Date of article writing: 08/19/2020 Quantity
()
Causes of pathology Symptoms of xerophthalmia Diagnosis Treatment Drug treatment Surgery Hardware treatment Prevention and recommendations
Dry eye syndrome (DES) is a pathological condition in which the conjunctiva and cornea are poorly moisturized. 10-20% of the population of our planet suffers from a similar problem. It occurs much more often in women (70% of cases) than in men.
The pathology is also known under other names - dry keratitis, dry keratoconjunctivitis, xerophthalmia.
Causes
The main reason is a decrease in the production of tear fluid and a deterioration in its quality characteristics. Because of this, it evaporates too quickly from the surface of the mucous membrane of the eye, and the remaining volume is not enough for good hydration.
There are a number of factors that provoke this phenomenon:
- Common diseases and syndromes. These are problems with the endocrine or genitourinary system, skin diseases or infections that disrupt the process of tear production.
- Eye diseases . The development of dry eye syndrome is caused by operations on the organs of vision, scars on the cornea or conjunctiva, neuroparalytic keratitis and similar pathologies.
- Age . Tear production may decline after age 40.
- Staying in a place with too dry air . The mucous membrane dries out faster when a person is in an air-conditioned room.
- Working for a long time behind a monitor screen, watching TV.
- Genetic predisposition.
- Pregnancy and lactation period.
If the syndrome appears due to dry air around, it is enough to make a damp compress or move to another room.
The most common reasons can be divided into several areas.
Special Conditions
This group includes body conditions that increase the evaporation of tears and reduce their production:
- Incorrect selection of compensatory drugs in the treatment of chronic diseases.
- Long-term use of antibiotics.
- Prolonged inflammatory process.
- Autoimmune conditions that cause connective tissue overgrowth. They lead to blockage of the lacrimal gland canals, which causes problems with the distribution of fluid throughout the mucous membrane.
With the dry eye effect, spontaneous lacrimation occurs. It partially compensates for the decrease in mucosal hydration.
Gadget screens
When you spend a long time in front of a TV, phone, tablet or monitor screen, the cornea gradually dries out. The screen emits a bright light that makes a person squint and look more closely at one point. This slows down the blink reflex, which helps moisturize the mucous membrane.
Dry air
An insufficient amount of moisture in the air leads to rapid drying of the mucous membrane of the eyes. Residents of apartments with central heating face this problem in autumn and winter. The batteries not only warm, but also dry the air. In summer, a similar effect is caused by air conditioning.
Hormones
The syndrome, caused by changes in hormonal levels, most often occurs in women. With the advent of menopause, the volume of estrogens in the body, which regulate fat metabolism, decreases. Because of this, the composition of tears changes, they become more liquid, are less retained on the surface of the mucous membrane, and moisturize it less.
Contact lenses
With constant wearing of lenses, the composition of tears deteriorates, the surface of the eyes dries out faster. Ideally, lenses should be worn only when necessary, alternating with glasses.
Laser vision correction
Exacerbation of dry eye syndrome may develop after laser vision correction. The reason is improper preparation, in which the patient was not tested for dry eyes, the Schirmer test. If indicated, the doctor should perform laser stimulation.
Medicines
Some drugs contain beta-blockers, anticholinergics and anesthetics, which contribute to dry eyes. The development of the syndrome can be caused by taking oral contraceptives and antidepressants. They affect hormonal levels, reducing the amount of fat in tears. This causes the tear film to become less stable.
To reduce the negative effects of medications, it is better to use moisturizing eye drops while taking medications.
Chronic diseases
Some chronic diseases, such as diabetes or conjunctivitis, cause dry eyes. In their treatment, drugs are used that disrupt the quality of tears. Blepharitis also negatively affects their composition.
The essence of the problem
Dry eye syndrome is changes that occur on the surface of the cornea and conjunctiva due to the absence or poor quality of tear fluid. As a result, the surface of the eye is poorly moisturized, which can cause discomfort, vision problems, and injury to the cornea and conjunctiva. This condition is not as harmless as it may seem. The frequency of its occurrence is very high. Among patients who see an ophthalmologist, this is one in three. Therefore, the manifestations of dry eyes cannot be neglected.
With dry eye syndrome, tear production decreases.
What are tears for? Right to cry! But the demonstration of feelings comes last. First of all, tears are needed for comfortable vision. A clear image, protection from germs, wind and dust - this is an incomplete list of what tear film provides. When it is disrupted, we feel constant discomfort. What is tear film and why is dry eye so relevant and has actually become a disease of modern humanity. By tear we mean both the tear fluid and the tear film. We can see the synthesis of this substrate with our eyes.
Tear fluid is formed and produced by the lacrimal gland. It is located at the top of the eye. It has ducts and through these ducts the tear fluid, like a shower, reaches the surface of the eye. This tear fluid is produced in large quantities. And its development depends on reflex reactions: on our joys and sorrows. You never know if something got into your eye. Then, when you literally need to wash it all with a shower, this liquid begins to be produced. When we talk about hydration of the ocular surface itself, we use the term tear film. But here everything is much more complicated. It is a liquid strictly oriented in space.
Here it is presented in a cross-section in the picture.
The very first layer that comes into contact with air is the lipid layer - these are fats. They are produced by the meibomian glands. Thanks to this layer, the cornea is shiny, very smooth and is one of the barriers to reduce the evaporation of the tear film. Then comes a layer of bound water. It is the largest in volume and thickness. And there is a mucin layer. Thanks to it, water is retained on the surface of the cornea. It seems to cling with the help of mucin to the epithelial cells covering the cornea. The cornea actually repels water because if water gets inside the cornea, it will develop swelling and a cataract.
And this very complex tear film “lives” for only 10 seconds. In fact, it is a full-fledged functional organ, but its lifespan is limited to 10 seconds. Imagine an arm, a leg that lives for 10 seconds. You used this substance and it was removed. To keep the tear film from thinning and the surface of the eye from drying out, the tear film is constantly renewed. It all depends on how aggressive the environment in which a person is currently located is. Normally this takes about 10 seconds. Then the eyelids blink and, like a car wiper, wash away all the remnants of the tear film. They go into the nose. And the wipers, washing off this film, apply a new one, renewing these 3 layers.
The role of blinking.
This is how we blink, we provide ourselves with vision. It turns out that if we remove the tear film, this thin anatomical structure, we simply stop seeing. Because it is thanks to this tear film that light, refracted, enters the eye and further forms an image on the retina. Those. This small structure is an important component of human vision.
