Optic nerve structure
The optic nerve is made up of retinal nerve cells, each of which has more than 1 million axons. Axons carry visual information from the retina to the cerebral visual centers. All retinal nerve fibers are collected in the optic disc.
The part of the nerve located inside the orbit is called intrabulbar. Extending beyond the orbit, the optic nerve penetrates the cranial cavity (retrobulbar part). The end of the nerve is located in the visual centers of the midbrain and diencephalon.
Throughout its entire length, the optic nerve is protected by membranes that are connected to the structures of the orbit, brain and cerebral membranes. Therefore, inflammation from these structures easily penetrates the optic nerve. This is how optic neuritis develops.
General information
Optic neuritis is an inflammatory process in the optic nerve. The disease in most cases involves the trunk and sheaths of the optic nerve (n. Opticus). Among the causes of ocular disability (low vision/blindness), inflammatory diseases of the optic nerve of various origins, according to various authors, occupy from 20 to 28%.
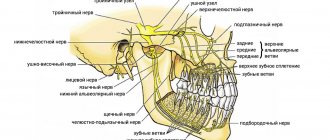
Optic nerve
The optic nerve is the 2nd pair of cranial nerves (cranial nerves), formed by the axons of retinal ganglion cells. The optic nerve is a part of the brain in its development, which distinguishes it from other cranial nerves. It begins with the optic disc located on the retina, exits the eyeball through the cribriform plate of the sclera, heading back in the orbit, then passes into the cranial cavity through the bony optic canal. Further, after leaving the optic canal, the optic nerves at the base of the brain form an incomplete optic chiasm and pass into the optic tracts (Fig. below).
The length of the optic nerve in adults varies between 35-55 mm. Along its length there are several sections:
- Intrabulbar (intraocular) - 0.5-1.5 mm long, the beginning of the nerve from the disc to the point of exit from the sclera.
- Retrobulbar (orbital) - 25-35 m long, from the point where the nerve exits the sclera to the orbital opening of the optic canal.
- Intracanal - 5-8 mm long, from the orbital canal of the optic nerve to its intracranial foramen.
- Intracranial (intracranial) - 4-17 mm long, from the point where the nerve exits the optic canal to the chiasm.
It should be noted that as inflammatory exudate appears and nerve fibers are compressed by edema, as well as the toxic effects of exudate on them, the axial cylinders/myelin sheaths of the optic fibers undergo dystrophic processes, degeneration and atrophy (death of the retinal ganglion mother cell). At the same time, the structural elements of the optic nerve do not possess any regenerative ability.
In accordance with the predominant localization of the inflammatory process, the following are distinguished:
- Actually, optic neuritis (optic neuritis), in which the optic disc is also involved in inflammation. In this case, intrabulbar neuritis can occur with isolated damage to the optic disc (optic disc neuritis/papillitis).
- Retrobulbar neuritis - with a predominant localization of the inflammatory process behind the eyeball.
Since the visual analyzer is connected to the entire body through various physiological/anatomical mechanisms, functional and morphological changes occur in it during general diseases. In fact, most pathological changes in the organ of vision (with the exception of local infections/traumatic injuries) are a manifestation of systemic or general diseases (for example, with progressive chronic demyelinating disease of the central nervous system, multiple sclerosis).
High level of disability due to the development of partial atrophy of n. Opticus, leading to irreversible changes in the visual apparatus, as well as the prevalence of the disease among relatively young people, give optic neuritis a high social significance.
Classification of optic neurites
The first signs may appear unexpectedly and abruptly. Usually the process begins with a decrease in visual acuity or pain in the orbital area. Depending on which part of the visual pathway is affected, retrobulbar and intrabulbar neuritis are distinguished.
Kinds:
- intrabulbar (true) neuritis, when the inflammatory process affects the optic nerve and optic disc inside the orbit;
- retrobulbar neuritis, when inflammation is concentrated behind the eyeball and affects the axial bundle of nerve fibers.
Forecast
In mild cases, optic nerve neuritis is benign and in 75% of cases, visual acuity is restored after 4-6 weeks. However, at the same time, other parameters of the visual analyzer function (contrast sensitivity/color vision) are often not fully restored. Progressive chronic disease leads to persistent disabling disorders - optic nerve atrophy and irreversible vision loss, the development rates of which vary between 22-25%.
