Home | About us | Delivery | Advertisers | Login | Registration
The pharmacy is closed on Sundays and holidays.
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2021 Pharmacy 84.
The use of a combination of metronidazole and miconazole in the correction of vaginal dysbiosis
Introduction
One of the most common complaints when women visit a gynecologist is pathological discharge from the genital tract (leucorrhoea). The cause of pathological vaginal discharge can be a number of diseases and conditions [1]. According to various researchers, in 22–50% of cases, leucorrhoea is a symptom of bacterial vaginosis (BV) [2]. BV is a non-inflammatory disease of the vagina associated with changes in its microflora. This condition is extremely widespread among women of fertile age (20–45 years), its incidence in this group reaches 80%, i.e., out of 10 women, 8 experience BV at least once in their life. The disease does not pose a danger to the patient herself, but can negatively affect her reproductive function. BV often causes miscarriages, intrauterine fetal infections, complications after childbirth, abortions, and invasive interventions on the genitals. It has now become known that the vaginal microbiocenosis is a dynamic and much more complex ecosystem than previously thought. The state of the microflora of the genital area most seriously affects the health of women as a whole [2]. For the first time in 1892, Doderlein presented descriptions and images of the vaginal bacillus, subsequently named after him, and divided the bacterial communities of the female genital tract into “normal” (with a predominance of vaginal lactic acid bacilli) and “abnormal” (containing other numerous organisms, often streptococci or staphylococci ) [2]. It is known that the vagina is normally populated by lactobacilli, which break down glycogen, which is rich in vaginal epithelial cells, to form lactic acid. Thus, an acidic environment is constantly maintained in the woman’s lower genital tract, which prevents the establishment and growth of pathogenic microflora. To maintain normal conditions and the protective function of the vagina, a large number of lactobacilli are necessary, so their share in its biocenosis is 95–98%. For various reasons listed below, lactic acid bacilli are displaced and replaced by other microorganisms. This situation facilitates the colonization of the vagina by pathogenic microorganisms - causative agents of sexually transmitted infections, but in most cases there is a change to nonspecific microflora. It includes bacteria that live on the skin of the perineum, perianal folds, and in the lower part of the urethra. They freely occupy a new habitat, multiply intensively, but cannot perform the functions of normal microflora. Their enzyme system is different from that of lactobacilli and does not break down glycogen to form lactic acid. Nonspecific microflora causes a number of disturbances in the metabolic and immune processes of the vagina as a whole. The level of production of protective immunoglobulin A decreases, which prevents pathogenic agents from attaching to the vaginal epithelium. Epithelial cells partially adsorb opportunistic bacteria on their surface and are intensively desquamated, which is associated with the appearance of discharge in BV. Lactobacilli are replaced mainly by anaerobes - bacteria that function without access to oxygen. Some of the products of their metabolism - volatile fatty acids and amino acids - are broken down in the vagina into volatile amines, which have a characteristic fishy odor. The described changes lead to a shift in vaginal pH from acidic to alkaline values. This entails progressive changes in the protein, carbohydrate, mineral and lipid metabolism of epithelial cells. Their production and mucus production increase, which clinically manifests itself as heavy discharge - the main symptom of BV. It should be noted that there is no inflammatory reaction in the walls of the vagina, and all changes are only functional in nature. Currently, a detailed study of the cultural and biochemical properties of representatives of vaginal biopsy specimens has led to the transformation of knowledge about the types of disorders of vaginal normocenosis and its infectious pathology [3]. So, BV is not a sexually transmitted infection
and does not have a single pathogen, which is why it is otherwise called “nonspecific vaginosis.” The root cause is a change in the vaginal environment, which entails disturbances in microbiocenosis. The microflora that replaces lactobacilli can be different and is most often represented by associations of opportunistic bacteria. Among them, the following groups are distinguished: bacteroids; peptococci; peptostreptococci; megaspheres; leptotrichia; atopobium; gardnerella; mycoplasma. It is also worth noting that disturbances of the vaginal microcenosis occur in 45–86% of patients in gynecological hospitals and lead to infectious complications after surgical interventions on the pelvic organs and contribute to the occurrence of diseases of the internal organs. By damaging the biological barrier, they increase several times the likelihood of infection with sexually transmitted pathogens. The growth of lactobacilli, as a rule, is excessive - their number in vaginal secretions reaches 1010 per 1 ml. However, comfortable conditions for their reproduction arise only after the influence of certain factors of the external or internal environment of the body [4].