This is why dry eye syndrome is one of the most important problems, although outwardly it is not so symptomatic. And there really isn’t even such a disease. However, this is a very serious condition.
The tear film covers the surface of the eye with a thin layer, serves as a lubricant between the eye and the eyelids, protects the eyeball from drying out, contains substances that nourish the cornea and protect the eye from pathogenic microbes. What happens when the physiological response that keeps the tear film stable is disrupted. Since this physiological reaction occurs every 10 seconds, when part of the lipid and water-mucin layer evaporates, a patch of dryness is slowly formed, and instantly, the signal goes to the brain and, by blinking, we moisturize the ocular surface.
The formation of the tear film is influenced by a very large number of different factors. If we are in an air-conditioned environment, the air currents cause this tear film to evaporate faster. As a result, the glands that form this tear film do not always have time to renew it, and this is a rather complex component. And over time, if this phenomenon continues, we will not be able to compensate for the required amount of components that form the tear film. So it turns out that either there are not enough tears, or they are “bad”, i.e. not all layers are represented in full, and such a tear film begins to dry out and evaporate faster. This results in symptoms of dry eye syndrome.
Here are some RISK FACTORS AND CAUSES that increase your risk of developing dry eye syndrome.
The effect of these factors is associated with either reduced tear production or increased evaporation of tears, which lubricates the ocular surface. As a result, the surface of the eye is poorly moisturized, which can cause discomfort and injury to the cornea and conjunctiva (“chafing”).
Conditions that promote faster evaporation of the tear film.
More often these reasons are typical for young people under 40 years of age:
- Professional reasons: people spend most of their time in front of all kinds of displays that are equipped with computers, mobile phones, televisions, and equipment.
- People with visual work have work that requires constant visual attention due to the fact that the gaze is constantly focused and blinking occurs less frequently. This also includes daily watching television, working with a microscope, with drawings, with small parts (for watchmakers).
- Long reading
- Long work on the computer, behind the monitor. In recent years, with the increase in the number of users of computers, gadgets, phones and other types of displays. Doctors have noticed this peculiarity: when looking closely at the screen, at any screen, of any size, of any quality, a person begins to blink less often. He is probably too focused, he enjoys looking at the image on the screen. And in this situation, by blinking less often, we leave the tear film without proper renewal. This kind of exhaustion will sooner or later also lead to the development of dry eye symptoms. If earlier we diagnosed this disease at the age of 50-55 years, now there are much more such patients, and they are much younger. We know the development of dry eye syndrome even in children. But in this situation, serious treatment is not required - just remove the gadget and everything is restored without any therapy.
- Driving for long periods of time, especially at dusk and at night;
- Improperly organized lighting in the room;
- Dry heated, dusty, air-conditioned, smoky, smoky rooms where air humidity is reduced. Such conditions dry out the tear;
- Long-term work associated with being outside in windy weather (construction workers, sailors), hot or windy climate. And also the use of hair dryers at hairdressers;
- Wearing contact lenses, using cosmetics. They disrupt the structure of the tear film;
- disruption of the squinting process, eyelids not closing properly (For example, with hyperfunction of the thyroid gland, which is called Graves' disease, as well as after eyelid injuries);
- Swimming in a pool with chlorinated water;
- after laser refractive surgery LASIK. Due to damage to the epithelium that covers the cornea, the tear film is not retained on the surface of the eye and evaporates faster.
The formation and replenishment of the tear film decreases more often in older people after 40 years of age:
- With age, the cells that produce tear fluid atrophy;
- Diseases (hypertension, diabetes, thyroid diseases, Parkinson's and Sjögren's diseases. With the latter disease, the secretion of not only the lacrimal, but also the salivary glands decreases);
- Taking diuretics and antidepressants, antihistamines, contraceptives;
- Hormonal background. Hormones regulate fat metabolism, as a result, the fatty layer of the tear film becomes thinner, and it evaporates faster.
- Vitamin A deficiency;
- The toxic effect of preservatives in eye drops used to treat other eye diseases, such as glaucoma, cataracts, conjunctivitis.
But all these factors were known to us before. But the problem is more complex than we imagine. And this is partly explained by the fact that for a long time, having a dry eye, a person does not realize it. He thinks about anything, but not about this disease, mistaking it for chronic conjunctivitis and treating this disease, although in this situation it is enough to properly moisturize the ocular surface, and you can minimize these symptoms.
Why is dry eye syndrome dangerous?
- • May lead to blurred vision, loss of vision, and formation of ulcers and erosions on the surface of the eye.
- • May lead to chronic infection in the eye
- • Surgical treatment may be required (impaired eyelid closure, trauma, perforation, corneal scarring)
- • Lacrimation in the initial stages
- • Poor tolerance to wind, cool air, smoke
- • Feeling of dryness, burning, stinging, irritation,
- • feeling of sand, itching, scratching, heaviness, “something got in the eye”
- • constant desire to blink, rub your eyes, close your eyes tightly, especially in the evening
- • Eye fatigue, blurred vision in the evening, photophobia
- • Difficult to drive in dark conditions
- • Difficult to put on contact lenses
- • Pressure behind the eye
- • Sensitivity to bright light
- • Redness, pain.
