Let's figure out what really helps and whether you need to take antibiotics right away for Covid-19
It is believed that the main threat from coronavirus is lung damage. How does covid infection occur, and at what point does the process become complicated by bacterial pneumonia? How to distinguish one from the other, is there a way to protect yourself in advance and prevent COVID-19 from turning into pneumonia, Vladimir Beketov, candidate of medical sciences, pulmonologist at Sechenov University, told kp.ru.
The first thing that is important to understand, the expert says, is that the new coronavirus infection is a viral infection and is included in the group of acute respiratory viral infections. The only thing that stands apart from this group is influenza. This means that COVID-19, like all respiratory viral infections that affect the upper respiratory tract and lungs, is characterized by the following phenomenon. Immune defenses in the lungs weaken. Therefore, it becomes possible for a secondary bacterial super-infection to occur approximately on the 5th – 9th day of the course of any acute respiratory viral disease.
“Since Covid is a special disease, and it does not progress as quickly as the flu, for example, the addition of a bacterial infection, as a rule, occurs with COVID-19 towards the end of the second week,” says pulmonologist Vladimir Beketov.
HOW PNEUMONIA DEVELOPES
In conditions of reduced respiratory and motor activity, when mucus moves less through the bronchi, against the background of intoxication of the body and decreased immunity, bacteria from the nasopharynx descend into the lower parts of the respiratory tract and can begin to multiply there.
Thus, bacterial bronchitis can be caused first, then bronchopneumonia with transition to pneumonia. The development of bacterial pneumonia can also be facilitated by the patient being on a ventilator for a long time. Despite compliance with all the strictest disinfection measures, ventilators are risk factors for the occurrence of ventilator-associated pneumonia.
Clarithromycin-Akrikhin, 500 mg, film-coated tablets, 10 pcs.
Allergic reactions to the components of Clarithromycin-Akrikhin tablets: often - rash. uncommon - anaphylactoid reaction, hypersensitivity, bullous dermatitis, itching, urticaria, maculopapular rash. frequency unknown - anaphylactic reaction, angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome).
From the senses: often - dysgeusia, taste perversion. infrequently - vertigo, hearing loss, ringing in the ears. frequency unknown - deafness, ageusia, parosmia, anosmia.
From the nervous system: often - headache, insomnia. uncommon - loss of consciousness, dyskinesia, dizziness, drowsiness, tremor, anxiety, increased excitability. frequency unknown - convulsions, psychotic disorders, confusion, depersonalization, depression, disorientation, hallucinations, nightmares, paresthesia, mania.
From the skin: often - intense sweating. frequency unknown - acne, hemorrhages.
From the digestive system: often - diarrhea, vomiting, dyspepsia, nausea, abdominal pain. uncommon - esophagitis, gastroesophageal reflux disease, gastritis, proctalgia, stomatitis, glossitis, bloating, constipation, dry mouth, belching, flatulence, increased concentration of bilirubin in the blood, increased activity of ALT, AST, GGT, alkaline phosphatase, LDH, cholestasis, hepatitis , incl. cholestatic and hepatocellular. frequency unknown - acute pancreatitis, discoloration of the tongue and teeth, liver failure, cholestatic jaundice.
Infectious and parasitic diseases: infrequently - cellulitis, candidiasis, gastroenteritis, secondary infections (including vaginal). frequency unknown - pseudomembranous colitis, erysipelas.
From the hematopoietic system: infrequently - leukopenia, neutropenia, eosinophilia, thrombocythemia. frequency unknown - agranulocytosis, thrombocytopenia.
From the side of metabolism and nutrition: infrequently - anorexia, decreased appetite, increased urea concentration, change in the albumin-globulin ratio.
From the musculoskeletal system: uncommon - muscle spasm, musculoskeletal stiffness, myalgia. frequency unknown - rhabdomyolysis, myopathy.
From the respiratory system: infrequently - asthma, nosebleeds, pulmonary embolism.
From the urinary system: infrequently - increased creatinine concentration, change in urine color. frequency unknown - renal failure, interstitial nephritis.
From the blood coagulation system: infrequently - increase in MHO value, prolongation of prothrombin time.
