Indications
Exjiva medicine is used to prevent the deterioration of bone cells. Similar symptoms occur when:
- frequent fractures;
- exposure to radioactive radiation;
- surgical procedures in patients with serious tumor metastases spreading to the bones.
Pharmacology
Retarder of bone epithelium resorption. Immune cells that produce protective proteins. The drug Denosumab is a human component that has the protective functions of polysaccharides and has the ability to bind the activated centers of molecules with a certain set of antibodies. RANK proteins are found in the body in membrane connections and are capable of dissolution. RANKL is an intermediary at the moment of transformation of the sequence of chemical processes that carry out the resorption of bone epithelium in the presence of huge multinucleated cells. The high energy of the latter causes the breakdown of bones in the presence of tumor foci. Denosumab prevents bone degradation, which is caused by malignant ulcers.
How to use Exjiva
Dose. How to take Exjiva is determined by highly qualified and trained medical personnel. The amount of medication taken is one dose of subcutaneous injection of one hundred and twenty milligrams for 4 weeks. The product is injected into the area of the shoulder, thigh or abdomen. During the therapy period, it is advisable to consume calcium at a rate of at least five hundred milligrams and vitamin D-400 ME.
Before use, Exgiva solution must be checked for the presence of foreign bodies, color changes or turbidity. And for painless administration, it is advisable to heat the drug to ambient temperature. The medication should not be shaken. The needle used for injection must be 27 gauge.
Release form, composition and packaging
Solution for subcutaneous administration
transparent, colorless to light yellow, practically free of visible inclusions.
1 bottle contains:
active substance:
denosumab - 120 mg;
Excipients:
sorbitol (E420) 78.2 mg, glacial acetic acid 1.8 mg, sodium hydroxide to pH 5.2, water for up to 1.7 ml.
1.7 ml - Glass bottles with a volume of 3 ml (1) - cardboard packs with first opening control. 1.7 ml - Glass bottles with a volume of 3 ml (4) - cardboard packs with first opening control.
Contraindications
- severe untreated hypocalcemia;
- pregnancy;
- lactation period;
- age under 18 years (not recommended for use in pediatrics, since the effectiveness and safety of this drug have not been studied in this age group. In experimental animal studies, inhibition of RANK/RANKL led to inhibition of bone growth and impaired teething. Thus , the use of denosumab in children with open growth plates can lead to impaired bone growth and open growth plates and impaired tooth eruption);
- hypersensitivity to the components of the drug.
Xgeva®
Mechanism of action
Denosumab is a fully human monoclonal antibody (IgG2) that has high affinity and specificity for receptor activator of nuclear factor kappa B (RANKL) ligand and interferes with the activation of the single RANKL receptor activator of nuclear factor kB (RANK), located on the surface of osteoclasts and their precursors. The RANK ligand is a protein present in the body in membrane-bound and soluble forms. RANKL is a major mediator of a metabolic pathway required for the formation, function and survival of osteoclasts, the only cell type responsible for bone resorption. Increased osteoclast activity induced by RANKL is a major cause of bone destruction in bone metastases from solid tumors and multiple myeloma. Prevention of RANKL/RANK interaction inhibits osteoclast formation, activation, and survival. As a result, denosumab reduces bone resorption and bone destruction caused by malignant neoplasms.
Giant cell tumors of bone are characterized by RANK ligand expression by stromal cells and RANK-expressing osteoclast-like giant cells. In patients with giant cell tumor of bone, denosumab binds to the RANK ligand, significantly reducing the number or eliminating osteoclast-like giant cells. Consequently, osteolysis is reduced and the proliferative tumor stroma is replaced by non-proliferative, differentiated dense new bone tissue.
Pharmacodynamic effects
Exgiva 120 mg subcutaneously every 4 weeks resulted in rapid reductions in bone resorption markers (urinary N-telopeptide adjusted for creatinine (uNTX/Cr) and serum 1C-telopeptide) with an average reduction of 82% in uNTX/Cr in within a week. Reductions in bone turnover markers remained stable and ranged from 74% to 82% for uNTX/Cr from weeks 2 to 25 of repeated doses of 120 mg every 4 weeks. In 2075 patients with metastatic cancer (breast, prostate, other solid tumors, multiple myeloma) treated with XGIVA®, the average reduction in uNTX/Cr was approximately 80% of baseline values over 3 months of treatment.
