Instructions for use NOVARING
To achieve an effective contraceptive effect, the drug NuvaRing must be used as indicated in the subsections “How to use NuvaRing” and “How to start using NuvaRing.”
Children
Safety and effectiveness of the drug NuvaRing in adolescents aged
under 18 years of age were not studied.
How to use NuvaRing
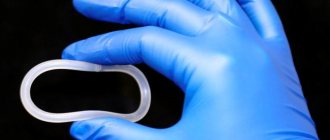
A woman can insert NuvaRing into her vagina on her own. The doctor should inform the woman how to insert and remove the NuvaRing. To insert the ring, the woman should choose a comfortable position, for example, standing, raising one leg, squatting or lying down. NuvaRing should be squeezed and inserted into the vagina until the ring is in a comfortable position. The exact position of the NuvaRing ring in the vagina is not decisive for the contraceptive effect (Fig. 1-4).
After insertion (see “How to start using NuvaRing”), the ring should be in the vagina continuously for 3 weeks. It is advisable for a woman to regularly check whether the NuvaRing ring remains in the vagina. If the ring was accidentally removed, the woman should follow the instructions in the section “What to do if the ring was temporarily removed from the vagina” (for more information, see also the section “Prolapse”).
NuvaRing should be removed after 3 weeks on the same day of the week that it was inserted into the vagina. After a one-week break, a new ring is inserted (for example, if the NuvaRing ring was installed on Wednesday at approximately 10:00 pm, it should be removed on Wednesday 3 weeks later at approximately 10:00 pm. A new ring is inserted on the next Wednesday). To remove the ring, you need to pick it up with your index finger or squeeze it with your index and middle fingers and pull it out of the vagina (Fig. 5).
The used ring should be placed in a bag (keep out of the reach of children and pets) and discarded. Bleeding associated with the discontinuation of the NuvaRing usually begins 2-3 days after removal of the NuvaRing and may not completely stop until a new ring is installed.
How to start using NuvaRing
No hormonal contraceptives were used in the previous cycle
NuvaRing should be inserted on the first day of the cycle (that is, the first day of menstruation). It is possible to install the ring on days 2-5 of the cycle, however, in the first cycle in the first 7 days of using NuvaRing, additional use of barrier methods of contraception is recommended.
Switching from combined hormonal contraceptives
A woman should be given NuvaRing no later than the day after the end of her usual pill-free, patch-free, or placebo-pill period of her previous combined hormonal contraceptive.
If a woman has been taking the combined hormonal contraceptive correctly and regularly and is confident that she is not pregnant, she can switch from using the previous method to using the vaginal ring on any day of the cycle.
After the previous method of contraception, the duration of the interval without the use of hormonal contraceptives should not exceed the recommended period.
Switching from progestogen-only (mini-pill, implant, or injection) or progestogen-releasing intrauterine device (IUD)
A woman taking the mini-pill can switch to using NuvaRing any day. When switching from using an implant or IUD, the ring is inserted on the day the implant or IUD is removed. When switching from an injectable contraceptive, the ring is inserted on the day when the next injection is due. In all these cases, it is necessary to use an additional barrier method of contraception during the first 7 days after insertion of the NuvaRing ring.
After an abortion in the first trimester
A woman can insert the ring immediately after an abortion. In this case, she does not need additional contraceptives. If the use of the NuvaRing ring immediately after an abortion is undesirable, you must follow the recommendations given in the section “Hormonal contraceptives were not used in the previous cycle.” During the period before the ring is inserted, the woman should be advised to use an alternative method of contraception.
After childbirth or abortion in the second trimester
For information regarding breastfeeding, see the Pregnancy and Lactation section.
A woman should be advised to have the ring inserted in the 4th week after childbirth or second trimester abortion. If the ring is installed at a later date, it is recommended to use an additional barrier method of contraception during the first 7 days after insertion of the ring. If sexual contact has already taken place, then before inserting the ring, pregnancy should be excluded or the use of NuvaRing should be postponed until the start of the first menstrual period.
When resuming use of the drug NuvaRing in the postpartum period, the increased risk of venous thromboembolism (VTE) should be taken into account (see section "Special Instructions").
