Protaphane® HM (Protaphane® NM)
Instructions for use for patients
You cannot use Protafan® NM:
- In insulin pumps.
— If you are allergic (hypersensitivity) to human insulin or any of the components included in the drug Protafan® NM.
- If you experience hypoglycemia (low blood sugar).
— If the protective cap is missing or not firmly attached. Each bottle has a protective plastic cap. If the protective cap on a new bottle is damaged, return the bottle to the pharmacy.
— If the storage conditions of the drug were violated or it was frozen.
— If the insulin does not turn uniformly white and cloudy after stirring.
Before using Protafan® NM:
— Check the label to make sure you are using the right type of insulin.
— Remove the protective cap.
How to use Protafan® NM
The drug Protafan® NM is intended for subcutaneous administration. Never give insulin intravenously or intramuscularly
.
Always rotate injection sites within the anatomical area to reduce the risk of lumps and ulcerations at the injection site. The best places for injections are: the buttocks, front of the thigh or shoulder.
How to administer Protafan® NM if only Protafan® NM is administered or if it is necessary to mix Protafan® NM with short-acting insulin:
- Make sure you use an insulin syringe that has a scale that allows you to measure the dose in action units.
— Fill the syringe with air in an amount corresponding to the required dose of insulin.
— Follow the instructions your doctor or nurse gives you.
— Immediately before taking the dose, roll the bottle between your palms until the insulin becomes uniformly white and cloudy. Resuspension is facilitated if the preparation is at room temperature.
— Inject insulin under the skin. Use the injection technique recommended by your doctor or nurse.
— Hold the needle under the skin for at least 6 seconds to ensure that the entire dose of insulin is injected.
Protafan® NM suspension for subcutaneous administration in FlexPen® syringe pens
Instructions for use for patients
Read these instructions carefully before using Protafan® NM in the FlexPen® syringe pen.
The FlexPen® is a pre-filled insulin pen with a pump. You can select a dose from 1 to 60 units in 1 unit increments. The FlexPen® syringe pen is designed for use with NovoFine or NovoTwist® disposable needles up to 8 mm in length. As a precaution, always carry a spare insulin injection system with you in case your FlexPen® syringe pen with Protafan® NM is lost or damaged.
FlexPen® syringe pen with Protafan® NM
See fig. 1 and fig. 2.
Storage and care
The FlexPen® syringe pen is designed for effective and safe use and requires careful handling. In the event of a fall or strong mechanical impact, the syringe pen may be damaged and insulin may leak.
The outside of the FlexPen® syringe pen can be cleaned with a cotton swab. Do not wash, immerse or lubricate the pen as it may this may damage the mechanism. FlexPen® syringe pens must not be refilled.
Preparing the FlexPen® syringe pen with Protafan® HM for use
Check the label to make sure that the FlexPen® pen with Protafan® NM contains the required type of insulin.
Mix the insulin before the first injection using the new FlexPen® pen.
A
To facilitate mixing, allow the preparation to warm to room temperature. Remove the cap from the pen (see Figure A).
IN
Raise and lower the pen up and down 20 times as shown (see Figure B) so that the glass ball moves from one end of the cartridge to the other. Repeat these steps until the contents of the cartridge become uniformly white and cloudy.
Before each subsequent injection
Stir the contents by lifting the pen up and down at least 10 times until the contents of the cartridge are uniformly white and cloudy.
After mixing, inject immediately.
- Always ensure there are at least 12 units of insulin left in the cartridge to ensure even mixing. If there are less than 12 units left, use a new FlexPen® syringe pen with Protafan® HM.
Attaching a needle
WITH
Remove the protective sticker from the disposable needle.
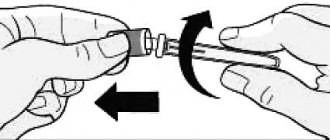
Carefully and tightly screw the needle onto the FlexPen® syringe pen (see Fig. C).
D
Remove the outer needle cap but do not throw it away (see Figure D).
E
Remove and discard the inner needle cap (see Figure E).
