reflux disease
inhibitors
proton pump
stomach ulcer
Drugs from the group of proton pump inhibitors (proton pump) are widely used for the prevention and treatment of diseases of the gastrointestinal tract (including reflux disease ). Most often, medications from this group are prescribed for disorders of the acid-forming function of the stomach or in combination with drugs that stimulate the production of hydrochloric acid in the lumen of the stomach.
Pharmacological properties and general characteristics
Proton pump inhibitors are actively used in gastroenterology for the prevention and treatment of acid-related diseases of the stomach, esophagus and duodenum.
All representatives of this group of drugs belong to the group of benzimidazole derivatives, have a similar chemical structure and a similar principle of action. For certain diseases accompanied by an increase in the secretion of hydrochloric acid in the stomach, proton pump inhibitors are a panacea and effective prevention of the development of gastric and duodenal ulcers.
Participation of hydrochloric acid and enzymes in gastric digestion
Hydrochloric acid is produced by the parietal cells in the body and fundus of the stomach, creating an acidic environment that is optimal for the action of gastric juice enzymes. Under the influence of hydrochloric acid, inactive pepsinogen in gastric juice is converted into active pepsin.
Gastric digestion
Protein foods are mainly digested in the stomach - this is the first stage of gastric digestion of protein: swelling, coagulation (denaturation) of protein occurs, dilution of food by the multicomponent contents of the stomach and enzymatic breakdown (hydrolysis, digestion) of plant and animal proteins of food.
Gastric digestion converts proteins into polypeptides and oligopeptides, smaller protein particles that are prepared for final digestion in the intestines by pancreatic enzymes. When a significant amount of undigested protein enters the intestine, the proteolytic action of enzymes secreted by the pancreas (trypsin, chymotrypsin, etc.) and the intestinal wall (polyamino- and dipeptidases) may be insufficient. On the surface of the villi of the small intestine, parietal hydrolysis of the protein occurs, the formation of amino acids and their immediate absorption into the blood to participate in the synthesis of protein structures in the human body, reducing body weight.
Along with the lack of digestion in the stomach and absorption of protein products in the upper intestinal tract, their transfer into thick porridge, where they are used by bacteria, increases. The process of bacterial breakdown of protein and amino acids (rotting) is accompanied by the formation of substances (proteinogenic amines - histamine, cadaverine, etc.) and aromatic compounds (indole, skatole, etc.). The neutralization of these compounds occurs in the liver. With excessive formation of protein decay products in the colon, bloating (flatulence) occurs, and general intoxication of the body with these substances may occur. A complex violation of the first stage of protein digestion in clinical practice is observed after gastric surgery (gastric resection), when 2/3 of the stomach or the entire stomach is removed, thus eliminating or sharply limiting the secretory function of the stomach and the partial flow of protein into the intestine. Gastric juice has a bactericidal effect on the microflora of the stomach and intestines.
The stomach contents of 10% of healthy people are sterile due to the bacteriostatic and bactericidal effects of hydrochloric acid and lysozyme. When gastric secretion is preserved, it does not exceed 103 microorganisms in 1 ml of gastric juice; anaerobic microorganisms predominate. When aggressive and protective factors of the stomach are violated, the use of drugs (antisecretory and antacids) disrupts the microecology of the stomach and gastric dysbiosis occurs when the opportunistic flora becomes pathogenic, so according to data published in Gastroenterol & hepatol (2000 Mar), taking antacids leads to increased increase in the number of H. pylori, Enterobacter, Staphylococcus and Propionobacterium.
The use of antisecretory drugs that reduce the acidity of gastric juice (PPIs, histamine H2 blockers) promotes the penetration of infection entering the stomach with food, changes in the composition and quality of microorganisms in the stomach and excessive growth of microflora in the intestinal lumen due to the lack of the bactericidal effect of active gastric juice.
About the Castle factor
The antianemic Castle factor is produced in the stomach, and food iron is converted from trivalent to divalent, which is more easily absorbed in the intestines. Without Castle factor, vitamin B12 is not absorbed in the intestines and does not enter the bloodstream, but is excreted in the feces. Disorders of the microflora lead to a decrease in the formation of B12-like substances, and some representatives of the microflora fight for vitamin B12, which enters the body with food.
A decrease in the formation of Castle factor in the stomach leads to the development of B12 deficiency anemia. The source of B12 in the human body is only animal food (see article B12-deficiency anemia).
The administration of antisecretory drugs (usually proton pump inhibitors - PPIs) reduces the acidity of gastric juice and thereby complicates the transition of 3-valent iron contained in food into 2-valent iron, which is absorbed many times faster in the small intestine. Iron deficiency anemia develops. When iron is deficient, there is a lack of absorption of iron in the intestines, appetite decreases, the frequency of meals decreases, weakness and fatigue develop, and body weight decreases.
Hydrochloric acid regulates the production of gastric juice, so when the pH in the antrum of the stomach is equal to 3.0, secretion begins to inhibit.
Hydrochloric acid has a regulating effect on gastric motility and the process of evacuation of gastric contents into the duodenum.
Indications for use
Different generations of proton pump inhibitors are prescribed for the prevention and complex treatment of the following diseases:
- gastritis with high acidity ;
- in combination with the eradication of Helicobacter pylori;
- gastroesophageal reflux disease;
- Zollinger-Ellison syndrome;
- functional dyspepsia;
- structural damage to the gastric mucosa caused by prolonged or uncontrolled use of non-steroidal anti-inflammatory drugs;
- stomach and duodenal ulcers;
- long-term antibiotic therapy.
Drugs from the group of proton pump inhibitors are also actively used during general anesthesia, when it is necessary to avoid Mendelssohn syndrome (reflux of gastric contents into the respiratory tract or reflux disease).
Drugs from this group are available in dosage forms such as tablets, lyophilisate, capsules (including enteric soluble), powders for the preparation of infusion solutions and oral solutions.