Repeated subcutaneous administration of 120 mg every 4 weeks or every 12 weeks resulted in a mean decrease in uNTX/Cr from baseline values after 3 to 6 months of treatment in patients with metastatic cancer and bone metastases (including patients with multiple myeloma and bone metastases), previously receiving intravenous bisphosphonates and an initial uNTX/Cr value of less than 50 nmol/mmol at week 25 of treatment.
In a phase 2 study in patients with giant cell tumor of bone who received subcutaneous injections of 120 mg of Exjiva® with loading doses of 120 mg on days 8 and 15 after the starting dose in the first month of treatment and then at a dose of 120 mg once every 4 weeks ( Q4W), starting from the second month of treatment, by week 9 there was an average decrease in uNTx/Cr and sCTx by approximately 80%. Reductions in bone turnover markers were maintained, with mean decreases in uNTx/Cr values from 56% to 77% and sCTx values from 79% to 83% from weeks 5 to 25 of continued 120 mg dosing.
Immunogenicity
Clinical studies have not shown the formation of neutralizing antibodies. In less than 1% of patients treated with denosumab, binding but not neutralizing antibodies were detected by sensitive immunoassay. There were no changes in the pharmacokinetic profile, toxic profile or clinical response due to antibody formation.
Clinical effectiveness
Prevention of bone complications (OSCT) in patients with metastatic cancer and bone metastases
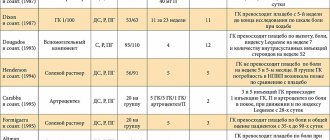
The effectiveness and safety of Exjiva® in the prevention of skeletal complications in patients with metastatic cancer and bone metastases was proven in 3 randomized, double-blind, active-controlled studies.
Exjiva® reduces or prevents the risk of developing OSCT or multiple OSCT (first and subsequent), compared with active control, in patients with malignant tumors that have metastasized to the bone.
Effect on pain
Pain analyzes included changes from baseline in the modified Brief Pain Inventory (BPI-SF), time to worsening pain, moderate to severe pain, improvement, and the proportion of patients meeting these criteria. The mean time to worsening (increased pain, greater than 4 scale points or greater than or equal to 2 points increase from baseline) was longer for XGIVA® compared to the active control. Time to improvement (i.e., greater than or equal to 2 points of pain improvement from baseline on the BPI-SF) was similar for denosumab and active control across individual studies and integrated analyses.
Overall survival and disease progression
Overall survival remained similar between the denosumab and active control groups for all three studies and in the pooled analysis of study data.
In each of the three studies, overall survival was balanced between the denosumab and active control groups in patients with malignancies that had metastasized to bone: breast cancer, prostate cancer, other solid tumors, or multiple myeloma.
Overall survival was higher in the Exjiva group in patients with non-small cell lung cancer and higher in the active control group in patients with multiple myeloma. Overall survival was similar between groups in patients with other solid tumors. In an integrated analysis of data from all three studies, overall survival was similar between the denosumab and active control groups.
Treatment of giant cell tumor of bone in adult patients or adolescents with a mature skeleton
The safety and effectiveness of Exjiva® were studied in two open-label, single-arm, phase 2 studies involving 305 patients with unresectable giant cell tumor of bone or in whom surgery was likely to be associated with a severe complication. Patients received 120 mg of Exjiva® subcutaneously every 4 weeks with loading doses of 120 mg on days 8 and 15.
Overall, 71.6% of patients responded to Exjiva®. Response rate was defined as at least 90% clearance of giant cells from baseline (or complete clearance of giant cells in cases where giant cells constituted <5% of tumor cells) , or the absence of progression of the target tumor lesion during radiographic studies in cases where pathohistological data were not available. The median time to response was 3.1 months. Median duration of response could not be assessed because several patients experienced disease progression with a median follow-up of 13.4 months. The efficacy results in skeletally mature adolescents were similar to those observed in adult patients.
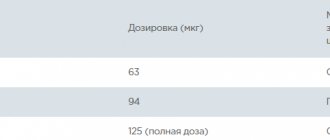
Dosage
Introduction
Injecting the drug requires prior training.