From the cardiovascular system: often - vasodilation. uncommon - cardiac arrest, atrial fibrillation, prolongation of the QT interval on the ECG, extrasystole, atrial flutter. frequency unknown - ventricular tachycardia, incl. "pirouette" type.
From the body as a whole: malaise, hyperthermia, asthenia, chest pain, chills, fatigue.
DOES PNEUMONIA REALLY FOLLOW COVID-19?
— Recently, an analysis of statistical data shows that the medical community is mistakenly addicted to antibiotics in the treatment of a new coronavirus infection, suggesting that changes in the lungs are immediately associated not only with the virus, but also with a bacterial component. This is not true, says pulmonologist Vladimir Beketov.
According to the expert, to date, a number of reputable medical associations have issued memorandums and open letters calling on colleagues to reduce the use of antibiotics during the treatment of COVID-19, because antibiotics do not provide benefit, but in this case cause harm, including toxic damage to the liver and development of antibiotic-associated diarrhea.
— That is, we seem to be trying to treat pneumonia, which in the doctor’s mind is strongly associated with bacteria, but in fact, at the stage, while there is no secondary pneumonia associated with Covid, we are only dealing with coronavirus lung damage, which is recommended not to be called pneumonia, and call it pneumonitis (inflammation of the vascular walls of the alveoli, as well as the tissue separating the alveoli from the lungs, which is accompanied by scarring - editor's note), says pulmonologist Vladimir Beketov.
The very phenomenon of secondary bacterial pneumonia due to coronavirus is overestimated, the expert continues. Such processes develop mainly in patients with heart failure, and for them there are increased precautions, restrictions on movement, recommendations for self-isolation and treatment at home.
- Smokers are also at risk for developing bacterial pneumonia. However, if smokers with COPD receive proper inhalation treatment and are vaccinated against pneumococcus, then their risks of secondary bacterial pneumonia are also minimized, says Vladimir Beketov.
Safety considerations for the use of clarithromycin in children
The macrolide antibiotic clarithromycin is widely used in pediatric practice because it is highly effective against many infectious diseases and has a favorable safety profile.
General characteristics of the drug
Clarithromycin is a semisynthetic drug belonging to a 14-membered macrolide. Like other macrolides, clarithromycin has high activity against many gram-positive bacteria - Staphylococcus (methicillin-sensitive), Streptococcus (including pneumococci), Enterococcus, Listeria monocytogenes, Corynebacterium diphtheriae. Some gram-negative bacteria are sensitive to clarithromycin - Moraxella catarrhalis, Bordetella pertussis, Neisseria, Campylobacter jejuni, Helicobacter pylori (activity against the latter microorganism is higher than that of other macrolides). Clarithromycin is one of two macrolides (along with azithromycin) with clinically significant activity against Haemophilus influenzae. Like other macrolides, clarithromycin is highly active against atypical bacteria - Mycoplasma, Ureaplasma, Chlamydia, Legionella, Rickettsia. An important feature of clarithromycin is its high activity against atypical mycobacteria (Mycobacterium avium complex). The drug is also active against some anaerobic bacteria and toxoplasma [1–2]. A feature of clarithromycin is the formation of an active metabolite in the body - 14-hydroxyclarithromycin (14-HOCM), which also has antibacterial activity. With regard to sensitive pathogens, clarithromycin and its active metabolite exhibit an additive or synergistic effect. In this regard, the effect of the antibiotic in vivo may be higher than in vitro. In particular, the activity of clarithromycin itself against Haemophilus influenzae in vitro is low, but it is enhanced in vivo by the action of 14-HOCM [1–2].
Clarithromycin has a predominantly bacteriostatic effect, but in high doses the drug can have a bactericidal effect on a number of pathogens - S. pyogenes, S. pneumoniae, H. influenzae, M. catarrhalis, L. pneumophila and M. avium. In addition to the main antibacterial effect caused by disruption of protein synthesis on bacterial ribosomes, clarithromycin has pronounced additional antimicrobial properties:
- post-antibiotic effect against certain pathogens (S. pneumoniae, H. influenzae and M. catarrhalis) [1–2];
- suppression of virulence factors of Pseudomonas aeruginosa - clarithromycin is able to suppress motor activity and the ability to form biofilms in this pathogen [3].
