Mitral valve insufficiency - classification and causes
Mitral valve insufficiency is caused by a violation of the closure function as a result of deformation of the valves, often of a fibrous nature, as well as subvalvular structures and disruption of the integrity of various elements of the valve or dilatation of the fibrous ring, which ultimately leads to the return of part of the blood volume during systole from left ventricle to left atrium. This leads to a decrease in minute blood circulation and the development of pulmonary hypertension. Isolated mitral valve insufficiency is a very rare occurrence, occurring in approximately only 2% of patients. Mostly, failure is combined with mitral valve stenosis and/or aortic heart defects.
Classification and reasons
A distinction is made between functional deficiency (also called relative) or organic.
Functional mitral valve insufficiency can develop as a result of:
- Mitralization (expansion of the volume of the cavity of the left ventricle) as a result of myocardial diseases, which lead to the formation of hemodynamic overload of this part of the heart muscle.
- Acceleration of blood flow as a result of vegetative dystonia and a change in tone in the papillary muscles.
Functional mitral valve insufficiency is not a heart defect. However, hemodynamic disturbances fully correspond to the nature of organic failure. Organic mitral valve insufficiency occurs as a result of anatomical damage to the tendons of the valve filaments or the valve itself. According to the nature of the process, acute and chronic mitral insufficiency are distinguished.
General information
Acquired heart defects include defects of the mitral, aortic and tricuspid valves. rheumatism was considered a factor in the development of heart valve defects , and in recent years - infective endocarditis and degenerative changes in the valves.
The most common defects are the aortic valve (they account for 43%) and the mitral valve. The mitral valve is located between the left atrium and the left ventricle, separating them. Blood enters the left ventricle through the mitral valve from the left atrium. From the left ventricle it enters the aorta - this is the systemic circulation. The condition of the valve determines the amount of blood that will enter the large circle to supply the entire body. Mitral defects disrupt hemodynamics and affect cardiac function. They are manifested by stenosis (narrowing) or insufficiency of the mitral valve. The narrowing of the mitral orifice makes it difficult for blood to flow from the atrium into the ventricle. Mitral insufficiency is characterized by a violation of the closing function of the valve (it does not close completely), which causes the return (regurgitation) of part of the blood from the ventricle during its contraction into the left atrium.
The mitral valve apparatus consists of two leaflets, the mitral ring, papillary muscles and chordae (tendon). The valve opens towards the ventricles, and its eversion into the left atrium is prevented by tendons attached to the papillary muscles. Complete closure and brief symmetrical overlap of both leaflets prevent backflow of blood into the atrium. With mitral insufficiency due to changes in the valves or subvalvular apparatus (chordae, papillary muscles), normal hemodynamics are disrupted.
Hemodynamic disturbances inside the heart lead to a decrease in minute volume of blood circulation and at the same time an increase in pressure in the pulmonary artery ( pulmonary hypertension ). Over time, the disease progresses and patients develop heart failure , which is first eliminated conservatively, and subsequently many require surgical correction of the defect.
It is important to determine the degree of progression and timely referral of patients to a cardiac surgeon to resolve the issue of surgical treatment. Patients with asymptomatic forms of defects are especially wary, since their prognosis is often unfavorable.
What it is
A defect of the mitral valve with reverse blood flow (regurgitation) from the left ventricle into the atrium as a result of incomplete closure of the valves is called mitral regurgitation. In its independent form, the acquired disease is rare and for a long time is benign in nature.
But as part of combined and concomitant defects, it is detected in half of all cases of cardiac defects and quickly leads to serious complications. Normally, the left ventricle ejects its contents into the aorta during systole, which branches, forming a systemic circulation. In this way, nutrients and oxygen are transferred to organs, including the myocardium. Under pressure, the butterfly valve closes and does not allow reverse movement. If there is a hole during contraction, regurgitation occurs, and some of the blood returns, stretching the left atrium. As the condition progresses, there is a steady increase in the volume of the heart cavities, increased pressure, and congestion in the blood vessels of the lungs.
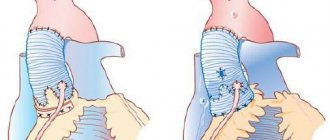
The mechanism of defect formation can be seen in the figure:
Pathogenesis
With rheumatism, all layers of the heart are involved in the process - the endocardium with valves, the myocardium, the vascular system and the pericardium. The rheumatic process causes deformation of the valve, soldering of them along the commissures, shortening of the tendon chords - all this limits the mobility of the valves. Degenerative valve changes occur in Marfan and Ehlers-Danlos . These include thickening and stretching of the valve due to collagen breakdown. At the same time, the resulting fibrous tissue causes thickening of the valves - they become dense, and shortening causes a limitation in the mobility of the valves. With this pathology, defects of the leaflets are formed along the edges, the edges are twisted, wrinkled and the leaflets are shortened, not closing during systole. Changes in the subvalvular apparatus also play a role—cicatricial shortening of the chordae and sclerosis of the papillary muscles. Subsequently, calcium is deposited in the valves, which sharply limits mobility. All these changes cause changes in intracardiac hemodynamics.
