Home | About us | Delivery | Advertisers | Login | Registration
The pharmacy is closed on Sundays and holidays.
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2021 Pharmacy 84.
URAPIDIL J
The drug Urapidil J is administered intravenously as a bolus or by long-term intravenous infusion - in the supine position.
Hypertensive crisis, refractory and severe arterial hypertension
Intravenous bolus administration
The drug Urapidil J in a dose of 10-50 mg is administered intravenously, slowly, under constant monitoring of blood pressure. A decrease in blood pressure is expected within 5 minutes. after introduction. Depending on the therapeutic effect, repeated administration of the drug is possible.
Intravenous drip infusion or continuous infusion using a perfusion pump
Maintenance dose (on average) - 9 mg/h, i.e. 250 mg of Urapidil J (10 ampoules of 5 ml or 5 ampoules of 10 ml) are dissolved in 500 ml of solution for infusion (1 mg = 44 drops ~ 2.2 ml). The maximum permissible ratio is 4 mg of Urapidil J per 1 ml of solution for infusion. The maximum initial rate of administration is 2 mg/min (depending on blood pressure).
The rate of drip administration depends on the patient’s blood pressure.
A solution for drip infusion intended to maintain blood pressure is prepared as follows: usually 250 mg of the drug (10 ampoules of 5 ml or 5 ampoules of 10 ml) is added to 500 ml of solution for infusion, for example, 0.9% sodium chloride solution, 5 % or 10% dextrose (glucose) solution.
If a perfusion pump is used to administer a maintenance dose, then 100 mg of the drug (4 ampoules of 5 ml, or 2 ampoules of 10 ml, or 1 ampoule of 20 ml) is injected into the syringe of the perfusion pump and diluted to 50 ml with 0.9% sodium solution chloride, 5 or 10% dextrose (glucose) solution.
Managed hypotension during and/or after surgery
Continuous
infusion with a perfusion pump or drip infusion is used to maintain blood pressure at the level achieved with intravenous administration.
Notes.
If other antihypertensive drugs have previously been used, then Urapidil J can be administered only after a period of time sufficient for the previously administered drug(s) to take effect. The dose of Urapidil J should be adjusted accordingly.
The drug is administered intravenously as injections or infusions with the patient lying on his back. Administration of the drug can be single or multiple. Injection administration of the drug can be combined with subsequent drip infusion. Parenteral therapy can be repeated if there is a new increase in blood pressure.
Elderly patients
Caution must be exercised when using antihypertensive drugs in elderly patients. The initial dose should be reduced compared to the recommended one, since elderly patients often experience a change in sensitivity to drugs of this pharmacological class (volume of distribution is reduced and T1/2 is increased).
Patients with impaired liver and/or kidney function
In patients with impaired liver and/or kidney function, a reduction in the initial dose of the drug may be required compared to the recommended doses.
Duration of therapy
Therapy for 7 days is safe, but, as a rule, when administering antihypertensive drugs parenterally, this period should not be exceeded.
If blood pressure rises again, parenteral therapy may be resumed. It is possible to initiate continuous therapy with oral antihypertensive drugs at the same time as emergency parenteral therapy. If other antihypertensive drugs have previously been used, then Urapidil J can be administered only after a period of time sufficient for the previously administered drug(s) to take effect. The dose of Urapidil J should be adjusted accordingly.
Special precautions for handling
Before administration, the ampoule should be inspected for the presence of suspended particles and discoloration. Only a clear, colorless solution should be injected.
The drug Urapidil J cannot be mixed with alkaline solutions for injections and infusions (it can lead to turbidity and the formation of a flocculent sediment).
The drug should not be mixed with other drugs with the exception of: 0.9% sodium chloride solution for infusion, 5% or 10% dextrose (glucose) solution. After opening the ampoule, the drug solution should be administered immediately.
Journal "Emergency Medicine" 5(30) 2010
Introduction
Arterial hypertension (HTN) is a well-known risk factor for cardiovascular disease and a leading cause of death worldwide.
