Introduction
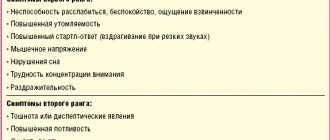
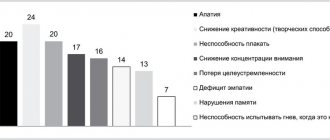
Autonomic dysfunction is a common syndrome characterized by a wide range of multisystem autonomic disorders, often combined with anxiety. In these cases, patient complaints of decreased memory, attention, and thought processes, which impede professional and social activities, are obligatory. In this regard, when choosing a drug for the treatment of anxiety-associated autonomic dysfunction, it is necessary to take into account, in particular, its effect on cognitive functions.
Many of the psychotropic drugs used to treat anxiety relieve vegetative symptoms well, but can aggravate cognitive impairment, which reduces the patient’s satisfaction with the treatment effect, increasing his maladjustment. In this regard, it is important to use drugs that do not have anticholinergic and muscle relaxant effects. These requirements are met by the drug mebicar, a synthetic compound (a derivative of bicyclic biureas) with tranquilizing ability [1]. Mebicar reduces feelings of anxiety, restlessness, reduces irritability, and has a mild sedative effect. The targets for the action of mebikar are the structures included in the limbic-reticular complex and the emotional zones of the hypothalamus. The wide range of pharmacological effects of mebicar is explained by its integrative effect on the serotonin, adrenergic, cholinergic and GABAergic systems. Along with the main stress-protective and anxiolytic effect, the drug has a pronounced nootropic effect: improves memory, mental functions, increases logic, coherence and speed of thinking, improves attention and mental performance, helps normalize mental functions in general under conditions of stress and overload. Mebicar does not have a muscle relaxant effect and does not impair coordination, which significantly distinguishes it from benzodiazepine tranquilizers [1-5]. Mebicar improves the quality of sleep, facilitating the process of falling asleep, normalizes sleep structure and reduces the frequency of anxious dreams, without having a direct hypnotic effect and without causing daytime drowsiness, which allowed the drug to be classified as a “daytime” tranquilizer. In combination with other psychotropic and hypnotic drugs, Mebicar enhances the hypnotic effect. Additional effects of mebicar are its modulating effect on lipid metabolism, due to the ability to change the ratio of high and low density lipoproteins, which helps reduce the concentration of cholesterol in the blood [6], as well as the ability to improve myocardial trophism by increasing coronary blood flow, reducing blood viscosity and intravascular aggregation erythrocytes [7, 8]. Mebicar does not cause euphoria or addiction. All this justifies the possibility of its use in various fields of medicine, including neurology.
The purpose of the study was to study the effectiveness of Mebikar in patients with autonomic dysfunction combined with anxiety disorder.
Hypothesis: Mebicar, while effectively eliminating symptoms of mild to moderate anxiety and autonomic disorders in patients with autonomic dysfunction, should not have a negative effect on cognitive function.
MEBIKAR (tablets)
I have no strength.
Anyone who doesn't know what it is will never understand. Everywhere you look, everything is bad, the condition is deteriorating rapidly, and here - like a demo version of a good life - a few days of enlightenment (like, look how well you can live). At one time I took antidepressants for a long time. Most of all, I am “driven” by children - usually after something bad - illness, trouble. When something happens, I am as collected as possible, but after that I am completely distraught. I will never take antidepressants again - they don’t make me feel like a zombie. But something needs to be saved. First there was Adaptol, but it was expensive, so I decided to try the same active ingredient in a different form. I found Mebicar. Also expensive, not cheaper than adaptol. Removes neuroses, improves sleep. But the effect is only while taking it; as soon as you stop, the condition worsens again. I am adding to the review on September 14, 2018, because something has changed in my attitude towards the drug. In general, judge for yourself. In July, we had a misfortune - a child was admitted to the hospital in an urgent condition. I won’t say what happened and what the diagnosis is, but the condition is serious and threatens long-term treatment without prognosis...