Mitral valve disease in the form of mitral insufficiency has the following hemodynamic features:
- The valves do not close completely, causing blood to return to the left atrium. The return of blood overloads the left atrium.
- The crowded left atrium begins to enlarge, and the left ventricle hypertrophies.
- The wave of regurgitation increases over time, and valvular insufficiency increases. Pulmonary hypertension develops - this is due to the fact that overload of the left atrium creates stagnation in the pulmonary circulation.
- In some cases, pulmonary edema . The contractility of the left ventricle decreases and its pumping function is weakened. Chronic heart failure develops .
The amount of backflow of blood into the atrium determines the severity of mitral regurgitation. Over time, volume overload of the left ventricle develops and the total stroke volume of the left ventricle can increase 3 times. Outflow into the aorta is normal until left ventricular failure develops. Enlargement of the left sections stretches the valve ring and contributes to the progression of insufficiency. The additional volume of blood in the atrium stretches its walls, they lose tone and at the same time the pressure in the atrium cavity and in the pulmonary veins increases (venous pulmonary hypertension develops).
Publications in the media
Mitral regurgitation is the inability of the left atrioventricular valve to prevent the reverse flow of blood from the left ventricle into the left atrium during ventricular systole.
Frequency. Mitral insufficiency is recorded in 50% of patients with various heart defects. In its pure form, mitral regurgitation is a rare disease. It is observed much more often in children than in adults. Often combined with mitral stenosis or aortic valve defects. Congenital mitral valve insufficiency accounts for 0.6% of all congenital heart diseases. In 65% of cases it is combined with septal defects, coarctation of the aorta or patent ductus arteriosus. About 5–6% of healthy women have some degree of mitral regurgitation detected by echocardiography.
Etiology • Rheumatism • Isolated mitral valve prolapse (myxomatous degeneration, Barlow's disease) • Idiopathic rupture of chordae (14–23% of cases of severe insufficiency, of which degenerative changes of the chordae are detected in 73–93% of cases) • Ischemic dysfunction or rupture of papillary muscles (5 % cases of transmural MI, more often with lower MI) • Infective endocarditis • Annular calcification of the elderly • Connective tissue diseases (Marfan and Ehlers-Danlos syndrome) • Complication of mitral valvuloplasty • Relative failure due to dilatation or submitral aneurysm of the left ventricle • Congenital forms of failure (e.g. due to splitting of the anterior leaflet of the mitral valve with a fully open AV canal).
Pathophysiology • Hemodynamics in acute regurgitation are significantly different from those in the chronic course of the disease, when compensatory hypertrophy and dilatation of the left ventricle, the degree of which depends on the severity of mitral regurgitation, maintain cardiac output, sometimes for many years • In acute mitral regurgitation (for example, due to rupture of the papillary muscle or chordae) the left ventricle does not have time to adapt to a sharp increase in preload. As a result of this, and also due to the low compliance of the normal left atrium, acute left ventricular failure occurs, leading to pulmonary edema and arterial hypotension • With chronically existing regurgitation, due to an increase in the volume load of the left atrium, its hypertrophy and dilation occurs, more pronounced than with mitral stenosis, leading to chronic stagnation in the pulmonary circulation • Often, with dilatation of the left atrium, paroxysmal or permanent form of atrial fibrillation occurs, as well as thrombosis of the left atrium.
Clinical picture and diagnosis . • During chronic mitral regurgitation, three periods are conventionally distinguished: compensation, pulmonary venous hypertension and right ventricular failure. • Complaints •• During the compensation period, an asymptomatic course can be observed for several years •• When clinical symptoms appear in patients, the most common complaints are shortness of breath (98%), fatigue (87%), hemoptysis (15%) •• With severe regurgitation there are symptoms of compression of the recurrent laryngeal nerve by the enlarged left atrium (the most common of them is Ortner's syndrome - hoarseness of voice), and during the period of right ventricular failure - by the pulmonary trunk •• In patients in the third stage - symptoms of stagnation in the systemic circulation (edema, enlarged liver, Plesch's sign, swelling of the jugular veins).
