Trichomoniasis, also known as trichomoniasis or trichomonas urogenital infection, all terms are absolutely equal. It is a well-known sexually transmitted infection, which people are not very afraid of contracting, and there is an explanation for this - it is easily treated. But this is still a sexually transmitted infection, and like all infections of this localization, it can cause inflammation of the organs responsible for reproductive capabilities, and under unfavorable clinical circumstances, lead to infertility.
Trichomoniasis (trichomoniasis) is a sexually transmitted disease, and according to the law, you cannot obtain a medical certificate without testing for this infection. If you have ever had sex without a condom, you may have trichomoniasis. The fact is that in the vast majority of women it does not manifest itself in any way.
Among all those suffering from sexually transmitted infections, every tenth person suffers from trichomoniasis, and often other urogenital infections coexist with it. It is estimated that a little more than 150 million people in the world suffer from trichomonas infection every year; in Russia, in every thousand adult citizens there is one patient with trichomoniasis, and in recent years the incidence has been decreasing. True, no one can guarantee that this frequency of the disease corresponds to reality, because no more than half of those suffering from trichomoniasis come to doctors. The other half does not even suspect that they have the simplest microorganism Trichomonas vaginalis.
What is trichomoniasis?
We have already published material about trichomoniasis in general, now we will analyze in more detail what its characteristics are in women.
According to WHO, this disease occurs more often in women than in men. In our material you will find out what is the reason for this inequality. Trichomoniasis is a sexually transmitted disease (STD). This infection is the most common compared to other diseases in this group. The results of a WHO study on four sexually transmitted diseases for 2021 indicate that trichomoniasis occurs among women more often than other sexually transmitted infections - in 5.3% of all observations.
Figure 1. The causative agent of trichomoniasis is Trichomonas vaginalis. Source: isis325/Flickr
Since Trichomonas vaginalis does not survive outside the human body, in the vast majority of cases the disease is transmitted through sexual contact. Cases of infection of women through objects contaminated with the secretions of a sick person - hygiene products or underwear - are rare. Even less common are cases of infection with medical instruments due to non-compliance with disinfection rules. Transmission from mother to fetus is possible, but it is impossible to become infected with trichomoniasis through the mouth or rectum; the parasite dies there.
Where does Trichomonas come from?
At the end of the fifties of the last century, several international conferences were held to discuss where Trichomonas comes from in the reproductive tract. They decided that this single-celled organism can be obtained not only through sexual contact, but also from a bath bench or basin, and even from swimming pool water and just tap water, not to mention wells. Bath accessories were blamed because trichomoniasis was practically not detected in men due to the absence of clinical symptoms. If a woman complains of inflammation, and a man is fine, then apparently the woman “caught the infection” somewhere else.
Where can a decent and faithful woman become infected with a sexually transmitted infection? Of course, in a public bath, where she is completely defenseless. And at that time, personal bathrooms were very rare; citizens went to the baths to wash themselves. Another five-year-old mankind was convinced that Trichomonas brought into a family was not at all a consequence of the infidelity of one of the spouses, but evidence of a woman’s failure to observe personal hygiene. One good thing is that this misconception helped save the family, because the infection happened through “non-sexual” means.
But in the mid-60s, scientific proof of the extremely poor survival of Trichomonas outside the human body came from Soviet Estonia, therefore infection by any other method other than sexual intercourse is simply unrealistic. Trichomonas does not like sunlight and hot water, and is immediately killed by any antiseptic. Indeed, Trichomonas is so delicate, so demanding of the external environment that even in the secretion of the genital tract collected for the purpose of research, it often dies before it is brought to the microscope. Since that time, the disease caused by Trichomonas vaginalis has been recognized as a venereal disease.
The main route of transmission of Trichomonas in adults, of course, is sexual, but oral sex does not contribute to infection, in any case, they could not prove this possibility of transmission. A woman in labor with trichomoniasis can infect her child, more often this happens to girls. This route of transmission of infection is called vertical. And today, 2–17% of newborns have trichomonas vaginitis or, in the old way, colpitis inherited from their mother. It is quite possible, because tests are taken from pregnant women several weeks before giving birth.
