Sign up
+7
Aortic heart disease is a valve lesion that may or may not involve the ascending aorta. Aortic stenosis is characterized by a narrowing of the aorta, which impedes blood flow. With this pathology, the valve functions are disrupted, complications arise, such as thromboembolism, chronic heart failure, strokes, and heart rhythm disturbances.
Causes of development of aortic stenosis
The disease can be congenital or acquired. The congenital form most often makes itself felt before the age of thirty. Acquired stenosis often becomes a consequence of rheumatism and manifests itself in adulthood. Other reasons for the development of stenosis include:
- Infectious form of endocarditis.
- Rheumatism.
- Myocarditis.
- Atherosclerosis.
- Aortic aneurysm.
- Morphan's syndrome and other systemic connective tissue diseases.
- Heart defects that occur after injuries.
- Tumors in the heart area.
Make an appointment with a specialist without queues, at a convenient time
Sign up
+7
Symptoms of the defect
For a long time, aortic valve stenosis may not manifest itself, as it is completely compensated due to left ventricular hypertrophy. The first symptoms to appear are reduced perfusion of the brain and heart during exercise:
- dizziness;
- loss of consciousness;
- dyspnea;
- weakness and fatigue;
- cardiopalmus;
- muscle weakness;
- pale skin;
- pain in the region of the heart of a compressive nature.
Pain from angina pectoris can last up to several hours; nitrates in this case are ineffective
Over time, these signs appear during less significant physical activity, and then are even observed at rest. Shortness of breath occurs more and more often, occasionally appearing at night, and may be accompanied by a cough. This set of symptoms indicates stagnation in the pulmonary circulation and the appearance of so-called “cardiac asthma”.
Important! The extreme severity of left ventricular failure is pulmonary edema, which can be fatal.
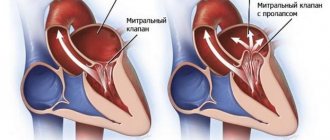
Edema in the legs is a manifestation of right ventricular failure, so they do not appear in the early stages of isolated aortic valve stenosis. Their addition to other signs of the disease indicates a decrease in the functional contractility of the left ventricle. Edema may appear earlier when there is also a mitral valve defect. The patient may also be bothered by painful sensations in the area of the right hypochondrium, which is explained by the overflow of blood in the liver and stretching of its capsule.
Aortic stenosis with a sharp decrease in the diameter of the valve ring can lead to sudden cardiac death. Complications occur in 5–10% of cases of the defect and occur most often in older people.
Features of the disease
Aortic stenosis itself occurs in 2% of all cases of acquired defects; in combination with valve insufficiency, the disorder can occur in almost 23% of cases. If the valve leaflets are inflamed, the tissues thicken and harden, causing the valve opening to narrow over time. Also, the valves can calcify and fuse along the commissures, greatly narrowing the useful area of the opening.
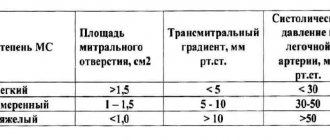
In normal condition, the useful area of the valve opening is from 2.5 to 3.5 square centimeters. If the hole decreases to approximately 0.8-1 cm2, hemodynamic disturbances begin. The critical indicator of the lumen area is 0.5-0.7 cm2. The left ventricle should constantly maintain systolic pressure within 200-250 mmHg. pillar At first, when the valve lumen narrows, the left ventricle compensates for the pathology, making maximum effort, and the person feels normal. Over time, blood begins to accumulate in the cavity, the myocardial fibers stretch, the ventricle begins to contract more actively, and the heart muscle “gets tired” and weakens. The myocardium of the left ventricle becomes hypertrophied, coronary insufficiency develops, and the muscle does not receive the necessary nutrition. Patients suffering from aortic valve stenosis are at high risk of sudden death.
Aortic valve insufficiency is a common companion to stenosis. Excessive pressure in the left ventricle provokes an increase in pressure in the left atrium, and then in the vessels of the pulmonary circulation. The changes primarily affect the connective tissue of the valve. As inflammation increases, the valve leaflets become deformed, their edges thicken, and can turn in and sag. As a result, the valves cannot close tightly, and blood returns to the heart. If the inflammatory process is stopped, valve deformation may continue, for example, due to the formation of scar tissue.