• Peripheral symptoms are due to small output syndrome - see Aortic valve insufficiency. • Valve symptoms •• Mesosystolic click occurs with mitral valve prolapse, separation of chords or papillary muscle •• Weakening of the first tone •• Systolic murmur over the apex of various timbres, carried out to Botkin’s point and the left axillary region; its intensity depends on the volume of regurgitation •• The most specific sign of a mitral regurgitation murmur is intensification or appearance during tests that reduce the volume of the left ventricle (Valsalva maneuver, orthostatic test), or in a clinostatic position when turning to the left side due to the closer location of the apex of the heart to the chest •• Systolic flutter over the apical region - with high velocity (usually fine jet) regurgitation •• Coombs murmur occurs due to relative stenosis of the mitral valve due to the increased volume of blood expelled from the left atrium.
• Symptoms associated with enlargement of the chambers of the heart • Increase in the boundaries of relative dullness to the left, up and to the right (with dilatation of the right sections) • Popov's symptom - different degrees of filling of the pulse in the radial arteries. • Symptoms of the underlying disease (rheumatism, Marfan syndrome, cardiomyopathy).
Special studies • ECG •• Signs of hypertrophy and overload of the left parts of the heart, primarily the left atrium, and in the third stage of the disease and the right parts of the heart •• Supraventricular tachyarrhythmias (atrial fibrillation and flutter, supraventricular extrasystole and tachycardia).
• X-ray of the chest organs •• Pronounced signs of pulmonary venous hypertension • Bulging of the arch of the left atrium and deviation of the contrasted esophagus along an arc of a large radius •• Bulging of the arch of the left ventricle •• In the third stage of the disease - signs of pulmonary hypertension and bulging of the arches of the right parts of the heart •• With compression of the pulmonary trunk by the dilated left atrium - weakening of the pulmonary pattern on the left •• With fluoroscopy in direct projection - a symptom of a “rocker arm” between the arches of the left ventricle and the left atrium.
• Echocardiography •• Hypertrophy and dilatation of the left heart, especially the left atrium •• Visualization of a flapping leaflet when the chordae or papillary muscle is avulsed •• Increased end-diastolic index (EDI = [end-diastolic volume of the left ventricle] / [body surface area]), degree which has prognostic significance: an increase in CDI above 30 ml/m2 is associated with postoperative left ventricular failure, above 90 ml/m2 - with high postoperative mortality •• In Doppler mode - the flow of mitral regurgitation, the volume of which (estimated in the color mapping mode) corresponds to the degree severity of the defect •• In the third stage of the disease - hypertrophy and dilation of the right heart, increased systolic pressure in the right ventricle •• Transesophageal echocardiography is performed to detect thrombosis of the left atrium in the presence of atrial fibrillation.
• Catheterization of the left and right ventricles •• Increase in end-diastolic pressure of the left ventricle, pressure in the left atrium, systolic pressure in the right atrium, pulmonary artery wedge pressure •• “Ventriculization” of the pulmonary capillary pressure curve (increase in wave V more than 15 mm Hg. ).
• Left ventriculography •• The presence and degree of regurgitation is determined by the degree of filling of the left atrium in one contraction with contrast injected into the left ventricle •• Combined valvular lesions are also diagnosed.
TREATMENT • Drug therapy •• Chronic mitral regurgitation ••• Asymptomatic mild and moderate mitral regurgitation does not require treatment, and the advisability of taking vasodilators is controversial ••• Asymptomatic severe compensated regurgitation (CDI less than 50 ml/m2, absence of pulmonary hypertension and normal left ventricular systolic function , negative stress tests): invasive studies of hemodynamics at rest and during stress tests are indicated, as well as continuous use of ACE inhibitors •• Acute mitral regurgitation ••• Vasodilators (sodium nitroprusside or ACE inhibitors) and IV diuretics ••• Intra-aortic balloon counterpulsation ••• In case of infective endocarditis, absence of progression of sepsis or severe refractory heart failure, preoperative antibiotic therapy is permissible for no longer than 3 days ••• In case of severe failure due to MI without rupture of the papillary muscles - intra-aortic balloon counterpulsation, vasodilators.
