Alendronate, 4 pcs., 70 mg, tablets
Alendronate should only be taken with plain water, since other drinks (including mineral water, coffee, tea, orange juice) reduce the absorption of alendronic acid. Absorption of bisphosphonates is significantly reduced when administered concomitantly with food. To reduce the irritating effect on the esophagus, Alendronate should be taken immediately after getting up in the morning with a full glass of water. After administration, you should be in an upright position (standing or sitting) for 30 minutes (it is dangerous to use the drug if the patient is unable to stand or sit straight for the specified time). Taking Alendronate before bed or in a horizontal position increases the risk of developing esophagitis.
The patient should be informed of the need to stop taking Alendronate and consult a doctor if dysphagia develops, pain when swallowing, chest pain or heartburn occurs. In case of hypocalcemia, it is necessary to correct it before starting treatment. It is also necessary to eliminate mineral metabolism disorders that lead to hypocalcemia (vitamin D deficiency, hypoparathyroidism, calcium malabsorption). Therapy should be carried out against the background of a diet enriched with calcium salts. When taking bisphosphonates (especially with concomitant therapy with glucocorticosteroid drugs), it is necessary to ensure the intake of adequate amounts of calcium and vitamin D from food or in the form of medications.
During treatment, due to the positive effect of alendronic acid on bone mineral density, a slight asymptomatic decrease in the concentration of calcium and phosphate in the blood serum may be observed. Before prescribing bisphosphonate therapy, patients with underlying risk factors (eg, cancer, chemotherapy, radiation therapy, corticosteroids, poor oral hygiene) should undergo a dental examination with appropriate preventative dental treatment. Patients being treated with bisphosphonates should avoid invasive dental procedures whenever possible. Osteonecrosis of the jaw, usually associated with tooth extraction and/or local infection (including osteomyelitis), has been reported in cancer patients receiving intravenous bisphosphonates (many of whom were also prescribed chemotherapy and corticosteroids). There are reports of the development of osteonecrosis of the jaw in patients with osteoporosis during the use of oral bisphosonates.
In patients with osteonecrosis of the jaw who are on bisphosphonate therapy, dental surgery may worsen the condition. If surgical interventions are necessary, it should be taken into account that there is no data on the possibility of reducing the risk of developing osteonecrosis of the jaw after discontinuation of a bisphosphonate. Prescriptions and recommendations of the attending physician should be based on an individual assessment of the benefit/risk ratio for each patient.
Prospects for the use of alendronate for the treatment of postmenopausal osteoporosis
Bisphosphonates are first-line drugs for the treatment of osteoporosis (OP) and fracture prevention. However, patient adherence to treatment with them remains low. It has been established that in Russia one of the leading reasons for discontinuation of therapy is the high cost of most original anti-osteoporotic drugs. Due to their availability and optimal effectiveness/cost ratio, generic alendronate has become widely prescribed for AP. However, the quality of the drugs is not uniform and requires careful evaluation. First of all, you need to find out whether they correspond to the original drug. The review discusses the possibility and feasibility of using generic drugs of alendronate, in particular the drug Forosa®, in patients with AP.
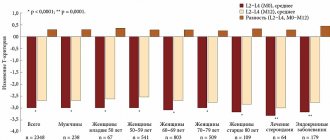
Rice. 1. Efficacy of alendronate 10 mg against vertebral (A) and proximal femoral (B) fractures in the FIT study
Rice. 2. Dynamics of bone mineral density over ten years of treatment with alendronate 10 mg/day in the FLEX study
Osteoporosis (OP) is called a silent epidemic due to its widespread prevalence and asymptomatic course. The main goal of therapy for AP is to prevent fractures, which develop against the background of decreased bone mineral density (BMD), disturbances in the microarchitecture of bone tissue, and are associated with an increased risk of disability and death. It is predicted that the number of fractures due to bone fragility will increase, which is associated with increasing life expectancy and changing demographics in the world.
