Many consumers will say that probiotics and beneficial bacteria complexes are quite expensive. Doctors prescribe them for almost every illness. Drugs are needed to restore microflora after taking antibiotics, with decreased immunity, during fungal diseases, and so on. Patients try to find inexpensive substitutes for prescribed drugs. Today’s article will tell you whether there is a cheap analogue of Vagilak. You will learn how to use this drug and become familiar with some substitutes.
"Vagilak" (capsules): official instructions
This medication is available in capsules for oral use. The composition includes several varieties of lactobacilli. They contain more than a trillion microorganisms. Additional components are starch, dextrose, magnesium stearate, microcrystalline cellulose.
The drug "Vagilak" has analogues. The price and instructions for using such products will be presented to your attention below. The original probiotic costs about 900 rubles. For this amount you will receive 15 capsules per package. They are used to restore vaginal microflora after it has been disrupted. The medication is also used for preventive purposes. The instructions indicate that the drug is over-the-counter. This means that it can be purchased without a doctor’s prescription at any pharmacy. The abstract also says that Vagilak is a dietary supplement; it has not become a medicine. Despite the fact that the capsules contain beneficial bacteria, the medication can be stored at room temperature no higher than 25 degrees.
Bacterial vaginosis is a common vaginal infection that occurs in 20% of women of reproductive age [1]. Despite the fact that bacterial vaginosis occurs mainly in a mild form, and in some cases occurs without symptoms, it can lead to endometritis and other inflammatory diseases of the pelvic organs [2, 3]. In the presence of bacterial vaginosis, pregnancy complications such as spontaneous abortion, chorioamnionitis, premature rupture of amniotic fluid, premature birth and postpartum endometritis can occur [4, 5]. In women in the IVF program, bacterial vaginosis reduces the implantation rate and can also cause intrapartum fetal death [6, 7]. The main pathological process characteristic of this disease is the excessive growth of anaerobic microorganisms such as Gardnerella vaginalis, Mycoplasma hominis
and
Mobyluncus
. This leads to an increase in pH in the vagina and the appearance of discharge with an unpleasant odor. The normal microflora of the vagina consists mainly of lactobacilli, which prevent the spread of the above pathogens. Lactobacilli produce lactic acid, which acidifies the vaginal contents [8], as well as hydrogen peroxide, which has a toxic effect on other microorganisms [9, 10].
In the treatment of bacterial vaginosis, metronidazole is most often used, which does not affect lactobacilli, but has a negative effect on anaerobic microorganisms. Clindamycin is also widely used [11, 12]. Although these drugs are considered safe, they may cause unwanted side effects. When using metronidazole, gastrointestinal disorders such as nausea and vomiting may occur, and less commonly, a metallic taste in the mouth, paresthesia and leukopenia may occur [13]. The most common adverse events with clindamycin include rash and gastrointestinal problems such as anorexia, abdominal pain, nausea, vomiting and diarrhea. The latter can also be a symptom of pseudomembranous enterocolitis. Less common adverse events include neutropenia, leukopenia, jaundice, and skeletal muscle paralysis [14]. Both drugs can be taken orally as well as vaginally. In 10-15% of women, initial antimicrobial therapy is not effective. Among patients who respond well to treatment, 69% develop relapses of bacterial vaginosis within 1 year, which leads to the need for repeated antibiotics [15].
The high rate of relapses, despite antimicrobial therapy, led to the search for alternative treatment methods that could be prescribed in conjunction with already used drugs or as monotherapy. The predominance of lactobacilli in the normal vaginal microflora and their absence in bacterial vaginosis has stimulated the use of various types of lactobacilli both orally and vaginally in order to restore the vaginal microflora [16]. These medications are also known as probiotics and are live microorganisms that, when taken in the right dosage, can improve vaginal health [17]. It is also known that some strains of lactobacilli can spread into the vagina after oral or vaginal administration [18]. In addition, lactobacilli can be used for a long time without the risk of developing dangerous adverse events, which makes them an attractive alternative to antimicrobial therapy, especially given the risk of relapse [19, 20].
