There are contraindications. Specialist consultation is required.
Forms of the disease Causes of development Symptoms Who is at risk? Classification What will happen if left untreated? Diagnostics Treatment methods and techniques Prevention
Chronic venous insufficiency, as well as its acute form, is associated with impaired blood flow. Thanks to the valve system, as well as the muscles of the body, blood from the lower extremities flows to the heart, overcoming the force of gravity. Therefore, moderate physical activity, gymnastics during sedentary work, and regular walks are recommended for each person. If, due to an incorrect lifestyle or poor heredity, varicose veins appear or the lumen of the vessel is clogged with a blood clot, venous insufficiency of the legs begins to develop. First, the affected vein expands, then the function of the valves is disrupted (they do not close completely), and the result is reflux, that is, reverse flow of blood - it flows not only to the heart, but also back to the legs. Due to the accumulation of blood, a person feels heaviness in the legs and swelling appears. These symptoms should not be attributed to fatigue; you need to urgently contact a phlebologist, otherwise chronic venous insufficiency will develop.
Important! Varicose veins and venous insufficiency are not the same thing. Varicose veins are only one sign of insufficiency, although the most common.
CVI – causes of chronic venous insufficiency
CVI is a symptom complex in which there are problems with the lumen of the veins. Usually the vessels have normal lumen. If there are disturbances, the capacity of the veins is significantly reduced. Overload of the venous system leads to impaired blood return, which is manifested by the appearance of symptoms of chronic venous insufficiency.
Impaired venous blood return leads to symptoms of CVI
Is CVI dangerous? Wikipedia states that CVI actively develops and progresses in women 30-50 years old, especially those with a hereditary predisposition. Often, symptoms of CVI appear during pregnancy, when body weight increases significantly.
Among the factors leading to CVI is weak physical activity.
The appearance of CVI is provoked by:
- travel in transport without changing position;
- long static position at the workplace;
- excess weight;
- tendency to constipation;
- staying in the heat for a long time;
- straining when lifting weights.
In addition, CVI can occur with systematic exercise and taking hormonal contraceptives; CVI often occurs during pregnancy.
The mechanism of the onset and development of the disease
Under the influence of gravity, the blood in the vessels descends to the lower extremities, the body has to make efforts to lift it. Venous valves prevent blood from flowing downwards, which are actively helped in this by physical activity, muscle contraction and bending of the knees. The combination of these factors ensures normal blood flow.
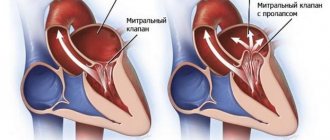
Maintaining a constant resistance to gravity is possible due to physiological changes in the lumen of blood vessels when changing body position, the operation of the valve apparatus and the tone (elasticity) of the venous wall. If one of these component mechanisms is disrupted, pathological processes begin to affect the entire system as a whole. Loss of elasticity of the section of the vein below the valve, and its expansion leads to valvular incompetence, the inability to maintain blood flow for subsequent rise. Stagnation of fluid leads to increased pressure to move blood upward. But, over time, increased pressure increases the volume of the part of the vein that has lost its elasticity.
Venous reflux (reverse flow of blood from top to bottom) can join the pathological process. The liquid begins to stagnate and put pressure on the walls of the vessel. As a result, blood plasma leaks into the surrounding tissue, causing swelling. The situation develops similarly with initial valvular insufficiency.
Simultaneously with circulatory failure, the lymphatic system is also overloaded. Trophic disorders contribute to the formation of trophic ulcers. Trophic ulcers are long-term non-healing wounds (6 months or more) affecting the skin and tissues. They form on the lower leg, are surrounded by an area of inflammation, and have a high risk of infection.
CVI - symptoms
CVI may not manifest itself for a long time, but the symptoms that appear significantly affect the patient’s quality of life. The first symptoms are a feeling of heaviness in the legs, very often swelling of the legs and feet appears. Next comes bursting pain. The calf muscles may cramp at night, and the patient experiences a feeling of heat in the lower extremities.