Dose
The recommended dose of the drug is one subcutaneous injection of 120 mg every 4 weeks in the thigh, shoulder or abdominal area.
During the course of treatment, it is recommended to additionally take calcium supplements in a dose of at least 500 mg and vitamin D-400 ME.
Elderly patients
Based on the available data on the effectiveness and safety of the drug in this age group, no adjustment of the drug dosage regimen is required.
Kidney failure
Based on the available data on the effectiveness and safety of the drug in this group of patients, no adjustment of the drug dosage regimen is required.
In patients with severe renal failure
(creatinine clearance <30 ml/min) or on dialysis there is a high risk of developing hypocalcemia. Such patients need to additionally take calcium supplements and vitamin D.
Liver failure
Efficacy and safety have not been studied.
Instructions for use
The solution should be assessed before administration for inclusions or color changes. The solution should not be used if it becomes cloudy or changes color. Do not shake.
It is recommended to administer the drug with a 27-gauge single-use needle.
To avoid discomfort at the injection site, the solution should be warmed to room temperature before injection.
Any unused quantities of the drug or unused materials must be destroyed in accordance with national requirements.
Exgiva, 120 mg (70 mg/ml), solution for subcutaneous administration, 1.7 ml, 1 pc.
Mechanism of action
Denosumab is a fully human monoclonal antibody (IgG2) that has high affinity and specificity for receptor activator of nuclear factor kappa B (RANKL) ligand and interferes with the activation of the only RANKL receptor, activator of nuclear factor kB (RANK), located on the surface of osteoclasts and their precursors. The RANK ligand is a protein present in the body in membrane-bound and soluble forms. RANKL is a major mediator of a metabolic pathway required for the formation, function and survival of osteoclasts, the only cell type responsible for bone resorption. Increased osteoclast activity induced by RANKL is a major cause of bone destruction in bone metastases from solid tumors and multiple myeloma. Prevention of RANKL/RANK interaction inhibits osteoclast formation, activation, and survival. As a result, denosumab reduces bone resorption, bone calcium loss, and bone destruction caused by cancer. Giant cell tumors of bone are characterized by RANK ligand expression by stromal cells and RANK-expressing osteoclast-like giant cells. In patients with giant cell tumor of bone, denosumab binds to the RANK ligand, significantly reducing the number or eliminating osteoclast-like giant cells. Consequently, osteolysis is reduced and the proliferative tumor stroma is replaced by non-proliferative, differentiated dense new bone tissue.
Pharmacodynamic effects
Exgiva 120 mg subcutaneously every 4 weeks resulted in rapid reductions in bone resorption markers (urinary N-telopeptide adjusted for creatinine (uNTX/Cr) and serum 1C-telopeptide) with an average reduction of 82% in uNTX/Cr in within a week. Reductions in bone turnover markers remained stable and ranged from 74% to 82% for uNTX/Cr from weeks 2 to 25 of repeated doses of 120 mg every 4 weeks. In 2075 patients with metastatic cancer (breast, prostate, other solid tumors, multiple myeloma) treated with XGIVA®, the average reduction in uNTX/Cr was approximately 80% of baseline values over 3 months of treatment.
Repeated subcutaneous administration of 120 mg XJIV® every 4 weeks or every 12 weeks resulted in a decrease in uNTX/Cr by approximately 80% of baseline values after 3 and 6 months of treatment in patients with metastatic cancer and bone metastases (including patients with multiple myeloma and bone metastases). bone) who had previously received intravenous bisphosphonates and an initial uNTX/Cr value of more than 50 nmol/mmol. 97% of patients in the ExGiva® group had at least 1 uNTX/Cr value less than 50 nmol/mmol before week 25 of the study.
In a phase 2 study in patients with giant cell tumor of bone who received subcutaneous injections of 120 mg of Exjiva® with loading doses of 120 mg on days 8 and 15 after the starting dose in the first month of treatment and then at a dose of 120 mg once every 4 weeks ( Q4W), starting from the second month of treatment, by week 9 there was an average decrease in uNTx/Cr and sCTx of approximately 80%. Reductions in bone turnover markers were maintained, with mean decreases in uNTx/Cr values from 56% to 77% and sCTx values from 79% to 83% from weeks 5 to 25 of continued 120 mg dosing.
