Pharmacological properties of the drug Vinorelbine 'ebeve'
Pharmacodynamics. Vinorelbine belongs to the antineoplastic agents of the vinca alkaloid group. It influences at the molecular level the dynamic balance of tubulin/microtubules and prevents tubulin polymerization. Vinorelbine acts primarily on mitotic microtubules. The effect on axonal microtubules is observed at high concentrations of the drug. The effect of tubulin helicalization under the action of vinorelbine is less pronounced than under the action of vincristine. Vinorelbine inhibits mitosis in the G2/M phases of the cell cycle and causes cell death during interphase and during mitosis. Pharmacokinetics. After intravenous administration, a three-phase decrease in the concentration of vinorelbine in the blood plasma is observed. The duration of the terminal half-life from blood plasma is 40 hours. The total clearance of vinorelbine is high (1.3 l/h• kg). Vinorelbine is excreted mainly in bile, renal excretion is insignificant (18.5%). The volume of distribution of vinorelbine exceeds 40 l/kg. Vinorelbine is moderately bound to plasma proteins (13.5%) and significantly bound to platelets (78%). Vinorelbine penetrates very well into lung tissue (the ratio of vinorelbine concentrations in lung tissue and blood plasma exceeds 300). In human urine, vinorelbine is determined predominantly in unchanged form, as well as its metabolite deacetylvinorelbine in low concentrations.
Use of the drug Vinorelbine 'ebeve'
Intended for intravenous administration only. It is strictly forbidden to administer the drug intrathecally! Before administering the infusion solution, you must make sure that the needle is in the vein. If the drug gets into the tissue surrounding the vessel, significant irritation may occur. In case of extravasation, the drug should be stopped immediately and continued into another vein. Use in adults In monotherapy, vinorelbine is usually administered in doses of 25–30 mg/m2 of body surface area weekly. In the case of combination therapy, the drug can be administered in the same doses, but at longer intervals, for example on the 1st and 5th day or the 1st and 8th day of a course lasting 3 weeks. Vinorelbine can be administered by slow IV injection (duration 5–10 min) after dilution of 20–50 ml of 0.9% sodium chloride solution or by short IV infusion (duration 20–30 min) after dilution of 125 ml 0 .9% sodium chloride solution. After completing the administration of the drug, 0.9% sodium chloride solution is always administered to rinse the vein. Dose adjustment In case of severe liver dysfunction, the dose of vinorelbine should be reduced (usually the dose is reduced by a third or more). In case of severe renal impairment, there is no need to reduce the dose, since vinorelbine is excreted primarily in bile. During treatment with vinorelbine, peripheral blood patterns should be constantly monitored. The maximum single dose of the drug is 35 mg/m2 of body surface. The maximum course dose is 60 mg. Instructions for personnel The concentrate for the preparation of solution for infusion can be diluted with 0.9% sodium chloride solution or 5% glucose solution. The amount of solution required is determined by the method of administration (slow IV injection or fast IV infusion). From a microbiological point of view, the diluted solution should be used immediately. If the solution for infusion is not used immediately after preparation, the period and conditions of its storage are controlled by the responsible person. From a microbiological point of view, the storage period for the solution should usually not exceed 24 hours at a temperature of 2–8 °C, unless it has been diluted under controlled aseptic conditions. Infusion solutions prepared by diluting Vinorelbine "Ebewe" with 0.9% sodium chloride solution or 5% glucose solution are physically and chemically stable for 28 days if stored in the refrigerator or at room temperature, protected from light place. If stored at room temperature, away from light, infusion solutions remain stable for 4 days. Only transparent, colorless or light yellow solutions can be used. When working with Vinorelbine "Ebewe", as with other cytotoxic drugs, you should be careful and be sure to use gloves, masks and protective clothing. The preparation of solutions for infusions should be carried out by trained personnel in a specially designated area. The workplace must be covered with disposable sheets of absorbent paper with a film coating on the reverse side. Pregnant women are not allowed to work with the drug. Avoid contact of vinorelbine with the eyes as this may cause severe irritation, including the formation of corneal ulcers. If this does happen, you should immediately rinse your eyes with a large amount of 0.9% sodium chloride solution (rinse for 15 minutes). Unused solutions, instruments and materials that have come into contact with vinorelbine solutions should be destroyed according to procedures determined by local health authorities.
Modern chemotherapy for solid tumors should preserve the quality of life of patients, the most important component of which is the convenience and safety of treatment. Drugs that meet these principles and expand treatment options include the oral formulation of vinorelbine (OVV).
The main area of application of vinorelbine is non-small cell lung cancer (NSCLC) and advanced breast cancer (BC). As an alternative to the intravenous dosage form of vinorelbine, VPV was created and introduced to the market in February 2001. Today, Navelbine capsules are used in more than 52 countries around the world, including Russia. The bioavailability of oral vinorelbine is 40%, a dose of ER 60 mg/m2 is equivalent to a dose of vinorelbine 25 mg/m2 when administered intravenously, a dose of ER 80 mg/m2 is equivalent to 30 mg/m2 [1] with a comparable toxicity profile. According to studies, the majority (74 %) of patients prefer taking vinorelbine orally rather than its intravenous form due to the convenience of treatment and better tolerability [2].
