Indications
Ministry of Health of Russia
G40.0 Localized (focal) (partial) idiopathic epilepsy and epileptic syndromes with seizures with focal onset
G40.1 Localized (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures
G40.2 Localized (focal) (partial) symptomatic epilepsy and epileptic syndromes with complex partial seizures
G53.0 Neuralgia after herpes zoster (B02.2+)
FDA recommendations
Partial seizures with or without secondary generalization
Neuralgia after shingles
Restless legs syndrome
UK Medicines and Healthcare Products Regulatory Agency guidelines
Epilepsy
Neuropathic pain
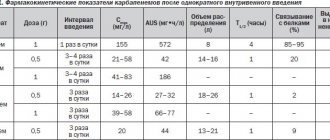
Treatment regimen
Dosage and dose selection
- 900-1800 mg/day in three divided doses
- Neuralgia after shingles (immediate release): 300 mg on day 1; 600 mg in two divided doses on day 2; 900 mg in three doses on day 3.
- Neuralgia after herpes zoster (extended release): 600 mg in the morning on day 1; 1200 mg per day in two divided doses on day 4.
- Restless legs syndrome (sustained release): 600 mg per day in one dose, around 5 p.m.
- Convulsions (adults and children over 12): initial dose 900 mg/day in three divided doses; recommended dose 1800 mg/day in three divided doses; the time interval between doses should not exceed 12 hours.
- Convulsions (children 5-12): initial dose 10-15 mg/kg per day in three divided doses; within three days, increase to 25-35 mg/kg per day in three doses; maximum dose 50 mg/kg per day; the time interval between doses should not exceed 12 hours.
- Convulsions (children 3-4): initial dose 10-15 mg/kg per day in three divided doses; within three days, raise to 40 mg/kg per day; maximum dose 50 mg/kg per day; the time interval between doses should not exceed 12 hours.
- If gabapentin is added to another anticonvulsant, increase the dose of gabapentin slowly over a week.
- Some patients with pain or anxiety may benefit from taking immediate-release gabapentin only twice a day.
- Very high doses can be divided into more than 3 doses per day.
- Any broken half of a tablet that is not used within a few days should be thrown away.
- Gabapentin extended-release tablets should not be crushed or chewed.
- Gabapentin extended-release tablets must be taken with food.
- If very strong sedation occurs, most of the daily dose can be taken at night
How quickly does it work?
The cramps go away after 2 weeks.
The pain goes away in 2 weeks or less.
May reduce anxiety in various disorders for several weeks.
Expected Result
Disappearance of symptoms.
If it doesn't work
If the pain does not go away after 6-8 weeks, you need to increase the dose or discontinue the drug.
How to stop taking it
Reduce dose for at least a week. If taken abruptly, epileptics may experience seizures [1].
Treatment combinations
- Gabapentin is itself an augmentant that is added to other anticonvulsants in the treatment of epilepsy; to lithium, atypical antipsychotics and anticonvulsants in the treatment of bipolar disorder.
- Gabapentin is added to antidepressants in the treatment of neuropathic pain
- In the treatment of anxiety, gabapentin is a second-line drug of choice, added to antidepressants or benzodiazepines [1].
Introduction
Intervertebral disc herniation (IVDD) is a common disease that causes back pain and radicular syndrome, leading to a significant limitation of physical activity, the development of a pain stereotype of behavior, which in turn contributes to the development of depressive syndrome and a decrease in quality of life;
It is estimated that up to 5% of the adult population suffers from this disease each year [1]. Radicular syndrome was first described by WE Dandy in 1929 as a clinical syndrome associated with extradural formation [2]; The main factors contributing to the development of radiculopathy include inflammation of the nerve root and IVD tissue. Mixter and Barr first developed a surgical approach to the treatment of lumbar IVD in 1934; Since then, various surgical interventions to remove the IVD for the treatment of persistent pain have been performed on a large number of patients. However, in most cases, pain relief from GMPD is possible with conservative treatment. Traditional nonsteroidal anti-inflammatory drugs (NSAIDs) are most often prescribed, sometimes in combination with muscle relaxants and/or weak opioids [3, 4]. Gabapentin has been reported to be effective against neuropathic pain [5, 6], including satisfactory results from clinical trials of the drug in patients with spinal stenosis and/or IVDD [7, 8]. In some cases, spontaneous regression of the IVD has been described. It is assumed that spontaneous regression of the lumbar spine IVD is associated with an inflammatory reaction involving macrophages and molecular mechanisms of phagocytosis [9]. The scientific literature describes a significant number of cases of regression of large IVDs without surgical intervention [10].
In this article, we present a clinical observation of three patients who experienced spontaneous regression of the lumbar spine IVD during physical and drug therapy with gabapentin.
Clinical example No. 1
Patient Shch., 41 years old, complained of severe pain in the lumbar region (5–6 points on the visual analogue scale - VAS) radiating to the right leg, numbness of the big toe of the right foot. From the anamnesis it is known that lower back pain has been bothering me for 3 years. She was treated on an outpatient basis 2 times (NSAIDs, B vitamins) with a positive effect. The real aggravation occurred after a long period of driving a car. The pain in the lower back intensified and became constant. Rest and painkillers (analgin, baralgin) did not bring relief.
Neurological status: forced body position with a tilt to the left and forward, movements in the lumbar region are sharply limited in all directions. Pain is detected on palpation of the spinous processes and paravertebral points L5–S1. Tendon reflexes from the arms are equal, from the legs S > D. Hypoesthesia along the L5–S1 dermatome, hypotonia and hypotrophy of the gastrocnemius muscles on the right. The symptoms of Lasegue, Dezherina, Neri are sharply positive.
Magnetic resonance imaging (MRI) of the lumbosacral spine (06/21/2016) revealed a dorsal right medial paramedian disc herniation L5/S1 with a sagittal size of up to 1.3 cm at the level of the IVD, a defect in the fibrous ring through which the sequestered fragment spreads IVD (size up to 1.1×0.9 cm in the axial plane), narrowing of the spinal canal up to 8.0 mm (Fig. 1).
The patient underwent 10 physiotherapeutic procedures (acupuncture and laser therapy in the projection of the GMTD). As analgesic therapy, she received gabapentin at a dose of 900 mg (300 mg 3 times a day; 20 days), a complex of B vitamins (tablet form).
After treatment, the pain syndrome completely regressed, which made it possible to gradually reduce and then discontinue gabapentin over 5 days. Numbness of the thumb persisted.