- Always use a new needle for each injection to prevent infection.
- Be careful not to bend or damage the needle before use.
— To avoid accidental needle sticks, never put the inner cap back on the needle.
Checking insulin delivery
When using a pen syringe, a small amount of air may accumulate in the cartridge before each injection. To prevent the entry of air bubbles and ensure that the correct dose of the drug is administered.
F
Dial up 2 units of the drug by turning the dose selector (see Fig. F).
G
Holding the FlexPen® pen with the needle pointing up, lightly tap the cartridge several times with your fingertip to force air bubbles to the top of the cartridge (see Figure G).
N
While holding the pen with the needle facing up, press the trigger button all the way. The Dota selector will return to zero.
A drop of insulin should appear at the end of the needle. If this does not happen, replace the needle and repeat the procedure, but no more than 6 times.
If a drop of insulin does not appear, the pen is faulty and cannot be used (see Figure H).
Setting the dose
Make sure the dose selector is set to position "0".
I
Turn the dose selector to set the number of units required for injection. The dose can be adjusted by rotating the dose selector in any direction until the correct dose is set opposite the dose indicator. To avoid releasing your insulin dose, be careful when turning the dose selector to avoid accidentally pressing the trigger button.
It is not possible to set a dose greater than the number of units remaining in the cartridge (see Figure I).
— You cannot use the insulin balance scale to measure your insulin dose.
Insulin administration
Insert the needle under the skin. Use the injection technique recommended by your doctor.
J
To inject, press the trigger button all the way until a “0” appears next to the dose indicator. Be careful: when administering the drug, you should only press the start button.
Turning the dose selector will not deliver the drug (see Figure J).
TO
While removing the needle from under the skin, keep the trigger button pressed fully. After injection, leave the needle under the skin for at least 6 seconds. This will ensure that the full dose of insulin is delivered (see Figure K).
L
Guide the needle into the outer needle cap without touching the cap. When the needle is fully inserted, put on the cap and unscrew the needle.
Discard the needle carefully and cap the pen (see Figure L).
— Remove the needle after each injection and never store the FlexPen® pen with the needle attached. Otherwise, liquid may leak out of the pen, which may result in incorrect dosage.
— Caregivers should handle used needles with extreme care to avoid accidental sticking.
— Throw away the used FlexPen® syringe pen with the needle disconnected.
— The FlexPen® syringe pen with the drug Protafan® NM and needles are intended for individual use only, they cannot be transferred to other persons.
Protafan nm suspension for subcutaneous administration 100 units/ml 10 ml
Indications for use Diabetes mellitus type 1. Diabetes mellitus type 2; stage of resistance to oral hypoglycemic drugs, partial resistance to oral hypoglycemic drugs (combination therapy); intercurrent diseases, surgical interventions (mono- or combination therapy), diabetes mellitus during pregnancy (if diet therapy is ineffective).
Compound
Insulin isophane (human genetically engineered).
Pharmacological action
Medium-acting insulin preparation. Reduces the concentration of glucose in the blood, increases its uptake by tissues, enhances lipogenesis and glycogenogenesis, protein synthesis, and reduces the rate of glucose production by the liver. Interacts with a specific receptor on the outer cell membrane and forms an insulin receptor complex. The decrease in glucose content in the blood is due to an increase in its intracellular transport, increased absorption and assimilation by tissues, stimulation of lipogenesis, glycogenogenesis, protein synthesis, a decrease in the rate of glucose production by the liver (decreased glycogen breakdown), etc. After subcutaneous injection, the effect occurs within 1-2 hours. Maximum effect - in the interval between 2-12 hours, duration of action -18-24 hours depending on the composition of insulin and dose, reflects significant inter- and intrapersonal variations. Absorption and onset of action depend on the route of administration (s.c. or i.m.), location (abdomen, thigh, buttocks) and volume of injection, concentration of insulin in the drug, etc. Distributed unevenly in tissues; does not penetrate the placental barrier and into breast milk. Destroyed by insulinase, mainly in the liver and kidneys. Excreted by the kidneys.