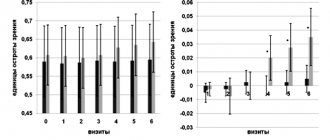
How do you know if you have dry eye syndrome?The OSDI Questionnaire presented below is used to assess the presence, severity of dry eye syndrome and the effectiveness of treatment. You can use this questionnaire yourself to determine whether you have dry eye syndrome or not. Other questionnaires are also used. The OSDI questionnaire has 3 blocks of questions, for each of which points are separately calculated in accordance with the table. Block 1: Have you experienced any of the following in the past week? Clinical symptoms Always Almost always Often Sometimes Never 1. Photophobia 4 3 2 1 0 2. Sensation of sand in the eyes 4 3 2 1 0 3. Sore and inflamed eyes 4 3 2 1 0 4. Blurred vision 4 3 2 1 0 5. Decreased vision 4 3 2 1 0 SUM OF POINTS FOR QUESTIONS 1-5: ____________________ (A) Unit 2. Have you experienced eye problems in the following situations in the last week? Clinical symptoms Always Almost always Often Sometimes Never Difficult to answer 6. When reading 4 3 2 1 0 7. When driving a car in the dark 4 3 2 1 0 8. When working at a computer 4 3 2 1 0 9. When watching TV 4 3 2 1 0 SUM OF POINTS FOR QUESTIONS 6-9: ____________________ (B) Unit 3. Have you felt discomfort in your eyes in the following situations over the past week? Clinical symptoms Always Almost always Often Sometimes Never Difficult to answer 10. In windy weather 4 3 2 1 0 11. In low humidity 4 3 2 1 0 12. In an air-conditioned room 4 3 2 1 0 SUM OF POINTS FOR QUESTIONS 10-12: ____________________ ( C) TOTAL SUM OF POINTS FOR ALL 3 BLOCKS OF QUESTIONS: A+B+C=D (D) TOTAL NUMBER OF UNANSWERED QUESTIONS (“I HAVE A HARD TO ANSWER”) (E) Then, using the sum of points received for all 3 blocks and the number of unanswered questions , you can determine the presence and severity of dry eye syndrome. Results: 0–9 points normal 10–39 points Mild dry eye syndrome 40–79 points Moderate dry eye syndrome 80–100 points Severe dry eye syndrome DIAGNOSIS Diagnosis of dry eye syndrome is relatively simple. You can find out how “dry” your eye is by measuring a piece of litmus paper moistened with a tear. This is called the Schirmer test. Normally it is 20 mm. With dry eyes it can decrease to 5 mm. • Defects in the tear film on the surface of the eye are detected by instilling fluorescent green-glowing drops and viewing under a special lamp. For example, in the picture below you can see that immediately after blinking, the entire surface of the eye is evenly covered with tear film, and later defects appear on the surface of the tear film in the form of uneven dark spots. • Despite the fact that the detection of dry eye itself is not difficult and is carried out in one visit to the ophthalmologist, nevertheless, firstly, in order to select the correct treatment, it is important to understand whether dry eye is an independent symptom or is it a manifestation of another disease, in particular thyroid disease or an autoimmune disease such as Sjögren's disease. In the latter case, to cope with dry eye, it is not enough to just moisturize the eye; you will also need to treat the underlying causative disease. Secondly, it is important to distinguish whether dry eye occurs on its own or is it superimposed on another eye disease, for example, conjunctivitis, chronic blepharitis. To understand these nuances and select the correct treatment and preventive measures specifically in an individual case, an examination by an ophthalmologist is necessary. And he, if necessary, will conduct additional research. Success in the fight against dry eyes largely depends on the ability of an ophthalmologist to determine the true causes of its occurrence and choose an effective strategy to combat it. If you know that you are susceptible to risk factors, if you have scored over 13 points on the OSDI scale, then you need to contact an ophthalmologist. How to PREVENT AND SLOW DOWN the development of dry eye syndrome? These measures are aimed at reducing the evaporation of tears from the surface of the eye. They can be divided into two groups: measures to care for the eye, and measures to correct unfavorable environmental conditions. Eye care measures • “Artificial tears”. To prevent dry eyes, doctors prescribe drops that replace natural moisture - tears. They are called “tear replacement drugs” or “artificial tears.” There are more than 40 drugs for the treatment of dry eyes in Russia alone, and there are more than 150 of them in the world. They differ in: • time of instillation (at any time of the day or only at night) • frequency of use (from 1 to an unlimited number of times a day) • possibilities applications with lenses (compatible or not) • presence and absence of preservatives in the composition • consistency (from liquid drops to viscous gels). Drops must be used more often than gels and ointments because they evaporate faster. On the other hand, gels and ointments are more viscous, so they last longer, but immediately after application they cause blurry vision, so they are not recommended for use by people who need to rely on their visual acuity, drivers, surgeons, and gels are preferably used at night before going to bed, when the eye is resting. • release form (tubes, droppers, bottles) • volume (single-dose and designed for many uses) • active ingredient (sodium hyaluronate, dextran, hypromellose) • price (from 150 to 1000 rubles). It is better to entrust it to an experienced ophthalmologist to choose the right product for you, taking into account your specific individual factors and lifestyle. If you use artificial tears more than 5 times a day, you should see an ophthalmologist to diagnose the cause of your condition. • Use eye drops that do not contain preservatives. For example, Hilo-Chest, which uses a special technology for manufacturing the Chest bottle, which prevents air from getting inside and prevents infection of the solution. • Contact lenses. Wearers with dry eyes benefit from highly hydrophilic contact lenses, which include hydrogel, silicone hydrogel, and hypergel lenses that are resistant to dehydration and deposits. low contact angle; good biocompatibility with eye tissues. The low wettability angle ensures that the lenses are sufficiently hydrated throughout the day. This means that they will attract tear fluid and will not disrupt the stability of the tear film. This is why it is especially important for people with dry eyes to select lenses together with an ophthalmologist, and not in optical shops. The doctor will be able to select lenses individually according to the curvature of the eye. When selecting lenses, the doctor takes into account the condition of the cornea, experience in wearing contact lenses, daily routine, work habits, concomitant diseases and other individual characteristics. Hydrogel lenses are lenses consisting of a polymer frame and water. They are comfortable to wear and the eye easily adapts to them. Most often, discomfort when wearing hydrogel contact lenses occurs in a room with low humidity or after working at the computer for a long time. Their disadvantage is their poor ability to transmit oxygen to the cornea, which does not have its own vessels and receives oxygen from the air and from the tear film. Therefore, these lenses are not suitable for you if you forget to take them off at night; they are intended for daytime use only. As for silicone hydrogel lenses, the silicone added to the structure of these lenses has high permeability to oxygen, while maintaining the advantages of hydrogel lenses such as high moisture content and wettability. Silicone hydrogel lenses are more comfortable for the cornea. Due to the presence of silicone, silicone hydrogel contact lenses are more rigid than hydrogel contact lenses. Therefore, they are more convenient to use. Due to the material structure of silicone hydrogel contact lenses, they accumulate less deposits compared to hydrogel contact lenses. This means a greater level of comfort and better quality of vision throughout the entire period of wearing contact lenses, and for people who sometimes violate the rules of care for contact lenses (for example, sleeping in contact lenses that are not intended for this purpose), it also means greater safety. Hypergel lenses are an innovative material of a new generation of materials that incorporate the best features of conventional hydrogel and silicone hydrogel lenses. The moisture content of the polymer is 78%, which corresponds to the moisture content of the cornea of a healthy eye. This phenomenal hydrophilicity ensures maximum eye hydration and wearing comfort for at least 16 hours, even in the most unfavorable conditions. In addition to a high degree of moisture, these contact lenses have a high oxygen permeability of 42 Dk/t, which meets the needs of a healthy eye when open. It is important to ensure that the use of these contact lenses and replacement intervals are approved or approved by the US FDA (and/or local regulatory authorities). All contact lenses must be prescribed by an ophthalmologist. • Use lenses that are replaced more frequently. Daily lenses are convenient because you do not need to use solutions for storing and cleaning lenses that contain preservatives, but simply put on a new pair, thereby reducing the risk of developing dry eyes. • Lens care products. Change your lens solution frequently. Use multifunctional and universal solutions that contain components that increase the hydrophilicity of contact lenses and promote their long-term hydration. For people with dry