Repeated MRIs (09/18/2016, 01/05/2017) did not reveal significant changes in the size and signal characteristics of the hernia and the migrated component. In the neurological status, decreased tendon reflexes on the right, hypersthesia along the L4–L5 dermatome, hypotonia and hypotrophy of the gastrocnemius muscles on the right remained. Symptoms of tension and pain on palpation of the spinous processes are less pronounced.
Subsequently, the patient underwent a similar set of physiotherapeutic procedures: once a week for 5 weeks. During this period she had no exacerbations or loss of ability to work.
An MRI dated February 2, 2017 revealed a significant decrease in the sequestered component. By this period, the numbness of the thumb was completely absent.
Subsequent MRI (February 23 and April 7, 2017) showed a significant reduction in the size of the IVD. Neurological status is normal.
Clinical example No. 2
Patient A., 39 years old, complained of severe pain (VAS score 8–9) in the lumbosacral spine, pain and numbness in the left leg. The pain intensified at night, when walking (I could walk no more than 100 meters). From the anamnesis it is known that a week ago, after physical activity, an attack of intense pain radiated along the lateral surface of the left lower limb, similar to “strap pain,” occurred. Neurological status: antalgic posture (bending forward and to the right), sharp limitation of movements of the lumbar spine, tension of the paravertebral muscles of the back, right-sided ischialgic scoliosis, smoothed lumbar lordosis. Pain on palpation of the spinous processes and paravertebral points at the level of L4–L5. Absence of the Achilles reflex on the left. Lassegue's symptom is positive, angle - 15 degrees, positive "landing" symptom, Soobraz's symptom, Larrey's symptom. There are no sensory disorders or paresis, pelvic functions are not impaired.
According to MRI data (12/08/2016), the patient was diagnosed with a dorsal medial disc herniation L4/L5 with a sagittal size of up to 0.8 cm at the level of the IVD. Along the upper contour of the hernia, a defect in the fibrous ring is determined, through which the IVD substance extends (up to 3.0 × 1.1 cm in size in the axial plane). The spinal canal at this level is narrowed to 6 mm in the anteroposterior direction (Fig. 2).
The patient underwent 10 physiotherapeutic procedures (acupuncture and laser therapy in the projection of the GMTD). As analgesic therapy, he received gabapentin 1200 mg (300 mg 4 times a day; 30 days), a B complex of vitamins (tablet form), and amitriptyline 25 mg (once a day before bedtime, 10 days).
During treatment and observation (December 16 and 23, 2016, January 14, 2017), MRI studies were performed, which revealed an increase in the MR signal on T2 VI from the IVD and the sequestering fragment, which could be a sign of an increase in the inflammatory process. At the same time, since January 12, 2017, the patient did not receive pain medication due to the absence of pain. Complaints of stiffness in the lumbosacral spine when walking persisted. The neurological status showed positive dynamics in the form of a slight restoration of the Achilles reflex on the left. Symptoms of tension and pain on palpation of the spinous processes were less pronounced. There were no exacerbations or loss of the patient's ability to work during that period.
A repeated course of physiotherapy was prescribed from January 13, 2017: once a week for 5 weeks. According to MRI data (01/28/2017), a decrease in the migrated component. At the time of the image there were no complaints, but a month later (02/19/2017) there was complete regression of the hernia and the sequestered fragment.
Clinical example No. 3
Patient N., 53 years old, complained of pain in the lumbosacral spine (7–8 points on VAS) radiating to the left leg, a feeling of numbness along the S1 root. From the anamnesis it is known that periodic pain was noted over the past 5 years and was relieved with medication. The real exacerbation occurred after intense physical activity; taking NSAIDs did not bring relief. In the neurological status: the gait is gentle, movements in the lumbar region are sharply limited in all directions. Pain was detected on palpation of the spinous processes and paravertebral points L5–S1 on both sides. Tendon reflexes from the arms and legs S=D. Larrey's and Volkmann-Eriksen's symptoms are sharply positive.
An MRI (07/12/2016) revealed a dorsal left-sided medial-paramedian disc herniation L5/S1 with a sagittal size of up to 1.4 cm with a tendency to sequestration, extending into the left intervertebral foramen. Along the posterior contour of the hernial protrusion, a defect in the fibrous ring is visualized. The hernia partially compresses the dural sac and the left nerve root (Fig. 3).
The patient underwent a 10-day course of physical therapy (acupuncture, laser therapy), as well as drug therapy: gabapentin 900 mg (300 mg 3 times a day, 17 days), vitamin B complex (tablet form). After the course of treatment, there were no complaints of pain and numbness. In the neurological status, positive dynamics were noted in the form of relief of antalgic posture, increased range of motion in the lumbar region, and relief of Larrey's symptom. The Volkmann–Eriksen sign persisted, and slight painful palpation of the spinous processes was observed at the level of L4–L5.
When performing a repeat MRI (08/05/2016), an increase in the vertical size of the hernial protrusion was noted to 1.55 cm (previously 0.84 cm) and a change in its signal characteristics due to the acquisition of a more hyperintense MR signal on T2 VI (indirect signs of increased inflammatory process) .
The next stage of treatment was repeated physiotherapeutic procedures once a week (5 times).
Subsequent MRIs (August 25, September 27, and October 20, 2016) showed a consistent decrease in the hernial protrusion and sequestering fragment to 0.75 cm in the sagittal dimension and to 0.6 cm in the vertical direction.
Discussion
The scientific literature describes cases of spontaneous regression of the IVD without surgical intervention, but the exact mechanism of this phenomenon is unknown. The possibility of spontaneous regression of the hernia was first suggested by FC Jr Guintaet et al. in 1980 [11]. In most cases, it is observed during the first year of the disease; according to some data, it can occur in the first 2–3 months [10, 12].
Possible mechanisms of spontaneous regression of disc herniation
There are several hypotheses to explain the mechanism of spontaneous regression of the GMPD. The first of them suggests that dehydration of the nucleus pulposus leads to mechanical retraction of extruded tissues within the annulus fibrosus, which leads to spontaneous regression of the hernia. The second hypothesis implies that a herniated IVD can undergo retraction back into its normal space, but theoretically this can occur when the disc protrudes through the annulus fibrosus without separating from it [1]. The third mechanism involves enzymatic destruction and phagocytosis of cartilage tissue as a result of the inflammatory reaction and neovascularization of the disc herniation [9]. Once the nucleus pulposus is disrupted and comes into contact with the epidural vascular space, its tissue is recognized as a foreign body and becomes the target of an autoimmune inflammatory response, resulting in neovascularization, enzymatic destruction, and phagocytosis by macrophages. On the other hand, the formation of matrix proteinases and increased levels of cytokines also play a role in the process of spontaneous regression [13].