Contraindications
Hypersensitivity, hypoglycemia.
Side effect
Allergic reactions (urticaria, angioedema - fever, shortness of breath, decreased blood pressure); hypoglycemia (pallor of the skin, increased sweating, perspiration, palpitations, tremor, hunger, agitation, anxiety, paresthesia in the mouth, headache, drowsiness, insomnia, fear, depressed mood, irritability, unusual behavior, uncertainty of movements, speech disorders and vision), hypoglycemic coma; hyperglycemia and diabetic acidosis (at low doses, skipping an injection, non-compliance with the diet, against the background of fever and infections): drowsiness, thirst, loss of appetite, facial flushing); impairment of consciousness (up to the development of a precomatous and comatose state); transient visual disturbances (usually at the beginning of therapy); immunological cross-reactions with human insulin; an increase in the titer of anti-insulin antibodies with a subsequent increase in glycemia; hyperemia, itching and lipodystrophy (atrophy or hypertrophy of subcutaneous fat) at the injection site. At the beginning of treatment, swelling and refractive error occur (they are temporary and disappear with continued treatment). Interaction
Pharmaceutically incompatible with solutions of other drugs.
The hypoglycemic effect is enhanced by sulfonamides (including oral hypoglycemic drugs, sulfonamides), MAO inhibitors (including furazolidone, procarbazine, selegiline), carbonic anhydrase inhibitors, ACE inhibitors, non-steroidal anti-inflammatory drugs (including salicylates), anabolic steroids (including stanozolol, oxandrolone, methandrostenolone), androgens, bromocriptine, tetracyclines, clofibrate, ketoconazole, mebendazole, theophylline, cyclophosphamide, fenfluramine, Li+ preparations, pyridoxine, quinidine, quinine, chloroquinine, ethanol. The hypoglycemic effect is weakened by glucagon, somatropin, glucocorticosteroids, oral contraceptives, estrogens, thiazide and loop diuretics, BMCC, thyroid hormones, heparin, sulfinpyrazone, sympathomimetics, danazol, tricyclic antidepressants, clonidine, calcium antagonists, diazoxide, morphine, marijuana, nicotine , phenytoin, epinephrine, H1-histamine receptor blockers. Beta-blockers, reserpine, octreotide, pentamidine can both enhance and weaken the hypoglycemic effect of insulin. Overdose
Symptoms: perspiration, palpitations, tremor, hunger, anxiety, paresthesia in the mouth, pallor, headache, drowsiness, insomnia, fear, depressed mood, irritability, unusual behavior, uncertainty of movements, speech and vision disorders, hypoglycemic coma, convulsions . Treatment: if the patient is conscious, dextrose is prescribed orally; Glucagon or a hypertonic dextrose solution is administered subcutaneously, intramuscularly or intravenously. When a hypoglycemic coma develops, 20-40 ml (up to 100 ml) of a 40% dextrose solution is injected intravenously until the patient emerges from the comatose state. Directions for use and dosage
Subcutaneously, 1-2 times a day, 30-45 minutes before breakfast (change the injection site each time).