Deviations from the recommended regime
The contraceptive effect and cycle control may be impaired if a woman does not comply with the recommended regimen. To avoid a decrease in the contraceptive effect in case of non-compliance, the following recommendations must be followed.
What to do if the break in using the ring exceeds the duration
The woman should insert a new ring as soon as possible. Over the next 7 days, you must additionally use a barrier method of contraception (for example, condoms). If sexual intercourse took place during the break in using the ring, pregnancy should be excluded. The longer the break in using the ring, the higher the likelihood of pregnancy.
What to do if the ring has been temporarily removed from the vagina
The NuvaRing ring must remain in the vagina continuously for 3 weeks. If the ring is accidentally removed, it should be washed with cold or warm (not hot) water and immediately inserted into the vagina.
If the NuvaRing was left outside the vagina for less than 3 hours,
then its contraceptive effect is not reduced. The woman should insert the ring into the vagina as quickly as possible, but no later than after 3 hours.
If the NuvaRing remained (or is expected to remain) outside the vagina for more than 3 hours in the first or second week of use,
then the contraceptive effect may be reduced. A woman should insert the ring into her vagina as soon as possible. Over the next 7 days, you must use a barrier method of contraception, such as a condom. The longer the NuvaRing ring was outside the vagina, and the closer this period is to the break in using the ring, the higher the likelihood of pregnancy.
If the ring remained (or is expected to remain) outside the vagina for more than 3 hours in the third week of use,
the contraceptive effect may be reduced. The woman should throw away this ring and choose one of two options:
- 1. Immediately install a new ring.
Note:
insertion of the new ring will be the start of the next 3-week period. Moreover, after the previous cycle, a woman may not have bleeding due to the cessation of the drug’s effect. However, spotting or bleeding in the middle of the cycle is possible.
2. Wait for bleeding associated with the cessation of the drug’s effect, and insert a new ring no later than 7 days (7×24 hours) after the previous ring is removed or falls out.
Note:
This option should only be selected if the ring has been in continuous use for the previous 7 days.
What to do if you exceed the duration of use of the ring
If NuvaRing has been used for a maximum of 4 weeks,
contraceptive effectiveness is still sufficient.
A woman can take a week's break from using the ring and then insert a new ring. If NuvaRing remained in the vagina for more than 4 weeks,
the contraceptive effect may be reduced, so pregnancy must be ruled out before inserting a new ring.
If a woman does not adhere to the recommended regimen of use, and after a week's break in using the ring, withdrawal bleeding does not occur, then pregnancy should be excluded before introducing a new ring.
How to postpone the start of menstruation or delay the onset of menstruation
In order to delay
the beginning of menstruation, the woman must insert a new ring without taking a break from its use. The next ring can be used for another 3 weeks. This may cause bleeding or spotting. The regular regimen of using NuvaRing is resumed after the usual 1-week break.
To transfer
the beginning of menstruation on another day of the week, the woman should be advised to make the upcoming break from using the ring shorter - for as many days as she needs. The shorter the interval between ring use, the higher the likelihood that there will be no bleeding after ring removal, and no bleeding or spotting will occur when the next ring is used.
NuvaRing®
If any of the following conditions/diseases or risk factors are present, a thorough assessment of the benefit-risk ratio of using the drug NuvaRing® should be carried out and discussed with the woman before starting to use the drug. In case of exacerbation of diseases, deterioration of the condition or the appearance of the first symptoms of conditions/diseases or risk factors, the woman should immediately consult a doctor to decide whether to discontinue or the possibility of further use of the drug.
Risk of developing VTE and ATE
The use of any combined hormonal contraceptives (CHCs) is associated with an increased risk of developing venous and arterial thrombosis and thromboembolism (such as DVT and PE, myocardial infarction, cerebrovascular disorders). These diseases are rare. The use of drugs containing levonorgestrel, norgestimate or norethisterone as a progestogen component has the lowest risk of developing VTE.
The use of other medications, such as NuvaRing®, can double the risk of developing this complication. An increased risk is present after initial use of CHCs or resumption of use after a break of 4 weeks or more. The choice in favor of a CHC with a higher risk of developing VTE can only be made after consultation with the woman to ensure that she fully understands the risk of VTE associated with the use of NuvaRing®; the effect of the drug on her existing risk factors and that the risk of developing VTE is greatest in the first year of using the drug.