Clarithromycin has a number of therapeutically beneficial non-antibacterial effects - immunomodulatory, anti-inflammatory, mucoregulatory, which are important for the treatment of respiratory diseases, not only bacterial, but also viral etiology, as well as diseases of non-infectious nature.
Experimental studies have established the mechanisms of non-antibacterial effects of clarithromycin:
- increased phagocytosis of apoptotic neutrophils by alveolar macrophages leads to the prevention of the release of neutrophil proteases and their effects on the respiratory tract [4];
- inhibition of the activation of nuclear transcription factor (NF-kappa-B) in mononuclear blood cells and pulmonary epithelial cells is accompanied by suppression of the production of pro-inflammatory cytokines - tumor necrosis factor-alpha (TNF-alpha), interleukins IL-6, IL-8, etc. [6 ];
- suppression of the expression of genes encoding inducible nitric oxide synthase (iNOS) leads to a decrease in the formation of NO in the epithelium of the respiratory tract and alveolar macrophages [5];
- a decrease in the level of IL-4 with an increase in the ratio of T helper cells type 1 and type 2 (Th1/Th2) [7];
- reducing the effect of lipopolysaccharide (bacterial endotoxin) on goblet cells of the respiratory tract epithelium leads to a decrease in mucus hypersecretion [8];
- inhibition of goblet cell hyperplasia in the airways induced by IL-13 also leads to a decrease in mucus hypersecretion [9].
The pharmacokinetics of clarithromycin have been well studied. The bioavailability of the drug when taken orally is 52–55%, while food does not reduce this figure. The maximum concentration of the drug in the blood after oral administration is observed on average after 2–3 hours. Clarithromycin is actively metabolized in the liver with the participation of cytochrome P450 with the formation of various metabolites, primarily 14-HOCM. The binding of the drug to plasma proteins ranges from 42% to 70%, which depends on the concentration in the blood. Clarithromycin and 14-HOCM create high concentrations in various organs, tissues and biological fluids, including nasal secretions, tonsils, middle ear fluid, lung tissue, and sputum. High concentrations of the drug and its active metabolite are observed in phagocytes [1–2]. Important data were obtained from a study of the intrapulmonary pharmacokinetics of clarithromycin in comparison with azithromycin, ciprofloxacin and cefuroxime in 68 volunteers. 6 hours after a single dose of a standard dose of drugs (500 mg for each), clarithromycin and 14-HOCM showed very high concentrations in alveolar cells (azithromycin was detected in them only after 12 hours). At the same time, high concentrations of clarithromycin and 14-HOCM remained in the blood serum (in total they exceeded the concentrations of all other antibiotics). In addition, clarithromycin was the only antibiotic found in the fluid lining the pulmonary epithelium [10]. The half-life of clarithromycin ranges from 3 to 8 hours, depending on the dose. From 20% to 40% of the drug is excreted in the urine unchanged, 10–15% in the form of metabolites. About 40% of the drug is excreted in the stool [1–2].
Recommendations for use in pediatrics
Clarithromycin is recommended for use in children with infections of various locations caused by sensitive bacteria:
- diseases of the upper respiratory tract and ENT organs - streptococcal tonsillopharyngitis, bacterial rhinosinusitis, acute otitis media [1–2, 11];
- diseases of the lower respiratory tract - acute bronchitis, exacerbation of chronic bronchitis, pneumonia (the drug is included in the standards of medical care for patients with acute bronchitis and pneumonia of the Ministry of Health and Social Development of the Russian Federation for adults and children in outpatient settings) [1–2, 12–14];
- diseases of the gastrointestinal tract associated with H. pylori (as part of eradication therapy) [1–2];
- diseases of the skin and soft tissues [1–2];
- diseases caused by M. avium (prevention and treatment) [1–2].
The literature also presents the results of clinical studies examining the use of clarithromycin for other respiratory diseases. Considering the ability of macrolides to suppress the virulence factors of P. aeruginosa and the presence of their anti-inflammatory and immunomodulatory effects, in recent years studies have been conducted on the effectiveness of long-term courses of macrolides in patients with cystic fibrosis. The scientific literature presents the results of a study on the use of macrolides in the treatment of bronchial asthma. The use of antibiotics of this class is due to both their activity against bacteria that play a role in the pathogenesis of bronchial asthma, and the presence of non-antibacterial effects in the drugs, which are therapeutically beneficial for bronchial asthma [1–2].