The purpose of this study was to evaluate the effectiveness of the oral probiotic Vagilak (Rijeka, Croatia) compared with placebo in women with bacterial vaginosis who do not suffer from any other diseases. Our hypothesis was that the percentage of restoration of normal vaginal microflora would be significantly higher in women taking probiotics compared to those taking placebo.
Material and methods
The study was planned as a randomized, double-blind, multicenter, placebo-controlled study. The study protocol was approved by the Ethics Committee of the University of Zagreb Medical School. Study participants were recruited from 55 primary care obstetric and gynecological care providers in central and northwestern Croatia. The study included women over the age of 18 years who were diagnosed with a vaginal infection (bacterial vaginosis, candidiasis, trichomoniasis, or a combination of these). Exclusion criteria include pregnancy, breastfeeding, menstruation, and the woman's unwillingness to give informed consent to participate in the study.
The initial (initial) diagnosis of bacterial vaginosis was made taking into account the Amsel criteria or the Nugent index. In routine clinical practice in Croatia, bacterial vaginosis is most often diagnosed based on the Amsel criteria [21], which include the presence of a thick grayish vaginal discharge, a pH level >4.5, the appearance of a special odor after adding potassium hydroxide to the discharge and the presence of so-called “ key cells" in a wet saline preparation. To confirm the diagnosis of bacterial vaginosis, at least three of these four criteria must be present.
However, some specialists more often use a method based on the Nugent index [22]. In such cases, vaginal smears are Gram-stained and scored using a 10-point scale, counting the total number of Lactobacilli, such as G. vaginalis
and
Mobiluncus
available in the field of view during microscopic examination. The initial diagnosis of vulvovaginal candidiasis and trichomoniasis was made using conventional diagnostic tests. If one of the above-mentioned diagnoses was made during the initial screening examination, additional smears were taken to confirm the diagnosis at the central laboratory.
After obtaining informed consent, all patients included in the study were divided into two groups, one of which took a placebo and the other took a probiotic. The randomization process was carried out using a computerized randomization list, which assigned each study participant to either group A or group B. Randomization lists were created using the software and methodology described by M. Saghaei [23]. Then the study participants took the necessary drug - 2 capsules of Vagilac (each containing >109 CFU of Lactobacillus rhamnosus
GR-1 and
L. reuteri
RC-14) or 2 identical placebo capsules per day for 6 weeks.
At 6 and 12 weeks after the start of the study, all study participants underwent two additional gynecological examinations. In patients with bacterial vaginosis, vaginal smears were assessed using the procedure that was used during the initial selection of study participants. If vulvovaginal candidiasis was present, assessment was performed using vaginal pH and 10% KOH wet mount testing. All patients with trichomoniasis took a single dose of 2 g of metronidazole orally. In addition, all study participants had vaginal smears examined by a clinical cytologist, and the process of culturing Lactobacillus
on agar plates.
Cultivation of Lactobacillus
was carried out using the method [24].
After treating individual cells in sterile phosphate-buffered saline (PBS), the solutions were plated on agar plates with or without tetracycline (50 μg/ml). After incubation, the plates were analyzed visually, Gram stained, and also examined for the presence of a catalase reaction. After this procedure, pale yellow, tetracycline-resistant, gram-positive bacterial colonies without catalase reaction were classified as Lactobacillus
spp.
The primary outcome of the study was the rate of restoration of normal vaginal microflora at the end of the 6-week follow-up period. Moreover, we monitored the recurrence rate of bacterial vaginosis after 6 weeks during which study participants were not taking the study drug. The sample size was calculated such that significant statistical significance could be achieved ( β
≥0.90) with a relatively low probability of type-1 errors (
α
<0.05). NCSS PASS software [25] was used with the null hypothesis of achieving a 40% cure rate in the placebo group compared with a 65% cure rate in the probiotic group. The null hypothesis was based on previous experience with the probiotic preparation. This assumption resulted in a sample size of 120 participants in each group. However, 544 women were ultimately included in the study.