Lung cancer
First-line treatment for NSCLC usually uses platinum doublets containing taxanes, gemcitabine or vinorelbine. In the general population of patients with different spectrums of toxicity, the regimens are equally effective. To date, comparable effectiveness has been established for both forms of vinorelbine in combination with platinum derivatives [3, 4].
In the first line, the combination of cisplatin and SPV induces an objective effect in 27.3% of patients, disease control was 57.6%, median time to progression (TTP) was 4.8 and overall survival (OS) was 11.5 months [5 ].
If there are restrictions on the use of platinum drugs, the first-line treatment option for NSCLC in the absence of activating mutations includes the independent use of vinorelbine. In a phase II study in stage IIIb and IV NSCLC. (mainly squamous cell – 52%) in previously untreated patients in 80% of cases, equal efficacy and safety of the use of ERV (60 mg/m2) and intravenous vinorelbine was demonstrated [6]. The therapeutic effect was achieved in 52 and 49% of patients, respectively.
The use of vinorelbine capsules in elderly patients seems promising. To date, equal therapeutic efficacy has been established for the independent use of taxanes, gemcitabine and vinorelbine [7–9].
The use of SPV in the maintenance phase in the absence of progression after 4 courses of induction chemotherapy seems relevant and perhaps most interesting. To date, the feasibility of this approach has been proven for NSCLC. There is a number of data on the rationality of this treatment option. In a multicenter study, after 4 courses of chemotherapy with cisplatin and oral vinorelbine, patients continued taking one VPV (80 mg/m2) [10]. Of the 56 patients included in the study, 25 (43.9%) received maintenance (consolidating) treatment. The objective effect was 26.5%, disease stabilization – 44.9%. The median duration of the effect reached 6 months. The median TDP was 4.2, and OS was 10 months. The main side effects were grade 3–4 neutropenia. in 29.1% of patients. It would be of interest to achieve a high median TDP comparable to that achieved with pemetrexed.
These results were confirmed in a multicenter study [11], in which the combination of carboplatin (AUC-5, day 1) and IPV (60 mg/m2, days 1, 8 and 15 followed by dose escalation to 80 mg/m2) during each 56 patients with stage IIIb–IV NSCLC received a 3-week course. In the absence of progression after 4 courses, treatment was continued with vinorelbine alone (60–80 mg/m2 weekly). The median dose intensity of vinorelbine in combination was 50.1 mg/m2/week (67.3%); 36 of 52 patients (69.2%) received a dose of 80 mg/m2. In the support phase it was 56.2 mg/m2/week (70.2%). Partial effect was achieved in 17.9% of patients, stabilization – in 53.6%. The median TFS was 4.3 months with a median OS of 9.7 months.
A later publication of the results of this study provided data on the incidence of stage 3/4 neutropenia, amounting to 67.9% during the combination period and only 20% during the consolidation period, which, in addition to high efficiency, indicated the safety of maintenance treatment with vinorelbine [12] .
The rationale for conducting the maintenance phase of treatment with vinorelbine was also demonstrated in the NAVotrial 01 study [13]. In non-squamous cell lung cancer, the effectiveness of cisplatin (75 mg/m2) and pemetrexed (500 mg/m2) was compared with a combination of cisplatin (80 mg/m2) and SPV (60–80 mg/m2). In the absence of signs of progression after 4 courses, cisplatin was excluded from the regimen and treatment was continued with pemetrexed or vinorelbine. Of the 153 patients included in the study, 51 received pemetrexed and 102 received IPV. The objective effect was 31.4 and 24.0%, disease control was 76.5 and 75.0% in the pemetrexed and ERV groups, respectively. Noteworthy are the equally high median TTP, amounting to 4.3 and 4.2 months with median OS of 10.8 and 10.2 months, respectively. In the support phase, the frequency of neutropenia is grade 3/4. those receiving pemetrexed were higher (30.3 vs. 20.8%); There were no cases of febrile neutropenia. The incidence of nonhematologic toxicity was comparable in both groups.
Oral vinorelbine is attractive as a component of adjuvant chemoradiotherapy. A direct comparison of the regimens demonstrated no statistical difference in median OS and TLR for both forms of vinorelbine. The side effect profile was similar, but gastrointestinal complications were observed more often in those receiving oral vinorelbine. This allows us to conclude that oral vinorelbine is an adequate replacement for the intravenous form in combination with cisplatin in adjuvant therapy [14].
Thus, in NSCLC, replacing the intravenous form of vinorelbine with SVC does not reduce the effectiveness of treatment, allowing one to avoid a number of complications of therapy. Taking into account the favorable side effect profile and ease of administration, the use of ERV seems rational not only in the first line, but also in the maintenance phase of treatment as a component of chemoradiation adjuvant therapy and when used independently by elderly and debilitated patients.