eye symptoms, peroxide systems are suitable for contact lens care. • Food. Use foods with omega-3 fatty acids. They are found in walnuts and fatty fish (for example, salmon, trout, tuna, sardines, anchovies). If you have a nut allergy or don't like fish, then you can use fish oil or dietary supplements or omega-3 vitamins. Omega-3 is involved in the formation of the lipid layer of the tear film, which reduces tear evaporation. • Eye care. Eyelid massage, warm compresses, baths, eyelid gel (Blepharogel) stimulate the sebaceous (meibomian) glands in the eyelids, which produce the lipid layer of the tear film, which will reduce tear evaporation. • Air humidification 50-60% (a humidifier and a hygrometer will help you with this). Also in winter, you can place a vessel with water near the heater. Measures aimed at eliminating provoking factors If you spend a lot of time at the computer, then take care of the convenience of work - use ergonomic solutions in the workplace - normalization of the work regime: • Conditions in the workplace. • correct posture: Use a kneeling chair to make it easier to maintain a straight posture when working while sitting. If you don't like using a kneeling chair, use a chair with wheels that has adjustable back and seat heights. • breaks Choose the frequency and duration of breaks for yourself. Recommended every 40-60 minutes. When working at the computer, take breaks of 10-15 minutes. (at least at 5!). Those. 40 minutes passed, we got up, walked around, looked out the window - 10 minutes passed, then we went on working. With this mode, your eyes will not get so tired. The free computer program EyeDefender will help you track this time, the main purpose of which is to display a screensaver at a certain interval of time. The time interval is set manually. When this time passes, the program will display “flowers” on the screen, no matter what application you are in. During this 10-15 minute pause, try to relax your eyes - to do this, do the following exercises: • It is best to go outside or go to the window and look into the distance. Then, after 20-30 seconds. turn your gaze to some flower on the window (or to an old mark on the window, some drop, etc.), i.e. no further than half a meter. Then look into the distance again, and so on several times. When you look into the distance, try to count how many branches there are on a tree or how many antennas are in the house opposite (or something else...); • Blink more often (this also applies to the time when you sit at the computer). When you blink, the surface of the eye becomes moist; • Make circular movements with your eyes (i.e. look up, right, left, down), you can also do them with your eyes closed; • By the way, it also helps to give vigor and reduce fatigue in general, a simple way is to wash your face with warm water; • • Comfortable position of the monitor: • install the monitor no closer than 40-70 cm from the eyes. If you are uncomfortable working at such a distance, then increase the fonts in the operating system. • Place the top edge of the monitor at eye level or slightly below. The screen should not be higher than eye level with correct posture. In this case, you will be looking at the monitor at an angle of 25-30%. • Try to position your monitor to avoid glare on the screen, or use a monitor with a matte rather than glossy finish. It is best to place the monitor sideways to the window. Do not place the monitor in front of a window. It is highly advisable not to place the monitor so that it receives direct sunlight from the window. Because of them, the picture becomes dim, the eyes strain, and begin to get tired. If there is no other way to place the monitor, then use curtains. • uniform lighting of the room during work reduces eye fatigue: if it is sunny outside, then turn off the lighting in the room; and vice versa, when it gets dark, turn on the lamps. Avoid contrasting room environments and light sources either behind or in front of the monitor. The illumination of the table with the keyboard and documents should be approximately the same throughout the work. It is advisable not to work in the dark: the room should be illuminated. If lighting is a problem in the room: install a small table lamp so that it can evenly illuminate the entire surface of the desktop. The photo below shows an example of how you can organize local lighting in a dark room if it is impossible to use general ceiling lighting. Don't forget to wipe off dust from your monitor. • If you wear glasses, use anti-glare glasses when working on a computer. • try to replace lenses with glasses when working on a computer • • Monitor settings. Many have noticed that if you work not at one monitor, but at several: then you can work at one of them for hours, and at the other after half an hour - do you feel that it’s time to quit and give your eyes a rest? Important monitor settings that affect eye fatigue: brightness, contrast, image refresh rate, screen resolution. • adjust the screen brightness, from minimum, gradually increasing, so that it matches the level of ambient light in the room, and is not higher or lower than this level. You can adjust the required backlight level by focusing on the white background of the text page. If it looks like a light source, then the brightness is too high. When it appears gray or faded, the brightness probably needs to be increased a little. • contrast. The higher the brightness and contrast at low light levels, the faster your eyes get tired. • refresh rate: set the highest possible image refresh rate on your monitor. On modern LCD monitors, it is usually 60 Hz. If the refresh rate of the LCD monitor is low, then rapidly changing images are blurred (lose clarity). In office applications and graphic editors, a frequency of 60 Hz is sufficient. This allows you to reduce image flickering and make the picture clearer. On some gaming monitors, the maximum refresh rate can be 144 or even 200 Hz. • monitor flicker reduction mode, • Most monitors allow you to adjust the color temperature manually. In dark rooms it is better to use warmer (yellowish) tones, and in good lighting - cooler (blue) tones. The factory setting usually produces a cool picture (high color temperature - 6500 K and above). In everyday life, we consider warm light more comfortable than cold light. It will be most comfortable to work on a monitor set to a low (warm) color temperature. White point D55 (5500 K) is quite suitable. This calibration may seem too yellow at first, but your eyes will quickly get used to it. To optimize the monitor's color palette, you can use special programs, for example, F. lux. It automatically adjusts the temperature based on the time of day and ambient light. • Set fonts of a convenient size in the operating system settings, select the monitor contrast • Use high-resolution monitors. It is better if the settings leave the “native” resolution of the monitor - the one for which the monitor is designed. If the resolution differs from that for which the monitor is designed, the image will be blurry, which will increase eye strain • https://www.lagom.nl/lcd-test/black.php link to check your monitor settings online • • change the view periodically Activities in your position • Wear windproof glasses if you have to be in the wind for a long time or ride a bicycle • dry eye syndrome is another way to quit smoking • Come in periodic prof. Examination at an ophthalmologist once a year • When is it worth consulting a doctor? • when there is no effect from preventive measures. • If, answering questions from the OSDI questionnaire above, the result showed the average or severe form of dry eye syndrome. Treatment is aimed at • Stimulation of the formation of tears, reducing inflammation • Compensation of insufficient amounts of tears (artificial tears) • Surgical treatment: blockage of lacrimal tubules. As a result, tears remain in the eye longer. Clogging of lacrimal tubules can be constant or temporary. Temporary blocking of tubules is used after surgical operations such as LASIK. In this case, traffic jams (obturators) are made from the material absorbing over time - collagen. Such obturators are absorbed in a few months. The constant blocking of the tubules is used in severe forms of dry eye syndrome, for damage to the lacrimal glands, when the production of their own tears is reduced (for example, with Shegren's disease). In this case, the obstructors are made of silicone or acrylic. They differ among themselves by viscosity. There are funds in the form of drops, gel and ointments. Drops must be used more often than gels and ointments, because they evaporate faster. On the other hand, gels and ointments are more viscous, so they operate longer, but immediately after application they cause vague vision, so they are not recommended to use people who need to rely on their visual acuity, drivers, surgeons, and gels preferably used at night Before going to bed, when the eye is resting. According to the mechanism of action of the main active substance, which is designed to hold moisture on the surface of the eye and moisturize it. The selection of a particular tool from the whole variety that is suitable for you, precisely for your eyes and in your situation, it is better to entrust an experienced ophthalmologist. Since, for example, one tool will be effective if the formation of fluid is reduced in the eye, and the other will give a greater effect if the loss of fluid from the surface of the eye is increased due to evaporation.