VTE can be life-threatening or lead to death (in 1-2% of cases).
Thrombosis of other blood vessels, for example, hepatic, mesenteric, renal, cerebral veins and arteries or retinal vessels, has occurred extremely rarely with the use of CGCs.
Symptoms of deep vein thrombosis (DVT):
unilateral swelling of the lower limb or along the vein, pain or discomfort only in an upright position or when walking, local increase in temperature, redness or discoloration of the skin in the affected lower limb.
Symptoms of pulmonary embolism (PE)
: difficulty or rapid breathing; sudden cough, including with hemoptysis; sharp pain in the chest, which may intensify with deep inspiration; sense of anxiety; severe dizziness; fast or irregular heartbeat. Some of these symptoms (eg, shortness of breath, cough) are nonspecific and may be misinterpreted as signs of other more common and less severe conditions (eg, respiratory tract infection).
ATE can lead to stroke, vascular occlusion, or myocardial infarction.
Symptoms of a stroke:
sudden weakness or loss of sensation in the face, limbs, especially on one side of the body, sudden confusion, severe or prolonged headache for no apparent reason, unilateral or bilateral loss of vision; problems with speech and understanding; sudden disturbance in gait, dizziness, loss of balance or coordination; sudden loss of consciousness or fainting with or without a seizure.
Other signs of vascular occlusion
: sudden pain, swelling and slight cyanosis of the extremities, “acute” abdomen.
Symptoms of myocardial infarction:
pain, discomfort, pressure, heaviness, a feeling of compression or fullness in the chest or behind the sternum, radiating to the back, jaw, upper limb, epigastric region; cold sweat, nausea, vomiting or dizziness, severe weakness, anxiety or shortness of breath; fast or irregular heartbeat.
ATE can be life-threatening and lead to death.
In women with a combination of several risk factors or high severity of one of them, the possibility of their mutual reinforcement should be considered. In such cases, the degree of increase in risk may be higher than with a simple summation of factors. In this case, the use of NovaRing® is contraindicated.
The risk of developing thrombosis (venous and/or arterial) and thromboembolism or cerebrovascular disorders increases:
- with age;
- in women who smoke (with an increase in the number of cigarettes or an increase in age, the risk increases, especially over the age of 35);
- if there is a family history (for example, venous or arterial thromboembolism in close relatives or parents under the age of 50 years). In the case of a hereditary or acquired predisposition, the woman should be examined by an appropriate specialist to decide on the possibility of using CHC;
— for obesity (UTI more than 30 kg/m2);
- with dislipoproteinemia;
- for arterial hypertension;
- for migraine;
- for diseases of the heart valves;
- with atrial fibrillation;
- in case of prolonged immobilization, major surgery, any operation on the lower extremities or major trauma. In these cases, the use of CHCs should be discontinued (in the case of planned surgery, at least four weeks before it) and not resumed for two weeks after the end of immobilization. Temporary immobilization (eg, air travel lasting more than 4 hours) may also be a risk factor for the development of VTE, especially in the presence of other risk factors.
The possible role of varicose veins and superficial thrombophlebitis in the development of VTE remains controversial.
The increased risk of thromboembolism in the postpartum period should be taken into account.
Peripheral circulatory disorders may also occur in diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis) and sickle cell anemia.
An increase in the frequency or severity of migraine (which may also precede cerebrovascular events) during the use of CHCs is grounds for immediate discontinuation of these drugs.
Biochemical indicators indicating a hereditary or acquired predisposition to the development of venous or arterial thrombosis include: resistance to activated protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
The risk of thrombosis and thromboembolism during pregnancy and the postpartum period is higher than when taking low-dose CHCs (containing less than 0.05 mg ethinyl estradiol).
If VTE or ATE is suspected or confirmed, use of the drug should be stopped immediately. In this case, it is necessary to use effective contraception, since anticoagulants (coumarins) have a teratogenic effect.
Risk of developing tumors
The most important risk factor for developing cervical cancer is infection with the human papillomavirus (HPV). Epidemiological studies have shown that long-term use of COCs leads to an additional increase in this risk, but it is unclear how much of this is due to other factors, such as increased frequency of cervical screening and sexual behavior, including the number of sexual partners and less frequent use of barrier contraceptives. and their cause-and-effect relationship. Epidemiological data regarding the incidence of cervical cancer in women using the drug NuvaRing®
There are no data from epidemiological studies regarding the risk of developing cervical cancer in women using the drug NuvaRing®.