At risk for trichomoniasis are citizens who have multiple sexual partners, workers in the illegal sex industry, drug addicts and HIV-infected people, socially disadvantaged people, in general, comrades. True, citizens are still actively using the idea of contracting trichomoniasis in the pool, the main thing is to get treatment, and let them decide for themselves how to explain the appearance of Trichomonas vaginalis to their partner.
Causes and causative agent of trichomoniasis
The causative agent of trichomoniasis is Trichomonas vaginalis (Trichomonas vaginalis) - a single-celled protozoan microorganism, pear-shaped, with several flagella. When infected, it causes inflammation of the genitourinary tract.
Trichomonas do not tolerate environmental influences well: they die from sunlight or exposure to air at temperatures above 40°C. They are easy to deal with; an antiseptic or a simple soap solution is enough.
Being defenseless in the external environment, Trichomonas feels comfortable in the vagina, especially if the acid-base balance is disturbed. The reasons for these violations include:
- problems in the functioning of the endocrine system;
- frequent change of sexual partners;
- bacterial contamination of the vagina;
- abortion;
- pregnancy;
- menstruation.
The intensity of the development of trichomoniasis depends on the menstrual cycle. Therefore, in the chronic asymptomatic form, relapses occur precisely after menstruation. This is explained by the fact that Trichomonas require organic iron for active life. It is found in abundance in menstrual blood. Decaying red blood cells are a valuable source of nutrition for pathogenic microflora. In addition, hormonal levels change during this period, and infectious agents are not so actively attacked by the immune system.
Trichomonas also need glycogen for nutrition - it is produced in excess in the vagina under the influence of estrogen. Men produce less of this hormone, and menstruation does not occur. The main reason for the more active development of the disease in women is the ideal vaginal environment for Trichomonas to live in.
How to prevent infection?
Trichomoniasis is a common infection caused by the protozoan microorganism Trichomonas. The reason for its occurrence is non-compliance with personal hygiene and culture of sexual relations. To prevent infection, you need to be careful when choosing partners, avoid casual relationships and use contraceptives.
Condoms allow you to protect the body not only from trichomonas, but also from other, more dangerous diseases. In addition, it is necessary to maintain genital hygiene - regularly wash your face and change your underwear. Preventing infection is much easier than treating it and getting rid of complications, so every woman who is sexually active needs to remember about protection and contraception.
Incubation period
Trichomonas enter the vagina through unprotected vaginal intercourse with an infected partner. From the moment of infection to the first signs of illness, it usually takes from 3 to 30 days. Once in the vagina or urethra, Trichomonas produce an enzyme that “looses” the tissue and helps the pathogen penetrate, weaken local immunity and change the acidity (pH) of the environment. As a result, inflammation of the urogenital area develops.
As in men, trichomoniasis in women is divided into three stages:
- fresh form – no more than 2 months;
- chronic form – over 2 months;
- Trichomonas carriage is a form that has no external signs, but the infection is present and is transmitted by the carrier through sexual intercourse.
The clinical picture of the disease depends on the pathogenicity of the pathogen and the reactivity of the body. Typically, the acute form is characterized by severe pain and profuse discharge.
The main symptoms in women with trichomoniasis:
- irritation, itching in the genital area;
- swelling, swelling of the labia minora and majora, perineum;
- unusual discharge, possibly with a strong, unpleasant odor;
- pain during sexual intercourse and urination.
Features of the disease during pregnancy
Since during pregnancy the acidity of the vagina is reduced, and the immune system is significantly weakened, trichomonas manifest themselves with clear signs, or an exacerbation of a chronic illness occurs. In this case, there may be several lesions at once. Affected:
- rectal mucosa;
- urethra and bladder;
- vagina.
When a woman becomes pregnant, the body begins to create conditions that will help protect the fetus from any negative external influence. Therefore, the immune system begins to work much more actively when any microorganism penetrates. Additional protective mechanisms are present from the moment of conception until the baby is born.
The possibility of infection depends on how far along the expectant mother is. From the first trimester, the body changes, the mucus in the cervical area becomes thicker and more viscous to prevent the penetration of bacteria and viruses.
Important! It is better to identify the disease at an early stage and then carry out full treatment than to face unpleasant symptoms and consequences of trichomoniasis. In acute cases, microorganisms can cause pathologies in the fetus, miscarriage or early birth.
