Types of intrauterine devices
There is no one-size-fits-all IUD that has exclusive benefits and is best for all women. Each type has its own pros and cons, so it is better to choose it after weighing the pros and cons. Let's consider what types of intrauterine contraception are offered by manufacturers, why they are better than others, and what advantages and disadvantages they have.
Inert models
They belong to the first generation IUDs and, due to the large number of disadvantages, are rarely used in medicine. It is better not to use inert models, because... they often shift and can fall out unnoticed, therefore they have low efficiency and other disadvantages. In some countries, this type of IUD is prohibited for sale.
Disadvantages include a high risk of uterine bleeding and pain after installation. Inert models do not have any significant advantages, so it is better to consider other types of intrauterine contraception.
Copper types of IUDs
Intrauterine devices containing copper are of better quality than their polymer predecessors and do not have their disadvantages. Compared to any inert models, they provide better protection against conception. The contraceptive effect, depending on the design, lasts from 3 to 5 years. Copper IUDs are also better than polymer intrauterine devices because their insertion is painless and in rare cases causes bleeding.
Why is a copper IUD dangerous? Despite the advantages, over time, such an intrauterine device oxidizes and can cause any inflammation of the internal genital organs. This is its main drawback.
Having studied the question of which IUDs containing copper are better, we recommend the following models:
- Multiload;
- JunoBio-T;
- Nova T.
IUD with silver
To increase the service life and reduce any harm to intrauterine devices, manufacturers began to add silver to the composition of copper-containing models. Due to the content of this metal, silver types of IUDs are better than copper models due to their antibacterial and antiseptic properties. An additional advantage is the increased contraceptive effect - they can be used for up to 7 years. In some women, a silver IUD may cause allergies.
Based on all the advantages, the best intrauterine models containing silver are:
- Simurgh Juno Bio-T Ag;
- Vector Extra Ag;
- Novaplus T 380 Ag.
Golden spirals
This improved type of intrauterine device is created as an alternative to the silver IUD. Gold intrauterine devices are better than silver types due to their hypoallergenic and anti-inflammatory properties. They are not dangerous to the body, do not harm the reproductive system and do not cause any complications. An additional plus is that models containing gold are durable and last up to 7-9 years.
Having studied the question of which types of IUDs are better, intrauterine contraceptives have the greatest advantage:
- Goldlily Exclusive;
- Juno Juno Gold;
- Vector Extra Au.
Hormonal patterns
The latest generation of intrauterine contraception, which includes a hormonal drug. Once inserted, the intrauterine device releases small doses of progesterone, thereby providing better protection against conception. The amount of hormone released is minimal, so it does not cause any harm to the body. The validity period of this type of intrauterine device reaches 5-7 years.
According to doctors about which hormonal IUD is better, Mirena received the largest number of positive reviews. This type of intrauterine contraception is better than others, because not dangerous to the body, better than metal-containing IUDs and does not cause any complications after installation.
Classification
There are 2 groups of spirals:
- hormonal;
- non-hormonal.
Both perform the same task - protection from unwanted pregnancy. But some of them have additional properties. For example, hormonal IUDs are often used in gynecological practice as a way to treat certain diseases, and non-hormonal IUDs with the addition of silver or gold have a bactericidal effect and protect the female reproductive system from unwanted infections.
There are 3 generations of spirals:
1st generation
- An IUD without any metal or hormone, consisting only of medical grade plastic.
- Their contraceptive effect is achieved only through the mechanical impossibility of attaching the fertilized egg to the endometrium.
- Often cause complications (infectious diseases, ectopic pregnancy and prolapse of the IUD - expulsion).
1st generation IUDs are no longer used because more reliable and effective IUDs exist.
2nd generation
- IUDs containing metal. That is, these are spirals that also consist of medical plastic, but have a contraceptive effect due to additional components - copper, silver, gold.
- Metals act not only on the female body, but also on the male factor - sperm, and thereby reduce the risk of unplanned pregnancy.
3rd generation
- Hormonal IUDs, which at this stage are used as therapeutic and contraceptive agents.
Intrauterine devices have different shapes:
- T-shaped;
- round or semicircular;
- in the form of an umbrella;
- horseshoe-shaped (semi-oval).
Each spiral has its own advantages and disadvantages and is selected individually depending on the characteristics of a particular woman’s body.
All IUDs have the same operating principle – protection against unwanted pregnancy.
IUD Shapes: Key Differences
Intrauterine contraceptives also differ in design, each of which has certain advantages and disadvantages. Having studied the question of which types of IUD spirals are better, three forms of IUD are in greatest demand.
T-shaped models
The most common type of IUD. T-shaped intrauterine contraceptives are better than other types due to easy installation and convenient use. Thanks to the flexible shoulders, the device is securely fixed in the uterine cavity. At the end of the intrauterine device there is a thin thread (antennae) for quick removal. An additional plus is that it is better to install coils of this shape after a cesarean section or the first vaginal birth. T-shaped models do not have any particular disadvantages; the disadvantages include a small risk of expulsion.
Ring IUDs
The spiral in the form of a ring is best placed on women after several natural births. The main disadvantage of this type is the painful installation. Many people complain of discomfort when inserting an intrauterine contraceptive. When considering which form of IUD is better, the advantage of the ring-shaped spiral is the low risk of injury to the walls of the uterus after installation. It is not hazardous to health and does not cause any harm after administration.
Loop IUDs
Models of this form are best used after the first spontaneous birth/caesarean section. The advantages include painless insertion and a low risk of expulsion. Loop-shaped spirals are allowed for women with a non-standard structure of the genital organs, when it is better not to use the T-shaped model due to the high risk of prolapse. These IUDs do not have any particular disadvantages.
Does the spiral grow into a woman’s internal organs?
Women wonder whether it is possible for a contraceptive device to grow into the uterus. The answer is obvious: wearing intrauterine devices beyond the prescribed period of use will cause foreign bodies to grow into internal organs. The usual method of extraction will not work if the IUD has completely grown into the thickness of the intrauterine walls.