Proton pump inhibitors
Proton pump inhibitors
(also called:
proton pump inhibitors, proton pump inhibitors, proton pump blockers, H+/K+-ATPase blockers, hydrogen pump blockers,
etc.) are antisecretory drugs intended for the treatment of acid-related diseases of the stomach, duodenum intestines and esophagus, blocking the proton pump (H+/K+-ATPase) of parietal cells of the gastric mucosa and thus reducing the secretion of hydrochloric acid. The most commonly used abbreviation is IPP, and less commonly, IPN. Proton pump inhibitors are the most effective and modern drugs in the treatment of ulcerative lesions of the stomach, duodenum (including those associated with Helicobacter pylori infection) and the esophagus, reducing acidity and, as a consequence, the aggressiveness of gastric juice.
All proton pump inhibitors are benzimidazole derivatives and have a similar chemical structure. PPIs differ only in the structure of the radicals on the pyridine and benzimidazole rings. The mechanism of action of various proton pump inhibitors is the same; they differ mainly in their pharmacokinetics and pharmacodynamics.
Mechanism of action of a proton pump inhibitor
Proton pump inhibitors, after passing through the stomach, enter the small intestine, where they dissolve, after which they first enter the liver through the bloodstream, and then penetrate through the membrane into the parietal cells of the gastric mucosa, where they are concentrated in the secretory tubules. Here, at an acidic pH, proton pump inhibitors are activated and converted into tetracyclic
| Mechanism of action of proton pump inhibitors (Maev I.V. et al.) |
sulfenamide, which is charged and therefore unable to penetrate membranes and does not leave the acidic compartment within the secretory tubules of the parietal cell. In this form, proton pump inhibitors form strong covalent bonds with the mercapto groups of cysteine residues of H+/K+-ATPase, which blocks the conformational transitions of the proton pump, and it becomes irreversibly excluded from the process of hydrochloric acid secretion. In order for acid production to resume, the synthesis of new H+/K+-ATPases is necessary. Half of the human H+/K+-ATPases are renewed within 30-48 hours, and this process determines the duration of the therapeutic effect of PPIs. When taking a PPI for the first time or once, its effect is not maximum, since not all proton pumps are built into the secretory membrane by this time; some of them are located in the cytosol. When these molecules, as well as newly synthesized H+/K+-ATPases, appear on the membrane, they interact with subsequent doses of PPI, and its antisecretory effect is fully realized (Lapina T.L., Vasiliev Yu.V.).
Types of Proton Pump Inhibitors
The Anatomical Therapeutic Chemical Classification (ATC) in section A02B “Antiulcer drugs and drugs for the treatment of gastroesophageal reflux” contains two groups with proton pump inhibitors. Group A02BC “Proton pump inhibitors” lists the international nonproprietary names (INN) of seven PPIs (the first six types of which are approved for use in the United States and the Russian Federation, the seventh, dexrabeprazole, is not approved for use):
A02BC01 Omeprazole A02BC02 Pantoprazole A02BC03 Lansoprazole A02BC04 Rabeprazole A02BC05 Esomeprazole A02BC06 Dexlansoprazole A02BC07 Dexrabeprazole
Esomeprazole, dexlansoprazole and dexarabeprazole are optical isomers of omeprazole, lansoprazole and rabeprazole, respectively, with greater biological activity. This group also includes combinations:
A02BC53 Lansoprazole in combination with other drugs A02BC54 Rabeprazole in combination with other drugs
Group A02BD “Combinations of drugs for eradication of Helicobacter pylori
” lists proton pump inhibitors in combinations with various antibiotics intended for the treatment of
Helicobacter pylori
-associated diseases of the digestive tract:
A02BD01 Omeprazole, amoxicillin and metronidazole A02BD02 Lansoprazole, tetracycline and metronidazole A02BD03 Lansoprazole, amoxicillin and metronidazole A02BD04 Pantoprazole in combination with amoxicillin and clarithromycin A02BD05 Omeprazole, amoxicillin and clarithromycin A02BD06 Esomepra zol, amoxicillin and clarithromycin A02BD07 Lansoprazole, amoxicillin and clarithromycin A02BD09 Lansoprazole, clarithromycin and tinidazole A02BD10 Lansoprazole, amoxicillin and levofloxacin
There are a number of new proton pump inhibitors in various stages of development and clinical trials.
The best known of these, and close to completion of trials, is tenatoprazole. However, some clinicians believe that it does not have obvious pharmacodynamic advantages over its predecessors and that the differences relate only to the pharmacokinetics of the active substance (Zakharova N.V.). Among the advantages of ilaprazole is that it is less dependent on the polymorphism of the CYP2C19 gene and that its half-life (T1/2) is 3.6 hours (Maev I.V. et al.) US Food and Drug Administration (FDA) in In January 2009, a sixth proton pump inhibitor, dexlansoprazole, which is an optical isomer of lansoprazole, was approved for use in the treatment of GERD; in May 2014, it received approval in Russia.
In the Pharmacological Index, in the section Gastrointestinal Drugs, there is a group “Proton pump inhibitors”.
By Order of the Government of the Russian Federation dated December 30, 2009 No. 2135-r, one of the proton pump inhibitors - omeprazole (capsules; lyophilisate for the preparation of a solution for intravenous administration; lyophilisate for the preparation of a solution for infusion; film-coated tablets) is included in the List of vital and essential medicines.
Currently, five standard doses of proton pump inhibitors (esomeprazole 40 mg, lansoprazole 30 mg, omeprazole 20 mg, rabeprazole 20 mg, pantoprazole 40 mg) and one double dose (omeprazole 40 mg) are licensed for the treatment of GERD. Standard-dose proton pump inhibitors are licensed for the treatment of erosive esophagitis for 4 to 8 weeks, and double-dose is licensed for the treatment of refractory patients who have previously been treated with standard doses for up to 8 weeks. Standard doses are prescribed once a day, a double dose is prescribed twice a day (V.D. Pasechnikov et al.).
Over-the-counter proton pump inhibitors
In the first decades after their appearance, antisecretory drugs in general and proton pump inhibitors in the USA, Russia, and many other countries were prescription drugs.