A meta-analysis of the results of 54 epidemiological studies found a small increase (1.24) in the relative risk of developing breast cancer in women taking COCs. The risk gradually decreases over 10 years after stopping the drugs. Breast cancer rarely develops in women under 40 years of age, so the additional incidence of breast cancer in women who take or have taken COCs is small compared to the overall risk of developing breast cancer. Women who use COCs are diagnosed with earlier clinical stages of breast cancer than women who have never used COCs. The observed increased risk may be due to earlier diagnosis of breast cancer in women taking COCs, the biological effects of COCs, or a combination of both.
In rare cases, cases of development of benign, and even more rarely, malignant liver tumors have been observed in women taking COCs. In some cases, these tumors led to the development of life-threatening bleeding into the abdominal cavity. The doctor should consider the possibility of a liver tumor in the differential diagnosis of diseases in a woman taking NuvaRing® if symptoms include acute pain in the upper abdomen, liver enlargement, or signs of intra-abdominal bleeding.
Hypersensitivity reactions
Hypersensitivity reactions, such as angioedema and anaphylaxis, have been observed during use of the drug NovaRing®. If you suspect angioedema and/or anaphylaxis, you should stop using the drug NuvaRing® and carry out appropriate treatment.
Hepatitis C
In clinical trials of the drug combination for the treatment of hepatitis C virus ombitasvir/paritaprevir/ritonavir with or without dasabuvir, increases in ALT levels greater than 5 times the upper limit of normal were observed significantly more often in women using drugs containing ethinyl estradiol, such as COOK. The use of NovaRing® should be discontinued before starting therapy with the combination of ombitasvir/paritaprevir/ritonavir with or without dasabuvir (see section “Contraindications” and “Interaction with other drugs”). The use of NuvaRing® can be resumed approximately 2 weeks after completion of treatment with the combination of these drugs.
Other states
- In women with hypertriglyceridemia (or a family history of this condition), the risk of developing pancreatitis may increase while using CHCs.
- Although slight increases in blood pressure (BP) have been described in many women using COCs, clinically significant increases in BP have been reported rarely. However, if a persistent clinically significant increase in blood pressure develops while using the drug NuvaRing®, the use of the drug should be stopped and treatment of arterial hypertension should be started. If normal blood pressure values are achieved with the help of antihypertensive therapy, use of the drug NuvaRing® can be continued.
- The following conditions have been reported to develop or worsen during pregnancy and when taking CHCs, but their relationship with the use of CHCs has not been proven: cholestatic jaundice and/or pruritus associated with cholestasis; formation of gallstones; porphyria; systemic lupus erythematosus; hemolytic-uremic syndrome; chorea; herpes during pregnancy; hearing loss associated with otosclerosis. Cases of Crohn's disease and ulcerative colitis have also been described with the use of CHCs.
— In women with hereditary forms of angioedema, exogenous estrogens may cause or worsen symptoms of angioedema.
— Acute or chronic liver diseases may require discontinuation of the drug NuvaRing® until liver function tests return to normal.
— Recurrence of cholestatic jaundice and/or itching caused by cholestasis, which first developed during pregnancy or previous use of sex hormones, requires discontinuation of the drug NuvaRing®.
- Although estrogens and progestogens can affect insulin resistance and glucose tolerance, in patients with diabetes mellitus using low-dose CHCs, as a rule, no dose adjustment of hypoglycemic drugs is required. However, patients with diabetes mellitus should be carefully monitored while using NuvaRing®.
- Chloasma can sometimes develop, especially in women with a history of chloasma during pregnancy. Women with a tendency to chloasma should avoid prolonged exposure to the sun and ultraviolet irradiation while using NuvaRing®.
— Conditions of a woman in which she will not be able to insert the ring correctly or in which the ring may fall out: cervical prolapse, bladder hernia and/or rectal hernia, severe chronic constipation.