Symptoms of negative manifestation
Often women do not complain about their condition. However, ultrasound examinations, or a test to remove the IUD during prolonged use, may show that the contraception is securely fixed in the body, and the IUD begins to grow into the walls.
General symptoms:
- pain in the pelvic organs (bladder, lower back);
- dizzy;
- the woman feels very weak;
- the skin turns pale (indicates a puncture of the uterus and internal bleeding).
A woman experiencing these symptoms should consult a doctor immediately. According to statistics, such complications occur very rarely (1 case out of 50,000).
Pros and cons of intrauterine devices
The IUD is better than other types of contraception for the following reasons:
- long service life - from three years and above, depending on what type of spiral is used;
- reliable protection against unwanted pregnancy – efficiency reaches 99%;
- saving money - in comparison with other types of contraception, using an IUD is more profitable;
- lack of constant monitoring - after installation, a woman does not need to worry about taking pills or having condoms;
- restoration of fertility immediately after removal - pregnancy can be planned already in the first month after removal of the IUD;
- use as an emergency contraceptive - installing the IUD within five days after unprotected sex helps to exclude pregnancy;
- compatibility with medications – the IUD can be used in combination with any medications;
- the possibility of installation after childbirth and during breastfeeding - the contraceptive does not have any effect on the woman’s hormonal levels and is safe for the health of the child during lactation.
(see video after article)
Disadvantages of intrauterine devices:
- risk of injury to the uterine cavity or cervix when inserting an IUD - damage is possible due to improper installation technique or due to some chronic inflammation of the genital organs;
- possibility of expulsion – in order to prevent the intrauterine contraceptive from falling out, you need to regularly check its presence in the uterine cavity.
- an increase in the amount or duration of menstrual flow can lead to the development of anemia;
- the likelihood of ectopic pregnancy - occurs in rare cases when using metal-containing types of spirals;
- lack of protection against STIs - the IUD does not protect against any sexually transmitted infections, so it is better to install it if you have a regular partner;
To exclude any harm to health when using this type of contraceptive, it is better to visit your treating gynecologist before purchasing. He will conduct an examination, find out possible contraindications and determine which shape, type and size of the intrauterine device is better.
Who is the IUD not suitable for?
This is a very convenient method of contraception, suitable for almost everyone: women over 40 and young girls. If previously it was believed that the IUD could be placed only after childbirth, today gynecologists recommend it for nulliparous women. Use is also possible after a cesarean section, but only 3 months after the operation.
Due to the constant presence of a foreign body inside the uterus, the cervix is always slightly open, which means it is more accessible to pathogens. In this regard, the use of the spiral is contraindicated in case of inflammation or infectious diseases, including chronic ones.
Gynecologists do not recommend uterine contraception for women with acute and cancerous pathologies of the genitourinary system, as well as with severe heart and vascular defects.
Other contraindications include:
- previous ectopic pregnancy;
- cervical dysplasia;
- anemia and pathologies of hemostasis;
- diseases of the endocrine system, including diabetes;
- deviations in the structure of the uterus.
What side effects are possible with intrauterine contraception?
When studying the question of which types of IUDs are better, you need to become familiar with possible complications. They can appear immediately after the introduction of a contraceptive or during its use. More often, women complain of the following side effects:
- disruptions of the menstrual cycle;
- discomfort during sexual intercourse or during menstruation;
- heavy blood loss during menstruation;
- ectopic pregnancy;
- allergy to copper and any other components of the IUD;
- negative reactions of the body to the drug included in hormonal spirals.
If any of the complications appear after the introduction of an intrauterine contraceptive, doctors recommend removing it and better considering other types of birth control.
When should you see a doctor urgently?
If spotting or nagging pain in the lower abdomen appears, there is no need to panic. This is considered the norm. You should seek medical help if there is heavy bleeding or the pain is severe and does not go away. It is also worth visiting a gynecologist in the following situations:
- Body temperature has increased;
- A woman or man feels a foreign body during sexual intercourse;
- There is itching, burning inside or perineum;
- Purulent exudate is released along with the blood;
- The barrier contraceptive fell out.
More often, adverse reactions appear in women who have had infectious diseases.
Indications and contraindications
It is better to use intrauterine contraception:
- for patients who have already given birth after an abortion, if there is no inflammation of the pelvic organs;
- giving birth to women aged 35+ who refused to take oral contraceptives due to any of their shortcomings;
- women with a low risk of STIs who have a regular sexual partner.
Before installation, you need to study contraindications to the IUD. Otherwise, it may cause serious harm to health.
It is better not to use an intrauterine device in the following cases:
- infectious and inflammatory processes of the genital organs;
- allergic reactions to metal or a hormonal drug in the IUD;
- suspicion of pregnancy;
- vaginal bleeding under unclear circumstances;
- oncology or benign tumors of the genitals;
- anomalies in the structure of the female reproductive organs;
- chronic diseases of the pelvic organs;
- erosion of the uterine cervix.
Having studied which type of intrauterine contraception is best, you need to undergo a thorough examination by a doctor before installing an IUD. This will help eliminate any contraindications, disadvantages of intrauterine contraception and reduce the risk of causing any harm to health.
Recommendations after IUD installation
It is important to follow simple rules after the procedure:
- Refrain from intimacy for 7-10 days.
- Avoid physical activity, especially on the abs and pelvic floor muscles.
- Proper and thorough hygiene of the external genital organs to avoid infection.
10 days after installation of the barrier implant, you need to come for a follow-up examination. Doctors recommend periodic examinations over the next 3 months. This way, the gynecologist will not miss the possibility of complications, for example, caused by the displacement of the contraceptive.