• Surgical treatment •• Indications ••• Severe mitral regurgitation, asymptomatic or functional class II, if the end-diastolic size of the left ventricle is more than 40 mm or the CDI is more than 40 ml/m2, or the left ventricular ejection fraction is less than 55–60% (with mitral insufficiency, if the contractile function of the left ventricle is not impaired, the left ventricular ejection fraction should not be lower than 65%) ••• Severe mitral regurgitation, functional class III–IV ••• Severe asymptomatic mitral regurgitation in combination with severe pulmonary hypertension ••• Symptomatic moderate failure with preserved systolic function of the left ventricle in case of positive results of an invasive hemodynamic study •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life ••• End-stage circulatory failure ••• Negative test result with aminophylline and oxygen •• Methods of surgical treatment ••• In the absence of calcification and preserved mobility of the leaflets and valve apparatus, it is permissible to perform valve-sparing interventions (annuloplasty with the Alain Carpentier ring or using the “double hole” technique, excision of the flapping portion of the posterior leaflet, shortening of the chordae) ••• Despite the greater physiology of valve-sparing operations and relatively low incidence of thrombosis and infective endocarditis, due to the high frequency of relapses of the defect and the need for repeated operations, plastic interventions on the valves are actually performed only in cases of prolapse, ruptures of valve structures, relative valve insufficiency during dilatation of its ring and before a planned pregnancy ••• Mitral valve replacement valves under conditions of artificial circulation using biological prostheses are performed on children or before a planned pregnancy ••• In other cases, the affected valve is replaced with a mechanical prosthesis.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Atrioventricular block • Dystrophic changes in biological prostheses and the need for repeated prosthetics. Prognosis • Only 5–10% of patients with mitral valve prolapse progress to mitral regurgitation • 5-year survival rate is more than 80%, 10-year survival rate is more than 60% • With ischemic genesis of the defect, 5-year survival rate does not exceed 30% • Surgical treatment improves survival and exercise tolerance if the initial left ventricular ejection fraction is more than 35%, cardiac index is more than 1.5 ml/min/m2 • Surgical treatment is ineffective for secondary mitral regurgitation due to dilated cardiomyopathy and primary - for left ventricular ejection fraction less than 30% • Surgical treatment is often effective for ischemic cardiomyopathy when coronary artery bypass grafting and annuloplasty are performed simultaneously • Mortality with mitral valve replacement is 2-7%, with annuloplasty - 1-4% • 5-year survival rate averages 90%.
Synonyms • Left atrioventricular valve insufficiency • Mitral valve insufficiency
Abbreviations. EDI - end diastolic index.
ICD-10 • I05.1 Rheumatic mitral valve insufficiency • I05.2 Mitral stenosis with insufficiency • I34.0 Mitral (valve) insufficiency • Q23.3 Congenital mitral insufficiency
Classification
The following types of mitral insufficiency are distinguished:
- organic (primary, degenerative), which develops when the valves are initially damaged;
- functional (relative, secondary), which occurs in diseases of the left ventricle.
The most common cause of chronic organic failure is valve prolapse , which has a wide range of manifestations. In young people, myxomatous degeneration is detected, in which redundancy of the valves and chords develops (in Barlow syndrome ). fibroelastic insufficiency develops , leading to rupture of the chordae. of ischemia and heart failure appear early : decreased exercise tolerance, shortness of breath.
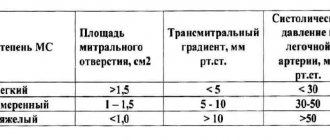
Depending on the volume of regurgitation, several degrees of mitral regurgitation are distinguished:
- I degree. Mitral regurgitation 1st degree, what is it? This is the initial degree of deficiency. Mitral valve insufficiency of the 1st degree is characterized by mild regurgitation. Its volume is less than 30 ml, and the area of the return flow hole is less than 0.20 cm2. Reverse blood flow occurs only at the valve.
- II degree. Mitral regurgitation of the 2nd degree is characterized by moderate regurgitation and reverse blood flow in the middle of the atrium. With this degree, the atrium is moderately dilated. At grade 2, the volume of regurgitation is 30-59 ml, the area of the regurgitation opening is 0.20-0.39 cm2.
- III degree. Mitral valve insufficiency of the 3rd degree is characterized by a regurgitation volume of more than 60 ml, and the area of the return flow hole is more than 0.40 cm2. At grade 3, the atrium is significantly expanded, and the jet reaches its posterior wall. This is a severe degree of deficiency.
By stages:
- Compensation stage.
- Stage of decompensation.
In the compensatory stage, increased preload and normal afterload facilitate left ventricular ejection, so effective stroke volume is observed. The compensatory phase continues for many years.
Prolonged volume overload ultimately leads to disruption of the contractile function of the left stomach and the stage of decompensation occurs.
Stages of NMC
The stage of the pathological process, along with the degree, plays an important role in the clinical picture.
Highlight:
- Stage 1 of uric acid deficiency corresponds to the complete absence of manifestations. Or they are so insignificant that they do not attract attention.
- Stage 2 (moderate) is determined by a more pronounced clinical picture. The patient suffers from shortness of breath at rest and with minimal physical activity, chest pain of unknown origin, and problems with rhythm. But the quality of life is still acceptable, which is why many do not go to the doctor. Especially smokers who attribute their condition to the consequences of consuming tobacco products.
- Stage 3 (severe) is determined by severe symptoms and a significant decrease in important indicators.
