In the treatment of psychiatric diseases, it is often impossible to do without pharmacotherapy, and in some cases, drugs - antipsychotics - are the main way to cope with complications.
The line of such antipsychotics has recently been supplemented with a new generation of atypical antipsychotics. These drugs suppress the negative symptoms of mental disorders and show positive results on the patient. In addition, they do not cause at all or almost no extrapyramidal (motor function disorders), hyperprolactinemia (increased levels of the hormone prolactin in the blood), that is, unwanted side effects.
A prominent representative of modern atypical antipsychotics is a drug called Seroquel, which contains the active component quetiapine. The developers recommended this remedy for the treatment of schizophrenia. In the Russian Federation, its use has been approved for the treatment of psychosis and other mental disorders since 1999, and it is also widely used for the same purposes in another seventy countries around the world. The most detailed information about Seroquel and the experience of its use is discussed in the scientific work of psychiatrist (psychotherapist and child and adolescent psychiatrist) Victoria Valerievna Krasavina, on whose material we will rely in this article.
Structure and receptor activity of the drug
Chemically, Seroquel (quetiapine) is a derivative of dibenzothiazepine. This atypical antipsychotic interacts with many neuroreceptors, so its spectrum of therapeutic effects is very wide. The drug blocks H1 receptors according to the following scheme: H1 >α>α1>5-HT 2a>α2>D2>5-HT1a>D1>M1. Due to this binding of quetiapine and blockade of α1 and α2 receptors, a nonspecific sedative effect occurs, and anxious affect and arousal are eliminated.
The absence of side effects (hyperprolactinemia and minor extrapyramidal effects) is explained by the weak effect on 5-HT2a and D2 receptors.
Seroquel in general psychiatry
At the moment, there is a significant amount of data on the practical use of Quetiapine, accumulated by specialists over the past five years. As already mentioned, this atypical antipsychotic has been introduced as a treatment for schizophrenia. Its long-term use leads to an increase in the general activity of patients, a decrease in autistic manifestations, and an improvement in social adaptation. In this case, hyperprolactinemia and extrapyramidal disorders are not observed.
Seroquel has a positive effect on cognitive function in people with schizophrenia:
• after 3 months of use, attention improves significantly;
• after six months to a year, the quality of executive function and verbal productivity improves.
It should be clarified that this effect is achieved at an average dose of 517.9 mg/day of the drug per day. Long-term use of the drug is not dangerous, as it is well tolerated. Among other things, it reduces suicidal risks.
Experts who have used the atypical antipsychotic in practice indicate its positive results for depressive symptoms. It has a stronger antipsychotic effect than haloperidol, surpassing it and other drugs in antidepressant, anti-anxiety and anti-manic properties.
Such abilities of Quetiapine made it possible to use it and prove its effectiveness in the treatment of:
• anxiety states;
• affective disorders;
• behavioral disorders;
• bipolar disorders, etc.
The drug has also been successfully used to relieve hostility and aggression, in acute mania, and to reduce psychotic symptoms.
The following positive points can be mentioned:
1. Thanks to Seroquel, monotherapy has become possible, that is, treatment of mental disorders with excellent results without side effects is available using only one, maximum two drugs.
2. If we talk about obsessive-compulsive disorders, then Seroquel has also been tried to treat patients with strong resistance to antipsychotics such as selective serotonin reuptake inhibitors. However, a small dose of the drug in monotherapy was ineffective. But, in cases of combination of Quetiapine with SSRIs, patients experienced significant improvement in their condition.
3. They tried to use an atypical antipsychotic in the treatment of post-traumatic stress disorder. 18 war veterans with this problem took Seroquel for 6 weeks, 25-300 mg per day. By the end of therapy, the patients' condition improved significantly; no deterioration in neurological parameters or negative changes in internal organs were recorded. As a result, it was decided to expand research on the use of the drug in the treatment of this disorder.