Mechanism of action of gabapentin
Gabapentin is an anticonvulsant and analgesic drug, an analogue of the neurotransmitter gamma-aminobutyric acid, which is increasingly used to treat neuropathic pain. However, the nature of its action remains poorly understood [8]. One of the mechanisms of action is believed to be binding to the α2δ subunit of the voltage-gated calcium channel, which is actively expressed in the dorsal root ganglia [7]. Another mechanism explaining the effect of gabapentin in reducing persistent sodium current also involves dorsal root ganglion neurons [8]. Gabapentin has demonstrated efficacy in reducing pain caused by spinal stenosis and intraspinal IVD. The drug also has a positive effect in acute radicular syndrome [7].
Also, some researchers noted minor anti-inflammatory properties of gabapentin. B. S. Lee et al. (2013) demonstrated that gabapentin reduces the levels of pro-inflammatory mediators (eg, tumor necrosis factor-α, inteleukin-1b and -6) and also increases the level of anti-inflammatory interleukin-10 in a rat model of neuropathic pain [14]. Subsequently, JM Dias et al. (2014) showed that gabapentin causes a decrease in inflammatory responses in known models of inflammatory processes in mice [15]. It is not yet clear whether the anti-inflammatory effect of gabapentin is associated with the regulation of calcium current or with other mechanisms (stimulation of endogenous antioxidant systems, suppression of NF-κB, blockade of NMDA receptors, activation of adenosine A1 receptor [14–16].
Currently, the immunoinflammatory theory of hernia resorption is increasingly confirmed in research, and in this light, gabapentin can become a good therapeutic alternative, on the one hand, from the point of view of pain relief, on the other, due to its lack of direct anti-inflammatory effect, which theoretically can reduce the rate of hernia resorption. Thus, it is hypothesized that drug treatment of lumbar vertebral disc lesions using gabapentin in combination with physical therapy may provide both clinical improvement and spontaneous regression.
Special patient groups
Patients with kidney problems
Reduce dosage [1].
The use of gabapentin in patients with renal failure younger than 12 years of age has not been studied.
Patients with liver disease
Use in normal dosage [1].
Patients with heart disease
No special recommendations [1].
Elderly patients
Elderly patients are more likely to experience side effects (ataxia, edema) [1].
Children and teenagers
- Gabapentin is approved for use in the treatment of seizures in children over 3 years of age [1].
Pregnant
- There have been no adequate studies in pregnant women [1].
- All risks should be weighed and compared
- When treating bipolar disorder or psychosis, discontinue gabapentin during pregnancy; For patients with bipolar disorder, stop taking gabapentin until pregnancy; You can resume taking it immediately after birth.
Breast-feeding
- The medicine passes into breast milk.
- It is recommended that you stop taking gabapentin or stop breastfeeding
Newspaper "News of Medicine and Pharmacy" Neurology (316) 2010 (thematic issue)
The main cause of lumbosacral radiculopathy is a herniated intervertebral disc, less commonly (usually in older age) it is caused by compression of the root in the area of the lateral recess, intervertebral foramen during spondylosis due to the formation of osteophytes, hypertrophy of articular facets, ligaments or other reasons [2, 4 , 5, 25]. Persistent maintenance of pain during a hernia may be associated not so much with compression of the root, but with secondary neurophysiological and metabolic processes that are triggered by the insertion of the disc into the epidural space and the effect of the material released from the nucleus pulposus on the nervous tissue [5]. According to clinical neuroimaging comparisons, pain intensity does not correlate with the degree of disc protrusion or mechanical deformation of the root. As experimental data show, inflammatory changes in the compressed root and (which is especially important) in the spinal ganglion can also play a key role in the development of radicular pain [27]. The result is irritation, intra- and extraneural swelling of the root or blockade of conduction along it. Changes in the neurophysiological characteristics of nerve fibers, neurons of the spinal ganglia and dorsal horns of the spinal cord also play an important role [1, 3, 5].
Clinically, lumbosacral radiculopathy is characterized by persistent or paroxysmal intense pain, at least occasionally radiating to the distal zone of the dermatome (for example, when taking Lassegue), pronounced muscular-tonic syndrome, often accompanied by scoliotic deformity of the spine, changes in sensitivity (pain, temperature, vibration, etc.) .) in the corresponding dermatome, a decrease or loss of tendon reflexes that close through the corresponding segment of the spinal cord, hypotension and weakness of the muscles innervated by this root [4, 5].
In the majority of patients with discogenic radiculopathy, conservative therapy can achieve significant weakening and regression of the pain syndrome, and only in a relatively small proportion of cases of uncomplicated discogenic radiculopathy, characterized by particularly intense persistent pain, severe limitation of mobility, and resistance to conservative therapy, surgical intervention is indicated. A recently published study [20] noted that although early surgical treatment for discogenic radiculopathy leads to faster pain relief, later (after six months, a year and 2 years) it does not have any advantages over conservative therapy and does not reduce pain. risk of chronic pain. On the other hand, later surgical treatment is not inferior in effectiveness to earlier ones [20].
As for conservative treatment of discogenic radiculopathy, it is subject to justified criticism [4, 9, 10]. The fact is that the traditionally used and still popular lumbar traction turned out to be ineffective in controlled studies [10]. It has been found [6] that epidural blocks with corticosteroids, although they can help relieve pain, have only a short-term effect. The practice of long-term bed rest also turned out to be untenable: with radiculopathy, as with other types of back pain, a faster return to daily activity prevents pain from becoming chronic [25].
The basis of conservative therapy remains NSAIDs, muscle relaxants and some other non-drug methods, mainly affecting the nociceptive component of pain, including massage, therapeutic exercises, effects on myofascial syndrome, some manual therapy techniques, etc. [4, 10]. However, the effectiveness of such therapy is limited and in a significant number of cases does not allow the intense pain syndrome characteristic of radiculopathy to be quickly relieved, which may be a condition for faster recovery. This forces us to look for additional opportunities to enhance the analgesic effect, primarily through methods that act on the neuropathic component of pain [7, 21].
Considering the mixed nature of the pain syndrome in discogenic radiculopathy, including nociceptive, neuropathic, and often psychogenic components, the impact on the neuropathic component of pain seems very promising [7, 8, 13]. However, the effectiveness of drugs traditionally used for neuropathic pain (anticonvulsants, antidepressants and others) in patients with back pain remains insufficiently proven [10].