- Terminal stage 4 is almost always fatal, and recovery is impossible. Palliative care is provided to alleviate the condition and ensure a dignified death.
Mitral regurgitation of the 1st degree is the most favorable moment to begin treatment. Later, as the clinical picture becomes more complex, recovery is less likely.
Causes
Organic (primary) mitral valve insufficiency is associated with anatomical damage to the valve or the tendons that hold it. The reasons are:
- valve prolapse is a syndrome that stands on the border between normal and pathological (bending of the valves into the atrium, associated with the “weakness” of the connective tissue of the valves, so they prolapse, occurs mostly in women);
- degeneration of valve leaflets ( calcific disease , myxomatous degeneration of valve leaflets );
- rheumatic heart disease;
- infective endocarditis;
- congenital defects of the valves (splitting of the valves);
- connective tissue diseases ( scleroderma , rheumatoid arthritis , systemic lupus erythematosus );
- violation of the integrity of the mitral valve.
Rheumatic disease accounts for 14% of valve defects. The main causative agent of rheumatism is β-hemolytic streptococcus A. The main manifestation of rheumatism is carditis and valve damage ( valvulitis , the mitral valve is predominantly affected, less often the aortic valve).
Cardiac surgery, injection drug addiction, hemodialysis and long-term venous catheterization play an important role in infective endocarditis. The causative agents of this disease are Staphylococcus aureus and Enterococcus spp. due to the prevalence of diseases of the abdominal cavity and pelvic organs. In infective endocarditis, the mitral valve is most often affected.
Among non-inflammatory mitral regurgitation, dysplasia . For a long time it is asymptomatic, but as the degenerative process progresses, the weakened chords rupture and acute mitral regurgitation .
In connective tissue diseases, in particular rheumatoid arthritis , rheumatoid nodules appear in the myocardium, pericardium and endocardium at the base of the mitral and aortic valves. Subsequently, sclerosis , which causes the formation of valve insufficiency. There are also often inflammatory changes in the valves ( valvulitis ). It proceeds favorably, without causing significant deformation of the valves. But in some patients, valvulitis occurs with deformation of the valves and mitral insufficiency develops, which often requires surgical correction. Thus, rheumatoid valve damage serves as a background against which significant changes in the structure of the valves develop.
Functional tricuspid valve insufficiency is not a heart defect, but the hemodynamic disturbances with it are the same as with organic valve insufficiency. The causes of functional mitral valve insufficiency are:
- expansion of the left ventricular cavity in myocardial diseases ( hypertrophic cardiomyopathy , coronary artery disease);
- subvalvular pathology (dysfunction of papillary muscles, rupture of chordae tendineae due to infarction or valve prolapse );
- acceleration of blood flow during vegetative dystonia.
Reasons for the development of pathology
The factors causing the problem are diverse. They always have a pathogenic origin.
Congenital and acquired heart defects
Paradoxically, the problem may arise as part of other cardiac changes and genetic abnormalities (more on this below).
Thus, against the background of aortic insufficiency, weakening of the muscles and tendon threads of the mitral valve is possible.
All pathological processes of this kind appear quite late. Some do not make themselves known at all until the result is fatal. Sometimes the diagnosis is made during the autopsy.
Valve prolapse
Clinical variant of organic changes in cardiac structure. It is characterized by retraction of the leaflets of the formation into the atria.
More often it is a congenital anomaly. In approximately 30% of clinical situations it is acquired, due to trauma or surgical interventions. Treatment, as in the case of defects, is surgical; the prospects for recovery are good. Read more in this article.
Cardiac ischemia
A typical age-related pathological process. Also occurs in patients who have had a myocardial infarction. It is accompanied by chronic malnutrition of cardiac structures, but there are no catastrophic phenomena yet.
The most likely consequence of a long-term condition is necrosis of cardiac formations. As a result of low trophism, dystrophy or weakening of the mitral valve occurs. Hence its inability to close tightly.
Even surgery is not a guarantee of recovery. We need to fight the root cause of the phenomenon.
Inflammatory pathologies of cardiac structures
Endocarditis as an option. Accompanied by severe damage to cardiomyocytes, usually of infectious origin (70% of cases), less often of autoimmune origin (the remaining 30%).
Both of these entail gradual destruction of anatomical structures. Treatment is combined with elimination of the inflammatory process and, as necessary, replacement of damaged atria.
The symptoms are pronounced, so it is almost impossible to miss the moment the process begins. Treatment is inpatient, under constant objective control.
Heart attack
Acute myocardial nutritional disorder. Accompanied by general necrosis of organ tissue. The extent depends on which vessel has undergone stenosis (narrowing) or occlusion (blockage).