4. There is evidence of success with this antipsychotic in elderly patients with psychotic symptoms, Parkinson's disease and Alzheimer's disease. Elderly patients had improved quality of life, motor functions, decreased behavioral disorders, and improved sleep. The attending physicians clarify that to achieve a positive effect, you should start with small doses of the drug and not increase them much.
5. There are isolated cases of effective use of Quetiapine for a patient with a mental illness aggravated by drug addiction and alcoholism.
Seroquel
Seroquel (quetiapine) is a new-generation antipsychotic drug for the treatment of schizophrenia and other psychoses. In terms of their therapeutic effects, antipsychotics are similar to each other: the main differences between drugs in this group are related to the spectrum and severity of side effects. Traditional antipsychotics cause a whole range of undesirable side reactions, the greatest clinical significance of which are extrapyramidal symptoms, which, in turn, increase the risk of developing depressive conditions, reduce compliance (patient adherence to treatment), and contribute to the formation of suicidal behavior. Other adverse reactions characteristic of standard antipsychotic therapy include sexual dysfunction, cardiovascular disorders, and weight gain. This, as well as the presence of patients resistant to the effects of traditional antipsychotics, necessitated the development of new antipsychotic drugs. An example of such a drug is Seroquel, which has proven its advantages over previous generations of antipsychotics in preclinical and clinical studies. One of its most obvious advantages is the fact that it is only minimally capable of causing the development of dystonia, which determines a low risk of extrapyramidal symptoms. The drug has proven its effectiveness in eliminating both positive (hallucinations, delusions) and negative (apathy, decreased volitional qualities) symptoms of schizophrenia. In terms of effectiveness, Seroquel is not inferior to traditional antipsychotics such as haloperidol and chlorpromazine, while having better tolerability. The key advantages of Seroquel are the absence of the risk of developing extrapyramidal symptoms and hyperprolactinemia.
The incidence of other adverse reactions with the drug is no higher than with previous generations of antipsychotics. The active component of Seroquel, quetiapine, is well absorbed from the digestive tract. The presence of food content in the latter has virtually no effect on bioavailability, which makes it possible to take Seroquel regardless of meals. The drug is not used in pediatric practice. In clinical studies, some side effects occurred more frequently in children and adolescents than in adult patients. The frequency of use of Seroquel is twice a day. The effective dose in elderly patients is usually less than in younger patients. For patients suffering from kidney disease, no dosage adjustment is required. Patients suffering from liver diseases take the drug under regular supervision. At the initial stage of pharmacotherapy, drowsiness usually occurs, which disappears with further use of the drug, and an increase in body weight is also noted. When combining Seroquel with other drugs that affect the central nervous system, extreme caution should be exercised. While taking the drug, you should refrain from drinking alcohol. Patients with suicidal behavior should take the drug under constant medical supervision until remission occurs. Abrupt interruption of the medication course is fraught with an increased risk of suicidal events. If severe drowsiness occurs during the first two weeks of treatment, you should be regularly monitored by a doctor. During treatment, it is recommended to refrain from activities associated with increased attention and concentration (driving a car, working with potentially dangerous mechanisms).
Child and adolescent therapy
At this time, few descriptions of the practical use of Seroquel in child and adolescent psychiatry can be found in the specialized literature. But they describe in sufficient detail the specifics of using the drug for this category of patients.
Due to good treatment results and mild side effects, experts suggest more active use of the drug in child and adolescent psychiatry. Already at 3-6 weeks, minor patients with schizophrenia taking Quetiapine in doses from 100 to 800 mg per day demonstrated a decrease in the symptoms of this disease, “extinguishing” hyperactivity and aggression.
Some patients experienced dry mouth, mild tremor, dizziness and hypotension as side effects. However, there were only a few such patients, and such manifestations were very weak. The usual strong increase in body weight after taking atypical antipsychotics was not observed, as well as disturbances in the endocrine system and problems with motor functions.