Types and forms of trichomoniasis
Depending on the location of the inflammation, trichomoniasis can be divided into several types.
Vaginitis is inflammation of the vagina. The acute stage is characterized by burning, itching, liquid, foaming, copious discharge with an unpleasant odor. In the chronic form, there are no symptoms, but itching and unusual discharge occur periodically.
Vulvitis is an inflammation of the external female genitalia. In the acute period - redness and swelling of the genitals, labia minora, and clitoris. In the chronic stage there are no obvious manifestations, periodically there is minor itching and pigmentation of the skin of the genitals.
Vulvovaginitis is a combination of the first two types - inflammation of the vagina and external genitalia.
Figure 2. On the left - a normal vagina, on the right - with vaginitis. Source: CC0 Public Domain
Bartholinitis is an inflammation of the glands of the vaginal vestibule. In acute inflammation, narrowing of the excretory duct of the gland is possible. The outflow is disrupted, the contents accumulate inside. The gland enlarges, and a swollen, large protrusion forms on the affected labia.
Urethritis is an inflammation of the mucous membrane of the urethra. In the acute stage - pain, burning when urinating, frequent urges, unusual discharge. In the chronic form, there is pain at the end of urination and frequent urge, but there is no discharge.
Cystitis is inflammation of the bladder wall. In the acute stage - symptoms are similar to those of urethritis, but without discharge. In the chronic form - dull pain in the lower abdomen, which intensifies during urination or when the bladder is full.
If trichomoniasis rises “above” the vagina, it manifests itself as:
- cervicitis – inflammation of the cervix;
- endocervicitis - inflammation of the cervical canal;
- cervical erosion;
- endometritis - inflammation of the endometrium, the mucous membrane of the uterine cavity;
- adnexitis - inflammation of the uterine appendages.
Often the infection is multifocal in nature, i.e. At the same time, for example, the urethra and genitals become inflamed. Another feature of this disease is that Trichomonas can be a kind of reservoir for other microorganisms: gonococci (the causative agent of gonorrhea) or Treponema pallidum (the cause of syphilis). Therefore, quite often trichomoniasis is combined with other STDs. This complicates the treatment of concomitant diseases and causes their relapse.
Important! After treatment for trichomoniasis, it is necessary to be tested for other STDs, including HIV.
What is the threat of the disease?
Possible complications of trichomoniasis occurring in chronic form:
- cervical oncology
- complications of pregnancy (chorioamnionitis, early rupture of water, miscarriage, etc.)
- sexual disorders
- fallopian tube obstruction
- chronic inflammation of the uterine appendages, which leads to infertility
Trichomoniasis increases the risk of the following diseases:
- genital cancer in women
- mastopathy
- allergies
- diabetes
Symptoms in women
Low-symptomatic, sluggish forms and Trichomonas carriage play a major role in the spread of the disease. In this case, there are no symptoms, and the carrier considers himself healthy. In this case, Trichomonas are present in the vagina or urethra and are transmitted to other partners. The asymptomatic form is more often observed in men.
Trichomonas carriage is not an ordinary carriage of protozoa, but is a systemic infectious process where Trichomonas, masquerading as host cells, suppress the activity of the immune response. This means that asymptomatic carriers pose the greatest danger in the spread of infection.
Chronic trichomoniasis can occur unnoticed, with periods of exacerbations. Typically, an exacerbation occurs once a month, after menstruation. With chronic trichomoniasis, itching and pain are observed from time to time. Signs of the inflammatory process are mild or absent altogether. The manifestation of the disease depends on the state of the immune system. For some time it restrains the infection, but, under unfavorable conditions, the disease manifests itself as an exacerbation.
Symptoms of untreated trichomoniasis disappear over time, but trichomonas remain in the patient’s body and can be detected by laboratory methods.
Diagnostic procedures
Diagnosis of trichomoniasis is aimed at detecting the causative agent of infection in the patient’s body. The primary diagnosis is formed based on the results of a patient’s examination by a doctor and on the basis of existing complaints. Laboratory tests can determine the presence of Trichomonas in the body of men and women:
- microscopy of urethral smears;
- PCR testing;
- culture for microflora.