Causes
The exact reasons for the development of neuritis remain unknown. Research shows that under certain conditions, the immune system begins to mistakenly attack myelin, the substance that covers the optic nerve. This leads to its damage and the spread of inflammation. Myelin serves to conduct electrical impulses (visual information) from the eyes to the brain. Neuritis is dangerous by disrupting this process and, accordingly, vision itself.
What diseases are associated with optic neuritis:
- Multiple sclerosis. In multiple sclerosis, the autoimmune system begins to attack the lining of the brain and spinal cord. It is believed that after one case of optic neuritis, the risk of developing sclerosis increases by 50%. An MRI scan can detect brain damage after neuritis.
- Neuromyelitis optica. This is an inflammation that simultaneously affects the optic nerve and spinal cord. A condition similar to multiple sclerosis, but with less damage to the nerves in the brain.
- Inflammatory processes in the brain and its membranes (meningitis, encephalitis, arachnoiditis).
- General diseases (diabetes mellitus, gout, blood diseases, sarcoidosis, lupus).
The development of the disease is often associated with acute or chronic general infections (syphilis, Lyme disease, measles, herpes, mumps, tuberculosis, brucellosis, gonorrhea, malaria, erysipelas, smallpox, typhus, diphtheria, tonsillitis, influenza). Even nasopharyngeal infections such as tonsillitis, otitis, sinusitis, sinusitis, and pharyngitis can play a role.
Ophthalmological reasons:
- inflammation of the orbit (phlegmon, periostitis);
- inflammation of the eyeball (iridocyclitis, keratitis, retinitis, panophthalmitis).
Often the cause of the onset or recurrence of neuritis is intoxication due to alcoholism. Women with pathological pregnancies and people with traumatic brain injuries are also at risk. Sometimes inflammation of the optic nerve is associated with taking medications (especially quinine and some antibiotics).
Symptoms
One of the main symptoms of ocular neuritis is a sharp deterioration in vision - it is observed in more than 90% of patients. Most often, only one eye is affected.
The second obligatory symptom is considered to be a violation of color vision - that is, the ability to perceive all the colors of the spectrum, interpret them correctly and distinguish between tones and shades. In the case of inflammation of the optic nerve, the picture acquires problems similar to color blindness; symptoms can manifest themselves in the form of complete color blindness or be characterized by a partial impairment of color perception.
A manifestation such as the positive Uthoff phenomenon is also a symptom of ocular neuritis. This is a clinical syndrome characteristic of patients with multiple sclerosis, which consists of a worsening of the mental and neurological symptoms of the disease - patients feel increased fatigue, weakness, tiredness, impaired attention, memory and other cognitive skills. The relationship of the phenomenon to optic neuritis can be explained by the fact that there is a certain connection between this disease and multiple sclerosis. Thus, it is believed that in 50% of patients, neuritis is the first sign of multiple sclerosis, and in patients with this form of sclerosis, neuritis manifests itself in approximately 40-50% of cases.
A third of patients complain of the appearance of optical phenomena - a kind of visual hallucinations, similar to the effect of the use of hallucinogenic or psychotropic substances, but caused by inadequate stimulation in the parts of the visual analyzer. The most common manifestation of neuritis is photopsia, characterized by the appearance of false moving images before the eyes, such as sparks, flashes, luminous circles, and so on. When the eye is inflamed, patients feel pain in the orbit, nausea occurs, darkening of the eyes, and with neuritis the eye swells.
What happens with optic neuritis
Optic neuritis begins with infiltration and proliferation. The inflammatory process passes from the soft membrane of the brain to the nerve fibers. Inflammation can develop in the optic nerve trunk or sheaths.
Tissue inflammation occurs with the involvement of leukocytes, lymphocytes and plasma cells. Infiltration and swelling will compress the fibers, impairing their functions and causing vision impairment. Subsequently, neovascularization develops and connective tissue is formed. Secondary damage to nerve fibers occurs.
After the acute phase, individual fibers can recover, but severe inflammation leads to total breakdown of the fibers and proliferation of glial tissue. Persistent neuritis leads to optic nerve atrophy with irreversible deterioration of visual function.