Also safe for children and adolescents is treatment with Quetiapine for bipolar and schizoactive disorders, antisocial behavior, psychopathy, Gilles de la Tourette syndrome and generalized tics, and other mental disorders. At the same time, experts warn about the danger of an overdose of the drug, which can cause tachycardia, hypotension, and agitation.
Side effect
As already mentioned, unlike other atypical antipsychotics, Seroquel does not cause negative side effects such as extrapyramidal disorders. The latter property allows the free use of this remedy, both among minors and elderly patients, who are more susceptible to such disorders than other categories of patients.
Data on the effect of the drug on metabolism vary, but most experts say that there is still weight gain, but it is insignificant compared to the effect of other atypical antipsychotics.
As for the side effect of hyperprolactinemia, it is quite serious. An increase in the level of prolactin in the blood, caused by the blockade of certain receptors, leads to the appearance of osteoporosis, galactorrhea (spontaneous leakage of milk from the breast), amenorrhea (lack of menstruation), sexual dysfunction, gynecomastia (breast enlargement in men). Seroquel does not increase prolactin levels and even helps correct sexual dysfunction caused by another drug.
Studies have been conducted on the effect of Quetiapine on the functionality of the cardiovascular system. It turned out that the drug is not cardiotoxin and does not affect intracardiac conduction. It also does not have any special effect on the electrophysiological activity of the brain.
From all of the above, we can conclude that, according to the experience of using Seroquel in world medical practice, the drug has an excellent therapeutic effect for various mental disorders, without serious contraindications or side effects.
Psychiatry Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina No. 08 2003
The introduction of new antipsychotics into widespread practice has brought to the fore old problems of neuroleptic therapy. One of them is the dose-dependent effect (N.B. Zharkova, 2002; L. Arvanitis et al., 1997; G. Chrouinard et al., 1993), which allows expanding the clinical indications for their use and using these drugs not only for therapy acute schizophrenia, but also for the treatment of sluggish (low-progressive) forms of this disease. A wide range of doses used in the treatment of typical antipsychotics (from ultra-low, for example 0.5 mg/day trifluperazine, to “extraordinary” - more than 80 mg/day haloperidol), as well as the ability to achieve various psychopharmacological effects by changing dosages (from psychostimulant, anxiolytic, antidepressant to antipsychotic) are the main feature of this class of psychotropic drugs, distinguishing them from antidepressants, tranquilizers, nootropics and psychostimulants. It is no coincidence that in American psychiatry the main characteristic of antipsychotics is not the spectrum of their clinical action, but the so-called aminazine coefficients, the concept of which is based on the presence of a dose-dependent effect in these drugs. The possibility of using small and medium doses of antipsychotics for sluggish (low-progressive) schizophrenia has been well studied in Russian psychiatry (S.N. Mosolov et al., 1998; A.B. Smulevich, 1999). Their use for senesto-hypochondriacal, obsessive-phobic, hystero-hypochondriacal and other disorders made it possible not only after a few weeks of therapy to reduce psychopathological symptoms and increase sensitivity to other groups of psychotropic drugs, but also to immediately achieve a nonspecific effect - the occurrence of tranquilization/sedation phenomena. The new atypical antipsychotic seroquel (quetiapine), with a wide range of recommended doses (50–750 mg), widely used in psychiatric clinics, provides a good opportunity to study the dose-dependent effects of atypical antipsychotics. Many clinical studies have confirmed its high effectiveness in the treatment of psychotic conditions in schizophrenia, the ability to reduce positive and negative disorders, have a positive effect on cognitive functions, and good tolerability (Yu.A. Aleksandrovsky et al., 2000; Ph.Meats, 1999). The effective doses of quetiapine recommended in these cases are in the range of 300–750 mg/day. Meanwhile, it was noted that, along with the antipsychotic drug, it clearly exhibits a tranquilo-sedative effect; the positive results of some studies of