Diagnosis of trichomoniasis in men is difficult due to the asymptomatic form of the pathology. Often the presence of a pathogen in the patient’s body is revealed during in-depth examinations when planning a pregnancy by married couples.
Diagnostics
Source: Leif Hellmann/Pixy.org
Diagnostic measures consist of determining the clinical signs of the disease and identifying pathogenic microorganisms. Laboratory methods help in this.
Smear microscopy
If Trichomonas vaginalis is immediately detected using microscopy, no additional studies are required to prove infection; treatment is prescribed.
Bacterial culture of samples
Usually used for the chronic form. Using this method, you can not only detect Trichomonas, but also find out its sensitivity to various drugs.
Serological method
Identifies specific proteins that the immune system produces in response to an infection in the body.
PCR (polymerase chain reaction)
Detects Trichomonas DNA or RNA in patient biological material. One of the most accurate modern methods makes it possible to detect the infectious agent even in small quantities.
Important! If trichomoniasis is suspected, it is advisable to prescribe additional tests for HIV, syphilis, hepatitis B and C, as well as for the presence of TORCH infections (a group of infections dangerous to pregnancy and the fetus).
Diet and restrictions
Also, while taking medications, the specialist will recommend a diet and introduce some restrictions. In particular, recommendations may be of the following nature:
- Eliminate fried, fatty, spicy foods from the diet;
- Add fermented milk products that help restore lactobacilli;
- Strictly refrain from intimacy, since during treatment the flora is most vulnerable and there is a risk of getting an additional infection or fungus.
Following these recommendations will speed up treatment and achieve the best result with minimal discomfort to the body.
Danger during pregnancy
When pregnancy occurs against the background of chronic trichomoniasis, its exacerbation in the early stages is possible. If the infection is recent, then damage to the internal genital organs of a pregnant woman by trichomoniasis depends on the duration of infection. If infected before the formation of membranes, the danger of an ascending infection is high. Possible inflammation of the membranes and endometritis. In such cases, spontaneous abortion most often occurs.
If infection occurs after the formation of the membranes, an ascending infection does not develop. But during childbirth there is a danger of developing ascending trichomoniasis in the future. When studying the characteristics of Trichomonas infection in pregnant women, the possibility of ascending infection of amniotic fluid and embryonic membranes with subsequent infection of the fetus by T. vaginalis was established.
Trichomoniasis is an extremely unfavorable factor during pregnancy. It can cause premature birth, low birth weight and be transmitted to the baby through the birth canal.
Control smear
To ensure the success of treatment, a control test for trichomoniasis is carried out 2 weeks after antibiotic therapy. If the result is negative, the patient is completely cured; further observation by a doctor is not required.
If the result is positive, a second course of treatment is prescribed for a longer period. The doctor selects other drugs or increases the dosage of previously prescribed ones. If during treatment there were deviations from the recommendations (the patient did not take antibiotics, did not follow the dosage regimen or dosage), the doctor should be notified about this.
Treatment of trichomoniasis in women
Medication
Trichomoniasis is treated depending on the stage of the disease, location, degree of damage and other factors. In each case, the dose of the drug and the regimen are calculated individually by a dermatologist-venereologist.
Treatment is mandatory for all sexual partners of the infected person.
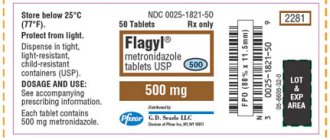
Typically, one of the 5-nitroimidazoles (5-NIMZ) drugs is prescribed - metronidazole, tinidazole and ornidazole.
They are effective and well tolerated. The effectiveness of 5-NIMZ is high - 80-100%. The drug is administered orally, that is, it is a regular tablet that you take with you. The active substance is poorly soluble, so intravenous injections of drugs are not given for trichomoniasis.
5-NIMZ do not act on other pathogenic organisms that are sexually transmitted - fungi, viruses, etc. Therefore, in case of cross-infections, combination therapy is prescribed.
During treatment, you should not drink alcohol - metronidazole and tinidazole are incompatible with it. They block enzymes that remove alcohol from the body, resulting in acute alcohol intoxication. Sexual abstinence is also recommended during treatment. Until complete recovery, this is dangerous in relation to other people, since the risks of further transmission of the infection remain.