Immunogenicity
Clinical studies have not shown the formation of neutralizing antibodies. In less than 1% of patients treated with denosumab, binding but not neutralizing antibodies were detected by sensitive immunoassay. There were no changes in the pharmacokinetic profile, toxic profile or clinical response due to antibody formation.
Clinical effectiveness
Prevention of bone complications (OSCT) in patients with metastatic cancer and bone metastases
The effectiveness and safety of Exjiva® in preventing skeletal complications in patients with metastatic cancer and bone metastases was proven in 3 randomized, double-blind, active-controlled studies. Exjiva® reduces or prevents the risk of developing OSCT or multiple OSCT (first and subsequent), compared with active control, in patients with malignant tumors that have metastasized to the bone.
Effect on pain
Pain analyzes included changes from baseline in the modified Brief Pain Inventory (BPI-SF), time to worsening pain, moderate to severe pain, improvement, and the proportion of patients meeting these criteria. The mean time to worsening (increased pain, greater than 4 scale points or greater than or equal to 2 points increase from baseline) was longer for XGIVA® compared to the active control. Time to improvement (i.e., greater than or equal to 2 points of pain improvement from baseline on the BPI-SF) was similar for denosumab and active control across individual studies and integrated analyses.
Overall survival and disease progression
Overall survival remained similar between the denosumab and active control groups for all three studies and in the pooled analysis of study data. In each of the three studies, overall survival was balanced between the denosumab and active control groups in patients with malignancies that had metastasized to bone: breast cancer, prostate cancer, other solid tumors, or multiple myeloma. Overall survival was higher in the Exjiva group in patients with non-small cell lung cancer and higher in the active control group in patients with multiple myeloma. Overall survival was similar between groups in patients with other solid tumors. In an integrated analysis of data from all three studies, overall survival was similar between the denosumab and active control groups.
Treatment of giant cell tumor of bone in adult patients or adolescents with a mature skeleton
The safety and effectiveness of Exjiva® were studied in two open-label, single-arm, phase 2 studies involving 305 patients with unresectable giant cell tumor of bone or in whom surgery was likely to be associated with a severe complication. Patients received 120 mg of Exjiva® subcutaneously every 4 weeks with loading doses of 120 mg on days 8 and 15. Overall, 71.6% of patients responded to Exjiva®. Response rate was defined as at least 90% elimination of giant cells from baseline (or complete elimination of giant cells in cases where giant cells constituted <5% of tumor cells), or absence of radiographic progression of the target tumor lesion in cases where pathological findings were unavailable. The median time to response was 3.1 months. Median duration of response could not be assessed because several patients experienced disease progression with a median follow-up of 13.4 months. The efficacy results in skeletally mature adolescents were similar to those observed in adult patients.
Treatment of hypercalcemia in malignant tumors
The safety and efficacy of Exjiva® were studied in an open-label, single-comparative, phase 2 study of 33 adult patients with hypercalcemia from malignant tumors (with or without bone metastases) refractory to treatment with intravenous bisphosphonates. Patients were administered 120 mg of Exjiva® subcutaneously every 4 weeks with additional doses of 120 mg on days 8 and 15 of the first month of treatment.
Refractory hypercalcemia in malignancy was defined as an albumin-corrected calcium concentration >12.5 mg/dL (3.1 mmol/L) despite treatment with intravenous bisphosphonates in the last 7 to 30 days. The primary endpoint was the number of patients achieving a response, defined as an albumin-corrected serum calcium concentration (CSC) ≤ 11.5 mg/dL (2.9 mmol/L), within 10 days of XGIV® administration. Exjiva® caused a rapid and sustained decrease in albumin-corrected serum calcium concentrations in most patients, including patients with or without bone metastases.
Side effects
Infections and infestations:
inflammation of the subcutaneous tissue.
From the immune system:
hypersensitivity reactions.
From the side of metabolism and electrolyte metabolism:
hypocalcemia, hypophosphatemia.
For the skin and subcutaneous tissues:
hyperhidrosis.
From the digestive system:
diarrhea, tooth loss.
From the respiratory system:
dyspnea.
From the musculoskeletal system and connective tissue:
osteonecrosis of the jaw.