If the cause of neuritis is multiple sclerosis, the disorder is based on demyelination of the fibers, that is, destruction of the myelin sheath. Despite the fact that the process of demyelination is not inflammation, such a lesion is identical to neuritis in clinical symptoms. Therefore, destruction of the optic nerve in multiple sclerosis is equated to retrobulbar neuritis.
Disease prevention
To prevent optic neuritis, it is recommended to give up bad habits, promptly treat infectious diseases, avoid eye and head injuries, and visit specialized doctors in the presence of chronic pathologies.
Article sources:
- Retrobulbar optic neuritis. Kukhtik S.Yu., Popova M.Yu., Tantsurova K.S. Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region, 2016
- Visualization of the optic nerve in the diagnosis and monitoring of retrobulbar neuritis. Yuryeva T.N., Burlakova E.V., Khudonogov A.A., Ayueva E.K., Sukharchuk O.V. Acta Biomedica Scientifica, 2011. p. 133-136
- Modern view on the problem of optic neuritis (systematic review). Krivosheeva M.S., Ioileva E.E. Saratov Scientific and Medical Journal, 2021. p. 602-605
- Results of treatment of optic neuritis. Latypova E.A. Saratov Scientific and Medical Journal, 2021. p. 875-879
Clinical picture
Symptoms of neuritis usually appear in only one eye. Inflammation is characterized by impaired visual functions and a narrowing of the visual field. The degree of visual impairment with neuritis depends on changes in the papillomacular bundle. Typically, the narrowing of the visual field is concentric, and central and paracentral scotomas (blind spots) occur. There may be a complete lack of color perception. The optic disc protrudes only when neuritis is combined with edema.
Symptoms of intrabulbar neuritis
Intrabulbar neuritis lasts 3-6 weeks. If treatment is started in time, complete restoration of vision is possible. In severe and advanced cases, there is a risk of complete loss of vision in the affected eye.
Damage to the optic nerve in the area located inside the eyeball always begins acutely. The first symptoms appear within 1-2 days, the patient’s condition deteriorates very quickly. The severity of symptoms will depend on the degree of damage to the optic nerve.
Characteristic symptoms of intrabulbar neuritis:
- Scotomas (blind spots in the field of vision). This symptom is observed in most patients with neuritis. With inflammation of the optic nerve, central scotomas predominate.
- Deterioration of vision (mainly myopia). Visual impairment is diagnosed in every second person with inflammation. Initially, visual acuity decreases by 0.5-2 diopters, but as the optic nerve is damaged, complete blindness may occur. Depending on the quality of treatment and the aggressiveness of the inflammation, blindness may be reversible or incurable.
- Deterioration of twilight vision. The eyes of a healthy person quickly adapt to poor lighting conditions (40-60 seconds), but with inflammation, the visual system begins to distinguish objects in the dark only after 3 minutes or more. Typically, deterioration of twilight vision occurs on the side of the affected eye.
- Change of color perception. With optic neuritis, patients lose the ability to distinguish certain colors. Due to nerve irritation, colored spots may appear in the field of vision.
Symptoms of retrobulbar neuritis
Inflammation of the nerve outside the orbit is diagnosed less frequently. Since in this zone the nerve is not surrounded by fiber and lies freely, the infection can affect the outer surface or the inner surface - peripheral and axial neuritis, respectively.
Symptoms:
- Axial: decreased visual acuity by 3-6 diopters, one-sided blindness, central scotomas.
- Peripheral: visual acuity remains normal, a decrease in the visual field from the periphery, dull pain in the orbit (intensified by movement of the eyeball, relieved by non-steroidal anti-inflammatory drugs and glucocorticosteroids).
Transverse neuritis, when the infection affects the entire thickness of the nerve, combines signs of two types of retrobulbar inflammation. Retrobulbar neuritis is characterized by the appearance of a central absolute scotoma. At first the spot is large, but as vision improves it becomes smaller and may disappear. Sometimes a central scotoma can turn into a paracentral annular scotoma.
At first, with retrobulbar neuritis, the fundus of the eye remains in a normal state, but slight hyperemia and blurring of the boundaries of the optic disc are possible. Usually the inflammation affects one eye, the disc enlarges, the boundaries are not defined, the veins expand and twist. Sometimes the clinical picture of retrobulbar neuritis resembles a congestive disc.