When tears do not sufficiently moisturize the eye, this MANIFESTS:
Features of the structure of the eye
In normal condition, the surface of the eyeball is covered with a special precorneal tear film, which protects the mucous membrane from harmful environmental influences, protects the conjunctiva and cornea from injury, and corrects minor optical defects.
The tear film is produced by special glands that are located along the edges of the eyelids. A violation of its structure causes dry eye syndrome, in which the cornea and conjunctiva begin to dry out, nutrients and oxygen do not saturate the tissues in sufficient quantities.
Because of this, patients experience discomfort and discomfort. As the syndrome progresses, damage to the cornea appears.
What signs and symptoms does a patient with dry eye syndrome exhibit?
Main signs of Dry Eye Syndrome
Even before the formation of any clinical manifestations and symptoms of dry eye syndrome, patients experience various subtle signs, which are often not given due attention and, moreover, are not always associated with eye disease. Also, these signs do not prompt patients to seek professional ophthalmological help. However, in conversations with their friends and acquaintances, patients often note fatigue, heaviness in the eyes, rapid fatigue when working with a computer or simply when reading, and also note periodic blurred vision. These precursors are subjective signs of the presence of serious problems in the ocular surface and mark the beginning of the development of dry eye syndrome.
Main symptoms of Dry Eye Syndrome
During the course of the disease, pathological changes occur in the tissues of the ocular surface, which leads to the formation and occurrence of persistent symptoms and characteristic complaints of varying degrees of intensity. At first, they simply periodically distract the patient’s attention, but, gradually intensifying in accordance with the course of the disease, they become a real painful, debilitating obstacle in everyday life.
Common symptoms include:
- tension and feeling of heaviness in the eyes;
- redness;
- itchy feeling;
- feeling of sand;
- sensation of a foreign body inside the eye;
- burning;
- decreased visual acuity (temporary or permanent);
- discomfort in front of intense light sources (photophobia);
- feeling of increased eye fatigue;
- double vision;
- pain (in severe cases).
These symptoms can worsen, creating serious difficulties in daily life, and also affect the psycho-emotional state of patients.
Development mechanism
The eye is moistened with tear fluid and a film covering the cornea.
The composition of tears is very complex, and the quality of hydration depends on its balance. A whole group of glands is responsible for the production, producing about 2 milliliters of fluid per day in a person who is in a normal emotional state. The tear film has three layers:
- Surface. It consists of fats that protect the film from excess moisture loss.
- Median. It contains tear fluid. Nourishes and protects the cornea, participates in the process of light refraction.
- Slimy. It is in close contact with the cornea and acts as the basis for the other two layers.
In addition to the system for producing tear fluid, there is a system responsible for removing excess moisture, which is based on the lacrimal canal. It carries tears into the nasal cavity. For this reason, when a person starts crying, his nose starts to run.
The outflow system nourishes the cornea of the eyes and promotes regular renewal of tear fluid.
What is the tear film and why is it necessary?
The tear film is a liquid, constantly renewed biostructure, which is part of the ocular surface, covers the cornea and performs important functions for the life of the eyes: optical, protective, immune, respiratory and nutritional.
The tear film is necessary for the proper, full functioning of the eyeball. Structurally, it is heterogeneous and consists of three layers. The tear film also has a very complex chemical composition, including water, numerous nutrients and special protective substances, all the necessary and balanced components for the normal functioning of the anterior surface of the eye. It also provides support for local immunity, antibacterial and respiratory functions. The tear film, leveling the surface of the cornea, provides its optical function and is a refractive medium, while having on its surface at the border with the air the highest refractive power of the order of 60D. In this regard, even minor disturbances in the tear film can greatly reduce visual acuity.
The amount of basic tear secretion per day is up to 2 ml, while the tear film has nothing in common with the tear produced by the lacrimal gland in a reflex state.
Need to know! The lacrimal gland provides only reflex lacrimation only for a protective purpose in response to physical or other irritation of reflexogenic zones (foreign body, volatile chemicals, thermal effects), as well as due to a psycho-emotional response.
The lacrimal gland is capable of secreting up to 30 ml of tears per minute, depending on the intensity of the irritating agent. Its secretion has a higher osmolarity and therefore moderately irritates the ocular surface and cannot replace the tear film.
Mucin layer of the tear film
The mucin layer is produced by goblet and granule cells, glands of Manz (limb) and crypts of Henle.
A gel consisting of mucin forms a smooth surface of the epithelium, facilitates the sliding of the eyelids along the cornea, cleanses and moisturizes the epithelium, and imparts hydrophilic properties to the epithelium.
The mucin layer makes up only 0.5% of the total thickness of the tear film. Its main task is to impart hydrophilic properties and adhesive ability to the primarily hydrophobic corneal epithelium. It is for this reason that the tear is held quite firmly on the cornea. In addition, mucin smoothes out all micro-irregularities of the epithelial surface and gives the cornea its characteristic mirror shine.