Mammary cancer
The effectiveness of oral vinorelbine as 1st or 2nd line treatment for metastatic breast cancer has been studied in several studies. The vast majority of patients had previously received neo- or adjuvant treatment with anthracycline- and/or taxane-containing regimens. The rate of achieving an objective effect in these prognostically unfavorable groups ranged from 25 to 41%, the median TDP was 4–7 months [15]. The regimens for the use of ERV (60 mg/m2 during the 1st course, followed by escalation to 80 mg/m2) were well tolerated. Side effects 3-4th century. were represented by neutropenia with a frequency of 7–39%. There were virtually no cases of alopecia development. Comparable data were obtained in other studies, where in the 1st line of treatment of metastatic HER2-negative breast cancer, self-administration of vinorelbine induced an objective effect in 29%, and stabilization of the disease in 39% of patients with a median TDP of 5.2 and OS of 16.0 months [ 16].
Given the ease of use, it seems appropriate to replace the injectable form of vinorelbine with capsules in the popular combination of vinorelbine and capecitabine (VinCap). The regimen has been found to be highly effective in the first line of treatment of HER2-negative breast cancer [17]. The rate of achieving an objective effect was 51%, a therapeutic effect was 63%, with a median effect duration of 7.2 months. Median TFS and OS were 8.4 and 29.2 months, respectively. The most common side effects are grade 3–4. were represented by neutropenia (49%, including febrile - 4%), vomiting (9%), stomatitis (7%). Alopecia stage 2 occurred in only 9% of patients. These results were confirmed in three similar studies, where the antitumor effect was achieved in more than 50% of cases.
Equal effectiveness of vinorelbine and capecitabine and the docetaxel + capecitabine regimen in the 1st line of treatment of patients with metastatic HER2-negative breast cancer who previously received anthracyclines in neo- or adjuvant treatment has been established [18]. Disease control was achieved in 70.5 and 70.8% of cases; median OS were 22.2 and 24.2 months, respectively. However, the complication profile was different. Those receiving VinCap were less likely to experience neutropenia, infectious complications, hand-foot syndrome, asthenia, and alopecia. In turn, the combination of docetaxel + capecitabine was less likely to be complicated by gastrointestinal toxicity.
The VinCap regimen was also effective in “late” lines of treatment, in cases of refractoriness to anthracyclines and taxanes. The combination of ERV 60 mg/m2 on days 1 and 8 and capecitabine 2000 mg/m2 on days 1–14 induced an objective effect in 38.8% of patients, stabilization in 37.8%. The median TDP was 7 months, OS was 10, which is a high indicator for these prognostically unfavorable patients [19].
Of interest is the effect of vinorelbine dose intensity on therapeutic results in patients who progress after anthracycline- and taxane-containing regimens.
The VinCap combination study included 41 patients [20]. Partial effect was achieved in 43.9%, stabilization - in 36.6% of cases; median TFS and OS were 9 and 27.2 months, respectively. Taking into account dose reduction and increasing intervals between courses, the median dose intensity for vinorelbine was 43.2 mg/m2 (72% of the planned), and for capecitabine - 1500 mg/m2 (75% of the planned). The frequency of achieving the effect did not differ significantly between the planned and reduced doses of vinorelbine and capecitabine. Median TFS and OS were higher in patients who received the planned doses of drugs, but there was no statistically significant difference between the indicators in the subgroups. Thus, reducing the dose of both drugs by 25% in the majority of patients did not clearly affect the therapeutic efficacy. For the sake of objectivity, it should be noted that these results must be treated with caution, since they were obtained in a retrospective study that included a small group of patients.
The use of vinorelbine capsules as a component of the treatment of patients with HER2-positive breast cancer seems relevant. In combination with trastuzumab in the first line treatment of metastatic disease, the effectiveness was 61–84%, including complete response in 18% of patients, with a median TFS of 9–12 months and OS of 31.0–35.6 months or higher [15].
It appears that inclusion of capecitabine in the regimen improves treatment outcomes in HER2-positive breast cancer. According to two studies, in the 1st line, a triple combination (vinorelbine + capecitabine + trastuzumab) induces an overall effect in 77–85% of patients with a median TDP of 12–13 months. Median OS had not been reached at the time of publication [21, 22].
Similar data were obtained in two parallel prospective phase II studies of VinCap + trastuzumab regimens with both forms of vinorelbine [23]. High and almost identical therapeutic efficacy of both regimens was demonstrated. The rate of achieving an objective effect was comparable in the groups with intravenous and capsulated vinorelbine, amounting to 73.1 and 76%, including a complete effect in 12.2 and 13% of patients, respectively. The median TDP reached 8.2 and 8.8 months, OS – 32.4 and 34.3 months, respectively.