There are acute and chronic retrobulbar neuritis. In acute neuritis, a decrease in visual acuity occurs over 2-3 days, and in chronic neuritis, it occurs gradually. Acute inflammation is accompanied by pain behind the eyeball. Vision begins to return after a few days, although in rare cases this may not occur.
Toxic neuritis
Typically, toxic neuritis is caused by methyl alcohol poisoning. In addition to the symptoms of poisoning, after 1-2 days the vision in both eyes drops sharply (up to complete blindness). The patient's pupils dilate and the reaction to light is weakened or absent. Mild hyperemia of the optic disc is possible; in rare cases, symptoms of ischemic neuritis occur (pale disc, blurred borders, narrowed arteries).
Serious disorders in the papillomacular bundle develop with chronic alcoholism and smoking strong tobacco with a high nicotine content. Alcohol and tobacco intoxication is diagnosed mainly in men over 30 years of age.
The disease occurs as a chronic retrobulbar inflammation. Changes in the fundus are not observed, only occasionally there is slight hyperemia of the optic disc. A central scotoma appears, but the peripheral boundaries of the visual fields remain normal. By giving up bad habits, vision improves and blind spots decrease.
Neuritis in tuberculosis
In this case, the development of ordinary neuritis or solitary optic disc tubercle is possible. Tubercle is a tumor-like formation on the surface of the disc that spreads to the retina.
Neuritis in diabetes
Neuritis associated with diabetes mellitus is usually diagnosed in men. Chronic inflammation is often bilateral, and vision deteriorates slowly. Central scotomas occur, although the peripheral boundaries of the visual fields remain normal. Initially, the optic disc is normal, but with the development of inflammation, temporal pallor is observed.
Neuritis in neurosyphilis
Against the background of relapse of neurosyphilis, an edematous form of neuritis is usually diagnosed. There are two possible options for the development of inflammation: mild (hyperemia and unclear boundaries) and severe papillitis (sharp deterioration of vision). Rarely, papulous neuritis develops when the disc is hidden behind a massive gray-white exudate that protrudes into the vitreous.
Advantages of treatment in Israel
- High level of qualifications and experience of doctors.
- Equipping clinics with modern equipment.
- Development of an individual comprehensive therapeutic program.
- Comfortable conditions for staying in the clinic.
- Reasonable prices.
Completing a full course of therapy in the initial stages of the disease will make it possible, after a short time, to restore visual functions and return to normal life. Don’t waste time, contact the clinic of your choice and start treatment.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
Diagnosis of optic neuritis
It is easy to recognize a typical case of optic neuritis. It is much more difficult to diagnose mild neuritis or inflammation with edema, which are similar to pseudoneuritis and congestive disc. The main difference is the preservation of visual functions.
If there are symptoms of increased intracranial pressure, a spinal tap is performed to confirm a congestive disc. It is most difficult to distinguish neuritis from edema or complications of a stagnant disc, since in both cases there are visual disturbances.
The diagnosis of neuritis can be confirmed by the presence of small hemorrhages or foci of exudate in the disc tissue or retina. The most informative method for diagnosing optic neuritis is fluorescein angiography of the fundus.
Signs of neuritis according to the severity of the process:
- mild: moderate hyperemia of the optic disc, unclear boundaries of the optic disc, dilatation of arteries and veins;
- pronounced: sharp hyperemia of the disc, the boundaries of the disc merge with the retina, white spots and many hemorrhages appear in the peripapillary zone;
- transition to atrophy: disc blanching, narrowing of arteries, resorption of exudate and hemorrhages.
Tests and diagnostics
The diagnosis of optic neuritis is made based on a thorough history (pre-existing diseases, symptoms, rate of progression) and ophthalmological/neurological examination of the patient.
Ophthalmological examinations include:
- Visometry. Characteristic is a decrease in visual acuity to 0.1-0.2 diopters, less often to light perception, which cannot be corrected by lenses.
- Determination of color perception using color tables. Characterized by a decrease in color saturation/brightness.
- Perimetry. Characteristic is the presence of scotomas (central, peripheral, paracentral) in the visual fields.
- Ophthalmoscopy. Allows you to determine hyperemia/swelling of the optic disc, the presence of petechial hemorrhages, disc pallor (with the development of atrophy).
- Tonometry. In order to identify increased IOP, characteristic of a number of diseases that can contribute to the development of neuritis.