Epidemiological studies have shown that about 40–50% of women and 13–30% of men after 50 years of age have one or more fractures associated with AP. These data are equivalent to the risk of cardiovascular diseases caused by atherosclerosis [1, 2].
In the world, 8.9 million fractures associated with AP occur annually, of which 4.5 million occur in America and Europe [3]. Unfortunately, there are no complete epidemiological data in Russia. However, using modeling of the epidemiological situation, it has been shown that over 9 million people have peripheral fractures and 3.8 million vertebral fractures occur annually [4].
The cost of treating all osteoporotic fractures in the countries of the European Union is 38.7 million euros per year [5], and the treatment and rehabilitation of patients after a hip fracture is more than 85% of all costs associated with AP [6].
As life expectancy increases in most countries, the financial and other costs associated with osteoporotic fractures will only increase unless preventive measures are taken.
The high prevalence of AP and associated fractures lead to disability and a significant decrease in quality of life.
The high costs of treating fractures place AP in the category of socially significant diseases and is currently one of the important problems of public health, but in Russia this disease has not yet been awarded the status of socially significant. Patients do not receive free examinations or medications. 76% of patients purchase drugs from personal funds [7].
The results of randomized clinical trials (RCTs) have shown that for the treatment of AP and the prevention of both primary and recurrent fractures, different classes of drugs can be used: those that reduce bone tissue destruction (antiresorptive) or increase its formation. Bisphosphonates are considered today as first-line drugs in the treatment of AP. Alendronate is recognized as the gold standard for the treatment of AP.
The recent increase in bisphosphonate prescriptions by physicians is due to the extensive evidence base demonstrating efficacy and an optimal safety profile, as well as the lack of need for constant monitoring of laboratory parameters to assess the risk of adverse events. However, patient adherence to treatment with them, as with other anti-osteoporotic drugs, remains low. Among the reasons for refusing to take the drug are poor patient awareness of the positive effect, the overall cost of treatment, the development of adverse events and poor motivation, which is associated with insufficient quality of medical care for AP [8, 9]. A year after the drug was prescribed, less than 50% of patients continue treatment with it [10]. At the same time, poor adherence to therapy (less than 50%) is associated with an increased risk of fractures by 40% (compared to patients whose adherence to treatment reaches 90%) [11]. It should be noted that if treatment adherence is less than 50%, then the effectiveness of therapy is equal to zero [12]. In addition, patients who are not adherent to treatment are at increased risk of hospitalizations associated with fractures and secondary complications such as severe pain, secondary nosocomial infections, and pulmonary thromboembolism; the quality of life deteriorates significantly [13, 14].
In Russia, one of the leading reasons for discontinuation of therapy is the high cost of most original anti-osteoporotic drugs. Thus, according to the results of a one-year observation in primary health care of 427 patients with postmenopausal AP who were prescribed Fosamax® 70 mg once a week, in 35.8% of cases, discontinuation of the drug was associated with its high cost [16].
These drugs are not available to patients with limited financial resources, especially pensioners, who make up a large proportion of patients with AP.
Despite the fact that at present, along with tablet drugs, there are drugs for subcutaneous, intramuscular and intravenous administration, the former are the most widely used [17].
It is important to recall that when choosing the optimal form of the drug for a patient, it is necessary to take into account concomitant diseases, individual characteristics and preferences in the regimen of taking the drug.
Pharmacoeconomic analysis conducted in different countries with the aim of identifying the least expensive methods of treating AP has shown that secondary prevention of fractures is most appropriate in women and men over 70 years of age with previous fractures and low BMD (-2.5 standard deviation according to the T-criterion) or other risk factors (eg, low body weight, history of stroke) [18]. It should be noted that it was the example of alendronate that demonstrated the greatest economic effectiveness of bisphosphonates in high-risk groups [19–21].