Local treatment
To treat trichomoniasis, both general and local therapy are used. For example, vaginal suppositories: they act on the pathogen locally and increase the effectiveness of general treatment. If trichomoniasis is combined with other STDs, the doctor will supplement the treatment with local medications. They have a combined composition, depending on the type of coinfection. For example, a combination of metronidazole and miconazole (an antifungal agent).
Treatment of inflammation
Along with the main treatment, treatment of the affected area is indicated. Miramistin spray is used to treat the outlet of the urethra for urethritis. If you suspect an infection, it is better not to experiment with folk remedies, but to immediately visit a doctor and get recommendations for effective treatment.
Important! Self-medication for trichomoniasis is unacceptable. Trichomonas easily take on an atypical form, and then treatment will require much more effort.
A control test is taken 7-10 days after taking the last drug. Then repeat twice within a month. As a result of the therapy, it is not always possible to destroy all Trichomonas. In some cases, a repeat course is prescribed.
Folk remedies
You should not carry out therapy and select treatment for trichomoniasis on your own, and especially with traditional medicine. This will not only not help you recover, but also threatens with additional complications. Such treatment methods can only be used as an addition to therapy prescribed by a doctor. And even so, you should first consult, and not take risks and use traditional methods of treatment.
Treatment during pregnancy
Source: StockSnap/Pixabay
On the one hand, treatment of trichomoniasis during pregnancy is necessary. Promptly carried out therapy will contribute to the normal course of pregnancy, cleaning of the birth canal and the birth of a healthy child.
On the other hand, this task presents a certain difficulty due to the danger of harming the fetus with the active ingredients of the drugs. Therefore, drug treatment is not carried out in the first trimester of pregnancy.
In the second trimester, therapy with drugs of the nitroimidazoles group is prescribed, but only in the form of vaginal forms. This is due to the fact that the stratified squamous epithelium of the vagina has little absorption capacity. In this case, the drug acts on the pathogen, but not on the embryo. The American Center for Genetic Research has found that when metronidazole is administered orally, 100% of the administered dose is detected in the blood of patients, and only 2% when administered vaginally.
If local treatment is ineffective in the third trimester of pregnancy, metronidazole is prescribed orally. After completing the course of treatment, a control bacteriological analysis is carried out. Follow-up lasts 3 months. If all tests during this time are negative, trichomoniasis is considered completely cured.
Important! Treatment of trichomoniasis in pregnant women is possible only from the second trimester. In the first trimester, the drugs used for treatment are unsafe for the fetus.
Metronidazole is excreted in breast milk. If it is necessary to use the drug during lactation, it is recommended to stop breastfeeding. It is resumed at the end of the course, 48 hours after the last dose of the drugs.
Definition of disease
Sexually transmitted diseases are a serious threat not only to the well-being of each individual person, but also to the entire population as a whole.
The widespread prevalence of sexually transmitted infections threatens the reproductive health of the population, one of the main indicators of the effectiveness of the national health care system. According to WHO, 357 million cases of infection with gonorrhea, syphilis and other STDs are registered annually in the world, with the highest incidence rates observed in young people of reproductive age. In Russia, the absolute leadership belongs to trichomoniasis; in 2016, it was diagnosed in 55% of people with STDs. The situation can be aggravated by a frivolous attitude towards this infection: it may seem that this disease is very easy to treat and does not require a visit to the doctor. As a result of uncontrolled use of antibiotics, the disease actually loses the severity of its symptoms, but the destructive effect of the infection on the body continues. The insidiousness of trichomoniasis is also due to the fact that it is usually often accompanied by other diseases, which makes its diagnosis difficult.
In medicine, trichomoniasis refers to protozoal invasions, i.e. diseases caused by the entry of single-celled microorganisms into the human body. In an environment favorable for reproduction, pathogens begin to parasitize tissues and organs, causing the development of an inflammatory process.
Trichomoniasis was officially included in the group of sexually transmitted infections only in the middle of the last century, later than gonorrhea and syphilis.
Underestimation of the seriousness of the epidemiological danger of trichomoniasis is associated with the absence of symptoms of infection in every third woman and most men. However, even with an asymptomatic course of the disease, it negatively affects the reproductive function of both. The chronic form of the pathology without adequate treatment leads to the development of inflammatory diseases of the pelvic organs and serious complications during pregnancy.