Features of intrauterine contraception
The mechanism of operation of the intrauterine device depends on its constituent components. The contraceptive effect of copper-containing IUDs is achieved as follows:
- metal ions released by the IUD inhibit the activity of eggs and sperm;
- the viscosity of cervical mucus increases, this becomes an obstacle to sperm entering the uterus;
- The intrauterine contraceptive enhances the peristalsis of the fallopian tubes, which makes it impossible for the implantation of the egg even after its fertilization.
Hormonal types of IUDs are better than metal-containing models, because... additionally protect against pregnancy due to the thinning of the endometrium in the uterine cavity. Microdoses of the hormone secreted by the contraceptive inhibit the proliferation of mucosal tissue, which is why the egg cannot reliably attach to the uterine wall.
Contraception in perimenopause (clinical lecture)
Perimenopause is the phase of menopause after 45-49 years, including premenopause (transition to menopause) and 2 years after the last independent menstruation. Perimenopause is characterized by a progressive decline and cessation of reproductive function and menstrual cycles.Perimenopause is characterized by the following changes in the hypothalamic-pituitary-ovarian system:
- progressive depletion of the ovarian follicular apparatus,
- progressive decrease in the level of estradiol in the blood;
- decreased secretion of inhibin by the ovaries;
- progressive increase in FSH levels in the blood;
- reduction in the frequency of ovulatory cycles;
- decreased fertility.
A clinical reflection of altered ovarian function in premenopause is menstrual cycles, which can be characterized as follows:
- regular cycles until menopause;
- alternating regular cycles with prolonged ones;
- delays in menstruation (oligomenorrhea) from a week to several months;
- alternation of delayed menstruation of varying durations with metrorrhagia.
During 1 year of premenopause, the same woman may experience different endocrine characteristics of cycles: from ovulatory, or luteal phase insufficiency, to anovulatory: from normal estradiol levels to reduced or occasionally increased;
from normal FSH levels to elevated (more than 30 IU/l). Accordingly, in the endometrium there can be both a full-fledged secretion phase, hyperplasia, and endometrial atrophy, depending on the hormonal function of the ovaries in the period closest to the study of the endometrium.
In practice, we often have to solve complex problems during the perimenopause period, one of which is contraception. The difficulty of solving this problem is explained mainly by the woman’s age, at which the frequency of extragenital diseases increases and, accordingly, contraindications for pregnancy and various medications increase.
Contraception in perimenopause is an important medical and social problem that is often underestimated. This problem is especially acute for women over 45-47 years old, with regular menstrual cycles or alternating regular cycles with prolonged ones. It is often quite difficult to assess whether the ability to conceive has been preserved.
For sexually active perimenopausal women who do not want to become pregnant, the possibility of pregnancy remains high. R. Gray (1972) reported that 50% of women over 40 years of age are still potentially fertile. It showed that the annual risk of pregnancy is approximately 10% for the age group 40-44 years and 2-3% for women 45-49 years old, the risk is not zero for women over 50 years of age. It has been established that in women over 45 years of age with amenorrhea within a year, the possibility of restoring menstruation, even with ovulatory cycles, is about 10%. These data highlight the need for contraception before menopause and for more than 1 year after menopause.
The frequency of ovulation and sexual intercourse decreases by the age of 45 and older, however, some women may experience increased sexuality, and 30% of women aged 35-45 years have new partners, therefore, the occurrence of unwanted pregnancy exists.
There are certain rules in practice:
- ovulation may appear until menopause;
- regular cycles between the ages of 45 and 55 may indicate possible ovulation;
- changes in menstrual cycles such as oligo-, amenorrhea more often indicate anovulation;
- contraception should continue for 1 year after the last menstrual period for women over 50 years of age;
- Contraception should be continued for 2 years after the last menstrual period for women under 50 years of age.
The doctor is required to prescribe reliable, harmless contraception. There are many reasons to perceive contraceptive failure during perimenopause as a disaster:
- the frequency of maternal morbidity and mortality increases - 4 times higher in the fifth decade than in the third;
- the frequency of chromosomal abnormalities (especially trisomy 21) is proportional to the age of the mother; at 35 years old, the frequency of Down syndrome is 1:3000, at 40 years old it is about 1:100;
- antenatal screening includes the use of invasive methods (chorionic villus biopsy, amniocentesis);
- perinatal mortality doubles;
- the highest frequency of induced abortions over the age of 40 in relation to the number of pregnancies, and is 45% in Europe;
- the frequency of spontaneous miscarriages reaches 25-50% at the age of 40-49 years, which is often regarded as menopausal ovarian dysfunction.
Severe mental trauma occurs not only because a pregnant woman is faced with the need for examinations, but she must make a difficult decision - to continue or terminate the pregnancy.
She is of mature age and understands the sinfulness of the decision made to terminate the pregnancy. And if she is lonely, then often the fear of her secret being revealed is still prevalent. Sometimes single women may even experience suicidal thoughts. Such a woman often feels guilty before her teenage daughter, whom she recently reprimanded for her irresponsible attitude towards sex. She becomes upset and unhappy with the situation because she wants to continue her career, which she has worked so hard to achieve. She and her husband were planning a new free life “for themselves,” since the children had grown up and left home. There may also be social pressure, for example, among some African peoples, pregnancy is unacceptable for a woman who has grandchildren. Basic methods of contraception during perimenopause:
1. sterilization (male or female). 2. intrauterine devices (IUDs). 3. barrier methods (diaphragms, caps, spermicides, creams/gels, foam, sponges). 4. low-dose combined oral contraceptives (Femoden, Logest, Mercilon, etc.). 5. progestogens [mini-pills in tablets, long-acting injections (Depo-Provera) or with an IUD (Mirena)].
Sterilization
In many countries, sterilization is the most popular method of contraception. This method is recommended at the age of 35-45 years, provides a long-lasting effect, but this method can be considered relatively invasive for women at 45-50 years old, when fertility is already declining.