Aqueous layer of the tear film
The aqueous layer is the most prominent, produced primarily by the tear glands (95% of the aqueous component of the tear film), with the additional glands of Krause and Wolfring producing the remaining 5%. The aqueous layer consists of water-soluble electrolytes and organic low-molecular and high-molecular substances. Continuously updating, this layer ensures, on the one hand, the delivery of oxygen and nutrients to the epithelium of the cornea and conjunctiva, and on the other, the removal of carbon dioxide, metabolic products and exfoliated epithelial cells.
Lipid layer of the tear film
The lipid layer is produced by the Meibom glands located in the upper and lower eyelids. Normal meibomian gland secretion is formed from unsaturated fats, and its oleic acid content determines its melting point. When the amount of oleic acid decreases, the secretion hardens (compacts) due to an increase in the melting point of lipids and normal body temperature becomes insufficient to maintain lipids in a liquid state. Under the influence of body temperature, the meibomian glands become denser, causing secondary blockage of the excretory ducts, which leads to inflammation. The lipid layer prevents excess evaporation of the aqueous layer and gives the outer surface of the tear film a smooth appearance.
Classification of the syndrome
Dry eye syndrome can be divided into types according to pathogenesis. The syndrome can develop due to a decrease in the amount of tear fluid produced, due to increased evaporation of tears from the surface of the tear film. There is also a combined pathogenesis that combines both causes.
Based on the etiology, dry eye mucosa can be artificial, symptomatic and syndromic.
The syndrome is divided according to clinical manifestations. It may be accompanied by dry keratoconjunctivitis, recurrent erosions of the cornea or conjunctiva, and filamentous keratitis.
According to the severity of the manifestations, DES can be mild, moderate, severe and especially severe. During diagnosis, the doctor determines the degree of pathology, which depends on the severity of the symptoms.
Biological tear substitutes
Production and use of biological tear substitutes
for the treatment of dry eye syndrome is currently limited by the legal requirements of different countries for blood products, mandatory serological testing for the presence of human immunodeficiency virus, hepatitis and other infections, as well as the short shelf life of drugs of this group in compliance with a special temperature regime. However, despite these difficulties, biological tear substitutes also have a number of significant advantages in the treatment of dry eye syndrome. For example, autologous serum has a pH similar to that of the tear fluid, and also contains vitamins and biologically active substances (epithelial growth factor, nerve growth factor, etc.). In addition, the serum inhibits the release of proinflammatory cytokines, increases the number of goblet cells in the conjunctiva and stimulates mucin production [23, 24]. Today, many platelet-based drugs have also been developed for use in clinical practice: platelet-rich plasma; plasma enriched with growth factors; platelet lysate. According to the results of the study by JL Alio et al. instillation of platelet-rich plasma 4–6 times a day in patients with dry eye syndrome helps to reduce the symptoms of the disease by 89% after just 1 month. after the start of treatment [25].
The use of cryopreserved amniotic membrane in the treatment of dry eye syndrome stops the inflammatory reaction by inducing apoptosis of neutrophils and monocytes, reducing infiltration by neutrophils and macrophages. In addition, the ability of the amniotic membrane to stimulate the regeneration of corneal nerves due to the presence of nerve growth factor has been proven [26].
Symptoms
The main complaint is dry eyes. Discomfort increases with strong winds and prolonged stay in an air-conditioned room. Associated symptoms include:
- Cutting or burning. Appears due to increased sensitivity of the cornea when it is irritated.
- Feeling of sand in the eyes. The cause of the symptom is insufficient moisture of the mucous membrane.
- Decreased visual acuity, blurred objects. Occurs due to problems with the smoothness of the optical layer.
- Increased lacrimation. It is caused by the accumulation of tears in the cavity of the lower eyelids.
With prolonged manifestation of the syndrome, damage appears on the cornea. This leads to corneal erosion, filamentous keratitis and keratoconjunctivitis sicca. Deep wrinkles are observed as the patient begins to squint more often.
Diagnosis of dry eye syndrome
The causes and treatment are determined by an ophthalmologist. During the consultation, he examines the patient’s complaints, evaluates the symptoms and manifestations of the syndrome, and collects anamnesis. During the physical examination, the doctor examines the characteristics of blinking movements, the condition of the eyelids and the level of their closure. Using biomicroscopy, the condition of the conjunctiva, tear film and cornea is analyzed, and the height of the tear meniscus is determined.
To diagnose dry eye syndrome, a fluorescein test with a staining solution is performed. It helps to calculate the period of tear film rupture and detect areas of the cornea without epithelium.
The Schirmer test and the Norma test are aimed at studying the rate of tear formation and the rate of film evaporation. During a full examination, the doctor studies crystallography and osmolarity of tears, and performs cytology of a conjunctival smear. The patient needs to undergo testing for hormones and immunity if there are systemic diseases or diseases of the endocrine system.
An ophthalmologist will be able to determine how to get rid of dry eye syndrome after receiving the results of all tests.
HOW THE “EYE-LIGHT” LASER WORKS
This is the only device with two patented technologies.
“OPE” - technology: this is the effect of polychromatic light, which, thanks to thermal impulses, normalizes the functioning of the meibomian glands. The area of light irradiation is the cheekbones and the periorbital region, thereby stimulating the contraction of the glands, increasing the volume of lipids entering the tear film and reducing its tendency to rapid evaporation. LIGHT MODULATION technology: This is a unique photobiomodulation technology used for many years in various fields of medicine (dermatology, dentistry, etc.). A beam of light of a certain wavelength causes endogenous heating of the eyelids, which facilitates the softening of the fatty secretion contained in the meibomian glands and its evacuation to stabilize the lipid layer of the tear.
Treatment of dry eye syndrome
Can xerophthalmia be cured? Yes. An important role in the treatment of dry eye syndrome is played by the environment and the creation of comfortable conditions. For example, you need to monitor the air temperature in the room and its humidity level. To do this, periodically ventilate the rooms and use humidifiers.
In the early stages, the pathology is easily treated using traditional methods: eyelid massage, folk remedies or medications. In difficult cases, surgery may be required.
Traditional Treatments
To stabilize the film and balance the hydration of the cornea, the doctor eliminates the factors that cause dryness and prescribes medications.
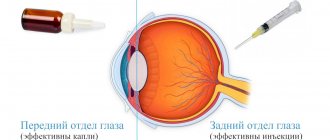
Most medications are ointments or eye drops (artificial tears), which contain electrolytes, carbomer or dexpanthenol. When prescribing drops, the doctor takes into account the course of the syndrome. For example, for mild cases, drugs with low viscosity are selected. As symptoms worsen, more viscous formulations are prescribed. The main disadvantage of drops when compared with ointments is their shorter duration.