The main causes of BV can be divided into 2 large groups.
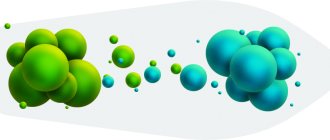
Internal (endogenous): hormonal imbalance with a predominance of progesterone; atrophy of the vaginal mucosa; intestinal dysbiosis; immune disorders in the body. External (exogenous): long-term treatment with antibiotics; drug immunosuppression (taking cytostatics, glucocorticoids); radiation therapy of tumors; foreign objects in the vagina (hygienic tampons, pessaries, contraceptive diaphragms, rings); use of spermicides, frequent douching; failure to comply with personal hygiene rules. All of these factors in one way or another disrupt the normal functioning of the vaginal mucosa or cause the death of a large number of lactobacilli. Thus, a niche is freed up for opportunistic microflora, and it immediately occupies it. Despite the fact that the disease is not a sexually transmitted infection, its occurrence is often associated with sexual intercourse, especially when changing partners. Signs of BV in women develop on average one day after sexual intercourse without a barrier method of contraception. If the cause of the disease was the use of antibiotics and other medications, changes in hormonal levels (menopause), then the symptoms of BV develop regardless of sexual activity. According to modern concepts, one of the key links in the pathogenesis of BV is the ability of etiologically significant bacteria to form biofilms [2]. A biofilm is a microbial community in which cells are attached to any surface and/or to each other and are enclosed in an interbacterial matrix of extracellular polymeric substances synthesized by them; bacteria in biofilms have altered physiological properties [5]. Biofilm microflora is more resistant to adverse factors of a physical, chemical and biological nature compared to free-floating (planktonic) bacteria. Under such conditions, bacteria are resistant to ultraviolet radiation, dehydration, viruses, antibiotics and immune defense factors. The stability factor of biofilms is the mucus-polymer layer produced immediately after adhesion and including lipopolysaccharides, proteoglycans, glycoproteins, endopolysaccharides, similar to the substance of the cell wall, glycocalyx and bacterial capsules [5]. Recent studies indicate that BV exists as a polymicrobial biofilm infection [6, 7]. It is believed that Gardnerella vaginalis
is the first to attach to the vaginal epithelium and then serves as a “scaffold” for the attachment of other bacteria.
R. Alveset al. [8] identified 30 species of bacteria associated with BV and, in model experiments, characterized their virulence, defined as high adhesion, cytotoxicity, and a predisposition to form biofilms. It was shown that most bacteria associated with BV tended to grow as biofilms, but G. vaginalis had the highest virulence (60–90%), and Atopobium vaginae had the lowest.
The diagnosis of BV is established after collecting the patient’s medical history, studying her complaints, examining her in a gynecological chair and obtaining laboratory data.
