Pain in the region of the costal arches is a fairly common symptom and intercostal neuralgia often has to be differentiated from pain of a cardiogenic nature. The term intercostal neuralgia means the involvement of the intercostal nerves and the presence of pain. The causes of intercostal neuralgia can be various diseases that lead to damage to nerve fibers. First of all, these are degenerative diseases of the spine (osteochondrosis, hernia, disc protrusion, spondylosis), rheumatological diseases such as ankylosing spondylitis, infectious diseases (herpes zoster, brucellosis, tuberculosis).
These may be diseases of the nervous system such as multiple sclerosis, polyradiculoneuropathy, systemic diseases (diabetes mellitus, hepatitis), vitamin deficiency due to alcoholism or malabsorption in the gastrointestinal tract. Damage to the intercostal nerves is possible due to intoxication (heavy metals, some drugs).
When the blood supply to the nerves is disrupted, hypoxia of the nerve trunks occurs and this occurs in cardiovascular diseases (hypertension, atherosclerosis) and anemia. Disturbances in the endocrine system can lead to changes in the spine, which in turn lead to intercostal neuralgia (thyrotoxicosis, adrenal diseases, endocrine system disorders in postmenopausal women). So there are quite a lot of factors contributing to the development of intercostal neuralgia and, as a rule, a combination of factors is important, and not just one factor. Intercostal neuralgia occurs most often in elderly people, when there are involutional changes in the spine and in the body
Symptoms
The main symptom of intercostal neuralgia is pain in the ribs, which has an acute burning character, sometimes dull. The pain can develop in paroxysms or appear periodically. During attacks, the pain can be intense and intensify with coughing, sneezing, and body movements. The pain is usually localized in the area of the lower ribs and can radiate to the shoulder or arm, which often makes such attacks of pain similar to cardialgia. Pain with intercostal neuralgia from pain in the heart in the more constant nature of the pain intensity, and in the absence of changes in the cardiovascular system (changes in pulse, pressure).
In addition, cardiogenic pain does not increase with trunk movement and there is no local tenderness in the rib area. Pain during intercostal neuralgia may be accompanied by vegetative manifestations (pallor or redness of the skin, sweating), fasciculations of muscle groups, impaired sensitivity in the area of pain (numbness). Palpation of the area of paravertebral points in the intercostal spaces in the area of attachment of the ribs to the sternum can be painful. Sometimes pain with intercostal neuralgia can radiate to the lower back and simulate renal colic.
Forms
There is no special classification of the disease. There are several separate forms depending on the mechanism of occurrence:
- radicular: associated with irritation of the spinal cord roots at the point of their exit from the spinal column;
- reflex: associated with overstrain of muscle fibers at the site of the nerve passage.
There is also a classification of neuralgia depending on:
- causes: primary (associated with damage or inflammation of the nerve itself) and secondary (due to other diseases);
- localization: unilateral and bilateral;
- course of the disease: acute and chronic.
Diagnostics
With classic manifestations, the diagnosis of intercostal neuralgia is not difficult (for example, with the consequences of herpes zoster). But given the possibility of pain in the rib area due to numerous diseases, it is often necessary to conduct a thorough examination. The diagnosis of intercostal neuralgia can be made based on the patient’s history of complaints (nature of pain, localization, intensity, duration of pain, presence of irradiation, increased pain with body movements), external examination (presence of spinal deformities), presence of pain on palpation in the area of attachment of the ribs to the sternum or paravertebral points in the thoracic spine. If it is necessary to differentiate with the cardiac nature of pain, an ECG is necessary. To identify degenerative changes in the spine, instrumental research methods such as radiography, CT, and MRI are used. In addition, densitometry is necessary to diagnose osteoporosis. EMG can be used to determine the extent of nerve fiber damage. Laboratory tests and ultrasound may be ordered to diagnose both rheumatological diseases and endocrine disorders or kidney diseases. The approach to diagnosing intercostal neuralgia should be based on the exclusion, first of all, of somatic causes of pain (heart disease, kidney disease, endocrine diseases).
Neuralgia during pregnancy
If intercostal neuralgia appears in a pregnant woman, how to diagnose it and how to treat it is decided by a neurologist together with a gynecologist. Therapy is selected taking into account possible negative effects on the fetus. Self-medication in this situation is considered unacceptable, as this can have a negative impact on the health of the expectant mother and child.
To prevent chest neuralgia from appearing during pregnancy, it is advisable to follow preventive measures. If a woman has previously had attacks of thoracalgia, then at the stage of preconception preparation she should visit a neurologist and osteopath. The doctor will conduct a diagnosis, and then the neurologist will give a number of recommendations on how to treat intercostal neuralgia. An osteopath will identify possible causes of neuralgia and conduct a treatment session aimed at eliminating them.
Treatment at the Energy of Health clinic
Doctors at the Energy of Health clinic will always come to the aid of patients with intercostal neuralgia. We offer each client:
- a full examination with consultations with specialists for an accurate diagnosis;
- individual selection of treatment regimen;
- services of a qualified chiropractor;
- own exercise therapy room for the most effective and safe exercises;
- modern methods of physiotherapy;
- massotherapy;
- drug blockades for severe pain syndrome.
Regular observation by a neurologist after the acute period of the disease has subsided will help prevent recurrent attacks.
Reviews
Most of the patients managed to cure intercostal neuralgia, since they consulted a doctor on time and followed his recommendations. But in some cases, therapy was delayed due to diagnostic difficulties.