In 1995, the FDA approved the over-the-counter sale of the H2 blocker Zantac 75, and in 2003, the first over-the-counter PPI, Prilosec OTC (omeprazole magnesium). Later, over-the-counter PPIs were registered in the United States: Omeprazole (omeprazole), Prevacid 24HR (lansoprazole), Nexium 24HR (esomeprazole magnesium), Zegerid OTC (omeprazole + sodium bicarbonate). All over-the-counter forms have a reduced content of active substance and are intended “for the treatment of frequent heartburn.” Pantoprazole 20 mg was approved for over-the-counter release in the European Union (EU) on June 12, 2009, in Australia - in 2008. Esomeprazole 20 mg - in the EU on August 26, 2013. Lansoprazole - in Sweden since 2004, later approved in a number of other EU countries, Australia and New Zealand. Omeprazole - in Sweden since 1999, later in Australia and New Zealand, other EU countries, Canada, and a number of Latin American countries. Rabeprazole - in Australia since 2010, later - in the UK (Boardman HF, Heeley G. The role of the pharmacist in the selection and use of over-the-counter proton-pump inhibitors. Int J Clin Pharm (2015) 37: 709–716. DOI 10.1007/s11096-015-0150-z).
In Russia, in particular, the following dosage forms of PPIs are approved for over-the-counter sale:
- Gastrozol, Omez, Ortanol, Omeprazole-Teva, Ultop, capsules containing 10 mg of omeprazole
- Beret, Noflux, Pariet, Rabiet, capsules containing 10 mg rabeprazole sodium (or rabeprazole)
- Controloc, capsules containing 20 mg pantoprazole
The general rule when taking over-the-counter PPIs is: if there is no effect within the first three days, consultation with a specialist is necessary. The maximum period of treatment with an over-the-counter PPI without consulting a doctor is 14 days (for Controloc - 4 weeks). The interval between 14-day courses must be at least 4 months.
Proton pump inhibitors in the treatment of gastrointestinal diseases
Proton pump inhibitors are the most effective drugs that suppress the production of hydrochloric acid, although they are not without some disadvantages.
As such, they have found wide application in the treatment of acid-dependent diseases of the gastrointestinal tract, including when it is necessary to eradicate Helicobacter pylori. Diseases and conditions for the treatment of which the use of proton pump inhibitors is indicated (Lapina T.L.):
- gastroesophageal reflux disease (GERD)
- stomach and/or duodenal ulcer
- Zollinger-Ellison syndrome
- damage to the gastric mucosa caused by non-steroidal anti-inflammatory drugs (NSAIDs)
- diseases and conditions for which eradication of Helicobacter pylori is indicated.
Numerous studies have shown a direct relationship between the duration of maintaining gastric acidity with pH > 4.0 and the speed of healing of ulcers and erosions in the esophagus, gastric and duodenal ulcers, the frequency of Helicobacter pylori eradication, and a decrease in symptoms characteristic of extraesophageal manifestations of gastroesophageal reflux. The lower the acidity of the stomach contents (i.e., the higher the pH value), the sooner the effect of treatment is achieved. In general, it can be said that for most acid-related diseases, it is important that the pH level in the stomach be more than 4.0 for at least 16 hours a day. More detailed studies have established that each of the acid-related diseases has its own critical level of acidity, which must be maintained for at least 16 hours a day (Isakov V.A.):
| Acid-dependent diseases | Acidity level required for healing, pH, not less |
| Gastrointestinal bleeding | 6 |
| GERD complicated by extraesophageal manifestations | 6 |
| Quadruple or triple therapy with antibiotics | 5 |
| Erosive GERD | 4 |
| Damage to the gastric mucosa caused by taking non-steroidal anti-inflammatory drugs | 4 |
| Functional dyspepsia | 3 |
| Maintenance therapy for GERD | 3 |
| Proton pump inhibitor | Maximum permitted dose for a single dose, mg |
| Omeprazole | 40 |
| Pantoprazole | 40 |
| Lansoprazole | 30 |
| Rabeprazole | 20 |
| Esomeprazole | 40 |
In the pathogenesis of gastric and/or duodenal ulcers, the decisive link is the imbalance between aggressive factors and protective factors of the mucous membrane. Currently, among the factors of aggression, in addition to hypersecretion of hydrochloric acid, there are: hyperproduction of pepsin, Helicobacter piylori, impaired gastroduodenal motility, effects on the mucous membrane of the stomach and duodenum of bile acids and lysolycetin, pancreatic enzymes in the presence of duodenogastric reflux, as well as ischemia of the mucous membrane, smoking, drinking strong alcohol, taking certain medications such as non-steroidal anti-inflammatory drugs. Protective factors include: secretion of gastric mucus, production of bicarbonates, which help neutralize intragastric acidity at the surface of the gastric mucosa up to 7 units. , the latter’s ability to regenerate, the synthesis of prostaglandins, which have a protective effect and are involved in ensuring adequate blood flow in the mucous membrane of the stomach and duodenum. It is important that many of these factors of aggression and defense are genetically determined, and the balance between them is maintained by the coordinated interaction of the neuroendocrine system, including the cerebral cortex, hypothalamus, peripheral endocrine glands and gastrointestinal hormones and polypeptides. The most important role of hyperacidity in the genesis of peptic ulcer disease is confirmed by the high clinical effectiveness of antisecretory drugs that are widely used in modern therapy of peptic ulcer disease, among which proton pump inhibitors play a leading role (Maev I.V.).
Proton pump inhibitors in Helicobacter pylori eradication regimens
Eradication of Helicobacter pylori
does not always achieve its goal.
The very widespread and incorrect use of common antibacterial agents has led to an increase in Helicobacter pylori
.