Advanced forms of venous insufficiency - trophic eczema and ulcers
Spider veins and veins begin to appear through the skin, which with varicose veins become noticeable in the form of plexuses, similar to a bunch of grapes. The skin becomes drier and becomes covered with brown “islands” that grow as the disease progresses. Eventually, a trophic ulcer forms in their center.
Classification of the disease
Acute venous insufficiency has no classification by stages. Let's consider the degrees and stages of the chronic form of the disease. To fully describe the patient’s diagnosis, doctors use the CEAP classification, that is, assigning a kind of “code”, for example: C4a, S, Eс, Ad, Pr, 8, 10, 11, 17. It is deciphered based on the following classification characteristics.
C – pathology class:
- C0 – no visible symptoms;
- C1 – spider veins;
- C2 – dilated veins from 3 mm;
- C3 – swelling in the areas of the legs and ankles;
- C4a – dermatitis, pigmentation and other skin lesions;
- C4b – increased pigmentation, thickening of the skin;
- C5 – self-healing skin wounds;
- C6 – non-healing trophic ulcers.
The following index indicates whether the patient has complaints: A – without symptoms or complaints, S – there are complaints.
E – cause of disease:
- EC – congenital;
- Er – etiology unknown;
- Es – the reason is known.
A – localization:
- As – saphenous veins;
- Ar - vessels that connect the deep veins and subcutaneous veins;
- Ad – deep veins;
- Аn – there are no pathologies of the venous system.
P – type of pathology:
- Po – cessation of blood movement through the veins;
- Pr – valve insufficiency;
- Pr,o – both;
- Рn – no disturbances in the movement of blood through the veins were detected.
The number is the area of the venous system where the pathology is detected: from 1 to 18.
CVI - stages of chronic venous insufficiency
The disease has several stages:
- first the venous wall changes;
- valves stop functioning;
- perverted blood flow occurs, leading to venous hypertension;
- varicose veins appear;
- skin pigmentation changes;
- Varicose eczema may appear;
- at this stage, thrombosis often develops, affecting the deep veins;
- complications include thrombophlebitis, pulmonary embolism.
The walls of the veins become more permeable, lymph enters the blood, trophism is disrupted and inflammation occurs (10-15% of cases). The last stage of CVI is a venous trophic ulcer (4% of cases)
What happens if venous insufficiency is not treated?
Venous insufficiency is a trigger for a number of disorders and diseases with more serious consequences:
- Skin changes (pigmentation)
- Eczema (skin inflammation)
- Ulcers (venous ulcers)
Compression jersey medi
Thanks to the breathable and elastic material, compression jersey provides high wearing comfort. Modern medical compression hosiery is visually indistinguishable from model hosiery, but provides high medical effectiveness when used.
The human body
How do veins work?
Vienna
Product Tips
Ideal compression product
Compression hosiery
CVI - Diagnostics
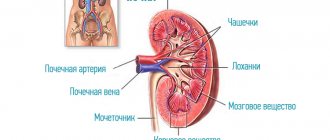
Typically, patients turn to a phlebologist when obvious signs of CVI are visible to the naked eye, and the diagnosis is easy to make. Specialized clinics use ultrasound methods to diagnose CVI:
- the condition of blood vessels is studied;
- assesses how blood flows through them;
- Disturbances in the functioning of venous valves are considered.
Ultrasound scanning gives a complete picture of the causes of CVI
With an ultrasound examination, the doctor receives a three-dimensional image of the vessel, reliable information about its functioning, and can make an objective diagnosis.
CVI – complications of chronic venous insufficiency
Many patients have a common belief that CVI is not too dangerous, that it is just cosmetic. In fact, disturbances in the venous blood flow of the legs provoke the formation of blood clots. Therefore, CVI has two main complications: thrombosis and thrombophlebitis. In the first disease, the deep veins suffer:
- the affected area acquires a bluish tint,
- tissues swell
- movements are accompanied by pain.