I have one peculiarity: when something happens, I “hold on” for several days, and then I begin to slowly and surely “fall apart” - it hits me. This time something similar happened - it started to get worse and I realized that I couldn’t cope on my own - I started taking Mebicar, fortunately at that moment I had a package of the drug, the dosage was 500. But in vain. It was probably necessary to divide the drug in two. And instead of helping, the drug began to have a negative effect (although it would be wrong to say here - after all, it is possible that the drug did not work at all, and I felt bad under the influence of circumstances). The despair was so strong, and the horror of what happened intensified every day (but they say that time heals...) I can say that I have probably never felt so bad. In 1 month I lost 5 kg, constant incessant trembling, I was like a walking exposed nerve - I reacted sharply to sounds (I even jumped at a rustle, and if someone unexpectedly approached, I screamed), I absolutely could not sleep - I woke up in the middle of the night and didn't sleep anymore. At first she could at least cry in order to “throw out” the negativity, but after some time she could no longer cry. After 10 days, the child was discharged from the hospital - I needed to prepare, support him, and show unquenchable optimism. What good could I “show” in such a state? All thoughts went so negative at that time that every word spoken reminded of the situation, nothing could distract, the critical attitude towards the situation was completely lost - EVERYTHING was bad, absolutely everything! A new symptom was added - I constantly began to monitor my son’s condition, expecting it to worsen. but he is a teenager! He needs to be let go of himself so that he grows up normal and does not consider himself defective. When he went for a walk, the soil ran away from under his feet, returning only when he arrived.
In general, I think the picture is clear. Everything was aggravated by the fact that I don’t work. If I could go away, it would be easier for me, but constantly being at home and “spying” on the child deepened my despair. I simply could not leave the house - I was afraid to leave the child and could not find a sufficiently serious reason for excommunication.
And all this happened while taking the same dose - Mebicar 500. And the most popular advice to “pull yourself together” was especially annoying - how can you pull yourself together when the will is paralyzed? Attempts to gather “in a small group” did not bring results, once again reminding us of the hopelessness of the situation.
It helped a little that my husband took the children for 3 days and went to visit his mother in another region, and at that time I stopped taking Mebicar. I just gave up and that's it. At the same time, the need for constant monitoring of the child disappeared - and I began to come to life, so it’s hard to say what helped. A few days earlier, my mother went to see a neurologist (for her diagnosis) and told her about my condition. The neurologist said that perhaps the dosage of Mebicar was too high or that it was simply not suitable for me and prescribed another drug for a month. I decided that if it got worse, I would start taking it, but I didn’t have to. I can’t say that I immediately returned to normal, but there was no deterioration in my condition.
I'm not taking anything now. Life goes on as usual, I worry about the child, but it’s not as acute and I don’t have that feeling of hopelessness, although I don’t have excessive optimism about my son’s illness.
This is the story. Therefore, I don’t know what to say about this drug now. Perhaps this is just a lifeline for those who are still not so bad, or maybe the dosage that turned out to be unnecessary aggravated the situation?
Material and methods
The study included 54 patients: 39 women (mean age 25±6.7 years) and 15 men (mean age 27±8.4 years).
Inclusion criteria
were as follows: age from 18 to 55 years, patients of both sexes with a diagnosis of autonomic dysfunction syndrome (ADS) and different types of anxiety disorder (generalized anxiety disorder, panic disorder, adjustment disorder) with manifestations of mild or moderate anxiety.
Exclusion criteria
were: age younger than 18 or older than 55 years; diagnoses of obsessive-compulsive, phobic disorder; severe anxiety (46 points or more on the Spielberger-Hanin scale); the presence of depression, dementia, as well as severe somatic diseases.
In all cases, patients were examined, including collection of complaints, medical history, somatic and neurological examinations.
The type of anxiety disorder was determined according to ICD-10 criteria. The severity of anxiety was assessed using the Spielberger-Hanin scale [9]. ICD-10 clinical criteria and the Hospital Anxiety and Depression Scale (HADS) were used to exclude depression.
In order to assess the initial autonomic tone (the state of autonomic indicators during the period of relaxed wakefulness), a questionnaire was used to identify signs of autonomic changes, filled out by the subject, and a chart to identify signs of autonomic disorders, filled out by the researcher (see Appendix).
Autonomic symptoms are systematized into groups: cardiovascular, respiratory, gastrointestinal, muscular-tonic and motor. The presence of sleep disorders, asthenic symptom complex, and neuroendocrine disorders were taken into account.