Thus, vinorelbine for oral administration, taking into account its ease of use, effectiveness and favorable side effect profile, serves as a rational alternative to its intravenous form, both when used alone and in combinations. The use of SVC seems promising for stage IIIb–IV NSCLC. in the maintenance treatment phase and as a component of chemoradiation adjuvant therapy. For breast cancer, SVC can be prescribed either alone or in combinations. Its use in the first line of treatment of metastatic HER2-positive breast cancer in combination with anti-HER2 agents is optional. Vinorelbine is effective and safe for elderly patients with regular medical monitoring.
Side effects of the drug Vinorelbine 'ebeve'
From the blood system The dose-limiting factor during vinorelbine therapy is neutropenia. It is reversible (indicators quickly (after 5–7 days) normalize) and non-cumulative. The following courses of treatment can be prescribed only after the granulocyte count has normalized. Anemia and thrombocytopenia also occur, but are rarely severe. On the part of the immune system Like other vinca alkaloids, vinorelbine in isolated cases can cause the development of shortness of breath and bronchospasm, and also extremely rarely - local and generalized skin reactions. From the nervous system: Peripheral neuropathy. Damage is usually limited to decreased or loss of deep tendon reflexes. Paresthesia is possible. These effects are dose-dependent and disappear after cessation of treatment. Autonomic neuropathy. Its main symptom is intestinal paresis, which causes constipation. In some cases, paralytic intestinal obstruction may develop. Treatment with vinorelbine can be continued after normal peristalsis has been restored. Vascular disorders: With repeated administration of vinorelbine, burning pain at the injection site and local phlebitis are possible. When vinorelbine is administered by bolus injections with further lavage of the vein with a large amount of 0.9% sodium chloride solution, this effect is less pronounced. In some cases, vinorelbine must be administered through a central venous catheter. From the gastrointestinal tract Constipation (see side effects from the nervous system), diarrhea, nausea/vomiting; To reduce the severity of these effects, antiemetic drugs are used. Skin and subcutaneous tissue disorders Alopecia (its severity may progressively increase with repeated courses of treatment). General side effects and local reactions Sometimes there is pain in the jaws. Paravenous administration can cause local reactions (in isolated cases, tissue necrosis). Apparently, vinorelbine has mutagenic properties, given its effect on the mitotic apparatus of the cell. With prolonged administration of vinorelbine to laboratory animals every 2 weeks, no carcinogenic effects were observed. Experiments on animals have demonstrated the embryo- and feto-lethal and teratogenic effects of vinorelbine.
Special instructions for the drug Vinorelbine 'ebeve'
During treatment with vinorelbine, hematological parameters should be constantly monitored (before each administration of the drug, the level of hemoglobin, the number of leukocytes, granulocytes and platelets should be determined). If the neutrophil granulocyte count decreases to ≤2000/mm3, administration of vinorelbine should be delayed until bone marrow function is restored and the patient should be under medical supervision. If symptoms of infectious processes appear, the patient must be immediately examined and appropriate treatment prescribed. In case of significant impairment of liver function, the dose of vinorelbine should be reduced. In case of impaired renal function, there is no need to reduce the dose of the drug, since renal excretion of vinorelbine is negligible. Vinorelbine should not be administered in combination with radiation therapy to the liver area. There are currently no data on the effectiveness and safety of treatment with vinorelbine in children. Vinorelbine should not be prescribed during pregnancy. Patients should use effective methods of contraception during treatment with the drug. If pregnancy occurs during vinorelbine therapy, a genetic specialist should be consulted regarding further actions. It is not known whether vinorelbine is excreted in breast milk, so breastfeeding should be discontinued before starting treatment with the drug. It is not known whether vinorelbine affects the ability to drive vehicles and use machines.
Vinorelbine
— The drug is intended exclusively for intravenous administration. Intrathecal administration can be fatal and is strictly prohibited!
— Treatment with Vinorelbine should be carried out under the supervision of a physician experienced in working with anticancer drugs. During the treatment period, careful hematological monitoring should be carried out - determining the number of leukocytes, neutrophils, platelets and hemoglobin on the day of each administration.
- If a concomitant infection is suspected, the patient should be examined on the day of starting therapy and the benefit-risk ratio should be assessed when deciding whether to administer the drug.
- If shortness of breath, cough or hypoxia of unknown etiology occurs, the patient should be examined to exclude pulmonary toxicity.
- If paralytic intestinal obstruction develops, the drug should be discontinued. Treatment can be continued after restoration of normal intestinal motility.
— Contact of the concentrate on the skin, mucous membranes or eyes can cause burns. If this occurs, the affected areas should be immediately and thoroughly washed with 0.9% sodium chloride solution.
— The drug Vinorelbine should not be used simultaneously with radiotherapy, especially involving the liver area.
- Vinorelbine should be used with caution with strong inhibitors or inducers of the CYP3A4 isoenzyme; simultaneous use of the drug with phenytoin, itraconazole, and live attenuated vaccines is not recommended.