According to research, the incidence rate in women looks like this:
- in the general population – 5-10%;
- among pregnant women – 13%;
- among patients who consulted a doctor with complaints of uncharacteristic discharge - 20-50%;
- among persons serving sentences in prisons and sex workers - 50-60%.
The trend in the incidence of trichomoniasis in Russia is similar to the global one. For example, among all requests for consultation with a gynecologist in women, from 20 to 40% of complaints are related to this infection, and in skin and venous clinics the number of such patients reaches 60%. The disease also leads among inflammatory lesions of the urogenital tract, for example, almost 35% of non-gonococcal urethritis is caused by the causative agent of trichomoniasis.
| Table 1. - Dynamics of trichomoniasis incidence per 100 thousand population of Russia for 2009-2015. | |||||||
| Age groups | Years | ||||||
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| Total | 144,7 | 126,8 | 111,4 | 93,9 | 82,0 | 69,8 | 62,9 |
| 0-14 years | 2,9 | 2,0 | 1,9 | 1,3 | 1,6 | 1,0 | 0,8 |
| 15-17 years old | 102,4 | 89,0 | 78,1 | 65,0 | 60,0 | 50,9 | 42,9 |
| 18-29 years old | 355,9 | 311,0 | 266,8 | 225,8 | 196,4 | 179,4 | 154,8 |
| 30-39 years old | 247,1 | 217,7 | 203,8 | 173,2 | 153,6 | 133,8 | 121,2 |
| 40 years and older | 70,4 | 62,7 | 56,6 | 49,0 | 43,0 | 36,3 | 34,7 |
The incidence and symptoms of trichomoniasis have strong gender differences. Women are three times more likely to become infected than men. But, if the asymptomatic nature of the disease is observed in half of the women, in men there are no clinical manifestations in 99 out of 100 observations.
Possible complications
Source: Shutterstock/FOTODOM
If treated incorrectly or untreated, trichomoniasis can lead to inflammation of the lining of the uterus or its appendages and cause complications. In particular, the formation of adhesions in the fallopian tubes - this can lead to infertility.
Doctors involved in the study of urogenital trichomoniasis (UGT) recommend that women with UGT be identified as a group at high risk for complications affecting reproductive function.
Questions and answers
Why is treatment for trichomoniasis necessary for both partners?
The incubation period of infection can reach several months. A negative test result for Trichomonas in one of the partners does not exclude the possibility that he is already infected. In this case, treating only one patient will lead to re-infection with trichomoniasis.
Is barrier contraception effective as a means of preventing trichomoniasis?
Yes. A man's use of a condom greatly reduces the risk of contracting the disease if he follows the recommendations of contraceptive manufacturers and observes personal hygiene rules by both partners.
Can you get trichomoniasis from using household items?
Infection is possible when a healthy person uses towels, underwear and bedding from a Trichomonas carrier. This pathology transmission route is common in younger age groups.
Prevention
The two main rules for preventing sexually transmitted infectious diseases are limiting the number of sexual partners and using a condom.
If unprotected sex was with a casual partner, it is necessary to treat the genitals with miramistin or chlorhexedine (0.05% aqueous solution) at the first opportunity. This is not recommended to be done regularly - frequent douching with these solutions can lead to vaginal dysbiosis. Sexually active people without a regular partner should regularly visit a dermatologist-venereologist.
How can you become infected with trichomoniasis: routes of transmission
The main cause of trichomoniasis is classical sexual contact; the disease is not transmitted by kissing. As for the domestic route of infection, such cases in the practice of doctors are very rare and are usually questioned.
The risk of infection through unprotected contact is up to 70%. When using a condom, the risks are minimal, but still remain - 10%. A condom is not an absolute protection, so if Trichomonas is detected, it is imperative to check your sexual partner, even if he does not have any symptoms of the disease.
Household transmission through shared towels, sheets or toilet seats is 98% excluded. Trichomonas are poorly adapted to existence in the open air and can live no more than 15 minutes outside the human body. According to statistics, the percentage of people infected through household contact does not exceed 2% of all infections.