According to the Global Burden of Disease study conducted by the World Health Organization, inadequate blood pressure (BP) control is recognized as a leading cause of death in both developed and developing countries [1]. Today, a doctor has a wide selection of effective pharmacological agents for the treatment of arterial hypertension at his disposal. However, despite this, blood pressure control often remains inadequate, and the number of people with uncontrolled blood pressure is constantly increasing [2]. A large number of studies have shown that many patients with hypertension are either not treated at all or are treated, but target blood pressure levels are not achieved. As part of an analysis of surveys on hypertension conducted in several countries, it was found that in Europe less than 1/3 of patients with blood pressure ≥ 140/90 mm Hg. receive antihypertensive treatment, only 23–38% manage to reduce blood pressure below 160/95 mmHg, and less than 10% - below 140/90 mmHg. [3]. Similar data were obtained in another international survey of patients with arterial hypertension: blood pressure control was observed in only 1/3 of patients [4]. Other studies have also reported similar findings of low rates of effective BP control [5, 6]. Inadequate reduction of blood pressure is a problem in all patients with hypertension, but is of particular importance in people at high risk of developing complications - those who suffer from type 2 diabetes mellitus or chronic renal failure [2].
Data from randomized trials suggest that the main benefit of antihypertensive therapy is directly related to blood pressure reduction, regardless of which drug is used for this purpose [7]. A meta-analysis of 147 randomized trials found that five major classes of BP-lowering drugs (thiazides, beta-blockers, angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), and calcium channel blockers) were equally effective in reducing the incidence of development of complications of coronary heart disease (fatal and non-fatal myocardial infarctions, with the exception of “silent” heart attacks, and sudden cardiac death) and strokes at a given level of blood pressure reduction. The only exception was the small additional protective effect of calcium channel blockers against stroke [8]. All classes of antihypertensive drugs have different properties, and therefore certain drugs may be more preferable in certain groups of patients. In particular, patients with hypertension often have multiple associated risk factors (eg, diabetes, hyperlipidemia), which may influence the choice of therapy [9].
Use of alpha blockers for hypertension
Most patients with hypertension require a combination of two or more drugs to achieve target blood pressure levels [7]. In this regard, the choice of second-line therapy drugs is of particular importance. Many drug combinations have been shown to be effective and well tolerated [7].
Alpha-1 adrenergic receptor antagonists (alpha-blockers) have a hypotensive effect much like that of other antihypertensive drugs [10]. A number of studies have shown that the administration of alpha-blockers as adjunctive therapy led to an effective reduction in blood pressure in patients with inadequately controlled hypertension [11]. In addition to their effect on blood pressure, alpha blockers have other positive effects - they improve the lipid profile and glucose metabolism, and reduce the symptoms of benign prostatic hyperplasia (BPH) [11]. These effects may be of particular importance for many patients, especially in older age.
Urapidil (Ebrantil, Nycomed) has alpha-blocking properties, but, unlike other alpha-blockers, it also has a central hypotensive effect [12]. Urapidil (Ebrantil) is available as long-acting oral capsules (for the treatment of hypertension) and as an intravenous solution (for the treatment of hypertensive crises, severe or treatment-resistant hypertension, perioperative and postoperative hypertension, and preeclampsia). A review was previously published that covered the pharmacodynamics, pharmacokinetics and therapeutic efficacy of urapidil (Ebrantil) in comparison with other antihypertensive drugs [13]. In this review, we focused on the potential role of urapidil (Ebrantil) as an additional agent in combination therapy for arterial hypertension, when prescribed to patients with arterial hypertension and the presence of concomitant diseases, and in the relief of hypertensive crises - situations in which the use of urapidil (Ebrantil) ) is the most shown.
A large amount of data has accumulated that urapidil (Ebrantil) effectively reduces blood pressure in patients with hypertension.