Hypocalcemia
In clinical trials in patients with tumors metastasizing to bone, hypocalcemia was more common in the Exjiva group (9.6%) than in the active comparator group (5.0%). Grade 3 decreases in serum calcium concentrations were observed in 2.5% of patients in the Exjiva group and in 1.2% of patients in the active comparator group. A grade 4 decrease in serum calcium concentrations was observed in 0.6% of patients and 0.2% of patients in the active control group.
Osteonecrosis of the jaw
In patients with metastatic cancer, osteonecrosis of the jaw was reported in 1.8% in the denosumab group and 1.3% in the active control group. Clinical symptoms did not differ between subgroups. Among patients with confirmed osteonecrosis of the jaw, the majority (81% in both subgroups) had a history of tooth extraction, poor oral hygiene and/or dental debridement. Most patients received chemotherapy.
Exgiva solution for injection 70 mg/ml syringe 1.7 ml 1 pc
Exgiva 120 mg subcutaneously every 4 weeks resulted in rapid reductions in bone resorption markers (urinary N-telopeptide adjusted for creatinine (uNTX/Cr) and serum 1C-telopeptide) with an average reduction of 82% in uNTX/Cr in within a week. Reductions in bone turnover markers remained stable and ranged from 74% to 82% for uNTX/Cr from weeks 2 to 25 of repeated doses of 120 mg every 4 weeks. In 2075 patients with metastatic cancer (breast, prostate, other solid tumors, multiple myeloma) treated with XGIVA®, the average reduction in uNTX/Cr was approximately 80% of baseline values over 3 months of treatment. Repeated subcutaneous administration of 120 mg every 4 weeks or every 12 weeks resulted in a mean decrease in uNTX/Cr from baseline values after 3 to 6 months of treatment in patients with metastatic cancer and bone metastases (including patients with multiple myeloma and bone metastases), previously receiving intravenous bisphosphonates and an initial uNTX/Cr value of less than 50 nmol/mmol at week 25 of treatment. In a phase 2 study in patients with giant cell tumor of bone who received subcutaneous injections of 120 mg of Exjiva® with loading doses of 120 mg on days 8 and 15 after the starting dose in the first month of treatment and then at a dose of 120 mg once every 4 weeks ( Q4W), starting from the second month of treatment, by week 9 there was an average decrease in uNTx/Cr and sCTx by approximately 80%. Reductions in bone turnover markers were maintained, with mean decreases in uNTx/Cr values from 56% to 77% and sCTx values from 79% to 83% from weeks 5 to 25 of continued 120 mg dosing. Immunogenicity Clinical studies have not demonstrated the formation of neutralizing antibodies. In less than 1% of patients treated with denosumab, binding but not neutralizing antibodies were detected by sensitive immunoassay. There were no changes in the pharmacokinetic profile, toxic profile or clinical response due to antibody formation. Clinical effectiveness Prevention of bone complications (OSCT) in patients with metastatic cancer and bone metastases. The effectiveness and safety of Exjiva® in preventing skeletal complications in patients with metastatic cancer and bone metastases was proven in 3 randomized, double-blind, active-controlled studies. Exjiva® reduces or prevents the risk of developing OSCT or multiple OSCT (first and subsequent), compared with active control, in patients with malignant tumors that have metastasized to the bone. Effect on Pain Pain analyzes included changes from baseline in the modified Brief Pain Inventory (BPI-SF), time to worsening pain, moderate to severe pain, improvement, and the proportion of patients meeting these criteria. The mean time to worsening (increased pain, greater than 4 scale points or greater than or equal to 2 points increase from baseline) was longer for XGIVA® compared to the active control. Time to improvement (i.e., greater than or equal to 2 points of pain improvement from baseline on the BPI-SF) was similar for denosumab and active control across individual studies and integrated analyses. Overall survival and disease progression Overall survival remained similar between the denosumab and active control groups for all three studies and in the pooled analysis of study data. In each of the three studies, overall survival was balanced between the denosumab and active control groups in patients with malignancies that had metastasized to bone: breast cancer, prostate cancer, other solid tumors, or multiple myeloma. Overall survival was higher in the Exjiva group in patients with non-small cell lung cancer and higher in the active control group in patients with multiple myeloma. Overall survival was similar between groups in patients with other solid tumors. In an integrated analysis of data from all three studies, overall survival was similar between the denosumab and active control groups. Treatment of giant