In all cases, this is a common process, with the death of significant areas of cardiac structures. Even with timely and competent treatment in the hospital, the possibility of a full recovery is almost zero.
In any situation, a gross scar defect will remain, the so-called cardiosclerosis, when functional tissues are replaced by connective tissues that are incapable of contraction and excitation.
Genetic syndromes
Caused by burdened heredity, less often by other phenomena. Classic variants are Marfan disease, Ehlers-Danlos disease.
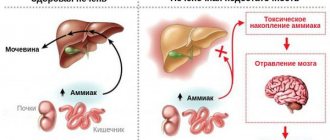
All processes, one way or another, are manifested by a group of symptoms, many have external signs. Disproportion of the limbs, deformations of the maxillofacial area, dysfunctional disorders of the liver, kidneys, and other organs.
The restoration is comprehensive. Usually the diagnosis can be made during infancy, the symptoms are pronounced, and many objective signs are present. Consultation with a geneticist is mandatory.
Autoimmune diseases
{banner_banstat9}
The classic process with cardiac abnormalities is systemic lupus erythematosus. Leads to the destruction of muscle and connective tissues of the body. Including heart ones. Mitral insufficiency develops relatively late, without treatment.
Rheumatism
Another variant of autoimmune disease. Accompanied by destruction of cadiomyocytes. It flows in waves, in fits and starts. Each episode worsens the condition of cardiac structures. Hence the need for ongoing treatment to prevent relapses and support heart function.
Subjective factors
Thus, according to clinical studies, the main contingent of cardiologist patients with suspected mitral regurgitation are people over 60.
Young people suffer less often and there are good pathological reasons for this. Older people experience natural aging and tissue degeneration. Smokers, alcoholics, and people with chronic hypertension of 2 and especially 3 degrees are at greater risk.
Men get sick more often than women, the ratio is approximately two to one. What this is connected with is not known for certain. Assumed to have hard work and a penchant for bad habits.
Symptoms
The main manifestations of mitral valve insufficiency are:
- dyspnea;
- rhythm disturbances;
- swelling;
- heart failure , which develops earlier or later.
In some patients the defect does not appear for a long time. With mitral insufficiency, shortness of breath is less pronounced than with mitral stenosis and appears later. Circulatory failure also develops late, and hemoptysis occurs rarely.
Clinical symptoms depend on the volume of blood return from the ventricle to the atrium, on the contractile function of the myocardium and the severity of pulmonary hypertension . With the development of significant circulatory failure, treatment becomes ineffective, since irreversible changes develop in the internal organs. First of all, the heart suffers due to chronic overload. In acute mitral valve regurgitation, rapid overload of the left ventricle occurs, which increases preload on the left ventricle. This is accompanied by symptoms of left ventricular failure - pulmonary edema and decreased blood pressure .
When auscultating the heart, the doctor notes:
- weakening of the first tone;
- systolic murmur at the apex of the heart;
- splitting of the second tone.
Systolic murmur at the apex radiates into the axilla. It occurs when a backward wave passes into the left atrium through an opening between poorly closed valves.
Prognosis and possible complications
Possible consequences:
- Myocardial infarction.
- Heart failure.
- Multiple organ failure.
- Stroke.
- Cardiogenic shock.
- Pulmonary edema.
These are potentially lethal phenomena. The prognosis for treatment is favorable only in the early stages. Survival rate 85%. With a long course of the pathological process, mortality reaches 60% in a five-year period. When connecting complications - 90%. The ischemic form of mitral regurgitation gives a worse prognosis.
Degenerative changes in the mitral valve, such as mitral valve regurgitation, are a common heart defect. The frequency is determined to be 15% of all congenital and acquired conditions.
Treatment is conservative at the initial stage or surgical at advanced stages, under the supervision of a cardiologist. The likelihood of complete relief from the pathology is low in the later stages. The process is difficult to detect at the initial moment, but this is the best time for therapy.
Tests and diagnostics
ECG . With a minor or moderately severe defect, the ECG does not change, but with severe pathology, hypertrophy of the left atrium is noted. With the development of pulmonary hypertension, hypertrophy of the right ventricle and right atrium appears. Atrial fibrillation occurs with prolonged mitral regurgitation and left atrium enlargement.
Transthoracic and transesophageal (transesophageal) echocardiography . With 3D echocardiography, the LV ejection function is determined - this is the most important indicator for the doctor. This study also evaluates the severity of the defect and the possibility of performing valve-sparing surgery. Transesophageal echocardiography is performed for prosthetic dysfunction, suspected blood clots , or infective endocarditis . Also, transesophageal echocardiography may be needed before surgical treatment to more accurately determine valve damage.
Magnetic resonance imaging . Allows you to determine cardiac function and the volume of reverse flow. CT scan. Determines the severity of valve calcification.