Effect on fertility
Men and women should use reliable methods of contraception during treatment with Vinorelbine, as well as for three months after the end of chemotherapy.
For patients planning to have children after completion of treatment, genetic counseling is recommended.
Due to the possibility of irreversible loss of fertility as a result of treatment with vinorelbine, patients should be advised to conserve sperm before starting treatment with vinorelbine.
Instructions for administering the prepared solution and disposing of waste
Preparation for administration and administration of Vinorelbine should be carried out by medical personnel trained in the use of chemotherapy drugs. Personnel should wear eye protection, disposable gloves, a mask and an apron. The drug should be administered strictly intravenously: it is very important to ensure that the needle or catheter is accurately positioned in the vein before starting the drug administration.
In case of extravasation, stop the infusion, “flush the vein” with 0.9% sodium chloride solution, and inject the remainder of the dose into another vein. In case of extravasation, intravenous glucocorticosteroids should be immediately administered to reduce the risk of phlebitis. Storing the prepared solution for infusion
From a microbiological point of view, the prepared solution should be used immediately. If the drug is not administered immediately, the healthcare professional assumes responsibility for the conditions and duration of its storage prior to administration. Unused solution or waste must be disposed of in accordance with the regulations of the medical institution.
Typically, storage time after reconstitution should not exceed 24 hours at +2°C +8°C, unless reconstitution is carried out under controlled and validated aseptic conditions.
After diluting vinorelbine in saline or 5% glucose solution, chemical and physical activity persists for 8 days at a temperature of +20 °C ± 5 °C or in the refrigerator (+2 °C - +8 °C), protected from light place, in a glass bottle, in a PVC or vinyl acetate bag.
Drug interactions Vinorelbine 'ebeve'
When used in combination with cisplatin, the pharmacokinetics of vinorelbine do not change. The concentrate for preparing a solution for infusions of Vinorelbine “Ebewe” cannot be diluted with alkaline solutions due to the risk of sedimentation. In the case of combination chemotherapy, Vinorelbine "Ebewe" cannot be mixed with other drugs. The concentrate for preparing a solution for infusions Vinorelbine “Ebewe” can be diluted only with the solutions specified in the APPLICATION section. Vinorelbine is not absorbed and does not interact with infusion systems made of polyvinyl chloride, polyethylene or neutral flint glass.
Navelbine (vinorelbine) in the treatment of lung cancer
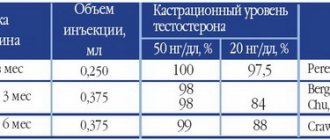
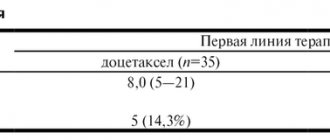
Non-small cell lung cancer is now considered a tumor sensitive to chemotherapy due to the introduction into widespread clinical practice of modern drugs such as navelbine, paclitaxel, docetaxel, gemcitabine, and irinotecan. The standards of first-line chemotherapy for NSCLC include combinations based on platinum derivatives and one of the above drugs, which allows for an overall effect in 40–60% of patients and a one-year survival rate of 30–50%. Navelbine, a semisynthetic vinca alkaloid, inhibits the polymerization of microtubule tubulin. Already during phase I–II clinical trials, the effectiveness of Navelbine in patients with disseminated NSCLC was noted. In these studies, Navelbine was administered at a dose of 25–30 mg/m2 once a week for 2–3 months until toxicity occurred. The dose-limiting toxicity was grade III–IV neutropenia in 21% [1]. A low level of other side effects was noted: infection, nausea, vomiting, alopecia, peripheral neuropathy. Table 1 presents the results of phase II study of Navelbine in stage III–IV NSCLC. [2]. When studying Navelbine monotherapy in 76 patients with NSCLC in the chemotherapy department of the Russian Cancer Research Center named after. N.N. Blokhin, Russian Academy of Medical Sciences, the overall effect was noted in 30.2%, the median survival was 36 weeks [3]. The results obtained (overall effect 12–31.1%, survival 25–52.4 weeks) served as the basis for organizing and conducting large phase III clinical trials of Navelbine in patients with NSCLC, to study the effectiveness of Navelbine in combination with platinum derivatives, because . Previously, the standard combination for the treatment of NSCLC was cisplatin + etoposide. The effectiveness of combinations of Navelbine with cisplatin and carboplatin is presented in Tables 2 and 3.