In particular, the feasibility of using anticonvulsants in patients with radiculopathy and back pain in general remains a subject of debate. Anticonvulsants have proven themselves to be an effective treatment for pain in cranial neuralgia, postherpetic neuralgia, and polyneuropathy. However, data from studies of their effectiveness in patients with back pain are contradictory. This inconsistency of results is largely determined by the heterogeneity and diversity of back pain variants, the variability of their mechanisms and, possibly, different timing of the start of treatment.
The purpose of this study was to evaluate the effectiveness of the anticonvulsant gabapentin, widely used in the last decade for the treatment of pain syndromes in patients with discogenic lumbosacral radiculopathy, depending on the timing of treatment.
Material and methods
The study included 25 patients (14 women and 11 men) with discogenic radiculopathy.
The diagnosis of radiculopathy was established in the presence of radicular pain syndrome (irradiation of pain to the distal part of the dermatome: spontaneous and/or with Lassègue's maneuver) plus at least one symptom of prolapse: decrease (loss) of the corresponding tendon reflex, decrease in pain, temperature (cold), tactile or vibration sensitivity in the dermatome area or weakness of the muscles innervated by this root.
The presence of a disc herniation of the appropriate localization was established using CT or MRI of the lumbosacral region. The study included 14 patients with L5 radiculopathy and 11 patients with S1 radiculopathy. The average age of the patients was 46.8 ± 9.1 years. The severity of pain as assessed by VAS ranged from 5 to 9 points (average 7.5 points).
Exclusion criteria were the presence of a tumor, infectious-inflammatory or other disease of the spine requiring specific treatment, severe spinal deformity, spinal cord compression, other concomitant neurological diseases, psychiatric diseases, serious or unstable somatic diseases (severe diseases of the liver, cardiovascular system, lungs or kidneys, decompensated diabetes mellitus, cancer).
The patients were divided into 2 groups: group 1 included 12 patients with a duration of exacerbation of pain syndrome of no more than 1 month, group 2 included 13 patients with a duration of exacerbation of more than 1 month. Accordingly, in group 1, treatment with gabapentin was started during the 1st month of exacerbation, in group 2 - after 1 month. and more from the onset of exacerbation.
From days 1 to 12, Gabapentin was prescribed in increasing doses. Starting from the 13th day, patients took the drug at a dose of 1800 mg. If there is no improvement over the next 2 weeks. the dose could be increased to 3600 mg per day. The total duration of the study was 8 weeks. In both groups, patients, in addition to gabapentin, were prescribed standard therapy, including NSAIDs, exercise therapy, physiotherapy and massage. During the previous week and throughout the study, patients were not prescribed muscle relaxants, B vitamins, antidepressants, other anticonvulsants, or therapeutic blockades.
There were no significant differences between the groups in terms of gender, age, therapy, including the dose of NSAIDs.
None of the patients had previously undergone surgery. The average dose of gabapentin in group 1 was 2110 ± 370 mg per day, in group 2 - 2200 ± 395 mg/day.
To assess the effectiveness of gabapentin, a Clinical Global Impression (CGI) scale was used, which included the following gradations: worsening, no change, minimal improvement, moderate improvement, significant improvement.
The back pain scale (BPS), based on the principle of a visual analogue scale (VAS), provided for patients to evaluate the following symptoms: spontaneous pain in the back, in the legs, pain when moving in the back and legs, limited mobility when bending forward and when extending, restriction ability to sit, stand, limited mobility and daily activities; the patient assessed the severity of each of these symptoms, marking it with a point on a segment of 100 mm, with 0 on this segment corresponding to the absence of violations, and the opposite end - the maximum possible severity of the symptom; the overall score on this scale was determined by summing the length of 10 segments (in mm) and could range from 0 to 1000 [3].
The vertebral syndrome scale, which is a modification of the scale of G. Waddel et al. [3, 25], provided for assessment on a 4-point system (from 0 to 3 points) of 10 indicators: the angle of flexion and extension of the lumbar region, the angle of lateral tilt to the right and left, the angle of elevation of the straightened right and left leg, tension of the paravertebral muscles and severity scoliosis, the ability to support both straightened legs, sitting up in bed from a lying position; the total score ranged from 0 to 30 points.
The Neuropathic Pain Scale (NPS) [12], which allows assessing the severity of 10 characteristics of the pain syndrome: intensity, severity, severity of burning, dull, cold and itchy pain, skin sensitivity in the pain area, pain tolerance, intensity of superficial and deep pain.
The patients' condition was assessed at the time of inclusion in the study (MI), at the 4th (M4) and 8th week (M8). The primary endpoint was the dynamics of pain and limitation of mobility, assessed using the BBS, in relation to the initial level. Additionally, the dynamics of vertebral syndrome, neuropathic characteristics of pain, the degree of improvement on the CGI scale, as well as differences in the dynamics of symptoms depending on the timing of initiation of gabapentin therapy were assessed.
Statistical processing was carried out using descriptive methods and the ANOVA model. The assessment of changes in indicators in comparison with the baseline and the control group was carried out using a t-test (significance level p < 0.05). Statistical processing was carried out using the standard Statistica 6 software package.
results
By the end of the study, the BBS score significantly decreased in both groups (Table 1). By the 4th week, the total BBS score in the 1st group decreased by an average of 25%, in the second group - by 23%, by the end of the 8th week, the total BBS score decreased in the 1st group by 44% compared with the initial level, and in the 2nd group - by 37%. In the first 4 weeks. The use of gabapentin in the group with earlier prescription of the drug showed faster positive dynamics in back pain (both spontaneous and with movement) and the degree of limitation of the ability to move. By the end of the 8th week of the study, in both groups, significant positive dynamics were noted in the following indicators of BPS: spontaneous pain in the back and legs, pain in the back and legs when moving, limitation of extension and the ability to sit, limitation of the ability to move and daily activities.
There was a trend toward higher effectiveness of early administration of gabapentin (within 1 month after the onset of exacerbation) compared with its late administration. As a result, the indicators of the 2nd group, which were initially lower than the indicators of the 1st group, became equal to them by the end of the 8th week (Fig. 1).