It is recognized that in different countries of the world (different regions) it is advisable to use different schemes. In the vast majority of regimens, one of the proton pump inhibitors is necessarily present in the so-called standard dosage (omeprazole 20 mg, lansoprazole 30 mg, pantoprazole 40 mg, esomeprazole 20 mg, rabeprazole 20 mg 2 times a day). The presence of a proton pump inhibitor in the regimen significantly increases the effectiveness of antibiotics and dramatically increases the percentage of successful eradications. An exception when proton pump inhibitors are not used is atrophy of the gastric mucosa with achlorhydria, confirmed by pH measurements. The choice of a particular proton pump inhibitor affects the likelihood of eradication, but replacing other drugs (antibiotics, cytoprotectors) has a much greater impact than PPIs. Specific recommendations for the eradication of Helicobacter pylori
are given in the Standards for the diagnosis and treatment of acid-dependent and Helicobacter pylori-associated diseases adopted by the Scientific Society of Gastroenterologists of Russia in 2010.
Proton pump inhibitors increase the risk of fractures, possibly cause Clostridium difficile-associated diarrhea and may cause hypomagnesemia and dementia in old age, and are also likely to increase the risk of pneumonia in the elderly
The US Food and Drug Administration (FDA) has issued a number of warnings about possible dangers from long-term or high-dose use of proton pump inhibitors:
- In May 2010, the FDA issued a warning about the increased risk of hip, wrist, and spine fractures with long-term or high-dose use of proton pump inhibitors ("FDA Warning")
- In February 2012, the FDA issued a notice warning patients and physicians that proton pump inhibitor therapy may increase the risk of Clostridium difficile-associated diarrhea (FDA Notice dated 2/8/2012).
Because of this and similar information, the FDA believes: When prescribing proton pump inhibitors, the physician should select the lowest possible dose or shorter course of treatment that is appropriate for the patient's condition.
Several cases of life-threatening hypomagnesemia (lack of magnesium in the blood) associated with taking proton pump inhibitors have been described (Yang Y.-X., Metz DC). Proton pump inhibitors, when taken in combination with diuretics in elderly patients, slightly increase the risk of hospitalization for hypomagnesemia. However, this fact should not affect the justified prescription of proton pump inhibitors, and the small risk does not require screening for magnesium levels in the blood (Zipursky J el al. Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study / PLOS Medicine — Sep 30, 2014).
According to studies conducted in Germany (German Center for Neurodegenerative Diseases, Bonn), long-term use of proton pump inhibitors increases the risk of dementia in old age by 44% (Gomm W. et al. Association of Proton Pump Inhibitors With Risk of Dementia. A Pharmacoepidemiological Claims Data Analysis. JAMA Neurol. Published online February 15, 2021. doi:10.1001/jamaneurol.2015.4791).
Scientists from the UK found that older people who received PPIs over a two-year period had a higher risk of pneumonia. The logic of the study authors is as follows: acid in the stomach creates a barrier to intestinal microbiota that is pathogenic for the lungs. Therefore, if acid production decreases due to PPI use, then due to high reflux, more pathogens can enter the respiratory tract (J. Zirk-Sadowski, et al. Proton-Pump Inhibitors and Long-Term Risk of Community-Acquired Pneumonia in Older Adults. Journal of the American Geriatrics Society, 2018; DOI: 10.1111/jgs.15385).
Still from video: Simanenkov V.I. Acid suppressive therapy for refractory forms of GERD, showing how many and what kind of adverse events (AEs) occur when taking PPIs.
Taking proton pump inhibitors during pregnancy
Different proton pump inhibitors have different FDA risk categories for the fetus:
- pantoprazole, lansoprazole, dexlansoprazole - B (animal studies did not reveal risks of negative effects on the fetus; there were no adequate studies in pregnant women)
- omeprazole, rabeprazole, esomeprazole - C (animal studies have shown negative effects of the drug on the fetus, and there have been no adequate studies in pregnant women, but the potential benefits associated with the use of this drug in pregnant women may justify its use despite the risks)
Taking proton pump inhibitors to treat gastroesophageal reflux disease during the first trimester of pregnancy more than doubles the risk of having a baby with heart defects (GI & Hepatology News, August 2010).
There are also studies showing that taking proton pump inhibitors during pregnancy increases the risk of asthma in the unborn child by 1.34 times (taking H2 blockers - by 1.45 times). Source: Lai T., et al. Acid-Suppressive Drug Use During Pregnancy and the Risk of Childhood Asthma: A Meta-analysis. Pediatrics. Jan 2018.
Selection of proton pump inhibitors
The acid-suppressing effect of proton pump inhibitors is strictly individual for each patient.
A number of patients experience such phenomena as “resistance to proton pump inhibitors”, “night acid breakthrough”, etc. This is due to both genetic factors and the condition of the body. Therefore, when treating acid-related diseases, the prescription of proton pump inhibitors should be individualized and promptly adjusted taking into account the response to the treatment. It is advisable to determine the individual rhythm of taking drugs and doses of drugs for each patient under the control of intragastric pH-metry (Bredikhina N.A., Kovanova L.A.; Belmer S.V.). See also: Rapoport S.I. etc. Selection of individual drug therapy for various diseases.
Daily pH-gram of the stomach after taking PPIs
Comparison of proton pump inhibitors
| Comparison of daily antisecretory activity of H2 receptor blockers (ranitidine) and omeprazole (Maev I.V. et al.) |
It is generally accepted that proton pump inhibitors are the most effective drugs for the treatment of acid-related diseases.