Effects of urapidil (Ebrantil) in patients with type II diabetes mellitus, hyperlipidemia
Patients with hypertension often have multiple underlying metabolic disorders, including diabetes mellitus and hyperlipidemia. Concomitant diabetes significantly increases the risk of developing damage to the kidneys and other organs, leading to increased cardiovascular morbidity and mortality. In this regard, more stringent blood pressure control (<130/80 mmHg) is recommended in patients with diabetes mellitus, and the prescription of combination antihypertensive therapy becomes particularly relevant here [7]. However, some antihypertensive drugs are known to have diabetogenic effects. For example, beta blockers and thiazide diuretics increase insulin resistance and increase the incidence of new-onset diabetes mellitus compared with other antihypertensive agents [19, 20]. In addition, beta-blockers and diuretics have adverse effects on plasma lipid levels and are therefore not recommended for use as first-line therapy in patients with diabetes, hyperlipidemia, and associated metabolic disorders (eg, metabolic syndrome) [7]. Calcium channel blockers, ACEIs, and ARBs are thought to have minimal or no effect on metabolic parameters. However, alpha blockers may have a positive effect on both glucose and lipid metabolism [11]. To date, there have been studies on the use of urapidil (Ebrantil) in patients with type 2 diabetes mellitus and/or hyperlipidemia.
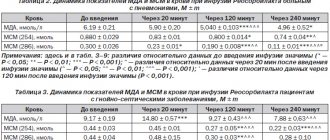
A large randomized trial included 309 patients with type 2 diabetes mellitus and mild to moderate hypertension. All patients were prescribed urapidil (Ebrantil) at a dose of 60 (n = 157) or 120 mg/day (n = 152) for 4 weeks [21]. The results showed that at the end of the 4th and 16th weeks, blood pressure was reduced in both treatment groups. In addition, during treatment with urapidil (Ebrantil) in both doses - 60 and 120 mg / day - the content of fasting glucose and glycosylated hemoglobin (HbA1c) levels decreased (Fig. 1). Additional administration of a thiazide diuretic did not cause any changes in the assessed parameters. Treatment with urapidil (Ebrantil) was also associated with significant reductions in total cholesterol, low-density lipoprotein (LDL) cholesterol and triglycerides, as well as a significant increase in high-density lipoprotein (HDL) cholesterol. The observed lipid-lowering effect was dose-dependent, with a significantly greater reduction in triglyceride levels in patients receiving a higher dose of the drug. Prescription of a thiazide diuretic to persons insensitive to treatment with urapidil (Ebrantil) led to a significant increase in total cholesterol and a significant decrease in HDL cholesterol.
Another study involved 33 patients with type 2 diabetes mellitus and diastolic blood pressure of 95–115 mmHg. They were prescribed urapidil (Ebrantil) at a dose of 60 or 120 mg/day, and then the dose was gradually increased (maximum value 180 mg/day) in order to reduce diastolic blood pressure < 90 mmHg. or a decrease in blood pressure while sitting by at least 10% [22]. As a result, over 12 weeks of treatment, there was a significant decrease (p < 0.0001) in systolic blood pressure (SBP) and diastolic blood pressure (DBP) in the sitting and standing position, while heart rate (HR) did not increase.
In contrast to the study by Fariello et al. [21] in another study, there was no positive effect of urapidil (Ebrantil) on HbA1c levels. The ratio of insulin to glucose (HOMA index - Editor's note), used as an indirect marker of insulin resistance, was significantly lower after treatment with urapidil (Ebrantil) at a dose of 60-180 mg. Consequently, urapidil (Ebrantil) improves insulin sensitivity, since patients taking this drug require less endogenous insulin to maintain the same glucose levels.
Urapidil (Ebrantil) had a positive effect on the lipid profile in patients with concomitant hyperlipidemia. In one study involving patients with hypertension and hyperlipidemia, treatment with urapidil (Ebrantil) at a dose of 30–90 mg/day for 12 weeks led to significant improvements in total cholesterol, LDL cholesterol and apolipoprotein B [23]. In another study, including patients with hypertension and hypercholesterolemia, the administration of urapidil (Ebrantil) showed a tendency to reduce total cholesterol and LDL cholesterol, while in the placebo group these indicators slightly increased [24].