Surgical techniques for female sterilization include tubal resection, cautery, ligation, and the application of rings or clamps. The last three methods can be performed on an outpatient basis using a laparoscopic approach. Male sterilization (vasectomy) can be performed on an outpatient basis and does not require special facilities or infrastructure.
In developed countries, sterilization is used in more than 40% of married couples over 40 years of age. This method is chosen as the dominant one of all contraceptive methods. The effectiveness of female sterilization is 99.6%, second only to vasectomy (99.8%).
Sterilization does not protect against sexually transmitted infections.
Intrauterine devices (IUD)
Intrauterine devices (without gestagens)
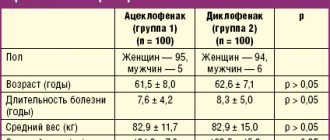
Modern IUDs are highly effective, long-lasting, and have no systemic side effects. Due to the high effectiveness of the IUD and the age-related decline in fertility, it is believed that if the IUD is inserted at the age of 35-40, then it should not be removed before menopause. There have been only a few studies on long-term IUD use in women aged 35-40 years. In Scandinavia, a randomized clinical trial compared Nova-T and Sopp-T-200 coils in 288 women. IUDs were installed in women over 35 years of age and the effects were studied for 5 years. Both devices were highly effective, safe, and genital infections requiring removal of the device were rare.
In another study, women were followed for 9 years after IUD insertion. In the group of women over 35 years of age, fewer coils were removed due to complications compared to the group of younger women. Similar results were obtained in a European prospective randomized five-year study, where it was noted that more often in the group of women under 35 years of age, the coil had to be removed due to bleeding, pain, and infection. Women in both groups (younger and older than 35 years) had previously had pregnancies. Older women usually experience more blood loss during menstruation than younger women.
The main problem with the IUD is that even without an IUD at this age, dysfunctional uterine bleeding may become more frequent. Therefore, if bleeding or pain occurs, it is best to remove the IUD. This is a kind of protection against anemia, etc. If bleeding stops after removal of the IUD, diagnostic procedures can be postponed to exclude organic causes. We believe that after 45 years of age, the IUD should not be used for contraception. If the IUD was inserted at the age of 35-40 years, then it is advisable not to remove it until menopause.
Levonorgestrel intrauterine system (Mirena)
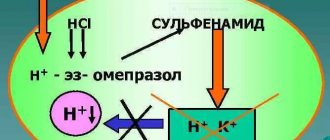
The idea of creating an intrauterine device that releases progestogen into the uterus was expressed in 1969 by T. Luukkanen (Finland). With the support of the Ford Foundation, the intrauterine hormonal releasing system was developed at the University of Helsinki in 1971. Levonorgestrel was chosen as a progestogen as it is an active, well-studied progestogen used in oral contraception for more than 20 years. It took years to find the optimal dose of levonorgestrel that would not block ovulation. The initial daily dose of levonorgestrel was 50 mcg and contributed to the inhibition of ovulation. Ultimately, the minimum optimal dose of levonorgestrel was determined to be 20 mcg/day.
This intrauterine hormonal releasing system is called Mirena. Levonorgestrel is released uniformly at 20 mcg/day. In terms of effectiveness, this method is equal to surgical sterilization, but is a reversible method. Mirena has an effect on cervical mucus, endometrium, the luteal phase of the menstrual cycle and gametes.
Under the influence of levonorgestrel, the water content in the cervical mucus decreases. The mucus becomes clumpy, which partially inhibits the migration of sperm through the cervical canal and thus provides a partial contraceptive effect.
Effect on the endometrium
Mirena has the main and most pronounced effect on the endometrium. Levonorgestrel is a derivative of 19-nortestosterone and has a pronounced effect on the endometrial stroma. In women using Mirena, the concentration of levonorgestrel in the endometrium is 1000 times higher than in the blood.
Mirena changes the sensitivity of the endometrium to estrogen. Despite the fact that Mirena does not block ovarian function (the level of estradiol in the blood is normal), the proliferation-stimulating effect of estrogen on the endometrium is still inhibited. Under the influence of intrauterine levonorgestrel, atrophy of the epithelium and a pronounced decidual reaction of the stroma occur.
Changes in the endometrium can be detected after 1 month of Mirena use; after 3 months, universal changes develop, which are similar after 1 year and after 7 years of Mirena use. These changes return to normal in most cases within 1 month after Mirena removal. The effect of Mirena can be achieved through its effect on estrogen and progestogen receptors, the number of which significantly decreases after 6-9 months of using Mirena.
Antiproliferative effect of Mirena during estrogen therapy
Andersson et al. [1992] were the first to report that Mirena has an antiproliferative effect on the endometrium, since no proliferation was detected in endometrial samples when estradiol valerate was prescribed for 12 months (2 mg/day). Similar effects were observed after 2 years of administration of 50 mcg of estradiol transdermally. The advantage of the combined administration of estrogens with progestogen (intrauterine) was the disappearance of scanty bleeding.
Effect of Mirena on the insulin-like growth factor-1 (IGF-1) system
It is believed that cyclic stimulation of the endometrium by estrogens is carried out through IGF-1, which is a kind of estrogen mediator. It has been established that Mirena stimulates the synthesis of protein that binds IGF-1, which, being in a bound state, cannot exert its stimulating effect on the endometrium.
The effect of Mirena on the luteal phase of the menstrual cycle
Ovulation is not blocked when using Mirena. Although the concentration of levonorgestrel released into plasma from Mirena is low, progesterone levels during the luteal phase of the cycle are lower than with neutral IUDs. Estradiol levels do not change with the use of Mirena. Consequently, levonorgestrel released from the IUD reduces the function of the corpus luteum.
Effect of Mirena on gametes
Removing the egg from the tube showed that while using Mirena, the egg does not divide.
Thus, the contraceptive effect of Mirena is achieved through the inclusion of multiple mechanisms. The effectiveness of Mirena is higher than that of copper-containing IUDs (NOVA-T), the Pearl index is 0.1 and 1.6, respectively.