Drug therapy
— There is no specific drug treatment. Drug treatment is aimed at stabilizing hemodynamics - Prevention of infective endocarditis is indicated. Indications for surgery: - pressure gradient between the left ventricle and the aorta is more than 50 mm Hg. Art., or the area of the aortic opening is less than 0.7 cm2 (normally its area in adults is 2.5-3.5 cm2) - angina pectoris, fainting, signs of heart failure. Surgical treatment: — Radical treatment — aortic valve transplantation. — Balloon valvuloplasty of the aortic valve is indicated for elderly, debilitated patients who may not undergo valve replacement surgery
Symptoms of aortic valve stenosis
Stenosis that is in the compensation stage may not manifest itself at all. The patient's general condition may remain normal or satisfactory. The first manifestation is shortness of breath after any activity, severe fatigue, and weakness. Over time, attacks of angina pectoris, fainting, shortness of breath, a feeling of heaviness in the right hypochondrium, and swelling throughout the body appear. One of the severe manifestations of stenosis is pulmonary edema.
- Available: doctor’s appointment from 1500 rubles
- Convenient: open daily from 8:00 to 21:00
- Quickly: we will carry out all the diagnostics at the first appointment
- Complete: has all the necessary equipment
Hemodynamic disorders, or what happens to the heart
An obstruction in the path of blood that should enter the aorta from the left ventricle leads to an increase in the pressure gradient in systole. Aortic stenosis leads to a sharp increase in the load on the myocardium of the left ventricle. Therefore, it thickens, which is called concentric left ventricular hypertrophy. However, its cavity does not expand for a long time and the defect is compensated for many years. If systolic function is preserved at this time, then left ventricular diastole is impaired.
Despite good indicators of systolic function, stroke volume remains practically unchanged, and this is necessary during physical activity. This explains the appearance of symptoms of insufficient blood supply to the brain and heart with increased physical activity in patients with aortic valve stenosis.
Unfortunately, the hypertrophied myocardium of the left ventricle cannot endlessly cope with heavy loads; its walls lose their tone, become thinner, and expand, which is called “myogenic dilatation.” Following this, the left atrium fills with blood and expands. This leads to an increase in pressure in the pulmonary veins (pulmonary hypertension) and the formation of left ventricular failure syndrome. In addition, the fibrous ring of the mitral valve expands, which manifests itself as its insufficiency and further aggravates the patient’s condition. Further hemodynamic changes lead to disturbances in the right side of the heart.
How is the diagnosis carried out?
At an appointment with a cardiologist, the patient is interviewed, physically examined, lifestyle and possible genetic predisposition to diseases are assessed. To exclude other pathologies of the cardiovascular system, differential diagnosis is used. Instrumental methods include:
- Electrocardiography, electrocardiogram.
- ECG.
- Echocardiography.
- Probing of the heart.
- Aortography.
- Coronary angiography.
- Ventriculography.
- Phonocardiography.
Diagnosis of pathology
When examining a patient, the doctor pays attention to the pallor of the skin, sometimes in combination with cyanosis of the extremities, which is more typical for the terminal stages of the disease. This phase is also characterized by the appearance of swelling in the legs. From other organs, there is an enlarged liver and moist fine rales in the basal parts of the lungs. Percussion reveals a shift of the left border of the heart to the left. The percussion picture in the last stages of the disease takes on the shape of an aortic configuration of the borders of the heart with the so-called emphasized “waist”. A tremor is felt by palpation during systole in the jugular fossa, the apical impulse is shifted to the left.
Auscultation reveals a rough murmur of systolic origin in the aorta, which is carried out to the vessels of the neck. You can also note a weakening of both heart sounds at the point of auscultation of the aorta.
Reference! Sometimes systolic murmur in the aorta can be heard even at a distance.
An alternative technique to traditional heart listening is phonocardiography. When registering it, almost the same changes are determined as during auscultation. Blood pressure also undergoes changes: systolic and pulse pressure decreases due to a decrease in blood flow into the aorta. At the onset of the disease, a decrease in heart rate is observed, which reflects the inclusion of natural compensatory mechanisms. In the future, tachycardia or arrhythmias predominantly occur.