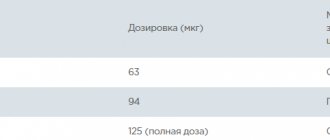
In special cases, the doctor may prescribe intramuscular injections of the drug. Intravenous administration of intermediate-acting insulin is prohibited! Doses are selected individually and depend on the glucose content in the blood and urine, and the characteristics of the course of the disease. Typically doses are 8-24 IU once a day. In adults and children with high sensitivity to insulin, a dose of less than 8 IU/day may be sufficient; in patients with reduced sensitivity, a dose exceeding 24 IU/day may be sufficient. At a daily dose exceeding 0.6 IU/kg - in the form of 2 injections in different places. Patients receiving 100 IU or more per day should be hospitalized when replacing insulin. Transfer from one drug to another should be carried out under the control of blood glucose levels. Special instructions
If foreign bodies appear, cloudiness or precipitation of the substance appears on the glass of the bottle, the drug solution cannot be used. The temperature of the administered insulin should be at room temperature. The insulin dose must be adjusted in cases of infectious diseases, thyroid dysfunction, Addison's disease, hypopituitarism, chronic renal failure and diabetes mellitus in people over 65 years of age. The causes of hypoglycemia can be: insulin overdose, drug replacement, skipping meals, vomiting, diarrhea, physical stress; diseases that reduce the need for insulin, changing the injection site, as well as interaction with other drugs. It is possible to reduce the concentration of glucose in the blood when transferring a patient from animal insulin to human insulin. Transferring a patient to human insulin should always be medically justified and carried out only under the supervision of a physician. The tendency to develop hypoglycemia can impair the ability of patients to actively participate in road traffic, as well as to maintain machines and mechanisms. Patients with diabetes can relieve self-perceived mild hypoglycemia by eating sugar or eating foods high in carbohydrates (it is recommended to always have at least 20 g of sugar with you). It is necessary to inform the attending physician about hypoglycemia in order to decide whether treatment adjustments are necessary. During pregnancy, it is necessary to take into account a decrease (I trimester) or increase (II-III trimesters) in the need for insulin. During and immediately after childbirth, the need for insulin may decrease dramatically. During lactation, daily monitoring is necessary for several months (until insulin needs stabilize). Storage conditions
List B. Store in a cool, dry place at a temperature of 2-8 degrees. WITH.
Instructions for use PROTAPHAN® HM (PROTAPHANE® HM)
The drug is intended for subcutaneous administration. Insulin suspensions cannot be administered intravenously.
Protafan® NM can be used both in monotherapy and in combination with rapid or short-acting insulin.
The dose of the drug is selected individually, taking into account the needs of the patient. Typically, insulin requirements range from 0.3 to 1 IU/kg/day. The daily insulin requirement may be higher in patients with insulin resistance (for example, during puberty, as well as in obese patients), and lower in patients with residual endogenous insulin production.
Protafan® NM is usually administered subcutaneously into the thigh area. If it is convenient, injections can also be made into the anterior abdominal wall, into the gluteal region or into the deltoid muscle of the shoulder. When the drug is administered to the thigh area, slower absorption is observed than when administered to other areas. If the injection is made into a retracted skin fold, the risk of accidental intramuscular injection of the drug is minimized.
The needle should remain under the skin for at least 6 seconds to ensure complete delivery of the dose. It is necessary to constantly change injection sites within the anatomical region to prevent the development of lipodystrophies.
Protafan® NM in vials can only be used together with insulin syringes, which have a scale that allows you to measure the dose of insulin in action units. Detailed recommendations for the use and administration of the drug should be followed (see “Instructions for use of Protafan® NM, which must be given to the patient”).
Dose adjustment
Concomitant diseases, especially infectious ones and those accompanied by fever, usually increase the body's need for insulin. Dose adjustment of the drug may also be required if the patient has concomitant diseases of the kidneys, liver, dysfunction of the adrenal glands, pituitary gland or thyroid gland.
The need for dose adjustment may also arise when the patient's physical activity or usual diet changes. Dose adjustment may be required when transferring a patient from one type of insulin to another.
Precautions for use
Protafan® NM should not be used if it has been frozen.
Before the first use, it is necessary to remove the bottle of Protafan® NM from the refrigerator and allow it to reach room temperature to facilitate mixing of the suspension.
The insulin suspension should not be used if it does not become uniformly white and cloudy after mixing.
Instructions for the use of Protafan® NM that must be given to the patient.
You cannot use Protafan® NM:
- In insulin pumps.
- If you are allergic (hypersensitivity) to human insulin or any of the components included in the drug Protafan® NM.
- If you experience hypoglycemia (low blood sugar).
— If the protective cap is missing or does not fit tightly. Each bottle has a protective plastic cap. If the protective cap on a new bottle is damaged, return the bottle to the pharmacy.
— If the storage conditions of the drug were violated or it was frozen.
— If the insulin does not turn uniformly white and cloudy after stirring.