seroquel in agitated depression, schizophrenia with symptoms of aggression/excitement confirm this (V.V. Kalinin, 2001; J. Bobes et al., 2001; J. Hellewell, J. Goldstein, 1998). At the same time, the issue of distinguishing the anxiolytic and sedative components in the spectrum of its psychopharmacological activity was not considered. Meanwhile, these two effects, one of which (anxiolytic) is assessed as therapeutic, and the other (sedative) as a side effect, reflect the discrepancy between the dichotomous concepts of therapeutic-side and desirable-undesirable. Thus, the sedative effect can be regarded as desirable in the treatment of severe psychotic states with symptoms of agitation, agitated depression and considered as a side effect during long-term maintenance neuroleptic therapy or in the treatment of low-progressive schizophrenia and borderline mental disorders. The purpose of this study was to study the effectiveness/tolerability and impact on cognitive function of the atypical antipsychotic seroquel (quetiapine) in patients with low-grade schizophrenia with a predominance of generalized anxiety. Patients with sluggish neurosis-like schizophrenia were selected for the study, whose condition was determined by generalized anxiety symptoms (GAD) within the framework of senesto-hypochondriacal disorders or anticipatory anxiety in agoraphobia. All patients were undergoing inpatient and outpatient treatment in the Department of Borderline Psychiatry of the State Scientific Center for SSP named after. V.P. Serbsky on the basis of PKB No. 12. Patients with severe somatic and neurological pathologies were excluded from the study. The age of patients was limited to 18–45 years to exclude negative effects on cognitive function due to advanced age. The simultaneous use of other psychotropic drugs (neuroleptics, antidepressants, anxiolytics, hypnotics) was excluded. If extrapyramidal symptoms occurred, anticholinergic drugs were prescribed. Research methods included clinical and psychopathological examination, as well as assessment of the dynamics of disease severity and overall effectiveness of therapy on the CGI scale, positive, negative and general pathological disorders on the PANSS scale, anxiety disorders on the HAM-A scale, and side symptoms on the UKU scale. All patients were discontinued from all psychotropic medications before the start of the study. The wash-out period depended on the half-life of the specific drug being discontinued. Patients examined before starting Seroquel therapy (background) began taking the drug at a dose of 25 mg/day at night for one week, after which a second examination was carried out. Subsequently, in the absence of a therapeutic effect, the dose of the drug was increased by 25-50 mg (over 1-2 days) until positive treatment results were achieved - the third examination (dosage regimen - 2 times a day). 2 months after this, under the condition of monotherapy with stable doses of the drug, the last (fourth) examination was carried out. The study design is presented in Table. 1
.
Research results
The study included 20 patients who had suffered from indolent neurosis-like schizophrenia for 3–10 years (average 5.6 years);
their average age was 34.3±9.1 years. Generalized anxiety in 13 of them was observed within the framework of the senesto-hypochondriacal state, in 7 – anxiety of anticipation in agoraphobia. 19 patients completed the study completely. One patient with a senestohypochondriacal condition refused to take seroquel at a dose of 25 mg on the 5th day of therapy due to increased anxiety, the appearance of tachycardia, and restlessness. These symptoms decreased when the drug was discontinued. The distribution of patients according to the level of doses of seroquel received by the end of the study is presented in table.
2 .
As follows from table. 2
, more than 60% of patients took Seroquel in doses of 50–75 mg/day, most often in a dose of 75 mg/day (36.8%).
Only in 21.1% of patients the drug dose reached 100 mg/day and in 10.5% – 300 mg/day. Only one patient took 25 mg/day of Seroquel. The severity of the disease on the CGI-S scale before the start of therapy in 83.3% of patients was characterized as moderate, and in 16.7% as significant, while by the end of treatment the condition of the majority of patients (83.3%) was assessed as borderline or mild. Only 16.7% of patients had “moderate severity” disease. The overall effectiveness of the treatment, assessed on the CGI-I scale, is presented in Table.