Assessment of symptoms of neuropathic pain using the NPS scale (Table 2) showed that when treated with gabapentin, both groups showed positive dynamics in pain parameters such as its severity, intensity, including burning, superficial and deep pain, as well as pain tolerance. Moreover, if initially in the first group the indicators of neuropathic pain were higher (a significant difference was noted only in the overall intensity of pain), then by the end of the 4th and especially the 8th week the indicators in both groups were compared, which indicates a more rapid regression of pain in 1st group.
The severity of vertebral syndrome by the end of the 8th week decreased in both groups approximately equally (Table 3). However, according to these indicators, the trend towards higher scores in group 1 leveled out by the end of the study, and the corresponding indicators in both groups turned out to be close (Fig. 2).
According to the CGI scale, with early use of gabapentin by the end of the 8th week of the study, a significant effect was noted in 3 patients (25% of patients included in the study), satisfactory (moderate effect) - in 4 (34%), minimal improvement - in 2 (16%), lack of improvement - in 3 (25%). With late initiation of gabapentin treatment, a significant effect was observed in 2 (17%) patients, satisfactory in 4 (34%), minimal improvement in 4 (34%), and no effect in 3 (26%). Thus, with early use of gabapentin, a clinically significant result was observed in 59% of patients, whereas with later use - in 51% of patients. The effectiveness of therapy is not affected by age, initial pain intensity, the presence of prolapse symptoms, or the severity of vertebral syndrome.
The study showed good tolerability of gabapentin. Drowsiness was noted in 2 (8%) patients, dizziness - in 2 (8%), mild swelling of the legs - in 1 (4%). Gabapentin tolerability rates were similar in both groups.
Discussion
The results obtained confirm the effectiveness and safety of gabapentin in the treatment of the neuropathic component of pain in patients with discogenic lumbosacral radiculopathy. Moreover, they support the advisability of prescribing gabapentin as early as possible after the development of a painful episode.
Initial condition of patients with a pain episode lasting more than 1 month. in a number of parameters (severity of pain, degree of limitation of mobility) was more favorable than in patients with relatively recent development of pain, which probably reflects partial regression of symptoms under the influence of previous conservative therapy or the natural course of events. However, by the end of the study, the condition of patients in both groups was similar in most of the parameters assessed, which may reflect more rapid subsequent regression of symptoms with early initiation of gabapentin treatment. This can hardly be explained by the tendency towards spontaneous recovery, which is characteristic of a certain part of cases of radiculopathy, since in this case a more favorable course would be more likely to be expected in patients with a longer duration of exacerbation.
The use of agents acting on the α2δ subunit of calcium channels, primarily gabapentin, in patients with radiculopathy seems especially promising in light of experimental data that show that when a nerve is damaged (ligation or transection of the spinal roots or sciatic nerve) in rats as a result of up- regulation, overexpression of the α2δ subunit of calcium channels develops in the cells of the spinal cord and dorsal ganglia, which correlates with the phenomena of allodynia [18]. It can be assumed that a similar process occurs due to compression of the spinal root by a herniated disc. By selectively binding to the α2δ subunit of calcium channels, gabapentin inhibits the release of excitatory neurotransmitters and thereby blocks the transmission of pain impulses at the level of the dorsal horn, and possibly at higher levels of the central nervous system [8, 22]. Because of this, earlier use of gabapentin can counteract the development of central sensitization and the formation of “pain memory” that supports the pain syndrome, and thereby contribute to its regression [8].
To date, a number of clinical studies have been conducted on the effectiveness of gabapentin for back pain. Thus, N. Hansen [14], in an open study that included 80 patients with back pain, noted that when prescribing gabapentin in a dose of 900 to 2400 mg per day, a decrease in pain syndrome by an average of 46%. J. Rosenberg et al. [22] also found a positive effect of gabapentin on neuropathic pain syndromes. According to M. Saracoglu et al. [23], gabapentin was useful in patients with back pain that persisted after surgical treatment, providing persistent pain relief. But G. McClean [19] in a placebo-controlled study that included 62 patients with lumboischialgia, noted that while taking gabapentin at a dose of up to 1200 mg per day for 6 weeks. reduction in irradiation of pain in the leg and pain during movement, did not establish a decrease in lower back pain, improvement in mobility or reduction in the need for analgesics. K. Yildrim et al. [26] in a 2-month placebo-controlled study that included 50 patients with chronic radiculopathy, showed that taking gabapentin at a dose of 900–3600 mg per day helps reduce the intensity and radiation of pain, limited flexion and sensory impairment. Thus, the results of K. Yildrim et al. (2003) are closest to our findings.
As for other anticonvulsants, their effectiveness for back pain has not been sufficiently studied. Thus, one study [16] showed that topiramate (at an average dose of 200 mg per day) helps reduce pain in chronic radiculopathy by 20%, but at the cost of a high incidence of side effects (86%), as a result, only 16 completed the study ( 26%) of patients out of 42 who entered it. A small open-label study [11] showed a threshold therapeutic effect of lamotrigine for back pain, but this study also reported a high incidence of adverse events. Only one small open-label study [17] examined the effectiveness of carbamazepine in patients with sciatica. To date, there are also no evidence-based studies confirming the effectiveness of pregabalin, oxcarbazepine, valproic acid for lumbosacral radiculopathy or other types of back pain [10].
The variability in the results of these studies on the effectiveness of anticonvulsants for back pain may be explained, at least in part, by the heterogeneity of the studied groups of patients and the different timing of drug administration after the onset or exacerbation of pain. The peculiarity of our study is the relative homogeneity of the study population of patients (only patients with clinical and neuroimaging signs of discogenic radiculopathy were included, undoubtedly having a neuropathic component of pain), complexity in assessing the effectiveness of the drug and, what seems especially important, assessing the influence of the time of administration of the drug on its effectiveness.
However, one should be careful not to extrapolate the results obtained to the entire group of patients with back pain, most of whom do not have a neuropathic component of pain (so-called “axial back pain”). In recent years, some authors, based on the results obtained using special questionnaires, have expressed the opinion that the neuropathic component may be more widely represented than previously thought, including in cases of chronic back pain where there are no signs of involvement spinal roots. Meanwhile, questionnaires for identifying neuropathic pain should be considered only as a screening tool; due to lack of specificity, they cannot be considered a method for the final diagnosis of neuropathic pain, which, in accordance with modern, more stringent criteria, requires clinical and/or instrumental confirmation of damage to neural structures, in this case, the spinal roots or ganglia (for example, a decrease in pain, temperature, especially cold, tactile or vibration sensitivity in the corresponding dermatome or electrophysiological signs of root involvement) [15, 24].