In the chemotherapy department of the Russian Cancer Research Center named after. N.N. Blokhin Russian Academy of Medical Sciences, 44 patients with stage III–IV NSCLC received the combination of Navelbine + cisplatin in the 1st line of treatment. The regimen used was: Navelbine 25 mg/m2 on days 1, 8, 15, 22 + cisplatin 100 mg/m2 on day 1. The treatment cycle is 28 days. The overall effect was obtained in 43.2%, the complete effect was 2.3%, stabilization of the process was 22.7%. Median survival was 46 weeks, one-year survival rate was 38.6%. The main types of toxicity were neutropenia (grade III–IV 77.2%), anemia (grade III–IV 22.7%), neurotoxicity (grade I–II 4.5%) [2]. In recent years, multicomponent chemotherapy regimens based on cisplatin and new cytostatics have been actively studied in NSCLC in order to increase the effectiveness of treatment. Similar studies are being carried out with Navelbine (Table 4). Summary data on clinical trials with three cytostatics for NSCLC are presented in Table 5. As can be seen from the presented data, Navelbine is well combined with both platinum derivatives and other new drugs for the treatment of NSCLC and is not inferior to them in effectiveness. In the work of K. Takeda, 2002 [22], there were also no differences in effectiveness when comparing combinations of irinotecan + cisplatin, paclitaxel + cisplatin, gemcitabine + cisplatin, Navelbine + cisplatin (cooperative study of 602 patients). If it is impossible to use platinum derivatives in patients with NSCLC, many researchers use combinations that include Navelbine. For patients with NSCLC who have received 1 line of chemotherapy, an active search is underway for effective combinations among new drugs. According to Pectasides et al., [27] in the 2nd line, Navelbine in combination with irinotecan (Navelbine 25 mg/m2 on days 1.15 + irinotecan 150 mg/m2 on days 1.15, every 28 days) was effective in 14. 6% of patients with stabilization in 21.3% of patients and median survival of 7.8 months. The combination: gemcitabine 1000 mg/m2 + Navelbine 25 mg/m2 1.5 days every 28 days in the 2nd line (after paclitaxel and carboplatin) was effective in 11 out of 28 patients (partial effect), stabilization of the process in 9 out of 28 patients, median survival was 18 weeks (Table 6) [28]. Given its good tolerability, Navelbine is actively used in elderly patients, both in monotherapy and in combinations (Table 7). Monotherapy with Navelbine in the elderly provides an effect of 19.7–39.1% with a median survival of 29–53 weeks [29]. In recent years, neoadjuvant chemotherapy for NSCLC has been actively developing and this has been proven for stage III. diseases [35]. Naturally, as one of the new drugs active in NSCLC, Navelbine is being studied in adjuvant and neoadjuvant chemotherapy regimens. According to Martins et al. [36], with neoadjuvant use of the combination Navelbine + cisplatin, 27% of patients with stage III. NSCLC were operated on, 70% had a complete effect, 22.5% were alive for 3 years. Combination of cisplatin + epirubicin + Navelbine (3 courses before surgery) in elderly patients with stage IIIA NSCLC. allowed to obtain an overall effect in 55% and 66% of patients underwent surgery [37]. According to MOKOB data [38], with neoadjuvant use of 2 cycles of chemotherapy according to the regimen of cisplatin 100 mg/m2 on day 1 + Navelbine 25 mg/m2 on days 1 and 8, an objective effect was noted in 63%, stabilization in 28.6%, surgery was performed 89% of patients. Pathomorphosis of grade III–IV – in 31% of patients. When assessing long-term results after 24 months of observation, there was a significant increase in life expectancy of patients receiving chemotherapy compared with simply operated patients. Table 8 summarizes the data from all 9 comparative randomized clinical trials of phase III, which most fully characterize the place of Navelbine in chronic NSCLC. Summarizing the data from the above studies (more than 1750 patients), we can conclude that the combination of Navelbine + cisplatin in stage IIIB–IV NSCLC. provides: objective response in 25–44%, median survival 8–11.6 months, 1-year survival 33–48%. Thus, the combination of Navelbine + cisplatin is one of the optimal first-choice options for chronic NSCLC, and the doctor’s decision is made taking into account the individual characteristics of the patient, the toxicity profile of cytostatics and the cost of treatment. For many years, the feasibility of adjuvant (postoperative) chemotherapy in patients with early stages of NSCLC who have undergone radical surgery has remained a subject of debate. A significant contribution to the argument “for” comes from the results of a phase III study published at ASCO 2004 (Winton T. et al. Phase III randomized trial or adjuvant vinorelbine and cisplatin in completely resected stage IB and II nonsmall cell lung cancer. Proc.Am Soc. Clin. Oncol. 