An ECG may reveal left ventricular hypertrophy, left ventricular systolic overload, various arrhythmias or impulse blockade. X-ray of the heart with the development of dilatation of the left chambers of the heart reveals its aortic configuration and symptoms of pulmonary hypertension.
The diagnosis of aortic valve stenosis is based on a comprehensive examination of the patient, but still only ultrasound examination of the heart helps to diagnose the defect even in the early stages.
Cardiac ultrasound is a safe method for diagnosing aortic valve stenosis at any age
When performing an echocardiography, it is possible to diagnose seals of the valve leaflets and their limited movements, bicuspid valve structure, thickening of the septum between the ventricles and the posterior wall of the left ventricle. Doppler techniques help measure the pressure gradient across the aorta and pulmonary valve. Less commonly used are ventriculography, probing of the ventricular cavities, aortography or coronary angiography.
Treatment
Patients with stenosis must be monitored by a cardiologist. Patients in this category should take antibacterial drugs before any interventions and invasive procedures for preventive purposes to prevent the development of inflammation (for example, before visiting the dentist). Also, drug treatment involves controlling blood pressure and stabilizing it.
Surgical treatment has several indications:
- Septic embolism.
- Suppuration on the valve.
- Third degree of reverse blood flow.
- A valve infection that cannot be treated.
- Heart failure with congestion.
Surgical treatment means removing the diseased valve and replacing it with an artificial one. The valve can be mechanical or biological. The main differences of the biological valve:
- Three months after its installation, anticoagulant therapy is not required.
- The prosthesis is as close to natural as possible.
- Unlike a mechanical prosthesis, the valve does not make clicks.
- The biological valve is less durable; degenerative changes can be observed already in the second year of operation with a total service life of 10 years.
A mechanical valve is installed for life; its only disadvantage is the need to constantly take anticoagulants (blood thinners).
Prices for services
| Name | Time | Price | |
| Appointment with a cardiologist, treatment and diagnostic, primary, outpatient | 1500 | ||
| Treatment and diagnostic appointment with a cardiologist, repeated, outpatient | 1000 | ||
| Preventive, outpatient appointment with a cardiologist | 550 | ||
| Comprehensive consultation with a cardiologist ECG with interpretation + Echo-kg | 3650 | ||
| Call a doctor to your home (Khimki, Starbeevo, Ivakino, Naberezhnye) | 15000 | ||
| Calling a doctor to your home (Skhodnya, Podrezkovo, Novopodrezkovo, Planernaya station, Firsanovka) | 15000 | ||
| Call a doctor to your home (Kurkino, Novogorsk) | 15000 | ||
| Call a doctor to your home (Left Bank, Moscow, within the Moscow Ring Road) | 15000 | ||
| Medical consultation | 3300 | ||
| Extract from outpatient card | 660 | ||
| Consultation (interpretation) with analyzes from third parties | 1300 | ||
| Consultation on treatment adjustments | 550 | ||
| Repeated reception of CMN | 1600 | ||
| Initial reception of CMN | 2000 | ||
| Express test for determining the level of Troponin in the blood. | 1900 | ||
| Expand all prices | |||
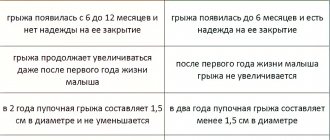
How does the defect manifest itself in children?
Congenital aortic valve disease with stenosis in children is most often diagnosed shortly after birth. During the period of intrauterine development, the pathology may not manifest itself in any way, which is associated with the peculiarities of blood circulation in the fetus - the presence of the arterial or botallus duct. After birth, it closes, and the left ventricle experiences enormous stress.
The child experiences shortness of breath, fainting, increased heart rate and breathing, pale skin, weakened pulse in the extremities. With a moderate degree of narrowing, severe heart failure is not observed. In addition to noise, the child may have mental retardation. The face takes on the features of an “elf”. Older children with aortic valve stenosis complain of weakness, shortness of breath, interruptions in heart function, and chest pain.
In cases of critical aortic valve stenosis, symptoms appear almost immediately after birth, so care should be provided to such children immediately
It is important to establish the diagnosis in utero. This becomes possible from the 6th to 7th month of gestation, thanks to antenatal ultrasound diagnostics.