Chest X-ray . Diagnoses calcification of the valve and its structures. An X-ray examination reveals an enlarged heart; it has no waist due to an enlargement of the left atrium. The atrium can reach gigantic sizes. Enlargement of the left ventricle predominates over the right. X-ray reveals venous congestion in the lungs.
Bacteriological examination of blood in rheumatism and infective endocarditis . However, there is a low level of isolation of significant pathogens, which is associated with antibiotic therapy.
Causes
The formation of a defect can occur in the prenatal period, in which case it is considered congenital. The causes of this pathology may be:
- alcoholism, drug use and maternal smoking during pregnancy;
- ionizing radiation;
- poisoning and taking certain drugs (antibiotics, non-steroidal anti-inflammatory drugs);
- systemic and infectious diseases.
The etiological factors of acquired deviation are usually:
- streptococcal and staphylococcal infections with the development of septic endocarditis;
- autoimmune diseases (lupus, multiple sclerosis);
- myocardial damage as a result of a heart attack;
- mitral valve prolapse;
- Marfan syndrome;
- chest injuries with rupture of the valves or fibers that hold them.
Relative mitral valve insufficiency is observed with pronounced enlargement of the left ventricle. The cause of this condition may be dilated cardiomyopathy, aortic valve disease, myocarditis and hypertension.
Diet
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Basic principles of dietary nutrition for patients with chronic heart failure:
- Limiting salt intake to 2g per day (in case of severe edema, it is completely excluded).
- Limiting fluid intake (0.8-1 liter).
- Frequent meals (5-6 times).
- Introducing foods that have a diuretic effect into the diet.
The more severe the heart failure, the more salt in the diet is limited. For CHF I, salty foods are excluded and no more than 3 g of additional salt can be consumed. For CHF II FC and higher, salty foods are excluded and salt is not used when preparing food (added salt is excluded).
Limiting fluid intake is recommended only in severe CHF. A weight gain of 2 kg in 1-2 days indicates fluid retention.
The diet should consist of easily digestible, high-calorie foods, high in protein and vitamins. The diet contains lean meat, vegetable and milk soups, lean fish, protein omelettes, vegetable side dishes, fruits, berries, juices (grape juice, which causes bloating, is excluded). Also limited are foods that cause bloating: beans, peas, beans, radishes.
Not recommended:
- Rich meat broths.
- Strong tea, coffee.
- Pork and animal fats.
- Smoked products.
- Canned food.
- Alcohol.
Prevention
The following will help reduce the risk of heart defects:
- Timely treatment of streptococcal infections.
- Sanitation of infectious foci.
- In case of a rheumatic attack, bicillin prophylaxis is carried out .
- Moderate hardening and a healthy lifestyle.
- To prevent infective endocarditis during dental procedures, antibacterial drugs are prescribed.
- Prescription of antibacterial drugs for invasive manipulations on the respiratory tract, gastrointestinal and urinary tracts.
Types and features of mitral prostheses
Cardiac surgeons use three types of prostheses:
- Mechanical ones, which were initially made in the shape of a ball, and a little later - in the form of hinges. Blood clots often form on them, and installation may be complicated by embolism. The patient has to constantly take antiplatelet drugs. The most modern are products that are processed with a biologically intact titanium alloy.
- Biological. They are created from pericardium or other natural tissues. They do not have the ability to form blood clots.
- Allografts are taken from a corpse and cryopreserved before being implanted into a suitable donor.
Case study: advanced mitral regurgitation
I would like to give an example of a clinical case in which the lack of timely treatment led to such a diagnosis - mitral regurgitation of the 3rd degree. A patient was admitted to the hospital with complaints of severe shortness of breath at rest, worsening with physical activity, cough with sputum, which sometimes contains streaks of blood, weakness, and swelling.
He considers himself unhealthy for many years, often suffered from sore throats, and had joint problems. The deterioration occurred after suffering from acute respiratory viral infection. When listening to the lungs, fine bubbling rales are detected, a weakening of the apical impulse, a click of the opening of the mitral valve, and systolic murmur are observed. The liver is enlarged, the lower edge is determined 5 cm below the hypochondrium. EchoCG shows thickening of the valve leaflets, calcification, dilatation of the left atrium, grade III mitral valve regurgitation.
The patient is scheduled for prosthetic surgery, after which he can be saved. Get treatment on time!
Prognosis for mitral valve insufficiency
With grade 1 mitral insufficiency, the prognosis is favorable. Such patients do not need drug and surgical treatment, but they need to be monitored over time and measures are taken only if necessary. Untimely treatment for grades 2-3 leads to disability of patients. If the overload of the heart continues for a long time, they develop heart failure as a result of myocardial damage. Patients quickly become disabled - they cannot even get out of bed without shortness of breath, swelling increases and cannot be treated, and the valves of the right half of the heart are affected. Without treatment, death inevitably occurs.