The class of antisecretory drugs that appeared before PPIs—H2-blockers of histamine receptors—are gradually being forced out of clinical practice and PPIs now compete only with each other. Among gastroenterologists, there are different points of view on the comparative effectiveness of specific types of proton pump inhibitors. Some of them argue that, despite some differences that exist between PPIs, today there is no convincing data to suggest that any PPI is more effective than others (Vasiliev Yu.V. et al.) or that during eradication The type of PPI included in the triple (quadruple) therapy does not matter (Nikonov E.K., Alekseenko S.A.). Others write that, for example, esomeprazole is fundamentally different from the other four PPIs: omeprazole, pantoprazole, lansoprazole and rabeprazole (Lapina T.L., Demyanenko D., etc.). Still others believe that rabeprazole is the most effective (Ivashkin V.T. et al., Maev I.V. et al.). According to Bordin D.S., the effectiveness of all PPIs for long-term treatment of GERD is similar. In the early stages of therapy, lansoprazole has some advantages in the speed of onset of effect, which potentially increases patient adherence to treatment. If you need to take several drugs to simultaneously treat other diseases, pantoprazole is the safest. There are many generic PPIs on the Russian and other CIS markets. It is known that all original PPIs have a high antisecretory potential, adequate in almost all situations where it is necessary to suppress secretion. As for generic drugs, they often differ in antisecretory activity both from the original drugs and from each other. This is due not only to the characteristics of the pharmacokinetics of individual classes of PPIs, but also to the quality of generics, as evidenced by the high “primary resistance” observed in certain drugs to the first standard doses, which decreases when the single dose is doubled (Kurilovich S.A., Chernosheikina L.E. .). Due to possible differences in the quality of drugs, an objective assessment of their clinical effectiveness is important. Currently, 24-hour monitoring of intragastric pH levels is an objective and accessible method for testing antisecretory agents in clinical practice (Alekseenko S.A.).
A group of scientists from Germany (Kirchheiner J. et al.) performed a meta-analysis of the dose-response relationship for the average level of 24-hour intragastric pH and the percentage of time with pH>4 in 24 hours for various PPIs. They obtained the following values for the effectiveness of various PPIs to achieve an average value of intragastric pH = 4:
| Type of IPP | Dose of PPI (mg/day) to achieve an average pH value of 4 during 24-hour intragastric pH-metry | ||
| Healthy | Patient with GERD | Patient infected with Helicobacter pylori | |
| Pantoprazole | 89,2 | 166 | No data |
| Omeprazole | 20,2 | 37,7 | 3,0 |
| Rabeprazole | 11,1 | 20,1 | 1,6 |
| Lansoprazole | 22,6 | 41,8 | 3,3 |
| Esomeprazole | 12,6 | 23,6 | No data |
The cost of generics omeprazole, pantoprazole and lansoprazole is much lower than the original drugs esomeprazole and rabeprazole, which is of no small importance for the patient and often determines the choice of drug based on financial capabilities, especially for long-term use (Alekseenko S.A.).
Trade names of drugs - proton pump inhibitors
The domestic pharmaceutical market offers a wide range of different drugs from the group of proton pump inhibitors:
- active substance omeprazole: Bioprazole, Vero-omeprazole, Gastrozole, Demeprazole, Zhelkizol, Zerotsid, Zolser, Chrismel, Lomak, Losek, Losek MAPS, Omegast, Omez, Omezol, Omecaps, Omepar, Omeprazole, Omeprazole pellets, Omeprazole-AKOS, Omeprazole- acri, Omeprazole-E.K., Omeprazole-OBL, Omeprazole-Teva, Omeprazole-Richter, Omeprazole-FPO, Omeprazole Sandoz, Omeprazole Stada, Omeprol, Omeprus, Omefez, Omizak, Omipix, Omitox, Ortanol, Otsid, Pepticum, Pleom -20, Promez, Risek, Romesek, Sopral, Ulzol, Ultop, Helitsid, Helol, Cisagast
- the active substance is omeprazole, in addition to which the medicine contains a noticeable amount of sodium bicarbonate: Omez insta
- active substance omeprazole + domperidone: Omez-d
- active ingredient pantoprazole: Zypantol, Controloc, Crosacid, Nolpaza, Panum, Peptazol, Pigenum-Sanovel, Puloref, Sanpraz, Ultera
- active substance lansoprazole: Acrilanz, Helicol, Lanzabel, Lanzap, Lanzoptol, Lansoprazole, Lansoprazole pellets, Lansoprazole Stada, Lansofed, Lancid, Loenzar-Sanovel, Epicur
- active substance rabeprazole: Bereta, Zolispan, Zulbex, Noflux (formerly called Zolispan), Ontime, Noflux, Pariet, Rabeloc, Rabeprazole-OBL, Rabeprazole-SZ, Rabiet, Razo, Hairabezol
- active substance esomeprazole: Nexium, Neo-Zext, Emanera
- active substance dexlansoprazole: Dexilant
- active substance naproxen + esomeprazole: Vimovo (prescribed for the treatment of pain due to osteoarthritis, rheumatoid arthritis and ankylosing spondylitis in patients at risk of developing peptic ulcers).
In Russia, drugs are registered that are three-component sets of capsules and tablets corresponding to the daily dose for “triple therapy” for the eradication of Helicobacter pylori: Pilobact with the combined active ingredient “omeprazole + tinidazole + clarithromycin” and Pilobact AM with the combined active ingredient “omeprazole + amoxicillin + clarithromycin." In addition, in the pharmaceutical markets of the former USSR republics there are a number of proton pump inhibitors that are not registered in Russia, in particular:
- omeprazole: Gasec, Losid, Omeprazole-Astrapharm, Omeprazole-Darnitsa, Omeprazole-KMP, Omeprazole-Lugal, Tserol
- pantoprazole: Zogast, Zolipent, Panotsid, Pantasan, Panatap, Proxium, Protonex, Ulthera
- lansoprazole: Lanza, Lansedine, Lanpro, Lansohexal, Lansoprol, Lancerol
- rabeprazole: Barol-20, Geerdin (powder for the preparation of solution for injection and enteric-coated tablets), Rabezol, Rabemak, Rabimak, Rabeprazol-Zdorovye, Razol-20
Brands registered in Germany: Antra and Antra MUPS (omeprazole), Agopton (lansoprazole), etc.
Proton pump inhibitors in the USA
Brands registered in the USA:
- prescription: Prilosec (formerly Losec; omeprazole), Zegerid (omeprazole + sodium bicarbonate), Protonix and Protonix IV (pantoprazole), Prevacid (lansoprazole), AcipHex (rabeprazole), Nexium (esomeprazole), Dexilant (dexlansoprazole) and Vimovo (esomeprazole + naproxen)
- over-the-counter (OTC) prescription drug options: Prilosec OTC (omeprazole magnesium), Omeprazole (omeprazole), Nexium 24HR (esomeprazole magnesium), Zegerid OTC (omeprazole + sodium bicarbonate) and Prevacid 24HR (lansoprazole).