3 . At the end of the study, high rates of treatment success were noted. This was confirmed by the fact that all patients showed an improvement of varying degrees of severity.
Thus, “pronounced” and “moderate” positive effects were observed in 84.2%, and “minimal” – in 15.8% of patients. No positive dynamics during treatment or minimal deterioration was noted in any patient. As the results of the study showed, the degree of effectiveness of therapy did not correlate with the characteristics of the clinical condition of patients with low-grade schizophrenia and did not depend on the psychopathological structure of their condition ( Table 4
). Complete remission was achieved in 50% of patients with senestohypochondriacal syndrome and 42.9% with anticipatory anxiety in agoraphobia. Partial remission was observed in 33.3% of patients with senestohypochondriacal syndrome and in 42.9% with anticipatory anxiety in agoraphobia, and minimal effect was observed in 16.7 and 14.2% of cases, respectively.
Therapeutic dynamics of the severity of psychopathological symptoms was carried out using the PANSS scale ( Table 5
).
A statistically significant reduction (p=0.0001) was observed when assessing the total score of this scale (by 17.3%). The reduction was subject to both general pathological (by 21.7%) (p = 0.0001) (mainly due to a decrease in the level of anxiety, somatic concern, tension) and negative (by 20.3%) (p = 0.0008 ) symptoms. The dynamics on the scale of positive syndromes did not reach the level of statistical significance due to the absence of acute psychotic disorders in patients with sluggish schizophrenia - delusions, hallucinations, ideas of grandeur, etc. Their existing disorders, classified as positive on the PANSS scale, consisted of disturbances in thinking in the form of reasoning, slipping, and thoroughness. Detection of the tranquilizing effect of the study drug was possible due to compliance with the inclusion criteria (the predominance of generalized anxiety in the clinical condition of patients) and the use of the appropriate assessment tool (HAM-A scale). In all patients ( Table 6
) there was a reduction in anxiety symptoms (from 17.30 to 9.66 points).
A tendency towards its decrease was observed already from the first week of therapy at all, even small (25 mg), doses of the drug, but significant changes in this indicator were noted only towards the end of therapy and amounted to 27% at doses of 25–100 mg and 20% at doses of 150 –300 mg (see figure).
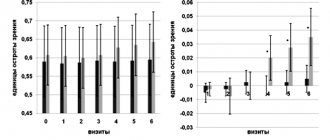
A decrease in the level of anxiety in patients with GAD as part of low-grade schizophrenia indicated a clear anxiolytic component of the drug’s action, which manifested itself already in the first week of therapy. At the same time, there was a tendency to a slight decrease in the severity of the anxiolytic effect with increasing dosages of the drug. Features of the tranquilizing component of seroquel, depending on its dose, were discovered when assessing the effect of therapy on cognitive functions. The results of the psychophysiological study are presented in table. 7
.
As can be seen from table. 7
, with the use of seroquel in the dose range of 25–100 mg, a clear optimization was observed when assessing attention functions.