With thrombophlebitis, blood clots form in the superficial veins. Wherein
- the skin turns red;
- Painful lumps form under the skin
- When walking, the patient experiences sharp pain in the legs.
A detached blood clot can clog a large vessel and cause death. Acute manifestations of these diseases are treated only in a surgical hospital. You can see the danger of CVI - photos, the results are on websites on the Internet.
CVI. How to treat the disease with creams?
Treatment with all kinds of ointments is very common at the household level. Many patients stop treatment at this point. Most ointments only temporarily relieve swelling and pain. CVI – how to treat it? This question is asked by all patients. Such popular remedies as heparin ointment, venoruton, venitan, hepatrombin cope well with the external manifestations of CVI at an early stage, but cannot eliminate its cause. For effective treatment that will give long-term results, a visit to a phlebologist or vascular surgeon is mandatory.
CVI - how to cure without consequences?
This can be done even in difficult cases; treatment of CVI in Moscow can be carried out at a high level. True, then surgery will be needed to restore blood flow in the veins. But in the early stages, conservative treatment of CVI without surgery is sufficient. In particular, elastic compression is used. For this purpose, special medical knitwear is used in the form of stockings, golf, tights (conservative treatment).
When treating CVI, it is very important not to waste time using various ointments that give a local and short-term effect, but to seek help from a qualified specialist.
CVI - treatment at home
Don't be afraid if you are diagnosed with CVI. Treatment with folk remedies will alleviate the situation. For example, venotonic drugs will help. They strengthen the walls of blood vessels, stimulate microcirculation, and quickly relieve the feeling of tired legs and swelling. Patients are also treated with blood thinning medications.
Do you need to relieve the pain of CVI? Treatment with traditional methods:
- Apple vinegar. Twice a day for 30 minutes. Apply gauze soaked in vinegar to your feet for 30 minutes. Keep your legs higher. Reviews about the product are contradictory, but the majority note a positive, weak effect.
- Bell pepper. Dilute a teaspoon of pepper powder in a glass of hot water and drink three times a day. The product stops leg pain and improves blood flow. But CVI does not go away that easily, treatment, the results are still not the same as when treated by a professional phlebologist.
Symptoms of the disease
Let's look at the general symptoms first. It should be remembered that in the initial stages of the disease they appear one at a time and are often “blurred”. The more the disease progresses, the more pronounced the symptoms, and they most often appear in groups. So:
- pain in the legs, feeling of heaviness, fullness;
- spider veins;
- swelling - first passing after rest, then permanent;
- night cramps in the legs;
- dryness, unhealthy shine of the skin, age spots or areas of discoloration;
- trophic ulcers at an advanced stage.
Consultation with a surgeon: when to contact, how is the appointment?
Symptoms of CVI by stage
| Stage | Description |
| 0 | The person is able to work, there are no symptoms, they do not appear after sports and other activities. |
| 1 | Slight pain, heaviness in the legs and swelling at the end of the day, which disappears in the morning, mild cramps. A person is not limited in physical activity and can work at the same pace. |
| 2 | Manifestations of venous insufficiency become pronounced. These are skin pigmentation, dermatological diseases, severe swelling, skin necrosis in some areas. It becomes difficult for a person to work physically or play sports. |
| 3 | Trophic ulcers appear and tissue metabolism is completely disrupted. A person loses his ability to work. |
Symptoms of AHF
Signs of the disease are more pronounced and appear much faster compared to CVI:
- Pain in the legs that increases with movement;
- just below the site of vein blockage there is large swelling;
- difficulties in any physical activity;
- pallor or bluishness of the skin;
- at the site of pathology, skin temperature decreases by 2-3℃;
- body temperature can rise to 40℃;
- increasing pain to unbearable;
- “referring” pain to the groin and pelvis area.
Important! To reduce the likelihood of a blood clot breaking off with subsequent thromboembolism, the patient needs to limit movement. Bed rest is recommended for up to 10 days; the affected leg should be higher than the body.