— In very rare cases, women have unintentionally inserted the NuvaRing® vaginal ring into the urethra and possibly into the bladder. When symptoms of cystitis appear, it is necessary to consider the possibility of incorrect insertion of the ring.
— Cases of vaginitis have been described during the use of the drug NuvaRing®. There are no clinical data regarding the effect of vaginitis therapy on the effectiveness of the use of the drug NovaRing®, as well as the effect of the use of the drug NovaRing® on the effectiveness of therapy for vaginitis.
— Very rare cases of a ring sticking to the vaginal mucosa have been described, requiring its removal by a medical professional. In some cases where tissue had grown around the ring, removal was accomplished by cutting the ring without cutting the vaginal tissue.
Medical examination/consultation
Before prescribing the drug NuvaRing® or resuming its use, you should carefully review the woman’s medical history (including family history) and conduct a gynecological examination to exclude pregnancy. It is necessary to measure blood pressure, conduct an examination of the mammary glands, pelvic organs, including a cytological examination of cervical smears and some laboratory tests, to exclude contraindications and reduce the risk of possible side effects of the drug. The frequency and nature of medical examinations depend on the individual characteristics of each patient. but medical examinations are carried out at least once every 6 months. A woman should read the instructions for use and follow all recommendations. The woman should be informed that NuvaRing® does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency
The effectiveness of the drug NovaRing® may decrease if the regimen is not followed (see the subsection “Deviations from the recommended regimen” of the section “Dosage and Administration”) or concomitant therapy is carried out that reduces the concentration of etonogestrel in the blood plasma (see section “Interaction with other drugs” ).
Changes in the nature of menstruation
During use of the drug NovaRing®, acyclic bleeding may occur (“spotting” spotting or sudden bleeding). If such bleeding is observed after regular cycles with the correct use of the drug NuvaRing®, you should contact your gynecologist to conduct the necessary diagnostic studies, including to exclude organic pathology or pregnancy. A diagnostic curettage may be required.
Some women do not bleed after the ring is removed. If the drug NuvaRing® was used according to the instructions, it is unlikely that the woman is pregnant. If the recommendations of the instructions are not followed and there is no bleeding after removing the ring, as well as if there is no bleeding for two cycles in a row, pregnancy must be excluded.
Effects of ethinyl estradiol and etonogestrel on a sexual partner
The possible pharmacological effects and extent of exposure of ethinyl estradiol and etonogestrel to male sexual partners (due to absorption through penile tissue) have not been studied.
Ring damage
In rare cases, when using the drug NuvaRing®, ring rupture was observed. The core of the drug NuvaRing® is solid, so its contents remain intact, and the release of hormones does not change significantly. Vaginal injury associated with ring rupture has been reported. If the ring ruptures, it usually falls out of the vagina (see the recommendations in the subsection “What to do if the ring has been temporarily removed from the vagina” in the “Dosage and Administration” section). If the ring ruptures, a new ring must be inserted.
Ring falling out
Sometimes the NuvaRing® vaginal ring may fall out of the vagina, for example, if it is inserted incorrectly, when a tampon is removed, during sexual intercourse, or due to severe or chronic constipation. In this regard, it is advisable for a woman to regularly check the presence of the NuvaRing® vaginal ring in the vagina (for example, before and after sexual intercourse). If the NuvaRing® vaginal ring falls out of the vagina, you must follow the recommendations of the subsection “What to do if the ring has been temporarily removed from the vagina” in the “Method of administration and dosage” section.
NOVARING vaginal ring 15+120 mcg/24 h No. 1
special instructions
If any of the diseases, conditions or risk factors listed below are present, the benefits of using the drug NuvaRing and the possible risks for each individual woman should be assessed before she starts using the drug NuvaRing.
In case of exacerbation of diseases, deterioration of the condition, or the first occurrence of any of the conditions listed below, a woman should consult a doctor to decide on the possibility of further use of the drug NuvaRing. Circulatory disorders
The use of hormonal contraceptives may be associated with the development of venous thrombosis (deep vein thrombosis and pulmonary embolism) and arterial thrombosis, as well as associated complications, sometimes fatal.