2004; Vol 23: abstr. 7018 - oral communication). It was shown that as a result of the use of x/t Navelbine 25 mg/m2 weekly. + cisplatin 50 mg/m2 D1, cycle 8 4 weeks, 4 cycles after radical surgery in patients with NSCLC achieved (compared to the control group): – increase in 5-year disease-free survival by 13% (61% vs48%) – increase 5– year overall survival by 15% (69% vs54%) The results are highly reliable. The combination of Navelbine with cisplatin, thus, provides a dramatic improvement in the results of treatment of early stages of NSCLC. Considering that the standard treatment for patients with inoperable stage III NSCLC is combined chemoradiotherapy, in recent years active research has been conducted on the use of new drugs, including Navelbine, in combination with various radiation regimens (hyperfractionation, combined use). When navelbine is used in combination with platinum derivatives and various irradiation regimens in inoperable patients with NSCLC, the overall effect can be obtained in 60–83% of cases [40,41,42]. Research continues. An oral form of Navelbine has been developed, which is equal in effectiveness to the intravenous form, is more convenient to use and is currently being actively studied in various combinations for NSCLC [43,44]. Standard regimen for oral Navelbine (monotherapy): 60 mg/m2 once a week for 3 injections, then 80 mg/m2 per week under the control of blood counts. In a few studies in small cell lung cancer (SCLC), the effectiveness of Navelbine in the 1st line is 27%, in the 2nd line – 12–16% with a remission duration of 10–17 weeks. The combination of Navelbine with Vepezid and cisplatin is effective in 77% in localized SCLC and 40% in disseminated SCLC [45]. One of the most actively studied areas in the treatment of NSCLC is the use of “targeted” drugs in combination with chemotherapy. Phase I of a clinical study of the combination Navelbine + Tarceva (an inhibitor of tyrosine kinase receptors of epidermal growth factor) in patients with HMSPL has begun [46]. When using cetuximab in combination with cisplatin and Navelbine in patients with NSCLC, the overall effect was observed in 59%, and in the group receiving only chemotherapy, the overall effect was 36% [47]. The research is ongoing. Thus, Navelbine is one of the effective drugs included in the standard treatment regimens for NSCLC, has moderate toxicity, is well combined with other drugs and radiation therapy, and can be used on an outpatient basis, as well as in elderly and debilitated patients.
References 1. Furuse K., Fukuoka M., Kuba M., et al. Randomized study of vinorelbine versus vindezine in previously untreated stage IIIB or IV NSCLC. Ann. Oncol., 1996, v. 7, N8, p. 815–820. 2. Marenich A.F., Gorbunova V.A. Modern antitumor drugs in the treatment of stage III–IV non-small cell lung cancer (NSCLC). In: “New in Lung Cancer Therapy,” ed. Prof. N.I. Perevodchikova, Moscow, 2003, p. 81–117. 3. Besova N.S. Results of a clinical study of new antitumor drugs navelbine and nitrulline for NSCLC. Abstract of Ph.D. diss. Moscow, 1997. 4. De Marinis F., Rimoldi R., Piacenza G., et al. Advanced non–small cell lung cancer: treatment with cisplatin and two different schedules of vinorelbine. Proc. 4th Int. Cancer Conf, Perugia, 1993. 5. Piazza E., Filipazzi V., Pho V., et al. Cisplatin – vinorelbine association chemotherapy in the treatment of locally advanced NSCLC. Proc. IASLC, 1994(suppl.l),p. 128, N490. 6. Martoni A., Guaraldi M., Piana E., et al. Phase III trial on high-dose epirubicin – cisplatinum (CP) vs vinorelbine + CP in advanced Non Small Cell Lung Cancer. Proc. ASCO, 1996, v. 15, p. 373, N 1108. 7. Terrasa J., Rifa J., Grcia-Bueno JM, et al. Cisplatin and Vinorelbine in advanced Non–Small Cell Lung Cancer. Ann. Oncol, 1996, v. 7, suppl. 5, p. 97, N416P. 8. Adam Z., Koler V., Rozaner P., et al. Combined treatment with Navelbine and Cisplatin in patients suffering from inoperable Non Small Cell Lung Cancer. Proc. SOMPS, 1995, p. 263, N.P6070. 9. Bretti S., Gorzengo G., La Ciura P., et al. Cisplatin and Vinorelbine Combination Chemotherapy in Stage III–IV Non Small Cell Lung Cancer: A Multicenter Phase II Trial. Ann. Oncol., 1994, v. 5, suppl. 8, p. 153 N. P7650. 10. Coppola F., Capo A., van Koten M., et al. Phase P study: Navelbine + Cisplatin in Non–Operable Non–Small Cell Lung Cancer Stage IIIB–IV. Ann. Oncol, 1994, v. 5, suppl. 8, p. 158, N792. 