In conclusion, it should be emphasized that our study should be considered preliminary, as the small number of patients and open-label nature limit the evidence of its results. Nevertheless, the data obtained may indicate the promise of early use of gabapentin in discogenic radiculopathy.
Side effects and other risks
Mechanism of side effects
Side effects are caused by blockade of voltage-gated calcium channels.
Side effects
- Sedation, dizziness
- Ataxia, fatigue, nystagmus, tremor
- Edema
- Blurred vision
- Nausea, diarrhea, constipation, dry mouth, dyspepsia
- In children under 12: emotional instability, increased mobility, impaired thinking
- Dangerous side effects: anaphylaxis and angioedema, suicidal ideation
- Weight gain: yes
- Sedation: yes, often; especially strong at high doses
What to do about side effects
- Wait;
- For sedation, take at night;
- Reduce dose;
- Switch to another drug [1].
Long term use
Safely
addictive
No.
Overdose
Confusion of speech, sedation, diarrhea, blurred vision
Side effects of the drug Gabapentin
From the cardiovascular system: increased blood pressure. From the gastrointestinal tract: dyspepsia, rarely - nausea, vomiting, abdominal pain, extremely rarely - dry mouth or pharynx, constipation, diarrhea, flatulence, anorexia, gingivitis, pancreatitis and increased activity of liver transaminases. When prescribed with other antiepileptic drugs - increased appetite. From the musculoskeletal system: rarely - myalgia, arthralgia. When prescribed with other antiepileptic drugs - back pain. From the nervous system : drowsiness, dizziness, ataxia, nystagmus (dose-dependent), fatigue, tremor, dysarthria, increased nervous excitability, rarely - headache, amnesia, depression, extremely rarely - impaired thinking, confusion, tics, paresthesia (dose-dependent) , asthenia, malaise, hyperkinesia; strengthening, hypo- or areflexia, anxiety, hostility. When prescribed simultaneously with other antiepileptic drugs - insomnia. From the respiratory system: rarely - rhinitis, pharyngitis. When prescribed together with other antiepileptic drugs - cough. From the genitourinary system: extremely rarely - urinary incontinence. When prescribed simultaneously with other antiepileptic drugs, there is a decrease in potency. From the senses: visual impairment (diplopia, amblyopia), ringing in the ears. From the hematopoietic organs: extremely rarely - leukopenia. Allergic reactions: extremely rarely - skin rash, itching, fever, erythema multiforme, exudative erythema malignant (Stevens-Johnson syndrome). Other: purpura, weight gain, extremely rarely - peripheral edema, discoloration of teeth, acne, facial swelling, fluctuations in glycemia in patients with diabetes. When prescribed simultaneously with other antiepileptic drugs, increased bone fragility.
Expert advice
Well studied as a remedy for cramps and neuralgia after shingles, but most often used off-label;
Off-label use is justified as a first-line remedy for neuropathic pain, a second-line remedy for anxiety;
There is not enough evidence for off-label use in bipolar disorder; lamotrigine has a stronger evidence base;
There is insufficient evidence for off-label use in schizophrenia [1].
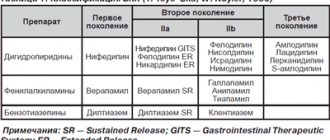
Pregabalin in the treatment of spondylogenic radiculopathy
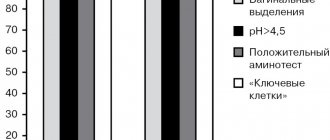
The main causes of radiculopathy are spinal canal stenosis, intervertebral disc herniation, spondylosis with the formation of osteophytes, hypertrophy of articular facets, ligaments, and less commonly - herpes zoster, diabetes mellitus, neuromas or other causes. It is known that the intensity of pain does not correlate with the degree of disc protrusion or the severity of root compression. The presence of a neuropathic component of pain significantly aggravates the course of back pain, contributes to its chronicity and rapid maladjustment of patients, disrupts their quality of life, increases treatment costs [10–12], and contributes to the development of insomnia, anxiety, and depression [13–15]. For many physicians, treating patients with chronic neuropathic pain remains a challenge [16]. Traditionally, for the treatment of back pain, most doctors use non-steroidal anti-inflammatory drugs (NSAIDs) [10–12], which relieve nociceptive pain well, but are ineffective for neuropathic pain that occurs with radiculopathies. The wrong choice of treatment tactics for patients with spondylogenic radiculopathies contributes to a decrease in its effectiveness and a significant increase in duration [18–20]. Recent systematic reviews indicate that among antidepressants, opioids and anticonvulsants used to treat neuropathic pain, gabapentin and pregabalin have the most favorable efficacy/tolerability ratio, making them currently the first choice drugs for the treatment of pain with a neuropathic component [16]. Pregabalin is a modern anticonvulsant and has established itself as an effective drug for the treatment of any neuropathic pain, fibromyalgia, anxiety and seizure syndrome. It is a g-aminobutyric acid analogue with high selectivity for the α-2-delta subunit of the neuronal voltage-gated calcium channel. In placebo-controlled clinical trials, pregabalin demonstrated not only high analgesic activity, but also effectiveness against concomitant mood disorders and insomnia in patients with peripheral diabetic polyneuropathy [23–26], postherpetic neuralgia [27–29], and spinal central neuropathic pain [30]. ]. In real clinical practice (“real world”), a study was conducted on the effectiveness of pregabalin in patients with cervical and lumbar radiculopathy [49]. This study showed that a more than 2-fold reduction in pain was observed in 63% of patients receiving pregabalin monotherapy and in 56% of patients receiving pregabalin as an addition to conventional therapy, which included NSAIDs, gabapentin, tranquilizers, amitriptyline and fentanyl [49]. (Fig. 1). A domestic study also demonstrated the high effectiveness of pregabalin in the treatment of neuropathic pain associated with spondylogenic lumbosacral radiculopathies [50]. According to the authors, in some patients, even in the presence of obvious signs of radiculopathy, the neuropathic component is not dominant in the structure of the pain syndrome, and therefore they recommend the mandatory use of the DN-4 questionnaire for the differential diagnosis of nociceptive and neuropathic pain in the structure of spondylogenic pain syndrome. These data confirm the previously obtained results of randomized controlled trials, in which the effectiveness of pregabalin