The original drug of clarithromycin, Klacid®, is registered in Russia for use in children in the form of film-coated tablets (250 and 500 mg) and powder for the preparation of an oral suspension (125 mg/5 ml and 250 mg/5 ml). The drug in oral form has no age restrictions, but tablets can be used in children from 3 years of age. In children under 12 years of age, it is preferable to use a suspension at a dose of 7.5 mg/kg every 12 hours (no more than 500 mg per day), over 12 years of age, 250–500 mg every 12 hours. The usual course of treatment is from 5 to 14 days.
Security Profile
The safety of drugs is of particular importance in pediatrics, since children may develop adverse reactions that are unusual for patients in adulthood. Macrolides are among the safest antibacterial drugs. They extremely rarely cause severe adverse reactions [1, 15].
The safety of clarithromycin, including in pediatric practice, has been well studied in numerous clinical studies. Children most often experience adverse reactions from the gastrointestinal tract (diarrhea, nausea and vomiting, abdominal pain) - their frequency is about 15%, as well as headaches - their frequency is about 1.6%. Also, when using clarithromycin, an increase in transaminase levels may be observed. Other reactions occurred in isolated cases. Adverse reactions when using the drug are usually mild and short-lived and rarely require discontinuation of the drug [1–2].
Scientific literature data indicate that macrolide antibiotics rarely cause allergic reactions [1, 16]. It has been established that in real clinical practice, allergies to macrolides are significantly less common than allergies to penicillins [17].
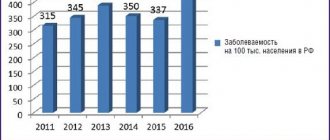
In a retrospective study of a large population (about 150 thousand people), the risk of skin reactions to various antibacterial drugs was assessed. Over a period of 1.5 years, more than 13 thousand people (including more than 2000 children) received almost 20 thousand courses of antibacterial therapy. Overall, skin reactions occurred in 135 patients, representing approximately 1%. However, the frequency of skin reactions to individual groups of drugs differed - it was least often observed when using macrolides, it was significantly less (3 or more times) than to penicillins, fluoroquinolones and co-trimoxazole (Fig.) [18].
A particular safety issue for macrolides is their hepatotoxicity, since the scientific literature has described cases of serious liver damage with their use [1]. A recent review of the scientific literature analyzed the safety data of various antibiotics on the liver. It has been established that hepatotoxic reactions when using fluoroquinolones, tetracyclines, macrolides and penicillin are observed significantly less frequently than when using amoxicillin/clavulanate, co-trimoxazole, sulfonamides, and drugs for the treatment of tuberculosis. In particular, the incidence of adverse liver effects when using erythromycin and clarithromycin is less than 4 cases per 100 thousand prescriptions, which is less than the average frequency of hepatotoxic reactions to antibacterial drugs in general. It has been noted that hepatotoxicity of antibiotics usually manifests itself with a long course of use, the use of high doses of the drug, in the elderly, in patients with underlying liver pathology, and with the simultaneous use of hepatotoxic drugs and alcohol [19].
When using clarithromycin, it must be taken into account that the drug has an inhibitory effect on cytochrome P450, which is involved in the metabolism of many drugs. When used simultaneously with such drugs, their concentration in the blood may increase and the risk of toxic effects may arise, as well as the effectiveness of clarithromycin may decrease [1–2]. It should be noted that the frequency and severity of drug interactions when using clarithromycin is lower than when using erythromycin [20].
Thus, more than 20 years of experience in the use of clarithromycin (Klacid®) in clinical practice and, in particular, in pediatrics indicates the high effectiveness and safety of the drug.
Literature
- Strachunsky L. S., Kozlov S. N. Macrolides in modern clinical practice. Smolensk: Rusich, 1998. 303 p.
- Rachina S. A., Strachunsky L. S., Kozlov R. S. Clarithromycin: is there potential for clinical use in the 21st century? // Wedge. microbiol. antimicrobial chemotherapy 2005, vol. 7, no. 4, 369–392.
- Wozniak DJ, Keyser R. Effects of subinhibitory concentrations of macrolide antibiotics on Pseudomonas aeruginosa // Chest. 2004, vol. 125, suppl. 2, p. 62–69.