The use of any COC increases the risk of developing venous thromboembolism (VTE) compared to the risk of VTE in patients not using COCs. The greatest risk of developing VTE is observed in the first year of COC use. Data from a large prospective cohort study of the safety of various COCs suggest that the greatest increase in risk, compared with the risk in women not using COCs, is observed in the first 6 months after starting COC use or resuming their use after a break (4 weeks or more). . In nonpregnant women not using oral contraceptives, the risk of developing VTE is 1 to 5 per 10,000 woman-years (WY). In women using oral contraceptives, the risk of developing VTE ranges from 3 to 9 cases per 10,000 women. The increase in risk occurs to a lesser extent than in pregnancy, where the risk is 5-20 cases per 10,000 YL (pregnancy data are based on the actual duration of pregnancy in standard studies, based on the assumption that pregnancy lasts 9 months, the risk is from 7 to 27 cases per 10,000 YL). In postpartum women, the risk of developing VTE ranges from 40 to 65 cases per 10,000 women. VTE is fatal in 1-2% of cases.
According to research results, the increased risk of VTE in women using NuvaRing is similar to that in women using COCs (adjusted risk ratio, see table below). A large prospective observational study, TASC (Transatlantic Active Study of the Cardiovascular Safety of NuvaRing), assessed the risk of VTE in women who started using NuvaRing or COCs, switched to NuvaRing or COCs from other contraceptives, or resumed using NuvaRing. or COCs, in a population of typical users. The women were followed for 24-48 months. The results showed a similar level of risk of developing VTE in women using the drug NuvaRing (incidence of 8.3 cases per 10,000 YL) and in women using COCs (incidence of 9.2 cases per 10,000 YL). For women using COCs other than those containing desogestrel, gestodene and drospirenone, the incidence of VTE was 8.5 cases per 10,000 women.
A retrospective cohort study initiated by the FDA (US Food and Drug Administration) showed that the incidence of VTE in women who started using the drug NuvaRing was 11.4 cases per 10,000 YL, while in women who started using COCs containing levonorgestrel, the incidence of VTE is 9.2 cases per 10,000 VL.
Assessment of the risk (risk ratio) of developing VTE in women using the drug NuvaRing, compared with the risk of developing VTE in women using COCs
Epidemiological study, population:
- TASC (Dinger, 2012) Women who started using the drug (including again after a break) and switched from other contraceptives.
- FDA-initiated study (Sydney, 2011) Women using combined hormonal contraceptives (CHCs) for the first time during the study period.
Comparator drug(s):
- All available COCs during the study1. RR2: 0.8 (0.5-1.5) Available COCs, except those containing desogestrel, gestodene, drospirenone.
- COCs available during the study period3.
Risk ratio (RR) (95% CI):
- RR2: 0.8 (0.5-1.5), RR2: 0.9 (0.4-2.0).
- RR4: 1.09 (0.55-2.16), RR4: 0.96 (0.47-1.95).
1 - Including low-dose COCs containing the following progestins: chlormadinone acetate, cyproterone acetate, desogestrel, dienogest, drospirenone, ethynodiol diacetate, gestodene, levonorgestrel, norethindrone, norgestimate or norgestrel.
2 - Taking into account age, BMI, duration of use, history of VTE.
3 - Including low-dose COCs containing the following progestins: norgestimate, norethindrone or levonorgestrel.
4 - Taking into account age, place and year of inclusion in the study.
There are extremely rare cases of thrombosis of other blood vessels (for example, arteries and veins of the liver, mesenteric vessels, kidneys, brain and retina) with the use of COCs. It is unknown whether these cases are related to the use of COCs.
Possible symptoms of venous or arterial thrombosis may be unilateral swelling and/or pain in the lower extremity, a local increase in temperature in the lower extremity, hyperemia or discoloration of the skin on the lower extremity, sudden severe chest pain, possibly radiating to the left arm, an attack of shortness of breath, coughing , any unusual, severe, prolonged headaches, sudden partial or complete loss of vision, double vision, slurred speech or aphasia, dizziness, collapse with or without a focal epileptic seizure, sudden onset of weakness or severe numbness of one side or any part of the body body, movement disorders, acute abdomen.