was recorded in 39–48% of patients with diabetic polyneuropathy [23–26], in 28–50% with postherpetic neuralgia (27–29%) and in 22% patients with central neuropathic pain associated with spinal cord injury [30]. It has previously been shown that correction of mood disorders and insomnia associated with neuropathic pain can significantly reduce both direct and indirect costs of treating patients with neuropathic pain and improve their quality of life [47]. Given the frequent co-occurrence of chronic pain with the above-mentioned disorders, the role of pregabalin in their correction appears to be very useful, especially given the evidence that opioids, which are effective in treating neuropathic pain [16, 21], do not improve long-term emotional disorders and quality of life. life of patients [45, 46], and tricyclic antidepressants have a number of psychotropic side effects and anticholinergic effects, which significantly limit their use in a large category of patients. One previous study showed a positive effect of pregabalin on comorbid sleep disorders, depression and anxiety in patients with cervical and lumbosacral radiculopathy [49]. Of particular interest is the discussion of the effective average daily dose of pregabalin for the treatment of neuropathic pain. Randomized clinical trials using flexible dosing schedules have found that the effective therapeutic range of pregabalin for various neuropathic pain syndromes ranges from 150 to 600 mg/day. [26]. However, a number of studies conducted in real clinical practice have demonstrated high analgesic activity of pregabalin even at lower daily doses [20, 43]. For example, in patients with lumbar and cervical radiculopathies, an average of 190 mg of pregabalin per day was required to reduce pain by 2 times or more compared to the baseline period, while a dose of almost 2 times more [26]. Whether lower doses of pregabalin can be recommended in actual clinical practice remains unclear. Currently, individual selection of the dose of pregabalin seems to be the most effective and safe. The recent emergence of a dosage form containing 25 mg of the drug makes it possible to use a very flexible dosage regimen. It is important to understand that one should not rush to a negative assessment of the effectiveness of treatment of neuropathic pain and refuse to use pregabalin if its dose has not been increased to an individual maximum and well tolerated. A guideline can be the dose of 150–300 mg/day, indicated in the instructions for use of the drug. In cases of insufficient effectiveness and good tolerability of the drug, a second drug from another class can be added to it. It has been shown that the combined use of gabapentin and pregabalin with antidepressants significantly increases the effectiveness of treatment in patients with chronic pain and depression [16, 21]. The combined use of an anticonvulsant and an antidepressant in a number of patients can reduce the average daily dose of each of them and the risk of side effects [21]. Of particular interest for discussion is the question of the possibility and feasibility of combining an anticonvulsant and NSAIDs in patients with spondylogenic back pain and radiculopathy. The theoretical validity of this combination is beyond doubt, since the pathogenesis of most back pain syndromes involves the presence of both nociceptive and neuropathic pain mechanisms. There is evidence that the combined use of pregabalin and celecoxib was more effective than monotherapy with either drug in patients with chronic back pain [48]. In this study, the combination of pregabalin and celecoxib reduced chronic back pain by 38.2%, while pregabalin monotherapy reduced pain by 10.4% and celecoxib by 12.4%. The effectiveness of treatment for back pain largely depended on the presence of the neuropathic component of pain in the clinical picture, which was identified and assessed using the LANSS diagnostic questionnaire. More details: si-sv.com In patients with a pronounced neuropathic component of pain (LANSS >12 points), the maximum reduction in pain compared to the initial period (by 51.8%) was achieved only when using a combination of pregabalin and celecoxib (Fig. 2). In summary, there is now evidence that pregabalin monotherapy, and especially its combination with NSAIDs, is effective for the treatment of patients with chronic back pain and radiculopathy. The inclusion of pregabalin in the treatment regimen of patients with this pathology not only promotes more effective pain relief, but also reduces the symptoms of anxiety and insomnia that often accompany chronic pain.
References 1. Verhaak PF, Kerssens JJ, Dekker J. et al. Prevalence of chronic benign pain disorder among adults: a review of the literature // Pain. 1998. Vol. 77(3). P. 231–239. doi: 10.1016/S0304–3959(98)00117–1. 2. Lawrence RC, Helmick CG, Arnett FC et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States // Arthritis. Rheum. 1998. Vol. 41(5). P. 778–799. 3. Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature // Spine. 1999. Vol. 24(17). P. 1813–1819. 4. Elliott AM, Smith BH, Penny KI et al. The epidemiology of chronic pain in the community // Lancet. 1999. Vol. 354(9186). P. 1248–1252. 5. Donk J., Schouten JSAG, Passchier J. et al. The association of neck pain with radiological abnormalities of the cervical spine and personality traits in a general population // J. Rheumatol. 1991. Vol. 18. P. 1884–1889. 6. Cote P., Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults // Spine. 1998. Vol. 23(15). P. 1689–1698. 7. Webb R., Brammah T., Lunt M. et al. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population // Spine. 2003. Vol. 28(11). P. 1195–1202. 8. Carey TS, Evans AT, Hadler NM et al. Acute severe low back pain. A population-based study of prevalence and care-seeking // Spine. 1996. Vol. 21(3). P. 339–344. 9. Loney PL, Stratford PW The prevalence of low back pain in adults: a methodological review of the literature // Phys. Ther. 1999. Vol. 79(4). P. 384–396. 10. Berger A., Dukes EM, Oster G. Clinical characteristics and economic costs of patients with painful neuropathic disorders // J. Pain. 2004. Vol. 5(3). P. 143–149. 11. McDermott AM, Toelle TR, Rowbotham DJ et al. The burden of neuropathic pain: results from a cross-sectional survey // Eur. J. Pain. 2006. Vol. 10(2). P. 127–135. 12. Lachaine J., Gordon A., Choiniere M. et al. Painful neuropathic disorders: an analysis of the Regie de l'Assurance Maladie du Quebec database // Pain Res. Manag. 2007. Vol. 12(1). P. 31–37. 