Using Mirena has some benefits for perimenopausal women. Mirena effectively protects against pregnancy; its use reduces the amount of bleeding and increases hemoglobin levels. With a high concentration of levonorgestrel in the endometrium, the concentration of estrogen receptors decreases, and the sensitivity of the endometrium to ovarian hormones decreases. At the same time, the concentration of estrogen in plasma does not change, therefore, the risk of developing osteoporosis does not increase. After the introduction of Mirena, the menstrual cycle changes in almost all women; often in the first time after the introduction of the system, very scanty discharge is observed. Women over 35 years of age are more tolerant of such discharge than younger women. This discharge is observed more often during the first 3 months after the introduction of Mirena; after 1 year, amenorrhea occurs in 20% of women. Although the plasma concentration of levonorgestrel is low when using Mirena, side effects characteristic of progestogens may still occur: a feeling of tension in the mammary glands, headache, depression, acne. Usually these changes are temporary. In such cases, it is advisable to prescribe mastodinone (30 drops 2 times a day) or clamine tablets, a dietary supplement made from algae containing iodine.
With the use of Mirena, the incidence of ectopic pregnancy is 0.2-0.3 per 1000 women per year, which is lower than in women who do not use contraception.
Several studies have demonstrated that Mirena use reduces the severity of premenstrual syndrome and may reduce the size of uterine fibroids after 6-18 months of Mirena use.
If symptoms of menopausal syndrome appear during the use of Mirena, used for contraception in premenopause, estrogens can also be prescribed. When prescribed hormone replacement therapy (HRT), Mirena prevents the development of endometrial hyperplasia. If the Mirena system is used together with estradiol to reduce menopausal symptoms during perimenopause, then amenorrhea occurs in 83% of women after 12 months of use. Many postmenopausal women willingly agree to use Mirena, but its administration in postmenopause can be difficult due to atrophic changes in the cervix.
The pregnancy rate after Mirena removal is comparable to that without the use of contraception.
Contraindications for inserting Mirena are the same as for inserting any IUD:
- pregnancy or suspicion of it;
- bleeding from the genital tract of unknown origin;
- acute and chronic inflammatory diseases of the genital organs;
- abnormalities of the uterus;
- malignant tumors of the uterus;
- acute thrombophlebitis, acute thromboembolism;
- acute hepatitis.
Mirena is introduced after an appropriate examination on any day of the cycle.
Given the slightly larger size of the Mirena compared to a conventional IUD, local anesthesia and slight dilatation of the cervical canal are required. Control examinations after 1 and 3 months, and then a routine annual examination by a gynecologist. In conclusion, it should be noted that the IUD, a hormonal system, is one of the new highly effective methods of contraception for perimenopausal women, which also provides a therapeutic effect.
Combined oral contraceptives (COCs)
According to earlier studies, COCs were not recommended for women over 40 years of age, since their use increases the risk of thromboembolic complications and myocardial infarction. Recommendations were based on data from epidemiological studies. These studies are outdated because modern COCs contain lower doses of estrogens and progestins. The use of COCs is not recommended for smoking women over 40 years of age. However, non-smoking women in the absence of other risk factors for coronary heart disease can continue to use COCs up to 50 years of age if they are satisfied with this method.
The improvement of COCs went in two directions - reducing the dose of ethinyl estradiol and progestogen and improving the quality of the progestogen. In first-generation COCs, the dose of estrogen corresponded to 50 mcg, and sometimes 100 mcg. Subsequently, the dose was reduced to 30-35 mcg. The newest drugs of the latest generation contain 20 mcg of ethinyl estradiol, as well as the third generation of progestogens (gestodene, desogestrel, norgestimate) with low metabolic effects.
Case-controlled studies conducted in Denmark showed that the risk of thromboembolism in users of high-dose COCs is 2.9 (1.6-5.4), for low-dose COCs - 1.8 (1.1-2.9), in taking pills only with progestogens - 0.9 (0.4-2.4). These studies showed no difference with increasing age.
In Russia, of the registered COCs, Marvelon, Silest, Femoden, Logest, and Mercilon are the most indicated for perimenopause (see table).
A drug
| Compound | ||
| ethinyl estradiol, mg | progestogen, mg | |
| Marvelon | 0,030 | Desogestrel 0.15 |
| Silest | 0,035 | Norgestimate 0.25 |
| Femoden | 0,030 | Gestodene 0.075 |
| Logest | 0,020 | Gestodene 0.075 |
| Mercilon | 0,020 | Desogestrel 0.15 |
The mechanism of action of COCs is carried out by inhibiting the hypothalamic-pituitary-ovarian system and turning off ovulation. In addition, the endometrium undergoes rapid regression in the proliferation phase and premature secretory transformation. Peristalsis of the fallopian tubes slows down, making it difficult for the egg to pass through. Changes in the quality of cervical mucus make it difficult for sperm to move. COCs provide almost 100% contraceptive effect.
It is also important to note that COCs have a beneficial effect on a woman’s body. At the same time, a regular cycle is maintained, the risk of developing endometrial and ovarian cancer is reduced, aldodysmenorrhea disappears, the incidence of salpingitis, ectopic pregnancy, ovarian cysts, endometriosis is reduced, and in many cases the intensity of premenstrual and menopausal symptoms decreases. The use of COCs prevents the development of osteoporosis at the onset of menopause in women. It has been established that in those who previously took COCs, bone mineral density is higher at the age of menopause than in those who did not take them.
Ethinyl estradiol, which is part of COCs, has more pronounced estrogenic properties than natural estradiol used for HRT. Therefore, COCs also reduce menopausal symptoms.
We consider it necessary to focus on COC preparations containing extremely low doses (20 mcg) of ethinyl estradiol and the third generation of progestogens - Logest and Mercilon. Experience with these drugs in Russia has been intensively accumulated in recent years.