Risk factors for the development of venous thrombosis and embolism:
- age,
- presence of diseases in the family history (venous thrombosis and embolism in brothers/sisters at any age or in parents at a young age). If a hereditary predisposition is suspected, before starting any hormonal contraceptives, the woman should be referred to a specialist for consultation,
- prolonged immobilization, major surgery, any surgery on the lower extremities or serious trauma. In such situations, it is recommended to stop using the drug (in case of planned surgery, at least 4 weeks in advance) with subsequent resumption of use no earlier than 2 weeks after complete restoration of motor activity,
- obesity (body mass index more than 30 kg/m2),
- possibly thrombophlebitis of the superficial veins with varicose veins.
There is no consensus on the possible role of these conditions in the etiology of venous thrombosis.
Risk factors for the development of complications of arterial thromboembolism:
- age,
- smoking (with heavy smoking and with age, the risk increases even more significantly, especially in women over 35 years old),
- dyslipoproteinemia,
- obesity (body mass index more than 30 kg/m2),
- increased blood pressure,
- migraine,
- heart valve disease,
- atrial fibrillation,
- presence of diseases in the family history (arterial thrombosis in brothers/sisters at any age or in parents at a relatively early age). If a hereditary predisposition is suspected, the woman should be referred to a specialist for consultation before starting any hormonal contraceptives. Biochemical factors that may indicate hereditary or acquired predisposition to venous or arterial thrombosis include activated protein C resistance, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant).
Other conditions that can cause unwanted circulatory problems include diabetes mellitus, systemic lupus erythematosus, hemolytic uremic syndrome and chronic inflammatory bowel disease (such as Crohn's disease or ulcerative colitis), as well as sickle cell anemia.
It is necessary to take into account the increased risk of thromboembolism in the postpartum period. An increase in the frequency or severity of migraine (which may be a prodromal symptom of cerebrovascular accidents) while using hormonal contraceptives may be a reason to immediately discontinue use of hormonal contraceptives.
Women using CHCs should be advised to consult a doctor if possible symptoms of thrombosis occur. If thrombosis is suspected or confirmed, CHC use should be discontinued. In this case, it is necessary to use effective contraception, since anticoagulants (coumarins) have a teratogenic effect.
Risk of developing tumors
The most important risk factor for developing cervical cancer is infection with the human papillomavirus (HPV). Epidemiological studies have shown that long-term use of COCs further increases this risk, but it is unclear how much of this is due to other factors, such as increased frequency of cervical smears and differences in sexual behavior, including the use of barrier contraceptives. It remains unclear how this effect is related to the use of the drug NuvaRing.
A meta-analysis of 54 epidemiological studies found a small increase (1.24) in the relative risk of breast cancer in women taking combined hormonal oral contraceptives. The risk gradually decreases over 10 years after stopping the drugs. Breast cancer rarely develops in women under 40 years of age, so the additional incidence of breast cancer in women who take or have taken COCs is small compared to the overall risk of developing breast cancer. Breast cancer diagnosed in women who use COCs is clinically less severe than cancer diagnosed in women who have never used COCs. The increased risk of breast cancer may be due to the earlier diagnosis of breast cancer in women taking COCs, the biological effects of COCs, or a combination of both.
In rare cases, cases of development of benign, and even more rarely, malignant liver tumors have been observed in women taking COCs. In some cases, these tumors led to the development of life-threatening bleeding into the abdominal cavity. A physician should consider the possibility of a liver tumor in the differential diagnosis of diseases in a woman taking NuvaRing if symptoms include acute pain in the upper abdomen, liver enlargement, or signs of intra-abdominal bleeding.
Other states
- Women with hypertriglyceridemia or a corresponding family history have an increased risk of developing pancreatitis when taking hormonal contraceptives.
- Many women taking hormonal contraceptives experience a slight increase in blood pressure, but clinically significant increases in blood pressure are rare. A direct connection between the use of hormonal contraceptives and the development of arterial hypertension has not been established. If, when using the drug NuvaRing, there is a constant increase in blood pressure, you should contact your doctor to decide whether it is necessary to remove the vaginal ring and prescribe antihypertensive therapy. With adequate control of blood pressure using antihypertensive drugs, it is possible to resume use of the drug NuvaRing.
- During pregnancy and during the use of combined oral contraceptives, the development or worsening of the following conditions was noted, although their relationship with the use of contraceptives has not been definitively established: jaundice and/or itching caused by cholestasis, formation of gallstones, porphyria, systemic lupus erythematosus, hemolytic -uremic syndrome, Sydenham's chorea (minor chorea), herpes of pregnancy, hearing loss due to otosclerosis, (hereditary) angioedema.