All statistical analyzes were performed using Statistica software (version 9, , Tulsa, OK, USA). Percentages and proportions were calculated for categorical data, and medians and ranges were calculated for continuous data. Differences in continuous variables were analyzed using the Student's t test (with normal distribution) or the Mann-Whitney U test (with non-normal distribution). Normality of distribution was checked using the Shapiro-Wilk test. For categorical variables, differences were analyzed using the &khgr;2 test. All obtained p
are two-sided.
p
value <0.05 indicated statistical significance.
results
Over a 12-month period (March 2008–March 2009), 544 women were included in the study. Detailed information about inclusion in the study is presented in the figure.
.
Figure 1. Study inclusion flowchart. Study participants were randomly divided into two groups: a placebo group ( n
=149; 27.39%) and a probiotic group (
n
=395; 72.61%).
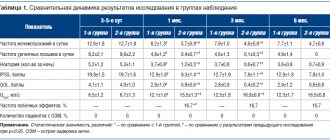
After recruiting the minimum required number of patients in the placebo group, the most effective way to achieve statistical significance without withholding treatment from patients with bacterial vaginosis was to increase the number of subjects in the probiotic group. At the initial visit, patients in the two groups had similar demographic parameters: age, number of children, number of sexual partners, age of first sexual intercourse, bad habits (smoking and drinking alcohol), marital status and contraceptive method used (Table 1)
.
In addition, the results of cytological smears were similar in patients of both groups (
p
= 0.149)
(Table 2)
.
The mean follow-up period was 44.16 days, i.e. approximately 6 weeks and 2 days, and was similar in both groups ( p
=0.733).
During the follow-up period, study participants took either placebo capsules or probiotic capsules twice daily, as described above. Patient adherence to treatment was similar in both groups (97.64% in the placebo group and 91.67% in the probiotic group; p
= 0.128).
After the above-mentioned follow-up period, restoration of normal vaginal microflora was observed in 40 (26.85%) study participants in the placebo group and in 243 (61.52%) in the probiotic group. Differences between groups are statistically significant ( p
<0.001). During this period, the number in need of treatment (NNT) was 2.9 with a relative risk reduction (RRR) of 47.4%.
After 6 weeks of observation, the normal state of vaginal microflora remained in more than half (51.14%) of women in the probiotic group and only in ⅕ (20.81%) of patients in the placebo group ( p
<0.001).
In this later period, the NNL rate was 3.3, while the TSR rate was 38.3%. Detailed information about the results of cytological smears is given in Table.
3 .
All study participants with negative results at the second visit (12 weeks) subsequently received the necessary treatment after their participation in the study was completed.
Additional cultivation on agar plates was carried out for the purpose of recovery and identification of lactobacilli in vaginal smears. Increased concentrations (>105 CFU/ml) of lactobacilli were observed in 81.5% of women taking the probiotic, compared with 28.9% of women taking placebo. Thus, the restoration of normal (balanced) vaginal microflora was accompanied by the presence of a large amount ( p
<0.001) lactobacilli in vaginal smears during the last two visits.
None of the demographic indicators given in table. 1
, did not have a significant impact on the results - the number of patients with restored normal vaginal microflora 6 and 12 weeks after measuring the initial indicators.
However, borderline significance ( p
=0.082) was found when comparing the number of children born. Women who gave birth to 3 or more children were less likely to experience restoration of normal vaginal microflora compared to women who gave birth to 2 children, 1 child, or nulliparous women. These results are apparently not due to the older age of women who gave birth to more children (40.1 years for women with 3 children or more vs. 29.9 years for women with 2 children or fewer), since age did not influence the results , as discussed above. One explanation may be the fact that the occurrence and recurrence of bacterial vaginosis (and other infections of the female genital tract) are more common in women who have given birth to more children, as has already been proven by other researchers [26]. However, a larger study with a longer follow-up period is needed to confirm or reject this hypothesis.
Discussion
Bacterial vaginosis is a condition associated with low levels of Lactobacillus
spp. in the vagina [27]. Although the source of vaginosis (re-infection or relapse) has not been fully determined, it is believed that lactobacilli, through the production of lactic acid, slow down the growth of other microorganisms, which leads to inhibition of their excessive growth [20, 28]. The same mechanism is responsible for maintaining low pH levels. The most commonly used strains of lactobacilli in the treatment process are a combination
L. rhamnosus
GR-1 and
Lactobacillus fermentum
in vitro
studies demonstrated the ability to adhere to vaginal epithelial cells [29]. Because of this, they can spread into the vagina after oral administration of drugs [13].