So, the dose of ethinyl estradiol in these two drugs is equally low, but the difference is in the types of progesterone. Logest contains gestodene (75 mcg), and Mercilon contains desogestrel (150 mcg). Unlike such precursor dosage forms as norgestimate and desogestrel, gestodene, which is part of logest, is characterized by almost 100% bioavailability. Since gestodene should not be converted into the active dosage form, its levels in the blood are more predictable and the risk of both insufficient and exceeding the optimal dosage is reduced. This is especially important for women of older age groups, who may experience a slight decrease in the rate of metabolic processes.
As the results of clinical and experimental studies have shown, gestodene has powerful antiovulatory activity, either alone or in combination with ethinyl estradiol. When using low-dose COCs, if you miss a pill, there may be a risk of a decrease in the contraceptive effect, especially if this happens at the beginning of the cycle (after a 7-day break in treatment). Therefore, with a decrease in compliance, the properties of the gestagen become especially important. The work of Van Heusden et al. (1998) showed that the level of 17b-estradiol in the blood was significantly lower on the 1st day of the cycle in the group of women who used Logest, i.e. a more pronounced inhibition of ovarian function was noted when compared with drugs containing other third-generation progestogens.
Due to a significant reduction in the dose of ethinyl estradiol (to 20 mcg/day), some concerns arose:
- ensuring reliable blockade of ovulation;
- quality of menstrual cycle control, since the appearance of spotting and breakthrough bleeding may reduce the acceptability of these contraceptives;
- influence on hemostasis, carbohydrate and fat metabolism.
Numerous multicenter studies have shown that Logest and Mercilon reliably block ovulation.
Isolated reports of pregnancy cases have been attributed to non-compliance with medication regimens. Blockade of ovulation was proven by determining the levels of FSH, LH, estradiol and progesterone for 6 months of taking both drugs, as well as by dynamic ultrasound of the ovaries and recording follicle growth.
In addition, it has been shown that Logest helps reduce the level of total and free testosterone and dehydroepiandrosterone sulfate by the end of the 3rd and 6th cycles of administration.
M. Gast and G. Grabb (1998) summarized data from 5 publications on the effect of low-dose COCs on the menstrual cycle. The frequency of menstrual-like reactions within 3-5 days ranged from 81 to 86% during the first 24 cycles. The frequency of menstrual-like reactions for more than 5 days decreased from 15.2% (before taking) to 10% by the 6-12th cycle and to 4.2% by the 36th cycle of taking COCs. The intensity of discharge decreased in 22.8% of women, and only 3.3% showed some increase in blood discharge. Amenorrhea occurred rarely, its frequency ranged from 0.4 to 1-3.1%.
The frequency of spotting was higher (8.6-11-31.7%) in the 1st cycle of taking low-dose COCs and progressively decreased (to 1.5-8-11%) in the 6th cycle of use. Similar data were obtained on the frequency of “breakthrough bleeding” - from 4.5-10 to 0.78-6% of cycles, respectively. According to the latest three-year data on the effect of Logest (670 women were examined), intermenstrual bleeding was observed in 10.2% of women by the 3rd cycle of taking the pill. By the 36th cycle of administration, their frequency decreased to 2.3%. The drug was well tolerated and rarely caused side effects. No clinically significant changes in body weight or blood pressure were noted. As a rule, the frequency of intermenstrual discharge decreased significantly by the 6th month of taking the drugs. Missing pills plays an important role, so it is extremely important for women to be clearly informed about the effect of skipping on ovulation and acyclic bleeding.
In a comparative multicenter clinical study, the effect of Logest and Mercilon on hemostasis was assessed. carbohydrate and fat metabolism. Both drugs have been shown to have minimal effects on both procoagulant and anticoagulant/fibrinolytic activity, as well as on carbohydrate and fat metabolism. The increase in factor VII activity was more pronounced with Mercilon than with Gestodene. The clinical significance of factor VII in women is unclear. Triglyceride levels increased to a lesser extent with 20 mcg ethinyl estradiol compared with 30 mcg ethinyl estradiol. The differences between both drugs were minimal.
However, it should be noted that, as a rule, all studies were conducted in age groups of women under 35 years of age. Therefore, extrapolation of these data to perimenopausal women should be done with some caution. Data on the response of perimenopausal women is only accumulating.
So, the advantages of low-dose COCs in perimenopause are their high effectiveness, in the prevention of menopausal symptoms, reducing the frequency of menstrual irregularities, estrogen deficiency, vegetative-vascular and atrophic processes and gynecological diseases, reducing the risk of osteoporosis, etc. However, one should remember about possible systemic side effects Therefore, it is extremely important to take into account the generally accepted absolute and relative contraindications for the use of COCs. It is extremely important to clarify that smoking is an absolute contraindication to the use of COCs during perimenopause.
Progestogens
With an increased risk of coronary artery disease, uterine fibroids, endometriosis, hyperplastic processes in the endometrium, mastopathy, it is advisable to prescribe progestogens: low-dose mini-pills, intrauterine systems with levonorgestrel (Mirena), high-dose MPA drugs (Depo-Provera).
Mini-pill
Mini-pills are oral contraceptives containing low doses of progestogens. This dose is 30% of the dose included in the COC. The mini-pill includes the following drugs: Continuin - 500 mcg of ethynodiol diacetate, Microlute - 30 mcg of lsvonorgestrel, Exluton - 500 mcg of linestrenol, etc.
Mini-pills change the composition of cervical mucus. The incidence of accidental pregnancy when taking the mini-pill in women aged 30 years is 0.8 per 100 women/years; by the age of 40 years and older, this figure decreases to 0.3 per 100 women/years. So, in older women, mini-pills are more effective than in younger women, since they are more likely to experience inhibition of ovulation. While taking the mini-pill, 30% of premenopausal women may experience amenorrhea, so it cannot be regarded as the onset of menopause.