- Acute or chronic liver diseases may serve as a reason to discontinue the drug NuvaRing until liver function indicators normalize. Recurrence of cholestatic jaundice, previously observed during pregnancy or during the use of sex hormones, requires discontinuation of the drug NuvaRing.
- Although estrogens and progestogens may influence peripheral insulin resistance and tissue glucose tolerance, there is no evidence to support the need to change hypoglycemic therapy during the use of hormonal contraceptives. However, women with diabetes should be under constant medical supervision when using NuvaRing, especially in the first months of contraception.
- There is evidence of a worsening of Crohn's disease and ulcerative colitis with the use of hormonal contraceptives.
- In rare cases, pigmentation of the facial skin (chloasma) may occur, especially if it occurred earlier during pregnancy. Women predisposed to the development of chloasma should avoid exposure to sunlight and ultraviolet radiation while using NuvaRing.
- The following conditions may prevent the ring from being inserted correctly or may cause it to fall out: cervical prolapse, bladder and/or rectal hernia, severe chronic constipation.
- In very rare cases, women have unintentionally inserted the NuvaRing vaginal ring into the urethra and possibly into the bladder. When symptoms of cystitis appear, it is necessary to consider the possibility of incorrect insertion of the ring.
- Cases of vaginitis have been described during use of the drug NuvaRing. There is no evidence that the treatment of vaginitis affects the effectiveness of the use of the drug NuvaRing, as well as evidence that the use of the drug NuvaRing influences the effectiveness of the treatment of vaginitis.
- Very rare cases of difficult ring removal have been described that required removal by a medical professional.
Medical examination/consultation
Before prescribing the drug NuvaRing or resuming its use, you should carefully review the woman’s medical history (including family history) and conduct a gynecological examination to exclude pregnancy. It is necessary to measure blood pressure, conduct an examination of the mammary glands, pelvic organs, including a cytological examination of cervical smears and some laboratory tests, to exclude contraindications and reduce the risk of possible side effects of the drug. The frequency and nature of medical examinations depend on the individual characteristics of each patient, but medical examinations are carried out at least once every 6 months. A woman should read the instructions for use and follow all recommendations. The woman should be informed that NuvaRing does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Reduced efficiency
The effectiveness of the drug NuvaRing may decrease if the regimen is not followed or concomitant therapy is carried out.
Reduced cycle control
While using the drug NuvaRing, acyclic bleeding may occur (spotting or sudden bleeding). If such bleeding is observed after regular cycles with the correct use of the drug NuvaRing, you should contact your gynecologist to conduct the necessary diagnostic tests, including to exclude organic pathology or pregnancy. A diagnostic curettage may be required.
Some women do not bleed after the ring is removed. If the drug NuvaRing was used according to the instructions, it is unlikely that the woman is pregnant. If the recommendations of the instructions are not followed and there is no bleeding after removing the ring, as well as if there is no bleeding for two cycles in a row, pregnancy must be excluded.
Effects of ethinyl estradiol and etonogestrel on a sexual partner
The possible pharmacological effects and extent of exposure of ethinyl estradiol and etonogestrel to male sexual partners (due to absorption through penile tissue) have not been studied.
Ring damage
In rare cases, when using the drug NuvaRing, ring rupture was observed. The core of the drug NuvaRing is solid, so its contents remain intact, and the release of hormones does not change significantly. If the ring ruptures, it usually falls out of the vagina (see recommendations in the subsection What to do if the ring has been temporarily removed from the vagina in the Dosage and Administration section). If the ring ruptures, a new ring must be inserted.
Ring falling out
Sometimes the NuvaRing vaginal ring may fall out of the vagina, for example, if it is inserted incorrectly, when a tampon is removed, during sexual intercourse, or due to severe or chronic constipation. In this regard, it is advisable for a woman to regularly check the presence of the NuvaRing vaginal ring in the vagina. If the NuvaRing vaginal ring falls out of the vagina, you must follow the recommendations of the subsection What to do if the ring has been temporarily removed from the vagina in the Method of administration and dosage section.