Prevention of chronic venous insufficiency
If you perform simple activities every day, the risk of developing CVI is reduced significantly. Even if CVI is discovered, treatment will not be so serious, especially in the early stages.
- You should lead a healthy lifestyle and play sports.
- Follow a diet.
- Wear comfortable shoes and use orthopedic insoles.
- Use elastic compression.
If the first signs of CVI still appear, you cannot postpone a visit to a phlebologist. He diagnoses the degree of CVI. Any delay in time is fraught with complications. Some of them are fatal. If the disease has nevertheless developed to a complex stage, you should not despair. Even complex cases can be cured using modern endovascular surgery, see the photo on our clinic’s website.
Frequently asked questions from our patients on the Internet
My legs are constantly swollen, how can I restore blood circulation in my legs? Maria from Arkhangelsk asks:
Dear Maria! To restore blood circulation in the legs, you first need to find out the cause of the swelling. As a rule, from a modern point of view, you need to start with an ultrasound duplex scanning of veins and consultation with a phlebologist.
How to identify blood clots in the legs? Oksana from Vladimir is interested in:
Dear Oksana! If you have the slightest suspicion of thrombosis, you should urgently seek medical help. A good diagnosis begins and always includes vascular ultrasound. This technique allows you to accurately determine not only blood clots in the legs, but also the cause of their occurrence. However, the method has a pronounced operator dependence, and it is better to trust professionals in their field.
How to understand that there are blood clots in the veins? Maxim from Yekaterinburg is interested in:
Dear Maxim! Only a specialist can reliably understand that there are blood clots in the veins, or exclude this situation. Thrombosis can be suspected based on the following signs:
- Swelling of the limb.
- Pain and/or redness.
- Feeling of heaviness and fullness in the limb.
- Vein thrombosis has already been previously diagnosed, since blood clots in the veins often recur.
The best solution would be to consult a phlebologist with an ultrasound scan of the venous vessels. You can make an appointment at our center for a consultation at any time convenient for you by phone.
How to check veins for blood clots in the legs? Asks Valentina from Smolensk:
Dear Valentina! You can check the veins for the presence of blood clots in the legs using ultrasound duplex or triplex scanning of the veins of the lower extremities at an appointment with a phlebologist.
How to treat chronic venous insufficiency at home? Zinaida from Tambov asks:
Dear Zinaida! Chronic venous insufficiency should be treated at home only after a good consultation with a specialist who will diagnose and give recommendations. Otherwise, you have a good chance of getting complications from the disease. When you find yourself on websites that colorfully describe how and what to treat at home, remember that most often professional doctors have nothing to do with such recommendations.
How to deal with the symptoms of chronic venous insufficiency? Nellie from Ufa asks:
Dear Nelly! It is better to start fighting the symptoms of chronic venous insufficiency in the legs before these symptoms appear, that is, with prevention: regular physiological exercise, a balanced diet, the use of compression hosiery for excessive loads, air travel. If signs of CVI appear: swelling, heaviness, varicose veins, you should consult a good specialist. This is the only way you can count on success.
PS I do not advise you to treat the symptoms of CVI at home via the Internet.
How to relieve pain from chronic venous insufficiency at home quickly? Asks Alexandra from Tyumen:
Dear Alexandra! The appearance of pain with varicose veins is most often a symptom of a developed complication, varicothrombophlebitis or deep vein thrombosis. If pain occurs due to varicose veins, stopping it at home is an extremely dangerous undertaking. It is necessary to quickly seek medical help, possibly calling an ambulance. You can quickly relieve pain with any NSAID, for example, ketoprofen or meloxicam (Movalis). But this is purely a temporary measure.
Varicose veins have started, what should I do? Maria from Nizhny Novgorod asks:
Dear Maria! If you have developed varicose veins or there are pronounced signs of varicose veins, you need to contact a professional. The most competent diagnosis and subsequent treatment can be provided to you by specialized centers for the treatment of venous pathology. After the examination, the center specialist will explain to you in detail what and how to do.