Before using Protafan® NM:
— Check the label to make sure you are using the right type of insulin.
— Remove the protective cap.
How to administer insulin
The drug Protafan® NM is intended for subcutaneous administration. Never give insulin intravenously or intramuscularly. Always rotate injection sites within the anatomical area to reduce the risk of lumps and ulcerations at the injection site. The best injection sites are:
- buttocks, front thigh or shoulder.
How to administer Protafan® NM if only Protafan® NM is administered or if it is necessary to mix Protafan® NM with short-acting insulin
- Make sure you use an insulin syringe that has a scale that allows you to measure the dose in action units.
— Fill the syringe with air in an amount corresponding to the required dose of insulin.
— Follow the instructions your doctor or nurse gives you.
— Immediately before taking the dose, roll the bottle between your palms until the insulin becomes uniformly white and cloudy. Resuspension is facilitated if the preparation is at room temperature.
— Inject insulin under the skin. Use the injection technique recommended by your doctor or nurse.
— Hold the needle under the skin for at least 6 seconds to ensure that the entire dose of insulin is injected.
Insulin Protafan HM penfill suspension for subcutaneous injection 100 IU/ml cartridge 3 ml No. 5
Indications
Diabetes mellitus type 1; type 2 diabetes mellitus: stage of resistance to oral hypoglycemic agents, partial resistance to these drugs (with combination therapy), intercurrent diseases; type 2 diabetes mellitus in pregnant women.
pharmachologic effect
Medium-acting human insulin produced using recombinant DNA technology. Interacts with a specific receptor on the outer cytoplasmic membrane of cells and forms an insulin-receptor complex that stimulates intracellular processes, incl. synthesis of a number of key enzymes (hexokinase, pyruvate kinase, glycogen synthetase). The decrease in blood glucose levels is due to an increase in its intracellular transport, increased absorption and assimilation by tissues, stimulation of lipogenesis, glycogenogenesis, and a decrease in the rate of glucose production by the liver.
The duration of action of insulin drugs is mainly determined by the rate of absorption, which depends on several factors (for example, dose, route and site of administration), and therefore the insulin action profile is subject to significant fluctuations, both between different people and within the same person. person.
On average, after subcutaneous administration, this insulin begins to act after 1.5 hours, the maximum effect develops between 4 hours and 12 hours, the duration of action is up to 24 hours.
Drug interactions
The hypoglycemic effect of insulin is enhanced by oral hypoglycemic drugs, MAO inhibitors, ACE inhibitors, carbonic anhydrase inhibitors, non-selective beta-blockers, bromocriptine, octreotide, sulfonamides, anabolic steroids, tetracyclines, clofibrate, ketoconazole, mebendazole, pyridoxine, theophylline, cyclophosphamide, fenfluramine, drugs lithium, preparations containing ethanol.
The hypoglycemic effect of insulin weakens glucagon, somatropin, estrogens, oral contraceptives, GCS, iodine-containing thyroid hormones, thiazide diuretics, “loop” diuretics, heparin, tricyclic antidepressants, sympathomimimetics, Danazole, clonidine, epinephrine, and hystamin-re-re-N1-RRETRICA Ceptors, slow calcium channel blockers , diazoxide, morphine, phenytoin, nicotine.
Under the influence of reserpine and salicylates, it is possible to both weaken and enhance the action of insulin.
Reduces tolerance to ethanol.
Dosage regimen
For subcutaneous administration only. The dose of the drug is determined by the doctor individually in each specific case, based on the concentration of glucose in the blood.
On average, the daily dose ranges from 0.5 to 1 IU/kg body weight (depending on the individual characteristics of the patient and blood glucose concentration).
Contraindications for use
Increased sensitivity to insulin; hypoglycemia.
Restrictions for children
No data
Use in elderly patients
Use with caution in elderly patients. Dose adjustment is necessary.
Restrictions for elderly patients
No data
Use for liver dysfunction
Use with caution in patients with impaired liver function. Dose adjustment is necessary.