11. Jacoulet P., Gamier G., Breton JI, et al. Navelbine and Carboplatin combination in advanced Non–Small Cell Lung Cancer: a phase MI study with a CBDCA dose–escalation scheme. Proc. SOMPS, 1995, p. 146. 12. Santomaggio S., Right R., Tucci E., et al. Carboplatin and Vinorelbine in metastatic Non Small Cell Lung Cancer. Preliminary results. Proc. IASLC, v. 11, suppl. l,p. 125, N478. 13. Masotti A., Borzelino G., Zaunini G., et al. Efficacy and toxicity of vinorelbine – Carboplatin combination in the treatment of advanced adenocarcinoma or large–cell carcinoma of the lung. Tumori, 1995, v. 81, pp. 112–116. 14. Garst J., Crawford J., O'Rourke M., et al. Vinorelbine and Carboplatin for the treatment of patients with advanced Non Small Cell Lung Cancer: a phase P response, toxicity and survival study. Proc. ASCO, 1996, v. 15, p. 404, N1233. 15. Colleoni M., Vicario G., Nelli P., et al. A randomized phase P trial of Carboplatin, Vinorelbine versus Cisplatin, Mitomycin C, Vinorelbine in advanced Non–Small Cell Lung Cancer. Ann. Oncol., 1996, v. 7, suppl. 5, p. 98, N464P. 16. Niho S., Kubota K., Araki K., et al. A phase P study of gemcitabine, vinorelbine and cisplatine in advanced NSCLC. ASCO, 2001, v. 20, p. 241b, N2716. 17. Friedman EL, Straus MI, Ambunder JM Vinorelbine, paclitaxel and carboplatin for adenocarcinoma of the lung. ASCO, 2000, v. 19, p. 512, N2004. 18. Bameto J., Sanchez RP, Noguer M., et al. Alteraant chemotherapy with cisplatin, vinorelbine and gemcitabine–paclitaxel as first–line treatment for advanced NSCLC. ASCO, 2001, v. 20, p. 241b, N2715. 19. Hosoe S., Komuta K., Shibata K., et al. Gemcitabine and vinorelbine followed by docetaxel in patients with advanced NSCLC: final results of phase II trial of sequential non-platinum triplet combination chemotherapy. Proc. ASCO, 2002, v. 21, 315a, N1259. 20. Buffani L., Dougiovanni D., Addeo A., et al. Sequential chemotherapy with cisplatin / vinorelbine followed by paclitaxel / gemcitabine in advanced NSCLC: a phase II study. Proc. ASCO, 2002, v. 21, p. 21 Ib, N2664. 21. Bum P., Kelly K., et al. Clinical Lung Cancer. 2000, 2 (suppl. 1), 23–8. 22. Takeda K., Negoro S., Ohashi Y., et al. Preliminary Results of Four Arm Cooperative Study for Advanced Non–Small Cell Lung Cancer in Japan. Lung Cancer, 2003, v. 41, suppl. 2, s. 64, N.0–219. 23. Katakami N., Nishimura T., Sugiura T., et al. Vinorelbine plus gemcitabine in the treatment of chemotherapy naive stage IIIB/IV NSCLC. ASCO, 2001, v.20, p.255b, N2773. 24. Westeel V., Breton J., Braun D., et al. Gemcitabine and vinorelbine – a phase II study of a weekly low-dose combination without rest in advanced NSCLC. ASCO, 2001, v. 20, p. 250b, N 2751. 25. Tsao A., Kirn ES, Nazario A., et al. Phase II study of vinorelbine and docetaxel in the treatment of advanced non–small cell lung cancer as front line and second line therapy. Proc. ASCO, 2003, v. 22, 691, N 2779. 26. Nagashima S., Nakamura Y., Kasai T., et al. Phase I study of vinorelbine and weekly irinotecan as first line chemotherapy in patients with advanced non–small cell lung cancer. Proc. ASCO, 2003, v. 22, 698, N 2808. A complete list of references can be found on the website https://www.rmj.ru 27. Pectasides DG, Fountzilas G., Rigopoulos A., et al. An outpatient second–line chemotherapy with irinotecan and vinorelbine in patients with NSCLC previously treated with cisplatin–based chemotherapy. Proc. ASCO, 2002, v. 21, p.327a, N1307. 28. Moutalar J., Lopez-Tendeno P., Diaz-Bedverdge R., et al. Gemcitabine–Vinorelbine as second line chemotherapy in advanced non–small cell lung cancer previously treated with Paclitaxel , Carboplatin. Lung Cancer, 2003, v.41, suppl.2, s.95, P–19. 29. Besova N.S. Chemotherapy of non-small cell lung cancer in the elderly. In: “New in Lung Cancer Therapy,” ed. Prof. N.I. Perevodchikova, 2003, pp. 133–143. 30. Lippe P., Imperatory I., Casadei V., et al. Weekly cisplatin and vinorelbine in advanced non small cell lung cancer elderly patients. A phase II study. Ann. Oncol., v. 11, suppl. 4, 2000, p. 73, N321. 31. Martins S., Perreira J., Ikari F., et al. Chemotherapy with cisplatin and vinorelbine for elderly non–small cell lung cancer patients. Proc. ASCO, 1999, v. 18, N1890. 32. Maestu I., Munoz J., Lorenzo GA, et al. Assessment of comorbidity, symptoms and functional status in advanced non small cell lung cancer elderly patients treated with gemcitabine and vinorelbine. Lung Cancer, 2003, v. 41, suppl. 2, s. 91, N. P–2. 33. Le Caer H, Delhoume JY, Thomas PA, et al. A multicenter phase II study of carboplatin / vinorelbine in advanced non–small cell lung cancer in elderly patients. Lung Cancer, 2003, v. 41, suppl. 2, s. 93, N.