4.Treatment
From the moment characteristic symptoms appear, the patient is at risk, where the average life expectancy without adequate treatment is significantly lower than the statistical average. Drug treatment is ineffective.
However, in some cases (for example, when preparing for cardiac surgery or its impossibility due to the presence of absolute contraindications), diuretics and cardiac glycosides are used symptomatically and with caution.
Surgical intervention with aortic valve replacement is the only radical solution.
Both biological transplants from animal donors are used (usually in the treatment of elderly people, where such a transplant provides a more long-term effect) and mechanical valve prostheses. If assistance is provided in a timely manner, with qualified training and subsequent rehabilitation, the prognosis is quite favorable: in the absence of severe complications, mortality in the postoperative period is 2-3%.
Treatment of the defect
There are two directions in the treatment of aortic valve stenosis: conservative and surgical. It is clear that drug therapy has no independent meaning, because only surgery can radically cure a patient from this pathology. At the initial stages of the disease, conservative management of the patient without surgery is possible.
Conservative treatment of aortic heart disease involves observation by a cardiologist with periodic examinations (ECG, EchoCG).
Drug treatment involves taking the following medications and a list of medications:
- cardiac glycosides;
- diuretics;
- nitrates;
- potassium preparations;
- dopaminergic drugs.
Attention! Self-medication of heart disease is dangerous for human health and life! Therapy should be prescribed by the attending cardiologist.
When a patient with aortic valve stenosis undergoes a procedure that could result in infection entering the body, a prophylactic antibiotic, for example, from the group of cephalosporins, is prescribed.
Indications for surgery for aortic valve stenosis: moderate or severe degree of disease, obvious clinical picture of the defect. Surgery should be performed before the onset of heart failure. For moderate stenosis, valvuloplasty surgery can be performed. If we are talking about a pronounced process that may be accompanied by heart failure, simply separating the valve leaflets from each other will not be enough. Therefore, the patient may be offered aortic valve replacement.
Attention! The last two stages of aortic valve stenosis are a contraindication for heart surgery
Valvuloplasty surgery can be performed for minor changes in the valve. There are two types of this intervention:
- open;
- endovascular.
The latter procedure is called balloon aortic valvuloplasty and is considered minimally invasive. Access is made through an incision in the femoral artery; all further manipulations are performed under the control of an X-ray machine. A deflated balloon is brought to the damaged leaflets, it is straightened, which makes it possible to disconnect the adhesions between the valve leaflets. Indications for balloon valvuloplasty:
- before pregnancy or childbirth if the woman has a severe defect;
- before surgery at another location in patients with severe stenosis;
- before aortic valve replacement in severe patients;
- as a palliative intervention when there are contraindications to open surgery.
During valve replacement, damaged leaflets are removed and a mechanical or biological xenogeneic prosthesis is placed in their place.
Patients undergoing aortic valve replacement should remain on anticoagulant therapy at all times.
In childhood, a Ross operation can be performed, the essence of which is to transplant the pulmonary valve into the aortic position.
Vascular stenosis
Atherosclerosis
Diabetes
Ulcer
4920 12 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vascular stenosis: causes, symptoms, diagnosis and treatment methods.
Definition
Vascular stenosis (Greek στενός - “narrow, cramped”) is a partial or complete persistent narrowing of the lumen of blood vessels with limitation or complete cessation of blood flow.
Causes of vascular stenosis
Depending on which vessels are affected, a distinction is made between stenosis of arterial vessels (aorta, arteries, arterioles) and stenosis of venous vessels (superior vena cava, inferior vena cava, veins, venules).
Vascular stenosis can be either congenital or acquired.
The main cause of acquired stenosis of the aorta, arteries of the lower extremities, and coronary arteries of the heart is atherosclerosis, a systemic metabolic disease with predominant damage to the vascular wall. The degree of narrowing of the artery and its length may vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, as a result, the blood clotting process is activated and a blood clot is formed.
Blockage of the vessel can lead to ischemia or necrosis of the tissue or organ.
Risk factors for the development of atherosclerosis include:
- male gender;
- elderly age;
- smoking;
- dyslipidemia (violation of the normal ratio of blood lipids);
- diabetes,
- arterial hypertension,
- increased blood homocysteine;
- elevated levels of C-reactive protein (CRP);
- increased blood viscosity and hypercoagulable states;
- chronic renal failure.