The goal of prevention and treatment of osteoporosis is to ensure an increase in bone mass, reduce the incidence and risk of fractures, and improve the quality of life of patients. This required the organization of three to five year randomized studies to prove the effectiveness of alendronate. The largest of these are FOSIT, a multicenter (34 countries), randomized, double-blind, placebo-controlled trial that included 1908 postmenopausal women with AP who received alendronate 10 mg daily for 12 months, and FIT, a multicenter (11 US centers), randomized, double-blind, placebo-controlled trial. A study of 2,027 postmenopausal women receiving alendronate at doses of 5 and 10 mg for three years, as well as a ten-year follow-up of patients who continued to receive alendronate at the same doses or placebo. Alendronate showed high efficiency: increasing BMD in all areas of measurement - from 5.4% in the femoral neck to 13.7% in the spine (level of evidence A), it significantly reduced the incidence of fractures in the spine (by 47%), hip (by 51 -56%), forearm (by 48%). The progression of vertebral deformities decreased in 64% of patients (level of evidence A).
However, in Russia, high-risk groups for AP are mainly represented by low-income citizens who have to bear the burden of drug costs themselves. Thus, the availability of more affordable drugs on the Russian pharmaceutical market will reduce the costs of the patients themselves and will allow a larger number of patients to receive adequate therapy.
Due to their availability and optimal effectiveness/cost ratio, generic alendronate has become widely prescribed for AP, but the quality of the drugs is uneven and requires careful evaluation. First of all, it is necessary to find out how closely the analogue corresponds to the original drug.
It is possible to minimize the risks when using generics by using a legal copy (the same active ingredient as in the studies) with proven bioequivalence.
Two pharmaceutical products are bioequivalent if they are pharmaceutically equivalent and their bioavailability parameters (rate and degree of availability) after administration at the same dose are similar to a degree that suggests that their effects will be the same. Assessment of pharmacokinetic equivalence assumes that generic drugs bioequivalent to the original provide the same effectiveness and safety of pharmacotherapy, that is, they are therapeutically equivalent.
Currently, publications have appeared on differences in the tolerability of original and generic bisphosphonates in patients with AP. As a result, adherence to therapy and its effectiveness decrease. Some studies have shown a decrease in BMD or a decrease in the rate of bone mass growth when treated with generic alendronate compared to the original drug [22, 23]. Other studies noted an increase in the frequency of adverse reactions and worsening adherence to therapy [24, 25]. In connection with the data obtained, the need to conduct prospective comparative studies is discussed in which the therapeutic equivalence of the original and generic drugs can be established [26].
Obviously, bioequivalence studies of drugs do not replace RCTs that evaluate the effectiveness of drugs. At the same time, the study of therapeutic equivalence in AP is not economically justified, since proof of the anti-fracture effect requires at least three to five years and the participation of large groups of patients. If they are regulated, there will be a significant increase in the cost of generics. In such a situation, they will no longer have the advantage of reducing financial costs.
The use of generics should be based on trust in the pharmaceutical company. That is why in clinical practice it is necessary to use drugs from well-known and well-established companies in the pharmaceutical market. One of these drugs is Forosa® (Sandoz, Switzerland). One tablet of Forosa contains 70 mg of sodium alendronate. Application mode: once a week.
Alendronate belongs to the aminobisphosphonates. The main mechanism of action is inhibition of farnesyl pyrophosphate synthetase. It is a key enzyme in the mevalonate pathway for the synthesis of cholesterol and isoprenoid lipids, which promote prenylation of signaling G proteins that regulate cellular processes necessary for the functioning and survival of osteoclasts [27].
Alendronate has a high affinity (affinity) for bone tissue. It quickly binds to hydroxyapatite. The substance is slowly absorbed into bone tissue and remains in it for a long time even after discontinuation of the drug. Alendronate exhibits greater desorption on the bone surface [28]. The maximum half-life of alendronate in the human body is about ten years [29]. This drug in vivo
does not form metabolites, which explains the small number of side effects. Aminobisphosphonates bind to serum proteins and are eliminated through renal excretion [30].