In a retrospective analysis of six clinical studies, it was found that treatment with urapidil (Ebrantil) at a dose of 120 mg/day for 3 months led to a significant decrease in total cholesterol (n = 427, -5.9%; p < 0.0001) and triglycerides (n = 64, –18.2%; p < 0.0001) [25]. LDL cholesterol also decreased (n = 21, –13.9%), while HDL cholesterol increased (n = 52, 12.3%) (Fig. 2).
The Zanchetti study [14] reported that urapidil (Ebrantil) had beneficial effects in a subgroup of patients with baseline total cholesterol ≥ 240 mg/dL. In the group receiving nifedipine + urapidil (Ebrantil), total cholesterol decreased by 8% and LDL cholesterol by 12%, while in the group receiving nifedipine + metoprolol, total cholesterol increased by 7% and LDL cholesterol by 10 %. In the entire study population, which included patients with or without hypercholesterolemia, the addition of urapidil (Ebrantil) led to a significant decrease in the levels of total cholesterol and LDL cholesterol (p < 0.001), and the addition of metoprolol led to a significant increase (p = 0.001) in these indicators (p <0.01 between the two treatment groups). The content of triglycerides did not change in the group receiving nifedipine + urapidil (Ebrantil), but significantly increased in the group receiving nifedipine + metoprolol (p < 0.001); intergroup differences were not significant. In addition, plasma glucose remained unchanged in the nifedipine + urapidil (Ebrantil) group, but increased significantly in the nifedipine + metoprolol group (p < 0.001); intergroup differences were not significant. In patients initially randomized to metoprolol, high levels of total cholesterol, LDL cholesterol and glucose decreased when switched to treatment with urapidil (Ebrantil).
Other effects of urapidil (Ebrantil)
In one study, patients with hypertension were randomized to double-blind treatment with urapidil (Ebrantil) at a dose of 120 mg/day or atenolol at a dose of 50 mg/day. As a result, a positive effect of urapidil (Ebrantil) on fibrinogen levels was found - after 12 weeks of treatment in the group with urapidil (Ebrantil), the fibrinogen content decreased by 24%, while in the group with atenolol it decreased by only 9% [29]. Plasminogen activator inhibitor activity decreased by 4% in the urapidil (Ebrantil) group and increased by 17% in the atenolol group, although these differences were not significant. A number of previous studies have indicated a correlation between plasma fibrinogen levels and subsequent development of heart attacks or strokes [30, 31].
Some studies have demonstrated a dose-dependent inhibitory effect of urapidil (Ebrantil) on platelet aggregation in vitro, in healthy volunteers and patients with hypertension [32–34]. However, the clinical significance of these data is unclear.
Urapidil (Ebrantil) has also been shown to effectively combat symptoms of BPH and can be used to prevent dysfunction in patients with neurogenic bladder [36, 37]. Indications for the use of alpha blockers include the treatment of BPH, a disease often found in older men with hypertension [7]. In addition, the combination of urapidil (Ebrantil) and cholinergic agents has been shown to be more effective in the treatment of detrusor insufficiency than monotherapy with either agent [38]. Urapidil (Ebrantil) did not cause significant changes in glomerular filtration rate in patients with normal renal function and did not lead to further renal impairment in a small study in patients with moderate/severe renal impairment [39]. Urapidil (Ebrantil) has been reported to reduce vascular resistance in the kidneys and increase renal blood flow in patients with hypertension [40].