Typically, women refuse to take the mini-pill due to frequent acyclic bleeding. At an older age, such bleeding is especially worrying for a woman and causes concern for the doctor; in such cases, additional examination is required.
Depomedroxyprogesterone acetate - DMPA (Depo-Provera)
DMPA suppresses ovulation. Endometrial proliferation decreases; 20-30 days after the first injection, the endometrium becomes thin and atrophic. Pregnancy develops very rarely. Most women experience acyclic bleeding; after a year, 50% of women have no bleeding, and the level of hemoglobin in the blood increases. When using DMPA, the risk of developing endometrial cancer is reduced and the incidence of salpingitis is reduced. Long-acting progestogens are highly effective, easy to use, and free of estrogen-dependent side effects. Gestagens are a real protection against inflammatory diseases of the genital organs: they have a beneficial effect on algodismenorrhea, premenstrual syndrome, anemia, mastalgia and help prevent endometrial cancer. However, they are not without drawbacks: the injection cannot be withdrawn, acyclic blood discharge, an increase in body weight, and a decrease in the level of antiatherogenic lipid fractions - high-density lipoprotein cholesterol - may appear. There may be a decrease in ovarian function and, accordingly, a decrease in estrogen levels can contribute to the appearance of symptoms of estrogen deficiency.
A natural question arises: when is it advisable to switch from using hormonal contraception to hormone replacement therapy?
Currently, it is accepted that this transition should be carried out at the age of 50-51 years. However, we cannot be sure that menopause has occurred. Therefore, it is recommended to discontinue COCs and after 4-6 weeks or more monitor the woman’s condition (absence or appearance of “menstruation” and symptoms of menopausal syndrome, indicating estrogen deficiency). If the blood FSH level is more than 30 IU/l, and the estradiol level is less than 100 pmol/l, then we can assume that menopause has occurred. Therefore, it is advisable to switch to hormone replacement therapy. It is extremely important to warn the woman that HRT does not provide a contraceptive effect.
Barrier methods
Barrier methods such as condom and spermocytes have some advantages as they do not cause systemic side effects and are an ideal defense against sexually transmitted infections. However, practice shows that couples who did not use condoms at a younger age often encounter difficulties later in life. This is explained by possible age-related changes in the vaginal mucosa and erection problems in men.
Natural Family Planning
There is no data on the effectiveness of the calendar method in perimenopausal women. Since the cycle of perimenopausal women is most often irregular, the use of this method is very difficult.
Summarizing clinical experience and literature data, we can conclude:
The use of contraception during perimenopause is indicated for regular menstrual cycles or when alternating them with irregular ones. Contraception is recommended for 12 months after menopause. In any case, the woman should be warned about the possibility of pregnancy. To avoid unpleasant surprises, a woman should remember this, and it is better to take another pregnancy test with hCG, measure basal temperature or perform an ultrasound. Preference is given to barrier methods, but at this age it is often difficult to start using condoms if there was no experience in reproductive age. Sterilization is too radical, but a reliable method for perimenopausal age; there are no problems when using hormone replacement therapy, as with hormonal contraception. If 40-year-old women have intrauterine devices, it is more advisable to remove them after menopause. Women can continue to take COCs after 40 years of age if they do not smoke and there are no other risk factors for the development of thrombosis and coronary heart disease. Depo-Provera reduces blood loss during menstruation, prevents the development of menopausal symptoms, and has a therapeutic effect in hyperplastic processes in the endometrium, fibroids, endometriosis and mastopathy. The minipill and depo-provera are effective as contraceptives, but acyclic bleeding may occur.
The Mirena levonorgestrel intrauterine system reduces menstrual blood loss. When hot flashes and night sweats occur, it is recommended to additionally prescribe oral natural estrogens: estradiol valerate 2 mg/day (Progynova), 17b-estradiol - 2 mg/day (estrofem) or estriol orally or vaginally. It is also possible to use parenteral estrogens in the form of a Klimar patch or gel (Divigel, estrogel).
Timely solution to problems - from contraception to hormone replacement therapy - is a real way to preserve women’s health, prevent trophic changes in postmenopause and maintain quality of life.
V.P.
Smetnik Scientific Center for Obstetrics, Gynecology and Perinatology, Russian Academy of Medical Sciences, Moscow
Review of popular types of IUDs - which model is better?
Below is a rating of the best types of intrauterine devices according to reviews from doctors and patients. Before purchasing, consult your gynecologist. Of all the types of intrauterine devices, only the doctor decides which is best for each patient after a thorough examination.
| Model | Design Features | Advantages | Flaws | Validity |
| Goldlily Exclusive | T-shaped spiral with a leg wrapped in copper and gold bimetallic wire | Anti-inflammatory effect, suitable for women with metal allergies, does not affect hormonal levels, long-term protection against pregnancy, low risk of expulsion | Contraindications: oncology, any infectious and inflammatory processes of the pelvic organs, pathologies of the uterus | 7 years |
| Nova T | T-shaped spiral, contains polypropylene, copper and silver | Painless installation, long-term protection against pregnancy, does not affect hormonal levels, can be installed during the postpartum period | Contraindicated for allergies to metals, cervical dysplasia, oncology, infectious and inflammatory diseases of the genital organs | 5 years |
| Multiload Cu-375 | F-shaped spiral with a leg wrapped in copper wire | Reliable fixation in the uterine cavity, does not affect hormonal levels, can be placed in the postpartum period, suitable for nulliparous women | Risk of allergic reactions, increased heaviness/duration of menstrual bleeding | 4-5 years |
| Juno Juno Gold | T-shaped spiral with a leg wrapped in bimetallic gold and copper wire | Long-term protection against pregnancy, anti-inflammatory properties, hypoallergenic, does not affect hormonal levels | Contraindications: endometriosis, cancer, inflammation of the genital organs, abnormal development of the uterus | 9 years |
| "Mirena" | T-shaped coil containing levonorgestrel in the core | Reducing the volume/duration of menstruation, suitable for women with endometriosis or fibroids, can be used for hormone replacement therapy | High price, possible intermenstrual bleeding, decreased libido, amenorrhea, dizziness, headaches | 5 years |
| Copper TCu 380A | T-shaped spiral, contains polypropylene and copper | Low price, long duration, does not affect hormonal levels, allowed for patients with inflammation of the appendages, ovarian dysfunction | Not suitable for women with copper intolerance, cancer, endometriosis, chronic inflammation of the pelvic organs | 10 years |
So, how does the IUD help prevent conception?