What is a good prevention for varicose veins on the legs? Nadezhda from Orenburg is interested in:
Dear Nadezhda! Prevention of varicose veins on the legs includes the following aspects:
- The closest to physiological load on the lower extremities, the involvement of the calf muscles, reducing the time of static load.
- Complete, balanced nutrition.
- For long-term static conditions and air travel, wear compression hosiery of I-II compression class.
Treatment of CVI
To treat pathology, a conservative method is used, if possible, and an operative one.
Conservative technique
Such therapy is possible when there are no irreversible changes in the veins. Treatment primarily involves wearing compression garments (knitwear), which creates a frame for the affected veins and prevents them from overstretching. It also increases blood flow through the veins, preventing the formation of blood clots.
Compression knitwear is knee socks, leg warmers, stockings, tights. It varies in compression strength. Selecting the optimal option individually is the task of a phlebologist.
Patients are also advised to lose weight if they are overweight and especially obese. Losing body weight means unloading the veins. When prescribing a diet, attention is also paid to the prevention of constipation in order to prevent constantly increased venous pressure.
The patient must be prescribed therapeutic exercises or exercise therapy. Swimming is especially beneficial.
In addition, drug therapy is carried out with the following types of drugs:
- angioprotectors;
- bioflavonoids;
- anticoagulants;
- local anesthetics;
- glucocorticosteroids.
An additional measure is external agents, that is, heparin-based gels and ointments.
Surgery
Radical method of treating chronic venous insufficiency. Indications for surgery are severe symptoms, pathological reflux, progression of trophic ulcers, low effectiveness of conservative treatment, pronounced progression of CVI.
Basic techniques:
- laser;
- surgical;
- ablative;
- bypass;
- phlebectomy, endoscopic phlebectomy.
Preparing for surgery
The patient undergoes a duplex scanning of the veins, as well as a standard examination, which includes:
- ECG;
- fluorography;
- coagulogram;
- general and biochemical blood tests;
- general urine analysis;
- blood tests for infections, group and Rh factor.
The test results are provided to the therapist. You also need to consult with an anesthesiologist.
Before the procedure, the patient should remove hair from the intended intervention area. The last meal is 4-6 hours before.
Progress of the operation
- Laser technique . Allows you to eliminate varicose veins and significantly enlarged veins. The affected vessel is irradiated from the inside with a laser at high temperature. As a result, its walls “stick together”, and gradually it completely disappears. No incisions are needed - just punctures. The procedure is carried out under ultrasound control.
- Surgery . To access the affected veins, several small incisions are made in the skin and soft tissue. The surgeon either completely removes the damaged vessel or ties the veins that connect the deep and superficial (in the area of the legs). Surgery is performed when the veins are significantly dilated.
- Phlebectomy . Removal of small veins. Several small incisions are made on the skin under local anesthesia, through which the doctor gains access to the affected vessel and removes it.
- Endoscopic phlebectomy . A microcamera is inserted into the vessel, allowing the doctor to remove the affected vein under visual control. The method is applicable when ulcers are present.
- Ablation . A flexible catheter is inserted into the vein. The heating electrodes, which are located at its end, thermally act on the venous wall, destroying it.
- Bypass surgery . An artificial vessel is used that connects the veins so as to allow blood flow to bypass the damaged area. Usually performed with the development of CVI and severe venous damage.
Rehabilitation
In the first days, swelling, hematomas and compactions in the affected area are possible. If stitches were applied, they are removed after 7-10 days.
From 1 to 2 months you need to constantly wear compression garments, and then - for the period recommended by your doctor - only during the day. Also, depending on the type and scale of the intervention, the patient is prescribed medications (primarily painkillers), physiotherapy, and exercise therapy. Walking at a calm pace is recommended.
Overheating of the intervention area and heavy physical activity are completely eliminated for about 2 months. During sleep, your legs should be placed on a slight elevation - about 15 cm.