Antihypertensive effects with long-term use of urapidil (Ebrantil)
Long-term use of urapidil (Ebrantil) is not addictive. In one study, 830 patients received urapidil (Ebrantil) at a dose of 60–180 mg per day for 2 years, and no addiction was observed [42]. In an open multicenter study that included 182 patients, after 1 year of treatment with urapidil (Ebrantil) at a dose of 60–180 mg/day, SBP decreased by 25 mmHg, DBP by 17 mmHg. [43]. During the 2nd and 3rd years of treatment with urapidil (Ebrantil) at the same average doses, retention of the achieved reduction in blood pressure was observed. This indicates that the effect of urapidil (Ebrantil) did not weaken over time. In another study, which included 73 patients, the reduction in blood pressure achieved with urapidil (Ebrantil) at a dose of 30–120 mg/day was maintained without developing the phenomenon of addiction for 3 years [44].
Therapeutic effects of urapidil (Ebrantil) when administered intravenously
Hypertensive crisis
Hypertensive crisis is an acute increase in blood pressure, which in some cases is accompanied by acute damage to target organs [45]. Hypertensive crises that occur with acute damage to target organs can be life-threatening and therefore require a rapid reduction in blood pressure. A number of antihypertensive drugs are used to relieve hypertensive crises, although there is virtually no data on the most optimal drugs [46].
Intravenous administration of urapidil (Ebrantil) leads to the development of a rapid antihypertensive effect (within 2 minutes) without reflex tachycardia. This suggests that the drug may be useful in relieving hypertensive crises. For example, French national guidelines recommend the use of intravenous infusions of urapidil (Ebrantil) to relieve hypertensive crises that occur with acute target organ damage [47]. Austrian guidelines recommend its use as a first-line drug [48].
A number of studies have demonstrated that intravenous administration of urapidil (Ebrantil) is an effective and safe method for treating hypertensive crises [49–52]. Other studies have shown that intravenous urapidil (Ebrantil) is associated with greater effectiveness compared with other antihypertensive agents.
The study [54] compared the effectiveness of intravenous administration of urapidil (Ebrantil) at a dose of 25 mg (n = 48), intravenous administration of enalaprilat at a dose of 5 mg (n = 43), and sublingual administration of nifedipine capsules at a dose of 10 mg (n = 47) and sublingual spraying of two doses of nifedipine spray 5 mg (n = 30). All patients were admitted to the emergency department with a hypertensive crisis without acute end organ damage (SBP > 210 mm Hg and/or DBP > 110 mm Hg) or with a hypertensive crisis and the presence of acute end organ damage ( DBP > 100 mm Hg and signs of acute target organ damage) [54]. The highest sensitivity to treatment (96%) was recorded with intravenous administration of urapidil (Ebrantil). With the introduction of enalaprilat it was 70%, nifedipine spray - 71% and nifedipine capsules - 72%. The authors concluded that urapidil (Ebrantil) should be used as first-line therapy in patients with hypertensive crisis. Another randomized trial of 81 patients with hypertensive crisis and the presence of acute end-organ damage (DBP > 110 mmHg and signs of acute end-organ damage) showed that treatment sensitivity with intravenous urapidil (Ebrantil) was the same as with intravenous sodium nitroprusside (89 and 97%; p = 0.18) [55]. However, only 2% of patients in the urapidil (Ebrantil) group experienced a re-increase in blood pressure within 4 hours after the crisis ended, compared with 24% of patients in the nitroprusside group. In addition, major side effects were more often observed in the group with nitroprusside than with urapidil (Ebrantil) (in 7 and 2 patients; p = 0.04).
Preeclampsia and eclampsia
Two studies reported that intravenous urapidil (Ebrantil) and dihydralazine were equally effective in lowering blood pressure in women with preeclampsia. However, urapidil (Ebrantil) had more predictable hemodynamic effects and was better tolerated [58, 59]. In another study, intravenous urapidil (Ebrantil) for the treatment of preeclampsia was associated with less effect on neonatal cardiovascular parameters compared with intravenous dihydralazine [60]. In Europe, dihydralazine is no longer recommended for the treatment of hypertension in preeclampsia because it is associated with a high number of perinatal side effects. Guidelines from Austria, France and Germany recommend intravenous urapidil (Ebrantil) for the treatment of preeclampsia [47, 48, 61].