Studies examining the effectiveness of probiotics in the treatment of bacterial vaginosis are rare. K. Anukam et al. [24] conducted a randomized, controlled, double-blind study that confirmed the positive results of the combined use of metronidazole and an oral probiotic compared with placebo in the treatment of bacterial vaginosis. After a 30-day period, 88% of patients taking probiotics had no signs of bacterial vaginosis, compared with 40% of those in the placebo group ( p
<0.001). The same authors conducted another randomized clinical trial examining the comparative effectiveness of intravaginal probiotics used in conjunction with metronidazole gel for the treatment of bacterial vaginosis [30]. During this study, similar results were obtained. Similar results were published by R. Martinez et al. [31] (combined use of tinidazole and probiotics compared with tinidazole and placebo) and W. Ya et al. [28], who recently conducted a randomized, double-blind, placebo-controlled trial examining the effectiveness of an intravaginal probiotic for the prevention of recurrent bacterial vaginosis.
Despite a number of shortcomings regarding the number of participants, inclusion criteria or methods used during follow-up, the above-mentioned studies provide significant evidence of the effectiveness of Lactobacilli
in the treatment of bacterial vaginosis.
Taking this fact into account, we planned to include a fairly large number of patients in our study. In addition, we carefully developed a diagnostic procedure both at baseline and during follow-up, and closely monitored patient compliance with treatment. Using this study design, we were able to study the condition of a sufficiently large number of patients during a specific period and avoid errors typical of single-center studies [32]. Finally, by recruiting study participants from the general population and testing treatment effectiveness in a variety of clinical situations, we have provided an experimental setting that is more representative of the future. The main limitation of the study was the relatively short follow-up period of 6–12 weeks, but we thereby avoided loss of contact with study participants. In addition, DNA testing for Lactobacillus
GR-1 and RC-14 would have facilitated the identification of strains in vaginal swabs taken during the follow-up period, but this was not possible during the study period.
Our results confirm the effectiveness of an oral probiotic as previously demonstrated. These results also demonstrate an association between the number of women with increasing numbers of Lactobacillus
spp. after treatment and the number of patients with restoration of balanced vaginal microflora, which was the main outcome of the study. In our opinion, the most important result of probiotic therapy in general (both intravaginal and oral) is the ability to reduce the concentration or completely eliminate metronidazole in the treatment of bacterial vaginosis. The intravaginal probiotic has already been proven to be more effective than metronidazole in the treatment of this disease [33], and our results confirm the similar effectiveness of the oral probiotic Vagilac. In our opinion, oral probiotics are an alternative treatment for common gynecological diseases, devoid of adverse effects, which makes it possible to combine them with both metronidazole and probiotics in vaginal capsules. We agree with W. Ya et al. [28], who believe that the potential effectiveness of probiotics compared to antibiotics should be confirmed in further randomized clinical trials.
Conclusion
Oral probiotics, such as Vagilak, are an alternative treatment for bacterial vaginosis with high efficacy and safety, which allows it to be combined with both metronidazole and intravaginal probiotics.
Cheap analogue of "Vagilak"
As you can already find out, the drug is quite expensive. Therefore, women often try to replace it with cheap products. Doctors strongly do not recommend doing this, because the medication is prescribed taking into account all the characteristics of the patient’s body. But let’s try to find out what a cheap analogue of Vagilak is.
- Capsules "Ecofemin Florovag". Available in 20 capsules. This drug costs about 800 rubles. This is somewhat cheaper than Vagilak. In addition, you purchase more capsules. The medication contains lactobacilli, lactic acid organisms and additional substances.
- Vaginal tablets "Lactozhinal". This drug will cost you about 700 rubles for 14 pieces. The product, unlike the original one, is inserted into the vagina. The composition contains lactobacilli of different types, anaerobic non-spore-forming microorganisms.
- Vaginorm product. Available in the form of vaginal tablets of 6 pieces. The drug costs approximately 600 rubles. The active substance is ascorbic acid, which reduces the pH of the vagina.
