristics of liver hemosiderosis // Russian Medical Journal. – 2002. – No. 6. – P.11–13.
- Eremina E. Yu. Hemochromatosis in the practice of a clinician // Medical almanac - 2015 - No. 1. pp. 75-76.
- Polunina T.E., Maev I.V. Iron overload syndrome: current state of the problem // Farmateka. - 2008. - No. 13. - P. 54–61.
- Clinical guidelines for the diagnosis and treatment of secondary iron overload / ed. Savchenko V. G. - 2014.
- Kuznetsova A.V., Dubotolkina E.V., Loifman E.A. Indicators of iron metabolism in chronic hepatitis C. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2009. No. 19 (5). P. 92.
Classification
There are classic (primary), genetically determined hemochromatosis and acquired (secondary) hemochromatosis.
Congenital hemochromatosis, according to the type of mutation, is represented by several types:
- HFE-associated hereditary type of hemochromatosis.
- Juvenile hemochromatosis.
- HFE-non-associated hereditary hemochromatosis.
- Hemochromatosis is an autosomal dominant type.
- Iron overload in newborns.
Secondary hemochromatosis is represented by several types:
- Post-transfusion hemochromatosis.
- Nutritional hemochromatosis.
- Metabolic hemochromatosis.
- Hemochromatosis of mixed origin.