The effectiveness of alendronate in reducing the risk of vertebral and nonvertebral fractures was shown in the FIT study, a multicenter (11 centers), randomized, double-blind, placebo-controlled study of 2027 postmenopausal women who took 5 and 10 mg of alendronate for three years, as well as a ten-year follow-up of patients who continued receive alendronate in the same doses or placebo [31, 32].
Research results showed a reduction in the risk of vertebral fractures by 59% (p
The long-term effects of alendronate were studied in the FLEX study, which included 1099 patients from a phase III study [34]. Some patients continued taking alendronate (duration of therapy - up to ten years). During the observation period, there was a persistent increase in BMD (Fig. 2) [35]. Patients who stopped taking the drug after five years showed a slight decrease in BMD and an increase in bone turnover markers. However, the risk of fractures did not increase compared with patients who continued to take alendronate. The conclusion was that stopping the drug in women at average risk of developing fractures did not increase the risk of subsequent fractures. However, for patients at high or very high risk of fracture, it is best not to stop therapy after five years [34].
To reduce side effects and improve patient adherence to therapy, a weekly form of alendronate (70 mg/week) was developed. The effectiveness of the new form has been proven in one- and two-year studies with a smaller number of patients and less duration than phase III RCTs, but with equivalent changes in surrogate endpoints (BMD and biochemical markers of bone turnover) [36].
When assessing patient preferences for using different treatment regimens - daily and once a week - more than 85% of patients chose the second option, 9.2% - the first [37].
Since alendronate has been used in Russia for more than 15 years, data on the effectiveness of treatment with the drug in different regimens have been accumulated. Studies show the effect of alendronate on surrogate parameters (BMD and biochemical markers of bone turnover) and good tolerability of the drug, which is consistent with the results of foreign studies [38–41].
A feature of bisphosphonates is their extremely low bioavailability when taken in tablet forms (0.7–1.8%). Therefore, their concentration in blood plasma is so low that it cannot be assessed.
Most of the drug (40–70%) binds to bone tissue hydroxyapatite, the rest is excreted from the body through the kidneys. Therefore, to determine the bioequivalence of the original drug and the generic, urinary excretion parameters are used: Ae0-72, Rmax, Tmax, where Ae0-72 is the cumulative renal excretion over 72 hours of observation after a single dose of the drug, Rmax is the maximum renal excretion, Tmax is the average time to achieve maximum excretion.
To determine the bioequivalence of the drug Forosa® - alendronate sodium 70 mg tablet (Sandoz, Switzerland) and the original alendronate Fosamax® 70 mg tablet (Merck Sharp & Dome, USA) in an independent laboratory Anapharm (Canada), specializing in phase studies I and bioequivalence of drugs, a single-center, open-label, randomized, double-crossover study was conducted involving 106 healthy, non-smoking men aged 18–55 years. The results obtained indicated the bioequivalence of alendronate sodium (Forosa®) to the reference standard and the possibility of its use for the treatment of postmenopausal, glucocorticosteroid AP and decreased bone mass in men: the bioavailability of alendronic acid did not differ significantly in elderly and young patients.
Forosa® should be used to meet the daily requirement for calcium and vitamin D. The optimal duration of therapy has not been established. The duration of bisphosphonate therapy should be assessed on a regular basis, especially after five or more years of use. To ensure proper absorption of the drug Forosa® tablets must be taken in the morning on an empty stomach, at least 30 minutes before the first meal, drinks or other medications, with at least 200 ml of water. Simultaneous administration of alendronic acid with food or within 2 hours after a meal sharply reduces the absorption of the drug. Bioavailability is characterized as negligible. When taken together with coffee or orange juice, it decreases by approximately 60% [42].
Differences in the effectiveness of original and generic drugs may also be due to the excipients they contain. These in the drug Forosa® are microcrystalline cellulose, colloidal anhydrous silicon dioxide, croscarmellose sodium and magnesium stearate. These substances are indifferent to bone tissue.