Proton pump inhibitors are the most popular prescription medications in the United States for the treatment of digestive diseases. In 2004, they occupied the top five positions in the table ranked by sales volume (see table below) and their total sales amounted to 77.3% of all drugs in this class:
| A drug | For all diseases | Incl. for the treatment of certain diseases | ||||
| GERD (all types) | Peptic ulcer of the stomach and duodenum | |||||
| Number of recipes, million pcs. | Total cost, million $ | Number of recipes, million pcs. | Total cost, million $ | Number of recipes, million pcs. | Total cost, million $ | |
| Lansoprazole | 21,0 | 3 105 | 14,2 | 2 187 | 1,3 | 177 |
| Esomeprazole | 19,5 | 2 846 | 14,3 | 2 181 | 0,7 | 86 |
| Pantoprazole | 11,7 | 1 408 | 10,0 | 1 224 | 1,1 | 124 |
| Rabeprazole | 8,0 | 1 136 | 6,0 | 914 | 0,2 | 27 |
| Omeprazole | 8,6 | 1 039 | 6,6 | 841 | 0,3 | 31 |
| Total | 68,8 | 9 534 | 51,1 | 7 347 | 3,6 | 445 |
Publications for Health Professionals
- Lapina T.L. Proton pump inhibitors: from pharmacological properties to clinical practice // Pharmateka. – 2002. – No. 9. – p. 3–8.
- Maev I.V., Vyuchnova E.S., Balashova N.N., Shchekina M.I. The use of omeprazole and esomeprazole in patients with bronchial asthma combined with GERD // Experimental and clinical gastroenterology. – 2003. – No. 3. – p. 26–31.
- Maev I.V. The place and significance of proton pump inhibitors in the modern treatment of peptic ulcer // Experimental and clinical gastroenterology. – 2003. – No. 3. – p. 12–13.
- Morozov S.V., Tsodikova O.M., Isakov V.A. and others. Comparative effectiveness of the antisecretory action of rabeprazole and esomeprazole in individuals who rapidly metabolize proton pump inhibitors // Experimental and clinical gastroenterology. – 2003. – No. 6.
- Lapina T.L. Proton pump inhibitors: how to optimize the treatment of acid-related diseases // Russian Medical Journal. – 2003. – T.11. – No. 5.
- Starostin B.D. Switching to another proton pump inhibitor if the previous one is ineffective in patients with gastroesophageal reflux disease. // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2006, no. 5, p. 13.
- Isakov V.A. Therapy of acid-related diseases with proton pump inhibitors in questions and answers // Consilium Medicum. – 2006.– No. 7. – from 3–7.
- Samsonov A.A. Proton pump inhibitors are the drugs of choice in the treatment of acid-related diseases // Pharmateka. – 2007. – No. 6. – p. 10–15.
- Kenneth R. McQuaid, Loren Laine. Relieving heartburn with proton pump inhibitors: a systematic review and meta-analysis of clinical trials. Clinical Gastroenterology and Hepatology. Russian edition. – 2008. – volume 1. – No. 3. – p. 184–192.
- Pasechnikov V.D. Keys to choosing the optimal proton pump inhibitor for the treatment of acid-dependent diseases // RZHGGK. - No. 3. – 2004.
- Bordin D.S. Safety of treatment as a criterion for choosing a proton pump inhibitor in a patient with gastroesophageal reflux disease // Consilium Medicum. – 2010. – Volume 12. – No. 8.
- Russian Society of Surgeons. Ulcerative gastroduodenal bleeding. National clinical guidelines.
- Mikheeva O.M. The use of proton pump inhibitors for the treatment of acid-related diseases // Therapy. – 2021. – No. 2(6). pp. 43-46.
- Kucheryavyi Yu.A., Andreev D.N., Shaburov R.I. Proton pump inhibitors in the practice of a general practitioner. Therapy. 2019; No. 5[31]:120–126.
- Hoshikawa Y., Nikaki K., Sonmez S., Yazaki E., Sifrim D., Woodland P. Exacerbation of gastroesophageal reflux symptoms after discontinuation of proton pump inhibitors is not associated with increased esophageal acid exposure. OP232. UEG Journal, 2021, Vol .7(8S) iv. Abstract issue, p.126. Translation into English: Worsening of gastroesophageal reflux symptoms after discontinuation of proton pump inhibitors is not associated with increased acid exposure to the esophagus.
On the website, in the “Literature” section, there is a subsection “Proton pump inhibitors”, which contains publications for healthcare professionals on the treatment of gastrointestinal diseases using PPIs.