Perioperative hypertension
Intravenous urapidil (Ebrantil) has been shown to be effective in reducing episodes of perioperative hypertension in patients undergoing a variety of surgical procedures, particularly on the coronary arteries [62–70]. Intravenous administration of urapidil (Ebrantil) is used to treat episodes of hypertension during operations on the abdominal aorta [71], during neurosurgical interventions [72], during tracheal intubation during general anesthesia [73], as well as to prevent episodes of hypertension in patients preparing for to surgery for pheochromocytoma [74].
Strokes and intracerebral hemorrhages
When administered intravenously, urapidil (Ebrantil) has been reported to be more effective than nifedipine in lowering blood pressure and reducing cerebral symptoms in patients with hypertensive crisis and acute end-organ damage [75]. In general, the decrease in blood pressure with the administration of urapidil (Ebrantil) is not associated with an increase in intracranial pressure and cerebral perfusion is not impaired [76]. Urapidil (Ebrantil) administered intravenously is one of the drugs recommended by European guidelines for lowering blood pressure in acute strokes [77].
The Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage study (INTERACT) showed that early aggressive blood pressure lowering was well tolerated and resulted in reduced hematoma growth in patients with intracerebral hemorrhage compared with standard approaches. to lower blood pressure [78]. Of the 207 patients randomized to aggressive blood pressure lowering, almost half (47%) received urapidil (Ebrantil). Hematoma growth is a strong predictor of poor outcomes in intracerebral hemorrhage. Therefore, these results support the hypothesis that early aggressive BP lowering is an important therapeutic intervention in these patients.
Portability and safety
The tolerability of urapidil (Ebrantil) was discussed in a previously published review [13]. In general, the drug is well tolerated. Side effects reported in clinical studies were mild and temporary, mainly occurring in the first week of therapy and disappearing with continued treatment. These include dizziness, nausea, headaches, fatigue and orthostatic disorders. In general, when treated with urapidil (Ebrantil), the incidence of side effects was comparable to that when prescribing other antihypertensive drugs [13]. However, due to the dual mechanism of action, a lower incidence of tachycardia and orthostatic hypertension is observed when using urapidil (Ebrantil) compared to other alpha blockers. The safety profile of urapidil (Ebrantil) when combined with other drugs is the same as with monotherapy with urapidil (Ebrantil). In the Zanchetti study [14], the most common side effects were gastrointestinal complications, fatigue, headache and palpitations (1 to 2% of patients). Orthostatic hypotension was not observed. In addition, taking urapidil (Ebrantil) did not increase the risk of heart failure.
Discussion
Achieving BP control remains challenging despite the availability of a large number of effective antihypertensive agents and the widespread use of combination therapy. Alpha blockers may be recommended to lower blood pressure in patients whose hypertension has not been adequately controlled with other antihypertensive agents. Alpha blockers have a number of other benefits, including improving lipid profiles and glucose metabolism and reducing symptoms of BPH [11]. Therefore, alpha blockers should be considered as second and subsequent line therapy in the treatment of hypertension, especially in patients with concomitant metabolic disorders and BPH.