13. Smith MT, Haythornthwaite JA How do sleep disturbances and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature // Sleep. Med. Rev. 2004. Vol. 8(2). P. 119–132. 14. Rush AJ, Polatin P., Gatchel RJ Depression and chronic low back pain: establishing priorities in treatment // Spine. 2000. Vol. 25(20). P. 2566–2571. 15. McWilliams LA, Goodwin RD, Cox BJ Depression and anxiety associated with three pain conditions: results from a nationally representative sample // Pain. 2004. Vol. 111(1–2). P. 77–83. 16. Finnerup NB, Otto M, McQuay HJ et al. Algorithm for neuropathic pain treatment: an evidence based proposal // Pain. 2005. Vol. 118(3). P. 289–305. 17. Harden N., Cohen M. Unmet needs in the management of neuropathic pain // J. Pain Symptom Manage. 2003. Vol. 25(Suppl. 5).S.12–S17. 18. Tolle T., Xu X., Sadosky AB Painful diabetic neuropathy: a cross-sectional survey of health state impairment and treatment patterns // J. Diabetes Complications. 2006. Vol. 20(1). P. 26–33. 19. Tolle T., Dukes E., Sadosky A. Patient burden of trigeminal neuralgia: results from a cross-sectional survey of health state impairment and treatment patterns in six European countries // Pain Pract. 2006. Vol. 6(3). P. 153–160. 20. Seventer R., Sadosky A., Lucero M., Dukes E. A cross-sectional survey of health state impairment and treatment patterns in patients with postherpetic neuralgia // Age Ageing. 2006. Vol. 35(2). P. 132–137. 21. Argoff CE The coexistence of neuropathic pain, sleep, and psychiatric disorders: a novel treatment approach // Clin. J. Pain. 2007. Vol. 23(1). P. 15–22. 22. Tassone DM, Boyce E., Guyer J., Nuzum D. Pregabalin: a novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders // Clin. Ther. 2007. Vol. 29(1). P. 26–48. 23. Rosenstock J., Tuchman M., LaMoreaux L., Sharma U. Pregabalin for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial // Pain. 2004. Vol. 110(3). P. 628–638. 24. Lesser H., Sharma U., LaMoreaux L., Poole RM Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trialm // Neurol. 2004. Vol. 63(11). P. 2104–2110. 25. Richter RW, Portenoy R, Sharma U et al. Relief of diabetic painful peripheral neuropathy with pregabalin: a randomized, placebo-controlled trial // J. Pain. 2005. Vol. 6(4). P. 253–260. 26. Freynhagen R., Strojek K., Griesing T. et al. Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomized, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens // Pain. 2005. Vol. 115(3). P. 254–263. 27. Dworkin RH, Corbin AE, Young JP Jr et al. Pregabalin for the treatment of postherpetic neuralgia: a randomized, placebo-controlled trial // Neurol. 2003. Vol. 60(8). P. 1274–1283. 28. Sabatowski R, Galvez R, Cherry DA et al. 1008–045 Study Group Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: results of a randomized, placebo-controlled clinical trial // Pain. 2004. Vol. 109(1–2). P. 26–35. 29. Seventer R, Feister HA, Young JP Jr et al. Efficacy and tolerance of twice-daily pregabalin for treating pain and related sleep interference in postherpetic neuralgia: a 13-week, randomized trial // Curr. Med. Res. Opin. 2006. Vol. 22(2). P. 375–384. 30. Siddall PJ, Cousins MJ, Otte A. et al. Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial // Neurol. 2006. Vol. 67(10). P. 1792–1800. 31. Saldaña MT, Navarro A., Pérez C. et al. Health, non-health resource utilization and costs of treating refractory painful Radiculopathy in Primary Care Settings (PCS) under routine medical practice in Spain // Value Health. 2007.10:A464. Abstract. 32. Bouhassira D., Attal N., Fermanian J. et al. Development and validation of the Neuropathic Pain Symptom Inventory // Pain. 2004. Vol.108(3). P. 248–257. 33. Bouhassira D., Attal N., Alchaar H. et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4) // Pain. 2005. Vol.114(1–2). P. 29–36. 34. Perez C., Galvez R., Huelbes S. et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component // Health Qual. Life Outcomes. 2007. Vol. 5. P. 66. 35. Melzack R. The short-form McGill Pain Questionnaire // Pain. 1987. Vol. 30(2). P. 191–197. 36. Sheehan DV, Harnett-Sheehan K., Raj BA The measurement of disability // Int. Clin. Psychopharmacol. 1996. Vol. 11(Suppl. 3). P. 89–95. 37. Hays RD, Stewart AL Sleep measures/Stewart AL, Ware JE, ed. Measuring functioning and well-being: The Medical Outcomes Study approach. – Durham, NC: Duke University Press; 1992. P. 235–259. 38. Rejas J., Ribera MV, Ruiz M., Masrramon X. Psychometric properties of the MOS (Medical Outcomes Study) Sleep Scale in patients with neuropathic pain // Eur. J. Pain. 2007. Vol. 11(3). P. 329–340. 39. Zigmond AS, Snaith RP The hospital anxiety and depression scale // Acta Psychiatr. Scand. 1983. Vol. 67(6). P. 361–370. 40. TheEuroQol Group EuroQol – a new facility for the measurement of health-related quality of life // Health Policy. 1990. Vol. 16(3). P. 199–208. 41. Kazis LE, Anderson JJ, Meenan RF Effect sizes for interpreting changes in health status // Med. Care. 1989. Vol. 27. S.178–S189. 42. Brooks R. EuroQoL: the current state of play // Health. Policy. 1996. Vol. 37. P. 53. 43. Gore M., Dukes E., Rowbotham DJ et al. Clinical characteristics and pain management among patients with painful peripheral neuropathic disorders in general practice settings // Eur. J. Pain. 2007. Vol. 11(6). P. 652–664. 44. Rodriguez MJ, Garcia AJ A Registry of the Aetiology and Costs of Neuropathic Pain in Pain Clinics: Results of the Registry of Etiologies and Costs (REC) in Neuropathic Pain Disorders Study // Clin. Drug. Investig. 2007. Vol. 27(11). P. 771–782. 45. Watson CP, Moulin D, Watt-Watson J et al. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy // Pain. 2003. Vol. 105(1–2). P. 71–78. 46. Gimbel JS, Richards P., Portenoy RK Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial // Neurol. 2003. Vol. 60(6). P. 927–934. 47. Ritzwoller DP, Crounse L., Shetterly S., Rublee D. The association of comorbidities, utilization and costs for patients identified with low back pain // BMC Musculoskelet. Discord. 2006. Vol. 7. P. 72. 48. Romano CL, Romano D., Bonora C., Mineo G. Pregabalin, celecoxib, and their combination for the treatment of chronic low-back pain // J. Orthop. Traumatol. 2009. Vol. 10 (4). P. 185–191. 49. Saldana MT, Navarro A, Perez C et al. Patient-reported-outcomes in subjects with painful lumbar or cervical radiculopathy treated with pregabalin: evidence from medical practice in primary care settings // Rheumatol. Int. 2010. Vol. 30 (8). P. 1005–1015. 50. Khabirov F.A., Esin R.G., Kochergina O.S. Pregabalin in the treatment of vertebrogenic radicular pain // Consilium Medicum (add. “Neurology”). 2011. No. 15. pp. 36–41.