Videos (reports and lectures) for healthcare professionals addressing issues of PPI therapy
| Bordin D.S. The most common mistakes in diagnosing and treating GERD | |
| Simanenkov V.I. Acid suppressive therapy for refractory forms of GERD | |
| Sablin O.A. Tactics and duration of therapy for GERD | |
| Embutnieks Yu. V. Principles of management of patients with refractory GERD | |
| Vovk E.I. Medicines for the treatment of heartburn and diseases associated with hyperacidity. Clinical pharmacology | |
| Uspensky Yu.P. GERD and other acid-dependent diseases of the digestive system. Principles of rational pharmacotherapy | |
| Sidorov A.V. PPI drugs in a patient with NERD: does it make a difference? Clinical Pharmacologist's Answer | |
| Abdulkhakov S.R. Modern approach to the treatment of acid-related diseases: which therapy to choose? | |
| Bordin D.S. Phenotypes of GERD. What should a practicing physician know? | |
| Kaibysheva V.O. Barrett's esophagus: PPI treatment and nutrition for patients with GERD | |
| Kucheryavyi Yu.A. Acid-dependent diseases of the esophagus: are there answers to all questions? | |
| Ilchishina T.A. GERD in everyday practice: patient misconceptions and doctor errors | |
| Kapralov N.V., Sholomitskaya I.A. Daily intragastric pH-metry at the second department of internal diseases of the Belarusian State Medical University | |
| Bakulin I.G. GERD: recommendations, clinical practice, treatment | |
| Zyryanov S.K. Off-label PPI prescription: causes and consequences | |
| Sugyan N.G. Use of proton pump inhibitors in children | |
| Bordin D.S. Errors in diagnosis and treatment of GERD | |
| Maev I.V. Key mistakes in the management of patients with GERD | |
| Alekseenko S.A. GERD complicated by pathology of ENT organs, diagnostic possibilities | |
| Berezhnaya I.V., Kamlygina M.V. Proton pump inhibitors. SIBO as a complication | |
| Tsukanov V.V. Rational choice of PPI for a comorbid patient with GERD | |
| Sablin O.A. Features of drug therapy for long-term treatment of erosive injuries of the esophagus | |
| Melnikov K.N. Drugs affecting the gastrointestinal tract. Lecture for 3rd year students of the Faculty of Medicine of the First St. Petersburg State Medical University. Academician I.P. Pavlova | |
| Kareva E.N. Could a patient's genetic makeup be the cause of refractory GERD? Pharmacogenetic management of PPI effectiveness | |
| Chirkova Y.A. New generations of acid-blocking agents: is new always better than old? |
Patient Materials
The GastroScan.ru website contains materials for patients on various aspects of gastroenterology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Proton pump inhibitors have contraindications, side effects and application features; consultation with a specialist is necessary. Back to section
The most popular medications
The most popular representatives of medications from the group of proton pump inhibitors used to treat gastroenterological diseases include:
- Omez;
- Omeprazole;
- Lansoprazole;
- Pantoprazole;
- Ilaprazole;
- Rabeprazole;
- Esomeprazole.
Additionally, the group of proton pump inhibitors includes the drug Tenatoprazole. All of the listed names of drugs from this group are actively prescribed by gastroenterologists not only for the treatment and prevention of acid-related gastrointestinal diseases, but also as part of complex therapy for Helicobacter pylori infection.
Legal aspects
Today it is clear that the interaction of H. pylori
with the human body is complex, to some extent individual and not fully understood.
The physician should know that H. pylori
reduces the risk of esophageal diseases (including malignant ones) [12–14], bronchial asthma and atopy, and possibly obesity and diabetes mellitus, and take this into account when prescribing treatment [15].
What should a practicing physician do in a situation of conflicting clinical recommendations? It is often claimed that eradication of H. pylori
is indicated for everyone who has it, based on various protocols, standards and clinical recommendations.
In order for the doctor not to find himself in a difficult legal situation, it is very important for him to know the basic provisions of Federal Law No. 323 “On the fundamentals of protecting the health of citizens in the Russian Federation.” On December 18, 2021, the President of the Russian Federation signed Law No. 489-FZ “On Amendments to Article 40 of the Federal Law “On Compulsory Health Insurance in the Russian Federation” and the Federal Law “On the Fundamentals of Protecting the Health of Citizens in the Russian Federation” on Clinical Recommendations.” The use of clinical recommendations in our country has become regulated not just by an order of the Ministry of Health of Russia, but by the amended Federal Law No. 323, Article 37 of which stipulates that clinical recommendations must be approved in the established manner before December 31, 2021. Previously approved clinical recommendations (treatment protocols) are applied until their revision in accordance with Federal Law No. 489 of December 25, 2021 only until December 31, 2021. From January 1, 2022, only those clinical recommendations that are posted on the official website of the Russian Ministry of Health will be in effect. Moreover, for each disease, condition (group of diseases, conditions) for adults and children, no more than one clinical recommendation can be approved and approved, respectively. For peptic ulcer disease, clinical guidelines have existed since 2021. They recognize peptic ulcer disease after surgical treatment as the only basis for eradication of H. pylori
(recommendation level A, level of evidence certainty 1) [16].
Mechanism of action
After entering the lumen of the stomach, proton pump inhibitors penetrate into the cavity of the small intestine, after which they dissolve, are absorbed into the systemic circulation and are transported through the bloodstream to the liver. Further, the active components of the drugs interact with the parietal (secretory) cells of the gastric mucosa.
During complex eradication of Helicobacter Pylori, before starting therapy, it is important to have pH measurements. For gastritis with zero acidity (achlorhydria), this group of drugs is not used, since complete atrophy of the gastric mucosa is observed, and the cells of the organ do not produce hydrochloric acid.
Side effects of PPIs
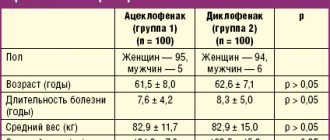
When conducting a survey among members of the Russian Gastroenterological Association, it was found that doctors most often prescribe the following PPIs: Omez®, Nexium®, Nolpaza®, Razo®, Pariet®. Preferences were divided by approximately 20%, but it should be noted that Razo® and Pariet® are rabeprazole. Why was rabeprazole preferred by doctors? Let's consider the possible side effects of these drugs, which are reflected in the instructions for medical use (IMP) (Table 1) [1, 4–7].
Side effects from the gastrointestinal tract (GIT), such as abdominal pain, diarrhea, flatulence, constipation, dry mouth, were noted in the UTI of all PPIs discussed (see Table 1). But there are also differences: for example, stomatitis and gastrointestinal candidiasis are listed among the side effects of the drugs Nexium® and Omez®, and microscopic colitis is a side effect of the drugs Nolpaza® and Nexium®.