Alpha blockers have become less commonly used to treat hypertension following the release of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) study, which reported an increased risk of chronic heart failure. (CHF) among patients randomized to treatment with doxazosin (as a first-line drug) compared with chlorthalidone [79]. However, CHF was not a predefined single endpoint in this study, but was a component of a composite secondary endpoint. In addition, the diagnostic criteria for CHF (one symptom and one sign) do not correspond to current practice, which may explain the very high incidence of clinically documented CHF (5.35 and 8.89% at 4 years when treated with chlorthalidone and doxazosin, respectively), and also the same distribution and low frequency of the “severe” end point - death from CHF (0.60 and 0.65% per 4 years, respectively) [80]. Despite criticism of the study, its data led to the fact that a number of guidelines stopped recommending alpha blockers for use (for example, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [JNC-VII ] (Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure), 2003 [81]), although some others (eg, European Society of Cardiology [ESC]/European Society of Hypertension [ESH] Society of Cardiology/European Society of Hypertension), 2007 [7]) note their potential when used as adjunctive therapy or in special groups of patients. More recently, the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) reported that doxazosin was effective and safe as third-line therapy and did not increase the incidence of heart failure [82]. In this study, heart failure was a predefined secondary endpoint and was assessed using more stringent criteria than in the ALLHAT study. After adding doxazosin to antihypertensive therapy, after 12 months of treatment, mean blood pressure decreased by 11.7/6.9 mmHg. (p < 0.0001) from 158.7/89.2 mmHg, and 29.7% of patients achieved the target blood pressure level. Administration of doxazosin was associated with a small positive effect on the plasma lipid profile, although a small increase in fasting plasma glucose was also reported. In an observational study of doxazosin prescribed as an additional antihypertensive agent in patients with CHF, no increase in complications of CHF was found [84].
The main effect of urapidil (Ebrantil) is associated with its alpha-blocking effect. However, it also has central sympatholytic effects mediated by stimulation of serotonin 5HT1A receptors in the central nervous system (Figure 3). The agonistic effect of urapidil (Ebrantil) on 5HT1A receptors leads to a decrease in the impulse activity of serotonergic neurons, which inhibits their excitatory inputs to sympathetic neurons. Such inhibition reduces the activity of the sympathetic nervous system at the receptor level [12]. In addition to contributing to a decrease in peripheral resistance, a decrease in sympathetic tone suppresses the development of reflex tachycardia, which often accompanies vasodilation therapy [12].
Research data indicate that urapidil (Ebrantil) either does not lead to changes in heart rate at all, or there is a slight transient increase in this parameter [13, 84, 85]. In a randomized, double-blind, placebo-controlled crossover study of 12 healthy male volunteers, doxazosin but not urapidil (Ebrantil) (p < 0.05) significantly increased resting heart rate, although both drugs were equally effective in lowering blood pressure. [86]. In addition, doxazosin, but not urapidil (Ebrantil), significantly increased the product of heart rate and resting pressure (Robinson index - editor's note), which suggests that doxazosin's increase in heart rate is more pronounced than its reducing effect on SBP. The authors concluded that this may be the reason why higher rates of heart failure and stroke were observed with doxazosin compared with chlorthalidone in the ALLHAT trial.
Unlike other antihypertensive agents, alpha blockers, including urapidil (Ebrantil), may have a positive effect on glucose and lipid metabolism and may therefore be particularly useful in a large number of patients with hypertension and concomitant type 2 diabetes mellitus, metabolic syndrome and/or or hyperlipidemia. It is difficult to achieve target blood pressure levels in these patients, even with combination therapy, and alpha blockers may be very helpful. In addition, urapidil (Ebrantil) has a positive effect on symptoms in patients with BPH and neurogenic bladder dysfunction. These effects of alpha-blockers may be of particular importance in older patients with hypertension, given the greater need for combination therapy and the increased prevalence of comorbidities with age. The potential role of urapidil (Ebrantil) in the treatment of elderly patients with hypertension has been previously reviewed [87].
conclusions
Hypertension is a leading cause of morbidity and mortality worldwide, despite the availability of effective treatment. Although alpha blockers have become less commonly used in the treatment of hypertension in recent years, they remain important, effective, and well-tolerated antihypertensive agents used as second and subsequent lines of therapy. Urapidil (Ebrantil), in addition to its alpha-blocking effect, has a central hypotensive effect, and therefore can be used to lower blood pressure in a variety of clinical situations. The role of urapidil (Ebrantil) in the treatment of hypertension should be reconsidered.
Printed in abbreviation. Original article published in Adv Ther (2010) 27(7): 1-18.