cell tumor of bone in adult patients or adolescents with a mature skeleton. The safety and effectiveness of Exjiva® were studied in two open-label, single-arm, phase 2 studies involving 305 patients with unresectable giant cell tumor of bone or in whom surgery was likely to be associated with a severe complication. Patients received 120 mg of Exjiva® subcutaneously every 4 weeks with loading doses of 120 mg on days 8 and 15. Overall, 71.6% of patients responded to Exjiva®. Response rate was defined as at least 90% clearance of giant cells from baseline (or complete clearance of giant cells in cases where giant cells were treated in Treatment of hypercalcemia in malignancy. The safety and efficacy of Exjiva® were studied in an open-label, single-arm, phase 2 study in 33 Adult patients with hypercalcemia from malignant tumors (with or without bone metastases) refractory to treatment with intravenous bisphosphonates.Patients were administered 120 mg of Exjiva® subcutaneously every 4 weeks with additional doses of 120 mg on days 8 and 15 of the first month of treatment. malignancies was defined as an albumin-corrected calcium concentration >12.5 mg/dL (3.1 mmol/L) despite treatment with intravenous bisphosphonates in the last 7 to 30 days.The primary endpoint was the number of patients achieving a response, as defined by as an albumin-corrected serum calcium concentration (CSC) ≤ 11.5 mg/dL (2.9 mmol/L), within 10 days after administration of XGIV®. Exjiva® caused a rapid and sustained decrease in albumin-corrected serum calcium concentrations in most patients, including patients with or without bone metastases.
Drug interactions
No drug interaction studies have been conducted.
In clinical studies, the drug was administered simultaneously with standard antineoplastic therapy, incl. patients previously treated with bisphosphonates.
Concomitant use with chemotherapy or hormone therapy did not change the pharmacokinetics/pharmacodynamics of denosumab, nor did previous IV administration of bisphosphonates.
Pharmaceutical incompatibility
The drug should not be mixed with other drugs.
special instructions
Hypocalcemia
Hypocalcemia must first be corrected by taking calcium and vitamin D supplements in adequate doses before starting denosumab therapy. It is recommended to take calcium and vitamin D supplements during use of the drug, in the absence of hypercalcemia.
Patients with severe renal impairment (creatinine clearance less than 30 ml/min) or on dialysis are at greater risk of developing hypocalcemia. Monitoring calcium concentrations in this subgroup of patients is necessary. If hypocalcemia occurs during treatment, additional short-term calcium supplementation is recommended as needed.
Infections of the skin and appendages
Patients receiving denosumab were more likely to experience infections of the skin and its appendages (mainly inflammation of the subcutaneous tissue), in some cases requiring hospitalization. Such reactions were reported more frequently in the denosumab group (0.9%) than in the comparison group (0.7%). Patients should be instructed to immediately seek medical attention if symptoms and signs of subcutaneous tissue inflammation develop.
Osteonecrosis of the jaw
It is recommended that an examination of the oral cavity and a preventive examination by a dentist before starting therapy in patients at risk of developing osteonecrosis of the jaw. Adequate oral hygiene should be maintained throughout the entire period of treatment with Exgiva. During treatment, invasive dental procedures should be avoided if possible. If such procedures are necessary, the decision should be made together with the attending physician. Patients who develop osteonecrosis of the jaw while using Exjiva should receive adequate dental treatment. An individual assessment of the benefit/risk ratio is required before prescribing Exgiva to patients with irreparable risk factors for the development of osteonecrosis of the jaw and for patients in whom osteonecrosis of the jaw developed while taking the drug.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted on the ability to drive vehicles and operate machinery.
Special Cautions
Exjiva should be taken with extreme caution if:
- hypocalcemia;
- renal failure;
- skin infections;
- osteonecrosis of the jaw.
For complications associated with a low amount of calcium in the blood (hypocalcemia), Exjiva is recommended to be used after a preliminary course of taking medicinal calcium and vitamin D.
Ability to manage transport and perform responsible functions. The effects of the drug on the ability to drive cars and other equipment have not been studied.
Use in old age. There is no need to change the dosage of the medication for older people.
Pregnancy and lactation
There are no data on the use of the drug during pregnancy. The drug is not recommended for use in pregnant women.