Another disease leading to arterial stenosis is obliterating endarteritis (spontaneous gangrene) - a chronic disease of peripheral blood vessels (mainly affecting the arteries of the feet and legs).
Mostly men under the age of 25-40 are affected. Those at risk include smokers, as well as people with frostbite on their feet. Diabetic angiopathy, characterized by damage to both small vessels and large and medium-sized arteries, develops in patients with diabetes mellitus. In diabetic macroangiopathy, when large blood vessels are affected, changes characteristic of obliterating atherosclerosis are found in the wall of the great vessels. With microangiopathies, when small blood vessels are affected, thickening of the walls of microvasculature vessels (arterioles, capillaries, venules) occurs, which leads to a narrowing of the lumen and deterioration of the blood supply to organs and tissues.
Coarctation of the aorta (congenital segmental narrowing of part of the aorta that obstructs blood flow) occurs as a result of improper fusion of the aortic arches in the embryonic period. The length of the narrowing is usually 1-2 cm. The ascending aorta and branches of the aortic arch expand, their diameter increases significantly, and the walls of the arteries participating in the collateral circulation become thinner. Two modes of blood circulation are formed in the systemic circle: up to the point of obstruction to blood flow there is arterial hypertension, and distal (or below) there is hypotension.
Venous stenosis most often occurs as a result of direct damage to the vascular wall during catheter insertion and is then aggravated by the constant presence of a foreign body and mechanical irritation. Inflammation and activation of the blood coagulation system are observed in the vessel wall. These changes lead to proliferation (multiplication) of smooth muscle cells, thickening of the vein wall, and the formation of microthrombi.
Thus, risk factors for the development of central venous stenosis are: the use of a central venous catheter, infections associated with the installation of a catheter, and concomitant diseases.
Systemic vasculitis, tumor diseases and other causes of vascular stenosis are detected much less frequently.
Classification of the disease
According to the type of blood vessels:
- arterial stenosis;
- venous stenosis
Due to the occurrence:
- congenital;
- acquired.
By localization:
- Stenosis of the arteries of the lower extremities.
- Stenosis of the carotid (carotid) and cerebral arteries.
- Stenoses of the arteries of internal organs:
- renal arteries,
- mesenteric arteries etc.
- Aortic stenosis.
- Stenosis of coronary vessels.
By caliber of damage:
- stenosis of large vessels (aorta and its branches);
- stenosis of medium-diameter vessels;
- stenosis of small vessels (arterioles and capillaries).
Symptoms of vascular stenosis
Damage to the blood vessels of the brain is one of the main causes of mortality and disability in the population. 2/3 of ischemic strokes are associated with narrowing and deformation of the carotid arteries.
The risk of developing ischemic stroke is directly related to the degree of narrowing of the artery lumen.
Occlusion (closure) of the internal carotid artery leads to the development of stroke in 40% of cases.
Damages to the blood vessels of the brain can occur in several forms:
- The asymptomatic form is characterized by the absence of focal and cerebral neurological symptoms (impaired consciousness, headache, vomiting, slow pulse).
- Discirculatory encephalopathy is characterized by a predominance of general cerebral symptoms; focal neurological symptoms are absent or appear in a very mild form.
- Transient ischemic attacks manifest themselves in the form of transient disorders of cerebral circulation of the ischemic type and are accompanied by the appearance of focal neurological symptoms that resolve within 24 hours.
- The consequences of a minor stroke are an acute ischemic cerebrovascular accident with the development of neurological symptoms, which almost completely regress within a month as a result of conservative therapy.
- The consequences of a completed stroke are an acute ischemic disorder of cerebral circulation, accompanied by the development of persistent focal neurological and cerebral symptoms.
- Ischemic stroke is damage to brain tissue with disruption of its functions due to obstruction or cessation of blood flow.
Atheroslerotic lesion of the coronary arteries of the heart is manifested by angina pain, but can sometimes be perceived by the patient as discomfort, a feeling of heaviness, compression, tightness, distension, burning or lack of air.