- Capsules "Lactonorm". The main component of this product is acidophilic live lactobacilli. The drug costs about 500 rubles. In the package you will find 14 vaginal capsules.
- The drug "Acilact". Vaginal suppositories cost about 150 rubles for 10 pieces. Contains acidophilic lactobacilli.
- Suppositories "Bifidumbacterin". The cost of this medication is about 100 rubles for 10 pieces. The active substance is bifidobacteria. The drug can be used rectally or vaginally.
Vagilak
Available in the form:
- Vaginal suppositories with the main active ingredients – Lactobacillus rhamnosus and Lactobacillus reuteri.
- Tablets for oral use with the same main active ingredients.
- Liquid soap for intimate hygiene based on lactic acid with extracts of medicinal calendula and chamomile.
- Moisturizing gel for intimate hygiene based on lactic acid.
The healing properties and effects of each form of the drug are distinctive:
- Vaginal capsules help normalize the vaginal microflora
, prevent recurrences of bacterial candidiasis, and eliminate pathogenic microbes. - Tablets for oral use revive the vaginal microflora, activate the protective and regenerative processes of the mucous membrane, and maintain an impeccable pH level.
- Soap maintains the traditional pH of the genital organs
, has an anti-inflammatory effect, and eliminates feelings of discomfort and dryness in the intimate area. - The gel moisturizes the vaginal mucosa, eliminates burning sensation, speeds up the regeneration process, and also maintains the necessary pH level in the intimate area, maintaining the balance of microflora.
Vagilak suppositories and tablets are indicated for the following pathologies:
- Vaginal dysbiosis.
- Chronic and acute inflammation of the female genital organs .
- Together with antibacterial drugs and in the treatment of sexually transmitted diseases (chlamydia, etc.).
- Preparation of the vagina before childbirth, gynecological procedures or surgery.
- While using contraceptives, such as spermicides, intrauterine devices or COCs.
- Hormonal or age-related colpitis.
Gel Vagilak is indicated:
- For complex treatment of vaginal dysbiosis (for example, use gel or soap together with capsules).
- As an additional remedy for inflammatory diseases of the female genital organs
. - For vaginal dryness of various etiologies.
- While taking oral contraceptives.
- After taking antifungal and antibacterial agents to improve microflora.
- For daily intimate hygiene.
- As a prophylactic agent to prevent any injuries when performing complex gynecological interventions.
Soap is used for daily genital
women and girls (from 10 years old). It is recommended for use during menstruation, after abortion, childbirth, examinations and actions through the vagina and so on.
Vagilak can be used during pregnancy and lactation.
Side effects
: rarely hyperemia of the vaginal mucosa.
Contraindications: acute inflammation and/or erosive lesions of the vaginal mucosa, intolerance to the components of the product.
Also on the topic: Causes, symptoms and treatment of colpitis
Mode of application
A cheap analogue of Vagilak, like the original medicine, is prescribed for disorders of the vaginal microflora. Indications for use will be the following situations:
- dysbiosis, bacterial vaginosis;
- long-term use of antibiotics and chemotherapy treatment;
- inflammatory and infectious diseases of the genital area;
- decreased immunity and exacerbation of chronic diseases (human papillomavirus infection, herpes);
- use of spermicides and installation of intrauterine devices;
- preparation for various gynecological manipulations (childbirth, curettage, hysteroscopy).
Depending on the type of drug, an individual method of its use is selected. Oral medications are used 1 to 2 times a day. Suppositories are usually administered before bedtime, but sometimes additional morning use is required. The course ranges from 7 days to several months.
Contraindications and unforeseen situations
To avoid negative consequences and side reactions, you should not look for a cheap analogue of Vagilak on your own. If necessary, consult your doctor first. All medications described above are prohibited for use in case of hypersensitivity. Some vaginal suppositories are not used for thrush in the acute stage. Depending on the composition of the medication, it may be prohibited for use during pregnancy and lactation.
Most sources do not describe adverse reactions. But patients still report them. Vaginal suppositories often cause burning and itching. Reviews from women say that these unpleasant symptoms go away on their own after a few days of use. Also, some prevailing opinions say that oral probiotics cause abdominal discomfort, increase gas production and provoke nausea.