Popular eye drops that are effective for dry eye syndrome include Gilan. The components of the drug reduce dryness, relieve eyes from irritation and fatigue. Its composition is similar to the composition of the intraocular fluid, so the body accepts the drops well.
Treatment methods depend on the course of the disease:
- Easy . Gel or water eye drops with low viscosity will be helpful. They moisturize and protect the cornea.
- Average . It is worth choosing gels or drops of medium viscosity. They have protective properties and help the mucous membrane to recover.
- Heavy . High viscosity formulations that form a strong film are required. It does not allow moisture to evaporate from the surface of the eyeball.
For complex therapy, you need to take vitamins, glucocorticoids, antihistamines and metabolic drugs. To select medications, symptoms are studied and treatment is tailored to solve specific problems.
Surgical methods of treatment
In difficult cases and in the absence of effectiveness of drug methods, the help of a surgeon is required to block the outflow of tears or tarsorrhaphy.
- Tarsorrhaphy is aimed at reducing the rate of evaporation of tears from the surface of the mucous membrane. To do this, the palpebral fissure is reduced.
- Blocking involves installing a special plug into the tear ducts or cauterizing them, which reduces the outflow of tears.
These are quite radical methods of treating dry eye syndrome, which are used only in extreme cases.
Eyelid massage
The procedure is performed by a doctor and may not be very comfortable for the patient. The eyelid is squeezed from the inside and gently massaged with a special glass rod. The process is controlled using a microscope. This enhances the production of tear fluid and moisturizes the mucous membrane.
Diagnostic examination for dry eye syndrome
Diagnostics
Diagnosis of dry eye syndrome should be carried out in a specialized ophthalmological clinic and include a number of professional tests, as well as specific diagnostic studies, based on the results of which the stage of dry eye syndrome is verified and determined. After this, the ophthalmologist prescribes the necessary physiotherapy and medication, as well as laser or surgical treatment individually for each patient.
In recent years, thanks to scientific research and the development of new devices, it has become possible to introduce into everyday ophthalmological practice a number of accurate diagnostic tests using the latest devices, which are indispensable in the diagnosis of dry eye syndrome and the proper correct assessment of the condition of dry eye syndrome.
Our clinic is equipped with professional equipment for specialized diagnostics for dry eye syndrome, which we use every day in our work to establish a diagnosis and monitor the therapy used.
Specialized diagnostic techniques for dry eye syndrome
It is impossible to assess the state of the secretory function of the ocular surface without diagnostic studies and specialized tests, on the basis of which modern diagnosis of dry eye syndrome is currently not possible. Among them are the main ones:
Digitized biomicroscopy
This is a diagnostic study that involves the study and subsequent clinical assessment of the anterior structures of the eye and eyelids using a slit lamp with an effective optical and computer system of digitized images at maximum resolution. Also, during the study, additional staining of the tear film, conjunctiva and cornea is carried out, which makes it possible to assess the severity of changes in the ocular surface and identify the presence of abnormalities in the tear film and secreting glands.
Meibography
This is a necessary and very important diagnostic study, which allows us to evaluate the morphology of the meibomian glands, which produce lipid secretions for the full formation of the tear film. In our clinic we perform this study using a special Me-Check device (Italy) for photomeibography. The device allows you to determine the state of functioning of the meibomian glands and set the degree of their dysfunction from 0 to 4 on the Meyboscale by Dr. Heiko Pult in a few minutes without additional devices and contrast agents. This study is also carried out at the stages of treatment in order to determine the effectiveness of the therapy used.
Interferometry of the tear film
It is an important diagnostic method for studying primarily the tear film, its quantity, composition and distribution, as well as the quality of tears. This technology also allows the assessment and study of the lipid layer of the tear film and its formation and distribution, providing extremely detailed images of the tear. The procedure is non-invasive and lasts less than five minutes. Before undergoing the interferometer test, patients are advised to remove contact lenses at least 48 hours in advance, not to use oil-based cosmetics around the eyes, and not to rub their eyes before the test.
Tear Film Osmolarity Test
This test is necessary to determine the total concentration of all dissolved particles in the patient's tear film. This is a very precise threshold value, which is 316 mOsm/L. By analyzing a sample of the patient's tear film using a special osmometer, we can identify not just deviations in the level of osmolarity, but in fact, disturbances in the body's ability to regulate the homeostasis of the tear film, which is the basis for the pathogenesis of the development of dry eye syndrome. Accordingly, the higher the osmolarity, the more concentrated the tear is and the more it can cause damage to the ocular surface.
The I-PEN® Tear Osmolarity System is a diagnostic device for quantitatively measuring the osmolarity (concentration of dissolved salts) of tears in normal and ocular patients.
Otto Schirmer test, or quantitative assessment of tear production
This diagnostic test allows you to determine the quantitative function of the secretory apparatus of the anterior surface of the eye, which is necessary for its proper hydration. The test is carried out within 5 minutes. The normal secretion rate is at least 15 mm of the test strip. The test is carried out both with the use of an anesthetic (to determine the basic secretion) and without (to determine the reflex and basic secretion).
Lipcof test
This test is quite informative for diagnosing dry eye syndrome. Over time, with dry eye syndrome, friction occurs between the eyelids and the surface of the eye, due to which the tension of the conjunctiva decreases and its folds are formed parallel to the eyelids, depending on the number and severity of which the severity of this symptom is assessed.
Norn's Test
This is a diagnostic test of tear dysfunction in which the breakup time of the tear film is determined after fluorescein staining to assess the quality and stability of the tear film in a blue filter at the slit lamp. If the patient being examined is in the age group from 16 to 35 years, then the normal time for the tear film to break up for him will be 21 seconds after the last blink. With age, this time decreases. For example, if the patient's age ranges from 60 to 80 years, then a tear film breakup time of 11-12 seconds would be considered normal.
Meniscometry
It occupies a special place in the diagnosis of dry eye syndrome. This is a measurement of the tear meniscus (tear rivulet) between the surface of the conjunctiva, the cornea of the eye and the edge of the lower eyelid. Its height is on average 0.4 mm. Changing its height has important diagnostic significance. Measuring the radius of curvature of the tear meniscus can be helpful in diagnosing dry eyes.
Test to determine the presence of inflammation
InflammaDry test is very convenient to use. This test examines a small sample of the patient's tears taken from the conjunctival fornix of the lower eyelid. This test detects increased levels of MMP-9 (matrix metalloproteinase-9) protein. This inflammatory marker in the tear film of patients provides tremendous information about the presence of inflammation of the ocular surface. In most cases, inflammation is present before clinical symptoms of the disease appear, so identifying dry eye disease at the preclinical stage using this test will allow it to be treated at an earlier stage. This test is also indicated before any ophthalmological operations in order to avoid complications in the postoperative period, as well as increase the safety of the rehabilitation period.