In favor of BV, they say: age - sexually active women of reproductive age are most often affected; relationship with a change of partner, treatment of other diseases, surgical intervention; moderate or mild severity of clinical signs of the disease. During the examination, the doctor assesses the condition of the vagina, cervix, and external genitalia. With nonspecific changes, the mucous membrane is pink, not inflamed, and unevenly covered with secretions. In acute BV they are white-gray, with an unpleasant odor. If the disease has become chronic and lasts for several years, the discharge changes its color to yellowish-green, becomes thicker, more viscous, resembles cottage cheese or has a foamy appearance. During the examination, the gynecologist measures the vaginal pH with an indicator strip: with BV, its value is above 4.8–5.0. It is also worth noting the Nugent criteria - one of the main diagnostic systems for BV, which, however, in the light of new data on the “lactobacillary-free” type of vaginal microflora has shortcomings. Thus, to characterize the microbiota, the number of lactobacilli relative to BV, the associated bacterial morphotypes, is assessed. Indeed, women with a predominance of Lactobacillus spp
. they do not have BV in the vaginal biopsy. However, the conclusion that a small number of lactobacilli or their absence clearly confirms the presence of BV is incorrect [2]. Laboratory diagnosis of BV involves microscopy of stained vaginal smears. Key cells are found in them - epithelial cells of the mucous membrane with microbial bodies adhered to their surface. The cell takes on a granular appearance, its boundaries become fuzzy and dotted. Also, microscopy reveals a sharp decrease in the number of lactobacilli, up to complete disappearance from the population [2, 9, 10]. Instead, nonspecific microflora is found: single cocci, streptococci, small bacilli. Bacteriological seeding of secretions is carried out in rare cases when it is necessary to accurately determine the composition of the altered microflora. Currently, the gold standard for diagnosing BV is real-time polymerase chain reaction.
Treatment of BV
It is known that bacteria in biofilms respond to antibiotic therapy differently than planktonic bacteria, since the intercellular matrix of the biofilm can bind or not allow and/or inactivate antibiotics [7, 8]. In this regard, the formation of biofilms in BV is considered one of the main causes of persistent and recurrent BV [7, 8]. The search for drugs capable of penetrating biofilms and destroying them seems to be an urgent task. In vitro
data indicate the ability of lactobacilli to effectively destroy biofilms [7], which allows us to consider the combination of antibacterial drugs with probiotics as a promising approach to the treatment of BV.
The following regimens are recommended for the treatment of BV: European recommendations for the management of patients with pathological vaginal discharge, published by the International Union against Sexually Transmitted Infections - IUSTI (International Union against Sexually Transmitted Infections)/WHO in 2011: metronidazole (gel 0.75%) 5 g intravaginally for 5 days or clindamycin (2% cream) 5 g intravaginally at bedtime for 7 days, or clindamycin per os 300 mg twice a day for 7 days [11]. 2010 Centers for Disease Control and Prevention (CDC) recommendations: metronidazole 500 mg orally bid for 7 days or metronidazole (0.75% gel) 5 g vaginally at night for 5 days, or clindamycin (2% cream) 5 g vaginally at night for 7 days [12]. We carried out a study, the purpose
of which was to compare subjective and laboratory parameters before the study and 14 days after using the drug metronidazole and miconazole (combined drug Metromicon-Neo® (JSC Avexima, Russia) in the treatment of BV.
Material and methods
A study was conducted at the Medsi CDC on Krasnaya Presnya, in which 40 women aged 20–45 years with disorders of the vaginal microcenosis took part. The diagnosis was established on the basis of complaints, an outpatient test to determine the level of acidity of the vaginal contents and the results of a dynamic microscopic examination. The study drug was Metromicon-Neo®, which is available in the form of vaginal suppositories containing 500 mg of metronidazole and 100 mg of miconazole. Metromicon-Neo® has antibacterial, antiprotozoal and antifungal effects.
Mechanism of action of Metromicon-Neo®:
Metronidazole belongs to the 5-nitroimidazoles and is a drug with a bactericidal type of action that exhibits tropism (the ability to interact) with deoxyribonucleic acid (DNA). The mechanism of action is the biochemical reduction of the 5-nitro group of metronidazole by intracellular transport proteins of anaerobic microorganisms and protozoa. The reduced 5-nitro group of metronidazole interacts with the DNA of microbial cells, inhibiting the synthesis of their nucleic acids, which leads to the death of bacteria. Active against protozoa: Trichomonas vaginalis, Entamoeba histolytica
, as well as obligate anaerobic bacteria: gram-negative -
Bacteroides spp
.