In toxicological studies in animals, at exposures 9.1 times higher than those recommended for clinical use in humans (120 mg every 4 weeks), denosumab had no effect on fertility or fetal development.
Animal experiments have shown that the absence of RANKL can lead to impaired development of lymph nodes in the fetus, and in the postnatal period can cause impaired teething and bone growth; It is also possible to influence the maturation of the mammary gland, which can lead to weakened lactation. It is unknown whether denosumab is excreted in breast milk. Because denosumab is known to potentially cause adverse reactions in infants, it is necessary to either stop breastfeeding or discontinue the drug.
Xgeva
Denosumab is a fully human monoclonal antibody (IgG2) that has high affinity and specificity for receptor activator of nuclear factor kappa B (RANKL) ligand and interferes with the activation of the only RANKL receptor, activator of nuclear factor kB (RANK), located on the surface of osteoclasts and their precursors. The RANK ligand is a protein present in the body in membrane-bound and soluble forms. RANKL is a major mediator of a metabolic pathway required for the formation, function and survival of osteoclasts, the only cell type responsible for bone resorption. Increased osteoclast activity induced by RANKL is a major cause of bone destruction in bone metastases from solid tumors and multiple myeloma. Prevention of RANKL/RANK interaction inhibits osteoclast formation, activation, and survival. As a result, denosumab reduces bone resorption and bone destruction caused by malignant neoplasms.
Pharmacodynamic effects
Denosumab 120 mg SC every 4 weeks resulted in rapid reductions in bone resorption markers (urinary N-telopeptide adjusted for creatinine (uNTX/Cr) and serum 1C-telopeptide) with an average reduction of 82% in uNTX/Cr in a week. Reductions in bone turnover markers remained stable and ranged from 74% to 82% for uNTX/Cr from weeks 2 to 25 of repeated doses of 120 mg every 4 weeks. In 2075 patients with metastatic cancer (breast, prostate, other solid tumors, multiple myeloma) treated with XGIVA, the average reduction in uNTX/Cr was approximately 80% of baseline values over 3 months of treatment. Repeated SC administration of 120 mg every 4 weeks or every 12 weeks resulted in a mean decrease in uNTX/Cr from baseline values after 3-6 months of treatment in patients with metastatic cancer and bone metastases (including patients with multiple myeloma and bone metastases ), previously treated with IV bisphosphonates and an initial uNTX/Cr value of less than 50 nmol/mmol at week 25 of treatment.
Immunogenicity
Clinical studies have not shown the formation of neutralizing antibodies. In less than 1% of patients treated with denosumab, binding but not neutralizing antibodies were detected by sensitive immunoassay. There were no changes in the pharmacokinetic profile, toxic profile or clinical response due to antibody formation.
Clinical effectiveness
Prevention of bone complications (OSCT) in patients with metastatic cancer and bone metastases.
The efficacy and safety of Exgiva in preventing skeletal complications in patients with metastatic cancer and bone metastases was demonstrated in 3 randomized, double-blind, active-controlled studies. Exjiva reduces or prevents the risk of developing OSCT or multiple OSCT (first and subsequent), compared with active control, in patients with malignant tumors that have metastasized to the bone.
Effect on pain
Pain analyzes included changes from baseline in the modified Brief Pain Inventory (BPI-SF), time to worsening pain, moderate to severe pain, improvement, and the proportion of patients meeting these criteria. The mean time to worsening (worsening of pain, greater than 4 scale points or greater than or equal to 2 point increase from baseline) was longer for XGIVA compared to the active control. Time to improvement (i.e., greater than or equal to 2 points of pain improvement from baseline on the BPI-SF) was similar for denosumab and active control across individual studies and integrated analyses.
Overall survival and disease progression
Overall survival remained similar between the denosumab and active control groups for all three studies and in the pooled analysis of study data. In each of the three studies, overall survival was balanced between the denosumab and active control groups in patients with malignancies that had metastasized to bone: breast cancer, prostate cancer, other solid tumors, or multiple myeloma.
Overall survival was higher in the Exgiva group in patients with non-small cell lung cancer and higher in the active control group in patients with multiple myeloma. Overall survival was similar between groups in patients with other solid tumors. In an integrated analysis of data from all three studies, overall survival was similar between the denosumab and active control groups.