The advantage of Forosa® is the patented film shell, which, in addition to microcrystalline cellulose, contains carrageenan and macrogol, which protect the esophageal mucosa from damage, facilitating the release of the main substance already in the small intestine.
The use of alendronates (Forosa®) is relevant in postmenopausal women to reduce the risk of vertebral compression fractures and hip fractures; in men for the purpose of treating AP and preventing fractures, as well as with glucocorticosteroid AP.
The use of generic drugs makes it possible to reduce healthcare costs and, above all, the costs of citizens themselves, which is especially important for countries with an imperfect system of compulsory health insurance and social security.
The use of high-quality alendronates with proven bioequivalence will help fulfill the strategic goal of the World Health Organization to ensure widespread access to medical care and expand the scope of preventive measures, which should ultimately lead to a reduction in the prevalence of osteoporotic fractures and an improvement in the quality of life.
Alendronate Canon (10mg, 70mg)
Adverse reactions from the upper gastrointestinal tract
Alendronic acid may cause local irritation of the mucous membrane of the upper gastrointestinal tract. In this regard, while taking alendronic acid, caution should be exercised when prescribing the drug to patients with diseases of the upper gastrointestinal tract, for example, with dysphagia, esophageal disease, gastritis, duodenitis, ulcers, serious gastrointestinal disease suffered in the previous 12 months, for example, with peptic ulcer, as well as with active gastrointestinal bleeding, surgery on the upper gastrointestinal tract, with the exception of pyloroplasty. For patients diagnosed with Barrett's esophagus, the question of prescribing alendronic acid should be decided individually based on an assessment of the ratio of expected benefit to possible risk.
When treating with alendronic acid, there are cases of adverse reactions from the esophagus (esophagitis, ulcer or erosion of the esophagus), sometimes severe and requiring hospital treatment, and in rare cases, complicated by the formation of a stricture. Therefore, physicians should pay special attention to any signs or symptoms indicating possible esophageal problems, and patients should be advised to stop taking alendronic acid and seek medical attention if symptoms of esophageal irritation, such as dysphagia, pain with swallowing, occur. or pain behind the sternum, the appearance or worsening of heartburn (see section "Side effects").
The risk of severe esophageal adverse events is higher in those patients who do not follow the drug dosage recommendations and/or continue to take the drug when symptoms of esophageal irritation occur. It is especially important to give the patient recommendations for taking the drug so that he understands that the risk of developing esophageal damage increases if these recommendations are not followed (see section “Dosage and Administration”).
Although no increased risk was observed in extended clinical studies of alendronic acid, rare cases of gastric and duodenal ulcers, sometimes severe and complicated, have been reported in post-marketing reports (see section "Side Effects").
Osteonecrosis of the jaw
Cases of osteonecrosis of the jaw, mainly due to previous tooth extraction and/or local infection (including osteomyelitis), have been reported in cancer patients treated with intravenous bisphosphonates. Many of the patients also received chemotherapy and corticosteroids. There are also known cases of osteonecrosis of the jaw in patients with osteoporosis who took oral bisphosphonates.
When assessing an individual's risk of developing necrosis of the jaw, the following risk factors should be considered:
-bisphosphonate activity (highest for zoledronic acid), route of administration (see above) and total dose;
-cancer, chemotherapy, radiotherapy, glucocorticosteroids, smoking;
-history of dental disease, poor oral hygiene, periodontal disease, invasive dental procedures and ill-fitting dentures.
Before starting therapy with oral bisphosphonates, patients with poor dental status are recommended to have a dental examination and preventive treatment measures.
During a course of bisphosphonates, such patients are advised to avoid invasive dental procedures if possible. If a patient develops osteonecrosis of the jaw while on bisphosphonate therapy, dental surgery may worsen the condition. It is unknown whether stopping bisphosphonates reduces the risk of osteonecrosis of the jaw in patients requiring dental procedures. In each case, the decision must be made by the attending physician based on an assessment of the ratio of the expected benefit to the possible risk for a particular patient.