The state of cognitive functions was assessed using the following tests: 16-word learning test FCSRT-IR [10], MoCA test [11], McNair memory self-assessment questionnaire [12]. The diagnosis of mild cognitive impairment (MCI) was made according to the NIA-AA criteria [13]. To exclude dementia, ICD-10 criteria and the Lowton-Brody Questionnaire for Assessing Daily Activities (1969) were used, which we present in full, since it is not known to all doctors (see Appendix).
Mebicar was prescribed at a dose of 300 mg 2 times a day for 3 months.
Adverse effects were assessed using the Udvalg for Kliniske Undersogelser Scale (UKU) (see Appendix).
The results were processed by the statistical method of paired comparison of patient groups using Microsoft Excel 7.0 and Statistica application programs. In case of normal distribution, comparative analysis between groups was carried out using Student's t test. Differences were considered significant at p
<0.05. The mean and standard deviation, as well as the error of the mean, were calculated. In the absence of normal distribution, medians, 1st and 3rd quartiles were calculated. Comparisons between groups were made using the Mann-Whitney test.
A drug used to treat bronchial asthma is effective against new coronavirus infection
The US Centers for Disease Control and Prevention (CDC) indicate that patients with asthma have an increased risk of severe coronavirus infection [1]. However, glucocorticosteroid therapy is associated with fewer complications of COVID-19 not only for asthmatics, but also for all other patients.
A multicenter study was performed in the United States that compared data from 562 patients with COVID-19 diagnosed with bronchial asthma and 2686 patients without asthma matched by age, gender, and date of diagnosis of COVID-19. The results showed that both study groups required hospitalization at similar rates (21% of patients with asthma and 18% without asthma), and the need for mechanical ventilation was 3% and 4%, respectively. 7 (1%) patients with asthma and 69 (3%) without asthma died. None of the 44 hospitalized patients with severe asthma experienced death due to COVID-19 [2].
Another recent analysis of 15 studies from different countries found no increased risk of severe disease and mortality among patients with asthma and coronavirus infection [3]. The researchers suggested that inhaled glucocorticosteroids used to treat bronchial asthma may have a protective effect in this case.
This hypothesis formed the basis of the STOIC study, which was carried out at the University of Oxford [4]. The study randomized 146 outpatients with confirmed COVID-19, and 139 patients underwent statistical evaluation of the results. 70 patients took 800 mcg of the inhaled glucocorticosteroid budesonide (Pulmicort® Turbuhaler®, AstraZeneca) twice daily. The control group (69 patients) received standard treatment. Therapy began in the first 7 days from the onset of the disease and continued as necessary up to 28 days.
The study showed that early use of budesonide reduced the need for emergency care and hospitalization in patients with COVID-19 by 90%. The use of budesonide was also associated with a reduction in time to recovery. The average time to recovery was 8 days in the budesonide group and 11 days in the standard therapy group. Symptoms on days 14 and 28 of therapy persisted in fewer patients receiving budesonide. The duration of hypoxia during the first 14 days of observation (number of days with blood oxygen saturation ≤94%) was 19% and 22% in the budesonide and standard treatment groups, respectively.
The study authors found these results very promising and intend to test them in larger studies.
“Mass vaccination programs have started around the world, but we don’t know how long it will take to implement them. “I am very encouraged that a relatively safe, affordable and well-studied drug can reduce the risk of complications and help billions of people who do not have access to hospital care,” said the study’s lead author, Professor Mona Bafadhel [5].
- https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html
- L. B. Robinson, L. Wang, X. Fu et al. COVID-19 severity in asthma patients: A multi-center matched cohort study. doi.org/10.1101/2020.10.02.20205724. Preprint. medRxiv.
- https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.202006-613RL
- S. Ramakrishnan, D. V. Nicolau, B. Langford et al. Inhaled budesonide in the treatment of early COVID-19 illness: a randomized controlled trial. doi.org/10.1101/2021.02.04.21251134. Preprint. medRxiv.
- https://www.ox.ac.uk/news/2021-02-09-common-asthma-treatment-reduces-need-hospitalisation-covid-19-patients-study