(including Bacteroides fragilis, Bacteroides distasonis, Bacteroides ovatus, Bacteroides thetaiotaomicron, Bacteroides vulgatus), Fusobacterium spp., Veillonella spp., Prevotella spp;
(Prevotella bivia, Prevotella buccae, Prevotella disiens) , gram-positive -
Clostridium spp., Eubacterium spp., Peptococcus spp., Peptostreptococcus spp:, Mobiluncus spp.
and facultative anaerobe -
Gardnerella vaginalis.
Aerobic microorganisms are insensitive to metronidazole, but in the presence of mixed flora (aerobes and anaerobes), metronidazole acts synergistically with antibiotics, with a positive result against ordinary aerobes.
Miconazole is an azole derivative antifungal agent. When used intravaginally, it is active mainly against Candida albicans
. The fungicidal and fungistatic effects of miconazole are caused by inhibition of the biosynthesis of ergosterol in the membrane and plasma membranes of fungi, changes in the lipid composition and permeability of the cell wall, which causes the death of the fungal cell. Indications for use: vaginal candidiasis; trichomonas vaginitis, BV; mixed vaginal infection.
Research results
Before treatment, patients were mainly concerned about the presence of vaginal discharge with an unpleasant odor, and less frequently complained of burning, itching and discomfort in the genital area (Table 1).
Before treatment, all women studied had a vaginal pH of more than 5.0. When microscopy of vaginal smears, the microflora was mainly represented by cocci, a large number of key cells were found, the presence of a large amount of epithelium was detected in 12.5% of cases (Table 2).
All women received Metromicon-Neo® vaginal suppositories, 1 suppository in the morning and at night for 7 days. After 2 weeks Subjective and microscopic findings were assessed. As a result, it was shown that after treatment the patients had a significant reduction in the number of complaints (Table 3).
After treatment, all patients had vaginal pH ≤4.5. According to microscopic examination of vaginal smears, normalization of its microflora was observed (Table 4).
Thus, with the use of the drug Metromicon-Neo®, positive treatment results were noted (clinical picture data, microscopic examination) and good tolerability of the drug.
Conclusion
Based on the data obtained, we can conclude that Metromicon-Neo® can be recommended for the treatment of BV.
The use of combined antimicrobial drugs at the initial stages of the development of BV leads to a reduction in the risk of formation of pathological biofilms, thereby reducing the frequency of disease relapses. Information about the authors:
Yulia Eduardovna Dobrokhotova - Doctor of Medical Sciences, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medicine. Federal State Budgetary Educational Institution of Higher Education Russian National Research University named after. N.I. Pirogov of the Russian Ministry of Health. 117997, Russia, Moscow, st. Ostrovityanova, 1. Ivanova Irina Igorevna - obstetrician-gynecologist, gynecologist-endocrinologist. CDC "Medsi" on Krasnaya Presnya. 123242, Russia, Moscow, st. Krasnaya Presnya, 16. Contact information: Ivanova Irina Igorevna, e-mail: [email protected] . Financial transparency: none of the authors has a financial interest in the materials or methods presented. conflict of interest . The article was received on August 23, 2018.
About the authors : Yulia E. Dobrokhotova - Doctor of Medical Science, professor Head of Department of Obstetrics and Gynecology, Medical Faculty, NI Pirogov Russian National Research Medical University.
1, Ostrovityanova str., Moscow, 117997, Russian Federation. Irina I. Ivanova - obstetrician-gynecologist, gynecologist-endocrinologist. CDC “Medsi in Krasnaya Presnya”. 16, Krasnaya Presnya str., Moscow, 123242, Russian Federation. Contact information: Irina I. Ivanova, e-mail: [email protected] . Financial Disclosure: no author has a financial or property interest in any material or method mentioned. There is no conflict of interests. Received 08/23/2018.