During bisphosphonate therapy, patients should be educated about the importance of good oral hygiene, oral health screenings, and to report any oral symptoms such as tooth mobility, pain, or swelling.
Osteonecrosis of the external auditory canal
Cases of osteonecrosis of the external auditory canal have been reported while taking bisphosphonates, mainly during long-term therapy. Possible risk factors for osteonecrosis of the external auditory canal include steroid use and chemotherapy and/or local risk factors such as infection or trauma. The possibility of osteonecrosis of the external auditory canal should be considered in patients taking bisphosphonates who have hearing problems such as pain, discharge, or chronic infection.
Musculoskeletal pain
There are known cases of pain in bones, joints and/or muscles during a course of bisphosphonates. During post-registration use, in rare cases, these symptoms were severe and/or led to disability (see section “Side Effects”). The time of onset of symptoms varied from one day to several months after the start of treatment. In most patients, symptoms resolved after cessation of treatment. In some of them, symptoms reappeared when they resumed taking the same drug or a different bisphosphonate.
Atypical hip fractures
Cases of atypical subtrochanteric or diaphyseal femoral fractures have been reported during treatment with bisphosphonates, mainly in patients receiving long-term therapy for osteoporosis. These transverse or oblique fractures can occur along the entire length of the femur from the lesser trochanter of the femur to the supracondylar extension. These fractures occur after little or no trauma, and some patients experience severe pain in the hip or groin area, often accompanied by radiographic symptoms of stress fractures, weeks or months before the full picture of a hip fracture appears. Fractures are often bilateral, so the other (contralateral) hip should be evaluated in patients with a hip fracture taking bisphosphonates. It is known that these fractures heal poorly. If an atypical hip fracture is suspected, discontinuation of bisphosphonate therapy should be considered until an individual assessment of the expected benefit versus possible risk is made.
Patients should be advised to report any pain in the hip or groin area during bisphosphonate therapy. All patients admitted with such complaints should be examined for an incomplete femoral fracture.
Skin reactions
During postmarketing use, there have been rare reports of severe skin reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis.
Skipping a drug dose
Patients should be warned that if they accidentally miss taking Alendronate Canon once a week, they should take 1 tablet in the morning of the next day after they remember. You should not take two tablets on the same day, but subsequently you must return to taking the drug once a week on the day of the week that was chosen at the beginning of treatment.
Kidney failure
The drug Alendronate Canon is contraindicated in patients with renal failure with creatinine clearance less than 35 ml/min (see section "Contraindications").
Bone metabolism and mineral metabolism
Causes of osteoporosis other than estrogen deficiency and age should be considered.
In the presence of hypocalcemia, the concentration of calcium in the blood must be normalized before starting treatment with alendronic acid (see section “Contraindications”). Other disorders of mineral metabolism (eg, vitamin D deficiency and hypoparathyroidism) should also be effectively treated before initiating alendronic acid therapy. In patients with these disorders, during therapy with Alendronate Canon, it is necessary to monitor the concentration of calcium in the blood serum and symptoms of hypocalcemia.
Because alendronic acid increases bone mineral content, decreased serum calcium and phosphate concentrations may occur, especially in patients taking corticosteroids in whom calcium absorption may be reduced. Usually this decrease is small and asymptomatic. However, there are rare cases of symptomatic hypocalcemia, which sometimes reached a severe degree and developed in patients with a corresponding predisposition (for example, hypoparathyroidism, vitamin D deficiency and calcium malabsorption) (see section "Side effects").
Excipients
This medicinal product contains lactose. Patients with rare hereditary diseases of galactose intolerance, lactase deficiency or glucose-galactose malabsorption should not take this drug.
Impact on the ability to drive vehicles and machinery
No studies have been conducted to assess the effect on the ability to drive vehicles or operate machinery. However, some adverse reactions observed with alendronic acid may affect the ability of some patients to drive vehicles or operate machinery. Individual reactions to the drug Alendronate Canon may differ (see section “Side effects”).