The use of Razo and Pariet does not cause visual impairment, which is noted in the instructions for the drugs Nolpaza®, Nexium® and Omez® (see Table 1). It is precisely because of the resulting blurred vision, as well as because of dizziness when taking a number of PPIs, that patients should be careful when driving vehicles or engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Speaking about the rarer side effects of PPIs, mental disorders should be noted. Over more than 30 years of practice, I have twice encountered the occurrence of hallucinations while taking hydrochloric acid secretion inhibitors. A description of the development of mental disorders when taking PPIs (omeprazole, pantoprazole) is found in the literature [8, 9]. Their danger lies precisely in their rarity, given the overall safety of PPIs. No mental disorders have been described when taking rabeprazole (neither depression, nor insomnia, nor aggressive behavior, nor hallucinations are noted among the side effects in the instructions for use of these drugs). Also, rare side effects of PPIs include bronchospasm, which, according to UTI, occurs when taking the drugs Omez® and Nexium® and is not noted in the UTI of the drugs Nolpaza®, Razo® and Pariet® (see Table 1).
It is known that the use of the drug Nolpaza® (see Table 1) can cause subacute cutaneous lupus erythematosus (SCLE). The IMP notes that in the event of skin lesions, especially in areas exposed to sunlight, or in the presence of arthralgia, the patient should immediately seek medical attention. PCLE due to prior PPI therapy may increase the risk of developing PCLE during subsequent therapy with other PPIs. There is no mention of the occurrence of PCLE when using the drugs Omez®, Nexium®, Razo® and Pariet® in the instructions for these drugs. But the possibility of alopecia and photosensitivity has been recorded with the drugs Nexium® and Omez® [1].
For most PPIs, pregnancy and lactation are contraindications for use (see Table 1), however, the PPI drug Omez® states that the results of epidemiological studies indicate the absence of a clinically significant negative effect of omeprazole on pregnancy and the health of the fetus or newborn. Omeprazole passes into mother's milk, however, when using the drug in therapeutic doses, no negative effect on the child is expected.
Of the PPIs used for renal and hepatic failure and in elderly patients, rabeprazole demonstrated the greatest safety (Table 2). Thus, in the IMP of the drugs Razo® and Pariet®, it was noted that patients with chronic compensated liver cirrhosis tolerate rabeprazole well at a dose of even 20 mg 1 time / day, although the therapeutic dose of rabeprazole is 10 mg / day (the lowest therapeutic dose of all PPIs) .
The minimum of side effects when using rabeprazole is due to its pharmacokinetic properties. Rabeprazole is metabolized in two ways: a significant portion of the administered dose of rabeprazole is metabolized systemically non-enzymatically to form thioether derivatives, and a smaller portion of the dose is metabolized in the liver via cytochrome P450 (CYP) to form sulfonic and desmethyl derivatives [3]. For example, when taking esomeprazole, it is recommended to monitor the international normalized ratio (INR) at the beginning and at the end of concomitant use of esomeprazole and warfarin or other coumarin derivatives. Rabeprazole, according to the results of studies involving healthy volunteers, does not enter into pharmacokinetic and clinically significant interactions with drugs that are metabolized by the CYP system (warfarin, phenytoin, theophylline and diazepam) [1].
Preventing recurrent heartburn
There are some rules that can help reduce the symptoms of heartburn.
To prevent heartburn, you need to follow simple rules that will help reduce the load on the stomach and reduce unpleasant symptoms:
- Small portions of food 4-5 times a day.
- Reduce consumption of very spicy, salty, fatty foods.
- Avoid carbonated drinks and foods that cause gas (soda, beer, simple carbohydrates)
- Raise the pillow 15-20 cm while sleeping.
- Try not to eat before bed and not to lie down after eating.
- Give up bad habits (alcohol, smoking).
- Reduce excess weight.
- Do not lean forward too much and do not strain, avoid lifting weights of more than 8-10 kg (do not strain your abdominal muscles).
- Remove corsets and tight belts from your wardrobe, wear looser clothes that do not squeeze your stomach.
Conclusion
Self-medication can be practiced for mild, rare symptoms. For this purpose, drugs from the group of antacids and alginates are used, and a single dose of Ranitidine 75 mg is also possible. If heartburn bothers you more than once a week , you need to consult a doctor . Taking medications should not be uncontrolled. Self-administration should not last longer than 7-10 days. Otherwise, you may not notice other serious diseases in time, one of the symptoms of which may be heartburn.
What you need to know about PPIs
Medicines must be prescribed by doctors. When using the API, you need to know the following information:
- with long-term treatment, PPIs can change the pH of the stomach, so it is necessary to monitor changes and promptly stop therapy;
- There are often misconceptions that drugs increase the effectiveness of antibiotics; experts note that PPIs contribute to the development of the necessary environment for the rapid action of drugs;
- While taking PPIs, it is forbidden to use acidic foods; such foods can increase acidity and block the effect of the drug;
- It is not recommended to use several PPIs at the same time; such therapy can lead to an overdose or lack of the desired result.
Before using the drugs, you must carefully read the instructions. Particular attention should be paid to side effects and possible contraindications.
Clinical guidelines
We have already discussed above what recommendation all doctors will use when eradicating H. pylori
.
The following clinical recommendation is not accepted by all, but by most physicians: eradication therapy is recommended for all patients with peptic ulcer disease who test positive for H. pylori
to prevent subsequent relapses of peptic ulcer disease (level of recommendation B, level of evidence 2) [16] .
Recommendation for eradication therapy to prevent peptic ulcer disease and its exacerbations for all persons with H. pylori
in the absence of contraindications, a minority of knowledgeable doctors will probably use it (level of conviction of recommendations C, level of certainty of evidence 5) [16], i.e., for some patients, implementation of this recommendation, as already written above, can do more harm than good, especially since taking into account new data [12].
But for a number of patients with a family history, this recommendation may be appropriate, although the recommendations for stomach cancer approved by the Russian Ministry of Health in the section “Prevention of stomach cancer” do not contain instructions on eradication therapy for all patients infected with H. pylori
.
A final limitation of the study [14] is the lack of data on the relationship between H. pylori
and gastric cancer incidence and mortality. However, reducing the effect of smoking and a high-salt diet on the incidence of gastric cancer, especially among men and East Asians, may be an optimal option for primary prevention [12–14].