- Yamaryo T., Oishi K., Yoshimine H. et al. Fourteen-member macrolides promote the phosphatidylserine receptor-dependent phagocytosis of apoptotic neutrophils by alveolar macrophages // Antimicrob. Agents Chemother. 2003, vol. 47, No. 1, r. 48–53.
- Tamaoki J. The effects of macrolides on inflammatory cells // Chest. 2004, vol. 125, suppl. 2, p. 41–50.
- Ichiyama T., Nishikawa M., Yoshitomi T. et al. Clarithromycin inhibits NF-kappa B activation in human peripheral blood mononuclear cells and pulmonary epithelial cells // Antimicrob. Agents Chemother. 2001, vol. 45, No. 1, r. 44–47.
- Williams AC, Galley HF, Watt AM, Webster NR Differential effects of three antibiotics on T helper cell cytokine expression // J. Antimicrob. Chemother. 2005, vol. 56, No. 3, r. 502–506.
- Tamaoki J., Takeyama K., Yamawaki I. et al. Lipopolysaccharide-induced goblet cell hypersecretion in the guinea pig trachea: inhibition by macrolides // Am. J. Physiol. 1997, vol. 272, p. 15–19.
- Tanabe T., Kanoh S., Tsushima K. et al. Clarithromycin inhibits interleukin-13-induced goblet cell hyperplasia in human airway cells // Am. J. Respira. Cell Mol. Biol. 2011, vol. 45, No. 5, 1075–1083.
- Conte JE Jr., Golden J., Duncan S. et al. Single-dose intrapulmonary pharmacokinetics of azithromycin, clarithromycin, ciprofloxacin, and cefuroxime in volunteer subjects // Antimicrob. Agents Chemother. 1996, vol. 40, No. 7, r. 1617–1622.
- Baranov A. A., Bogomilsky M. R., Volkov I. K. et al. The use of antibiotics in children in outpatient practice: practical recommendations // KMAH. 2007, vol. 9, no. 3, p. 200–210.
- Community-acquired pneumonia in children: prevalence, diagnosis, treatment, prevention. Scientific and practical program. M.: Original layout, 2011. 64 p.
- Order of the Ministry of Health and Social Development of the Russian Federation dated February 12, 2007 No. 108 “On approval of the standard of medical care for patients with acute bronchitis.”
- Order of the Ministry of Health and Social Development of the Russian Federation dated June 8, 2007 No. 411 “On approval of the standard of medical care for patients with pneumonia caused by Streptococcus pneumoniae; pneumonia caused by Haemophilus influenzae (Afanasyev-Pfeiffer bacillus); bacterial pneumonia, not elsewhere classified; pneumonia caused by other infectious agents, not classified elsewhere; pneumonia without specifying the pathogen; lung abscess with pneumonia (when providing specialized care).”
- Periti P., Mazzei T., Mini E., Novelli A. Adverse effects of macrolide antibacterials // Drug Saf. 1993, vol. 9, no. 5, p. 346–364.
- Araujo L., Demoly P. Macrolides allergy // Curr. Pharm. Des. 2008, vol. 14, no. 27, p. 2840–2862.
- Lutomski DM, Lafollette JA, Biaglow MA, Haglund LA Antibiotic allergies in the medical record: effect on drug selection and assessment of validity // Pharmacotherapy. 2008, vol. 28, no. 11, p. 1348–1353.
- Van der Linden PD, van der Lei J., Vlug AE, Stricker BH Skin reactions to antibacterial agents in general practice // J. Clin. Epidemiol. 1998, vol. 51, no. 8, p. 703–708.
- Andrade RJ, Tulkens PM Hepatic safety of antibiotics used in primary car // J. Antimicrob. Chemother. 2011, vol. 66, no. 7, p. 1431–1446.
- Principi N., Esposito S. Comparative tolerability of erythromycin and newer macrolide antibacterials in pediatric patients // Drug Saf. 1999, vol. 20, no. 1, p. 25–41.
N. A. Geppe, Doctor of Medical Sciences, Professor I. A. Dronov, Candidate of Medical Sciences
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health and Social Development of Russia, Moscow
Contact information for authors for correspondence