Most often, the pain is localized behind the sternum or along the left edge of the sternum; it can radiate (give) to the neck, lower jaw, teeth, interscapular space, and less often to the elbow or wrist joints, mastoid processes. Pain with angina pectoris usually lasts from 1 to 15 minutes. Occurs during significant physical or emotional stress. After taking nitroglycerin or stopping the exercise, the pain stops. As angina progresses, an attack may occur with minimal exertion and then at rest.
The main symptom of renal artery stenosis is a persistent increase in blood pressure, which is difficult to respond to drug therapy. Approximately 90% of cases of renal artery stenosis are caused by atherosclerosis; in 10% of cases, stenosis occurs due to fibromuscular dysplasia, a group of diseases that affect the walls of the arterial vessel.
With renal artery stenosis, the blood supply to the kidney tissue is reduced, hormonal factors (renin-angiotensin-aldosterone system) that regulate blood volume and blood pressure are activated, and the development of chronic kidney disease is accelerated.
Stenosing damage to the vessels supplying blood to the abdominal organs (mesenteric arteries) is more often observed in middle-aged and elderly people and manifests itself as chronic abdominal ischemia syndrome, so the main complaint of patients is pain, which appears after 20-25 minutes. after eating, lasts 1-2 hours and usually subsides on its own. The pain can be localized in the epigastric region, directly under the xiphoid process, and radiate to the right hypochondrium or spread from the periumbilical region throughout the abdomen. Some patients note a feeling of constant heaviness in the abdomen, and vomiting is rarely observed.
Other symptoms of chronic abdominal ischemia are intestinal dysfunction, expressed by disturbances in its motor, secretory, absorption functions, and progressive weight loss.
Obliterating atherosclerosis of the aorta and main arteries of the lower extremities is more common in men over 40 years of age and deprives them of their ability to work. The process can be localized in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal).
Small atherosclerotic lesions of the arteries of the lower extremities may not be clinically manifest. With continued vasoconstriction, intermittent claudication occurs, which is manifested by discomfort or pain in the muscles of the lower limb during physical activity. Damage to the terminal aorta and iliac arteries can cause pain in the buttocks, thigh, and calf. Impaired patency of the femoral-popliteal segment is characterized by pain in the calf. Occlusion of the arteries of the leg usually causes pain in the calf, foot, absence or decrease in skin sensitivity in them.
With obliterating endarteritis, trophic disorders are observed (cracks, dry skin, brittle nails, ulcers), intermittent claudication, leg pain, necrosis and gangrene of the limb.
In the generalized form of obliterating endarteritis or atherosclerosis, not only the vessels of the extremities are affected, but the visceral branches of the abdominal aorta, branches of the aortic arch, cerebral and coronary arteries.
The clinical picture of diabetic macroangiopathy consists of the clinical picture of microangiopathy and atherosclerosis of the great vessels, but is characterized by a more severe and progressive course, often ending in gangrene.
The clinical picture of diabetic microangiopathy of the lower extremities is similar to that of obliterating endarteritis.
With coarctation of the aorta, symptoms depend on the severity of the disease. In the case of significant narrowing of the aorta, the parents of the newborn pay attention to the pale skin, sweating, and difficulty breathing of the child. In older children and adults, the symptoms are usually mild: high blood pressure, headache, cold extremities, nosebleeds.
Stenosis of the central veins is clinically manifested by swelling of the extremities, pain in them and trophic changes (cyanosis, thinning of the skin, cracks, ulcers, etc.).
Diagnosis of vascular stenosis
Diagnosis of the disease is based on the analysis of patient complaints, medical history data, clinical picture, data from laboratory and instrumental research methods.
To clarify the cause of vascular stenosis, the following may be recommended:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);
Disease prognosis
Is it scary to live with aortic valve stenosis? Medical statistics indicate mortality within 2-5 years when signs of the defect appear, such as syncope, chest pain and symptoms of left ventricular failure. Therefore, it is so important to carry out prompt surgical treatment of the disease, because after it the 5-year survival rate exceeds 85%, and the 10-year survival rate is about 70%.
There are no specific measures to prevent the vice; you should adhere to a healthy lifestyle: do not abuse fatty and fried foods, eliminate bad habits, and exercise regularly.
Thus, aortic disease with stenosis may not make itself felt for a long time, so preventive examinations by a doctor play an important role in the early diagnosis of the disease.