All spirals consist of medical plastic, which rarely causes an allergic reaction in women. But such cases do occur. For this reason, you need to carefully monitor your sensations and monitor the body’s reaction after installing the spiral.
In addition to medical plastic, modern spirals include:
- metals (silver, copper, gold);
- hormones.
Hormonal IUD
This type of IUD releases a certain amount of a hormone that affects not only the female body, but also reduces the activity of sperm. The spiral does not affect male potency or men's health! Only on sperm that have already entered the woman’s reproductive tract. The only noticeable disadvantage that intrauterine devices can bring to a man is the feeling of the antennae of the device during sexual intercourse. This issue can be easily resolved: you need to come to see a doctor, and the gynecologist will simply shorten the interfering tendrils of the spiral.
The hormone in the spiral affects the maturation and release of eggs by a woman’s ovaries and does not have a destructive effect on the hormonal balance as a whole.
The very presence of the IUD in the uterus prevents the attachment of the fertilized egg and, accordingly, pregnancy does not occur. This is a mechanical factor in preventing pregnancy. The coil also causes a local reaction, which has a detrimental effect on sperm, inhibiting and destroying them.
Hormonal IUDs affect many female diseases (endometriosis, uterine fibroids, etc.) and are recommended for use by gynecologists to treat the latter.
Non-hormonal IUD
As for IUDs containing metals, such designs, in addition to the mechanical factor of pregnancy protection inherent in all spirals, have a detrimental effect on the male factor. For example:
- Copper, oxidizing the environment, inhibits the movement of sperm that enter the uterine cavity and damages them.
- Silver and gold increase the shelf life of spirals and have a beneficial effect on local immunity, protecting a woman from inflammatory diseases of the pelvic organs.
All types of spirals have a stimulating effect on the fallopian tubes and enhance their peristalsis. While the fertilized egg is rapidly moving into the uterine cavity, the endometrium does not have time to prepare to accept a new life, and as a result, the embryo ends up in an unfavorable environment that is not suitable for further development.
To summarize, we can identify the links of fertilization that are influenced by any spiral:
- On the male factor (inhibitory and spermicidal effect).
- For the maturation and release of the egg from the ovaries.
- For the delivery of the egg and fertilized egg through the fallopian tubes.
- Attaching the fertilized egg to the endometrium.
- A local reaction that causes the release of enzymes that are harmful to sperm.
Methods for removing an ingrown helix
Using hyteroscopy, a gynecologist can see the overall picture of the patient’s condition. The diagnostic method is the most reliable. Further treatment tactics depend on how deeply the contraceptive is immersed in the wall of the uterus and the location of its location. Women wonder when removing an IUD: what to do when the IUD has grown into the uterus?
The choice of method for removing a spiral that has grown into the wall of the uterus depends on the location of the foreign object. It is quite dangerous if the spiral grows close to vital organs or blood vessels. For example, near the ureter or bladder, the removal process will not be an easy process and quite dangerous. This is due to the fact that the organ can be damaged. The fact that there is a clear need for surgical intervention by surgeons is undeniable.
In order to perform the operation efficiently, special laparoscopic forceps are used. This device is the only surgical option in this case. If it is observed using ultrasound that most of the IUD is located in the thickness of the uterus, then it’s time to think about removing it. Laparotomy will help in eliminating the IUD. If the spiral is not deeply embedded in the organ, then hysteroscopic forceps are used.
Advantages of using forceps:
- Tissues are little damaged;
- Bleeding is not as profuse as during surgery.
This is a special device that will allow you to get rid of a foreign object without using laparotomy.
Cost of some services in our clinic
| Medical abortion MIROPRISTONE (all medications, appointment with a gynecologist, ultrasound included) | 3300 rub. |
| Gynecologist appointment | 1200 rub. |
| Control ultrasound after medical termination of pregnancy | 1000 rub. |
| Gynecological ultrasound (pelvis) using Doppler techniques (transabdominal and transvaginal) | 1200 rub. |
VIEW ALL PRICES
UP
MAKE AN APPOINTMENT
[contact-form-7 id=”296″ title=”Untitled”]
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.
Doctors' recommendations
Despite all the advantages of intrauterine contraception, doctors recommend using it for patients who have already given birth and who have a regular sexual partner. For them, installing a spiral has no disadvantages and will not cause harm to health.
Doctors also warn that in the first days after insertion of the intrauterine device, a woman may experience slight bleeding and pain in the lower abdomen. These symptoms are considered normal, because the body needs time to get used to the foreign body. A month later, the gynecologist schedules a follow-up appointment, which helps eliminate possible complications and check the location of the device in the uterine cavity.
(see video after article)
It is recommended to remove the intrauterine device during the last days of your period. This will reduce the pain of the procedure and make the extraction procedure easier. The IUD is removed on an outpatient basis using special forceps. Of the minuses, it is noted that after removing the coil, a woman may experience muscle spasms and an increase in the amount of bleeding. Doctors do not attribute these symptoms to the shortcomings of the intrauterine device, believing that they are not dangerous to health.
According to doctors, the intrauterine device is a reliable means of contraception, but the method, with all its advantages, requires responsibility and more frequent medical examinations. By following all the recommendations of the gynecologist, you can not worry about disadvantages or health problems and can easily bear a healthy child in the future.