What additional studies and tests are prescribed for dry eye syndrome?
The mandatory complex when examining patients with dry eye syndrome includes examination of other parts of the eye to exclude the presence of concomitant pathologies. Among these studies, we can note some general clinical tests that need to be prescribed to patients.
In some cases, tests may need to be ordered, such as a test that measures an iron-binding protein called lactoferrin. The amount of this molecule is closely related to tear production. Patients with dry eye syndrome have low levels of this protein. This analysis may be especially valuable for such patients, since this is one of the areas of pathogenetic treatment. It is also valuable to evaluate tears for the content of lysozyme, an enzyme that is usually found in tears.
Another necessary item is tests for a number of hormones. These are thyroid hormones, male and female sex hormones, as well as some others. Many studies have been conducted that have proven the relationship between the condition of the tear film and the hormonal status of the patient.
How to hide the appearance of dry cornea?
With dry eye syndrome, the eyes often become red, the surrounding skin flakes and swells. This makes the patient look sick and tired, which can raise questions among others. What to do in this case?
There are a number of medications designed to improve eye health. For example, Gilan drops, which contain hyaluronic acid. It nourishes the mucous membrane, saturates it with oxygen and beneficial microelements. Regular use of the composition reduces irritation and dryness, and reduces the feeling of fatigue.
You can reduce the appearance of dryness and redness with the help of moisturizing preparations that have a vasoconstrictor effect. However, they have a number of contraindications that make their use impossible. These include infectious diseases. Drops of this group cannot be used for more than 4 days in a row.
To mask the symptoms, traditional medicine aimed at reducing swelling under the eyes is suitable. They can be used more often, but their effect will be less pronounced. This point should be discussed with your doctor, who will determine how to treat dry eye syndrome.
To mask the symptoms, traditional medicine aimed at reducing swelling under the eyes is suitable. They can be used more often, but their effect will be less pronounced. This point should be discussed with your doctor, who will determine how to treat dry eye syndrome.
Prognosis and prevention
Prevention helps prevent the onset and progression of dry eye. To do this, you need to follow a number of recommendations:
- In rooms with dry air, you should use a special humidifier, which significantly reduces the risk of developing the syndrome.
- If you work for a long time behind a monitor screen, you need to take 15-minute breaks every hour. At this time, it is worth doing eye exercises, blinking rapidly. This helps moisturize the mucous membrane and restore muscle tone.
- When using contact lenses, you need to choose high-quality optics. It can be purchased after consulting an ophthalmologist in a specialized salon.
An annual examination with an ophthalmologist will be helpful. This will allow timely identification of the disease and determine how to treat dry eye syndrome in the early stages of its development.
Why does this disease develop?
The causes of dry eyes in a patient can be very different. Most often, this disease appears in older people (often women who have reached menopause), as well as those who suffer from arthritis.
Dry and tired eyes in young people indicate a disruption in the structure and stability of the tear film. The causes of symptoms are as follows:
- prolonged stay in a room in which an air conditioner or heater is operating, reducing air humidity;
- hot or windy climate;
- wearing contact lenses;
- vitamin A deficiency;
- taking diuretics and antidepressants, as well as drugs with decongestant, antihistamine, and contraceptive effects;
- smoking;
- thyroid diseases;
- eyelids not closing properly;
- Parkinson's and Sjögren's disease;
- disruption of the squinting process.
Risks and consequences of self-medication
Caution must be exercised when self-treating xerophthalmia. If it is caused by external factors that do not pose a danger to the body, home therapy will relieve the patient of unpleasant sensations.
However, there is a risk that symptomatic treatment of dry eye will hide the underlying disease. This will complicate its further diagnosis. Only an ophthalmologist can find out exactly what causes dry eye syndrome and how it can be cured.
The consequences include deterioration of health with uncontrolled use of eye drops. If almost any drops are suitable as a preventive measure and for daily moisturizing of the mucous membrane, then when treating the eyes, the issue of choice must be approached more seriously.
When selecting drops for the treatment of the syndrome, it is necessary to accurately establish the cause of the pathology and its stage. The duration of the course and the set of additional components included in the drops depend on this: soothing, antimicrobial, painkillers. It is difficult to choose a treatment regimen on your own, so patients usually opt for moisturizing drops and antiseptic ointment. This leads to gradual damage to eye tissue and destruction of the cornea, since these remedies are not effective enough.
In general, the main danger of self-medication is a more active development of the disease and greater severity of dry eyes.
Infections and late stages of dry eye syndrome
Xerophthalmia is sometimes a symptom of a serious medical condition, such as Sjögren's syndrome. If dryness is ignored, eye health can deteriorate significantly. Complications develop such as:
- Defect of the cornea in the form of recurrent microerosions. They regularly appear on its surface, causing discomfort to the patient.
- Conjunctival xerosis. The shine of the eyes disappears, plaques appear on the conjunctiva.
- Filamentous keratitis. Pathologies appear on the cornea in the form of pale threads that move along the surface of the eye during blinking. They irritate the mucous membrane, causing itching.
- Dry keratoconjunctivitis. Deformation of the conjunctiva and cornea develops. It is inflammatory and degenerative in nature.
- Deterioration of vision. When the syndrome develops, there is a risk of developing blindness.
Drivers should be especially careful when they have CVD. The pathology reduces concentration while driving and slows down the reaction.
Proper prevention and timely treatment of the syndrome minimize the risk of unpleasant complications. To quickly relieve dry eyes, try using hydrating drops with hyaluronic acid, such as Gilan.
How is DES treated at the Rassvet Clinic?
First of all, Dawn ophthalmologists will rule out other serious eye diseases that mimic the symptoms of dry eye syndrome and determine the true causes of the development of this condition.
Our doctors have all the necessary equipment for high-quality eye diagnostics. If the diagnosis of dry eye syndrome is confirmed, we will provide adequate treatment, depending on the degree of manifestation of the patient’s symptoms and complaints. We do not prescribe Emoxipin, Taufon and other “vitamins” for the eyes to maintain their health. In the case of treatment of severe forms of dry eye syndrome (Sjögren's syndrome and other concomitant diseases that provoke manifestations of dry eye syndrome), we involve related specialists (rheumatologist, endocrinologist, etc.) and use a multidisciplinary approach, which guarantees the patient the best result.