Neurological studies to assess the neurological status of the patient, allowing to identify cerebral/focal cerebral:
- MRI of the brain/orbit of the eye. To visualize brain pathology (areas of demyelination, inflammatory foci, tumor) and identify compression/edema/damage to the orbital part of the n. Opticus. X-ray of the paranasal sinuses/chest organs.
- Ultrasound of the optic nerve.
- Study of cerebrospinal fluid (chemical/cellular composition of the cerebrospinal fluid).
To identify the etiology of optic neuritis, blood cultures for sterility, ELISA/PCR studies, consultations with an immunologist, neurologist, infectious disease specialist, endocrinologist and other specialists may be prescribed.
Differential diagnosis of optic neuritis is carried out with intrabulbar lesions, ischemic optic neuropathy, and neuromyelitis optica. With the gradual development of atrophy n. Opticus it is necessary to exclude the hereditary mitochondrial disease Leber's disease (syn. Leber's syndrome).
Treatment of optic neuritis
If neuritis is suspected, the patient must be hospitalized immediately. Until the reasons are clarified, drugs are prescribed to suppress infection and inflammation, as well as measures for dehydration, desensitization, immunocorrection and improvement of metabolism.
Treatment regimen:
- For 5-7 days antibiotics (injections or droppers). Do not use drugs with ototoxic effects (Streptomycin, Gentamicin, Kanamycin, Neomycin).
- Retrobulbar administration of corticosteroids is indicated (dexamethasone solution 0.4%, 1 ml for 10-15 days). Orally Prednisolone 0.005 g 4-6 times a day for 5 days with a reduction in dosage.
- Diacarb orally 0.25 g three times a day (after three days of taking two days off), while taking Panangin 2 tablets three times a day.
- The dosage of Glycerin is calculated from the ratio of 1-1.5 g/kg body weight.
- 10 ml of magnesium sulfate solution 25% is injected intramuscularly.
- Intravenous glucose 40%, hexamethylenetetramine solution 40%.
- Intranasal tampons with 0.1% adrenaline solution every day for 20 minutes with constant monitoring of blood pressure levels.
- B vitamins orally.
- Piracetam up to 12 g per day.
- Solcoseryl intramuscularly.
- Dibazol 10 mg twice a day for 2-3 months.
After determining the diagnosis, the underlying disease is treated and the patient’s condition is normalized for chronic disorders. In the case of toxic retrobulbar neuritis, similar treatment is carried out, excluding antibiotics. Additionally, detoxification of the body is required: taking a 30% ethyl alcohol solution (first 90-100 ml, then 50 ml every 2 hours).
Optic neuritis cannot be ignored. Any inflammation in the visual system without treatment can lead to blindness, so at the first signs of neuritis you should urgently consult a therapist or ophthalmologist.
Sources used:
- Vitreous replacement in eye surgery / G.G. Bordyugova. - M.: Medicine, 2002.
- Ophthalmological manifestations of common diseases / E.A. Egorov, T.V. Stavitskaya, E.S. Tutaeva. - M.: GEOTAR-Media, 2009.
- Penetrating wounds and contusions of the eye / R.A. Gundorova, G.A. Petropavlovskaya. - M.: Medicine, 1975.
- The University of Chicago's Department of Ophthalmology and Visual Science
List of sources
- Borisevich E. S. Clinical manifestations, diagnosis and outcomes of optic neuritis / Borisevich E. S., Shamal D. Yu., Klyuiko Yu. D., Kachan T. V. // Young scientist. - 2021. - No. 13 (147). — pp. 146-149.
- Zhaboedov G.D. Lesions of the optic nerve / G.D. Zhaboyedov, R.L. Skripnik // GEOTAR-Media. - 2006. - 286 p.
- Gustov A.V. Practical neuro-ophthalmology / Gustoe A.V., Sigriansky K.I., Stolyarova Zh.P. // Nizhny Novgorod State Medical Academy, 2014. - pp. 260-263.
- Kruzhkova G.V. Pathology of the fundus and optic nerve/G.V. Kruzhkova, M.S. Agronovich //MEDpress-inform, 2014. - pp. 32-35.
- Kanski, D. Clinical ophthalmology: a systematic approach. - M.: Logosphere., 2006. - 744 p.