Valery, 39 years old: “I had my first attack of neuralgia 2 years ago. I suffered for a week, and then went to the doctor. The pain was due to hypothermia. I was prescribed medications, vitamins, and physical therapy. I completed the course and the pain subsided. Now I am fighting the disease with the help of physical therapy and massage. There was no relapse."
Alina, 45 years old: “I turned to a neurologist at the very height of my illness. To relieve the pain, I was prescribed NSAIDs. Then I found a good manual therapist who helped consolidate the result. In addition, she attended reflexology sessions. At home, she massaged the sore areas with warming ointments and performed a set of exercises. It’s been a year now and the pain doesn’t bother me.”
Elena, 42 years old: “I believe that first of all you need to understand what exactly caused the intercostal neuralgia. If there are problems with the spine, then there is no point in taking a lot of medications, putting blockades, you need to find a good chiropractor. I was given blockades for about 4 weeks to relieve severe pain, but there was no point, it returned very soon. Only after treatment by a chiropractor, who corrected the displaced vertebrae, the pain disappeared. Now I do gymnastics and go to massage to prevent a relapse.”
Treatment
Intercostal neuralgia requires complex and often long-term treatment, including medication, physiotherapy, massage, etc.
Drug therapy
In the acute phase of the disease, therapy is aimed at relieving pain and improving the patient's condition. Depending on the specific clinical situation, the following are prescribed:
- non-steroidal anti-inflammatory drugs (NSAIDs): products based on diclofenac, nimesulide, ibuprofen, meloxicam and their derivatives; used in tablet, injection and local (creams, ointments, patches) form;
- analgesics: analgin and products based on it; like NSAIDs, they relieve pain;
- muscle relaxants to eliminate muscle spasms: mydocalm, etc.;
- group vitamins: milgamma, neuromultivitis, etc.; necessary to restore normal functioning of nerve fibers;
- sedatives to reduce the psycho-emotional component of pain and improve sleep.
If necessary, the following may additionally be prescribed:
- anticonvulsants: inhibit the passage of pain impulses;
- antidepressants to relieve tension;
- antihistamines and diuretics: relieve tissue swelling, especially relevant for pinched nerve roots;
- antiviral drugs for herpes zoster;
- glucocorticosteroids for persistent pain and severe inflammation that cannot be relieved by milder means.
Physiotherapy and exercise therapy
Physiotherapeutic procedures are prescribed after the acute pain subsides. Help speed up recovery:
- UHF;
- reflexology;
- magnetic therapy;
- electrophoresis;
- laser treatment;
- paraffin applications;
- mud therapy.
These procedures help improve blood circulation and metabolism in the affected area and accelerate the regeneration of nerve tissue.
Physical therapy exercises are prescribed after complete recovery. The main goal of gymnastics is to unload the back muscles. The complex is developed individually. The first classes should be carried out under the supervision of a specialist; in the future, home exercises are allowed.
Other treatments
Since very often the cause of intercostal neuralgia is pathology of the spine and spinal cord, the following are often used as additional methods of influence:
- acupuncture;
- manual therapy;
- therapeutic massage, including the use of warming agents;
- Shiatsu massage (acupressure);
- osteopathy;
- underwater traction and other techniques.
Like all medical procedures, these techniques are used only in a clinical setting and are carried out by specialists with medical education and the appropriate certificate.
Complications of the disease
Complications arising from neuralgia can be successfully treated in the early stages of the development of the disease. But in advanced cases, when the patient experiences pain for quite a long time, the “problem” nerve may even die. Then the excruciating pain disappears, but this is the first sign of the disease moving to a new stage, for which the characteristic symptoms are shortness of breath and the appearance of a feeling of heaviness in the chest.
Finding a person in a constant sitting position or other static position can result in dysfunction of the spinal canal and the development of osteochondrosis and other related pathologies. The occurrence of complications can only be prevented by timely treatment and prevention.
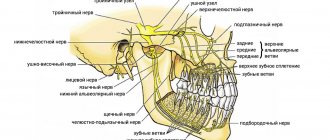
Structure of nerves
Intercostal nerves consist of several types of fibers: motor, sympathetic and those responsible for sensitivity. Each of these nerve endings is located in the intercostal space and runs along the lower edge of each rib. The closing pair of nerve roots is called “subcostal” and is located under the 12th rib.
Each pair of nerve fibers is covered by a special pleura, starting from the spinal canal to the corners of the ribs. The intercostal nerves are responsible for the sensitivity of the muscle tissue of the chest, abdomen and mammary glands, and also innervate the skin in these areas of the body.
Analgesics
A number of patients do without medications in this group, but if the patient experiences severe pain attacks, then it is necessary to relieve them with painkillers. The most popular analgesics based on analgin are Baralgin, Sedalgin, Spazmalgon. As soon as severe pain subsides, you should stop taking them.
These tablets also have a number of disadvantages and side effects, in particular on the digestive tract. If the patient additionally uses ointments and creams with an anesthetic component, then it is necessary to take into account the total amount of the product that the patient receives.
Prevention
Prevention of intercostal neuralgia is mainly general measures aimed at strengthening the muscle frame and improving the health of the body. Neurologists recommend:
- lead an active lifestyle, play sports at an amateur level;
- minimize hypothermia and colds;
- watch your posture;
- avoid lifting heavy objects;
- maintain a high level of immunity;
- eat a balanced diet, if necessary, take additional vitamins, especially group B;
- treat chronic diseases in a timely manner;
- avoid stress, get proper rest and ensure yourself at least 8 hours of sleep every night.
Following these simple rules will significantly reduce the risk of developing intercostal neuralgia.