When performing the “correction test” test, an improvement in the volume and productivity of attention was noted (an increase in the number of correct answers and a reduction in the proportion of erroneous answers). The positive dynamics were also different in relation to the reaction time indicator, which was manifested in a reduction in the latent period of the sensorimotor reaction of choice. The improvement in memory functions turned out to be statistically unreliable - an increase in the total number of answers and a decrease in the proportion of erroneously reproduced answers. Such a dissociation between the restoration of attention functions and the lack of a clear improvement in memory indicators is typical for tranquilizers belonging to the type of selective anxiolytics, a characteristic feature of which is the presence of an anxiolytic effect in the absence of a sedative component of their action. Thus, the tranquilizing effect of small doses of quetiapine reflected the properties of selective anxiolytics. The positive effect of Seroquel on attention functions described above is of independent significance. The ability to selectively respond to significant environmental circumstances, filter them out and not react to distracting or irrelevant factors is the leading ability of a person’s target behavior, closely related to the processes of his adaptation. Thus, restoration of attention functions when using Seroquel in doses of 25–100 mg in patients with low-grade schizophrenia can be considered as one of the fundamental cognitive processes that implement the adaptive activity of such patients. The effect on basic cognitive functions of Seroquel monotherapy in doses of 150–300 mg turned out to be different. A vectorial decrease in productivity and memory and attention, a decrease in reaction time reflected the appearance of a tranquilosedative component in the spectrum of psychotropic activity of the drug. This dose-dependent two-stage nature of the tranquilizing effect of seroquel, characterizing it in small doses as a selective anxiolytic, and in medium doses as a sedative anxiolytic, is the main feature of the spectrum of psychopharmacological activity of the drug. The number/range of side effects when using Seroquel also turned out to be dose-dependent ( Table 8
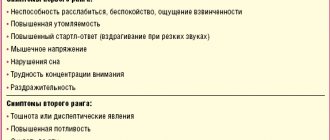
).
In table the number of side effects increases more than 2 times when the dosage of the drug increases from 25–100 to 150–300 mg (from 1.3 to 2.8 per patient). The spectrum of side effects of the drug was characterized mainly by effects affecting the mental sphere (see Table 8
). Moreover, if during therapy with small doses (25–100 mg) the adverse events were increased anxiety and worsening sleep, which reflected the activating effect of the drug, then when the dose was increased to 150–300 mg, patients more often complained of drowsiness, asthenia, increased sleep duration, which characterize its sedative property. The second place in frequency of occurrence was occupied by autonomic disorders: orthostatic disorders, dry mouth, nausea, tachycardia, which were characterized by mild severity, went away on their own and did not depend on the dose level of the drug. Less frequently, and only with therapy with small doses of the drug, so-called other side effects occurred, among which headaches predominated. Neurological (extrapyramidal) side effects were the rarest and did not depend on the dose of seroquel. They were represented by two cases of short-term small-scale tremor that did not require additional anticholinergic therapy due to self-reduction. Thus, a study of the use of seroquel in low-grade schizophrenia with a predominance of GAD within the framework of senesto-hypochondriacal states and anxiety of expectations in agoraphobia showed the effectiveness of its dosage from 25 to 300 mg. However, most often (in more than 60% of patients) positive therapeutic results were achieved with treatment at doses of 75–100 mg/day. An increase in the seroquel dose to 300 mg was required in 10.5% of cases. Positive therapeutic dynamics were achieved due to the reduction of general psychopathological and negative symptoms, as well as anxiety disorders, which indicated a clear anxiolytic effect of the drug. The anxiolytic effect was observed in the early stages of therapy (week 1) across the entire dose range of the drug. The conducted psychophysiological study revealed a dose-dependent two-stage pattern in the anxiolytic effect of seroquel. Improvement in cognitive functions (attention) when using the drug in doses of 25–100 mg reflected its properties as a selective anxiolytic, while increasing its dosage to 150–300 mg indicated the appearance, along with a tranquilizing sedative component, in the spectrum of its psychopharmacological activity. This was also evidenced by the analysis of dose-dependent side effects of the drug. During therapy with doses of 25–100 mg, activation phenomena occurred, and with 150–300 mg, moderate sedation occurred. The incidence of other types of side effects (neurological, autonomic) did not depend on the dose level of the drug and did not require drug correction (including the prescription of anticholinergic drugs). The study allows us to conclude that it is advisable to use Seroquel in patients with low-grade schizophrenia with a predominance of anxiety disorders and to optimize the method of prescribing the drug to such patients. Seroquel doses in the range of 75–100 mg in this group of patients at the initial stage of treatment are an adequate choice, reducing the time to achieve the effectiveness of therapy.