Restrictions for liver dysfunction
Use with caution
Use during pregnancy and breastfeeding
There are no restrictions on the treatment of diabetes mellitus with insulin during pregnancy, because insulin does not cross the placental barrier. When planning pregnancy and during it, it is necessary to intensify the treatment of diabetes mellitus. Insulin requirements usually decrease in the first trimester of pregnancy and gradually increase in the second and third trimesters.
During and immediately after childbirth, the need for insulin may decrease dramatically. Shortly after birth, insulin requirements quickly return to pre-pregnancy levels.
Restrictions when breastfeeding
Possible use
Restrictions during pregnancy
Possible use
Use for renal impairment
Use with caution in patients with impaired renal function. Dose adjustment is necessary.
Restrictions for impaired renal function
Use with caution
special instructions
During insulin therapy, constant monitoring of blood glucose concentration is necessary.
In addition to insulin overdose, the causes of hypoglycemia can be: drug replacement, skipping meals, vomiting, diarrhea, increased physical activity, diseases that reduce the need for insulin (impaired liver and kidney function, hypofunction of the adrenal cortex, pituitary gland or thyroid gland), change of injection site, as well as interactions with other drugs.
Incorrect dosing or interruptions in insulin administration, especially in patients with type 1 diabetes, can lead to hyperglycemia. Typically, the first symptoms of hyperglycemia develop gradually over several hours or days. They include the appearance of thirst, increased urination, nausea, vomiting, dizziness, redness and dryness of the skin, dry mouth, loss of appetite, and the smell of acetone in the exhaled air. If left untreated, hyperglycemia in type 1 diabetes can lead to life-threatening diabetic ketoacidosis.
The dose of insulin must be adjusted in cases of thyroid dysfunction, Addison's disease, hypopituitarism, liver and kidney dysfunction, and diabetes mellitus in patients over 65 years of age.
Due to the increased risk of cardiac and cerebral complications of hypoglycemia, insulin should be used with caution in patients with severe stenosis of the coronary and cerebral arteries.
With caution in patients with proliferative retinopathy, especially those not receiving treatment with photocoagulation (laser coagulation) due to the risk of amaurosis (total blindness).
If the patient increases the intensity of physical activity or changes the usual diet, adjustment of the insulin dose may be necessary.
Concomitant diseases, especially infections and conditions accompanied by fever, increase the need for insulin.
Transferring a patient to a new type of insulin or an insulin preparation from another manufacturer must be done under the supervision of a physician.
When using insulin drugs in combination with drugs of the thiazolidinedione group in patients with type 2 diabetes mellitus, fluid retention in the body may occur, which increases the risk of development and progression of chronic heart failure, especially in patients with diseases of the cardiovascular system and the presence of risk factors for chronic heart failure. heart failure. Patients receiving such therapy should be monitored regularly for signs of heart failure. If heart failure occurs, therapy should be carried out in accordance with current standards of care.
Side effect
Side effects due to the effect on carbohydrate metabolism:
hypoglycemic conditions (pallor of the skin, increased sweating, palpitations, tremor, hunger, agitation, paresthesia of the oral mucosa, headache, dizziness, decreased visual acuity). Severe hypoglycemia can lead to the development of hypoglycemic coma.
Allergic reactions:
skin rash, angioedema, anaphylactic shock.
Local reactions:
hyperemia, swelling and itching at the injection site, with long-term use - lipodystrophy at the injection site.
Other:
swelling, transient decrease in visual acuity (usually at the beginning of therapy).
Possible product names
- Insulin Protafan HM penfill suspension d/i 100 units/ml penfil 3.0ml N5
- PROTAFAN NM PENFILL 100 UNITS/ML 3 ML No. 5
- PROTAFAN NM PENFILL 100IU/ML 3ML N5 CART
- PROTAFAN NM PENFILL SUSP. FOR P/C INPUT. 100IU/ML CARTRIDGES 3ML No.5
- PROTAFAN NM PENFILL 100IU/ML SUSP. D/SUBCUTANEOUS ENTER 3ML CARTRIDGE X5 (R)