In the natural course of events, only 30% survive for 5 years with myocardial ischemia , 80% survive in the absence of ischemia, and 60% survive for 10 years. An unfavorable prognosis is a decrease in left ventricular output of less than 50%, an increase in pressure in the pulmonary artery and an increase in the left atrium of more than 4.0 cm. In this case, patients do not respond to drug treatment. Timely correction of the defect cures patients. Mortality for this pathology decreased significantly after valve replacement, which indicates the effectiveness of surgical treatment. However, if atrial fibrillation occurs before surgery, survival after surgery is reduced.
Characteristic symptoms
As already noted, there are 3 phases of the pathological process. Slightly less common 5, this is a more accurate clinical option, but they are more of a scientific value than a practical one.
An approximate picture is this:
- Dyspnea. First, at the moment of intense mechanical load. In this case, it is difficult to understand where normal physiology ends and the disease begins. Because within the framework of poor body training, identical manifestations are possible. Later, in the subcompensated and completely uncontrolled stage, the symptom occurs at rest, even when the patient is lying down. This significantly reduces the quality of life and leads to pulmonary problems; compensatory mechanisms destroy the entire respiratory system and lead to increased pressure in the artery of the same name. This is a factor that worsens the underlying disease and worsens the prognosis.
- Arrhythmia. In different variations. From tachycardia to atrial fibrillation or group extrasystoles. It is extremely rare that so-called non-dangerous forms of the pathological process occur within the framework of mitral insufficiency. Much more often these are threatening phenomena leading to cardiac arrest or heart attack. It is possible to determine interruptions yourself, but not always. The most accurate diagnostic method is electrocardiography.
- Fall in blood pressure. Sometimes to critical levels, especially during an acute process. Cardiogenic shock may develop. This is a lethal condition; in approximately 95% of situations it leads to the death of the patient, even with timely resuscitation and comprehensive treatment. Recovery is impossible, the prognosis is extremely unfavorable.
- Pulmonary edema.
- Also weakness, drowsiness, apathy. In the acute period, a panic attack occurs with inappropriate behavior and increased motor activity.
- Ascites. Or fluid accumulation in the abdominal cavity.
- Edema of the lower extremities. Diuretics are effective only at the first moment, then they do not bring the desired effect.
List of sources
- Nesukai E.G. Mitral regurgitation/Heart failure. - 2010. - No. 3, pp. 84-91.
- Knyshov G.V., Bendet Ya.A. Acquired heart defects. /Kyiv: Institute of Cardiovascular Surgery, 1997. – 280 p.
- Kovalenko V.N., Nesukai E.G. Non-coronary heart diseases. Practical guide / K.: MORION, 2001. – 480 p.
- Shikhverdiev N.N., Marchenko S.P. Fundamentals of reconstructive surgery of heart valves / St. Petersburg: Deaton, 2007. – 270 p.
- Mitral regurgitation. Clinical recommendations. 2021. - 30 p.
- Danilov A.I., Kozlov R.S., Kozlov S.N., Dekhnich A.V. Practice of managing patients with infective endocarditis in the Russian Federation // Antibiotics and chemotherapy. 2017; 62 (1–2): 7–11.
Treatment methods
Treatment of mitral valve insufficiency at the compensation stage consists of constant monitoring of the patient, reducing physical activity and using medications to prevent the progression of the disease. If complications arise and there is no way to solve the problem surgically, symptomatic therapy is used:
- cardiac glycosides;
- diuretics;
- beta blockers;
- calcium antagonists;
- ACE inhibitors;
- anticoagulants and antiplatelet agents.
No drugs can cure the disease. Conservative methods only help to temporarily delay deterioration and improve the quality of life. The only way to fix the problem is to perform an operation.
Surgical interventions: indications and techniques
The indication for surgical treatment is a gross violation of the structure of the valves, leading to a pronounced deviation of hemodynamics. Valve restoration or replacement is required in the following cases:
- history of endocarditis;
- first manifestations of heart failure (shortness of breath, swelling);
- rhythm disturbances;
- frequent severe pain in the chest, signs of congestion in the pulmonary system.
You cannot operate in the following cases:
- onset of an acute disease or exacerbation of a chronic one;
- stroke or heart attack;
- heat;
- extreme degree of heart failure.
The main types of interventions are complete replacement or valve repair. The second option is carried out in the following ways:
- annuloplasty using soft or hard rings;
- valve resection;
- replacement of chords with artificial materials;
- edge-to-edge technique.