Most people associate hormone replacement therapy with the female menopause. However, it is used not only in gynecological practice, and not only among women of retirement age. The method of hormone replacement therapy is actively used in men. It is especially in demand among those who are interested in building muscle mass, are involved in professional sports, and want to maintain an athletic figure.
Hormone replacement therapy: what is it and why?
In developed countries, the prescription of HRT is a common practice after the appearance of noticeable age-related changes, as well as in people whose lives are closely connected with sports. In the post-Soviet space, such therapy is still viewed with caution. This is not surprising, given the thoughtless prescription of hormone replacement drugs in the 50-60s of the 20th century. Soviet doctors prescribed them to women suffering from gynecological diseases in “horse doses”, which led to unpleasant side effects, including the appearance of unwanted hair and obesity. With the correct selection and reasonable dosage of medications, such consequences can be avoided. But the positive effect will be noticeable immediately.
According to unofficial statistics, HRT is used by more than 50% of English women, about 25% of German women and at least 10% of French women over 45 years of age, while among Russian women this figure does not exceed 1-2%. The numbers are indicative: the medical sector in the post-Soviet space is developing more slowly and lags behind in many areas. The habit of Russians to tolerate inconveniences if they do not pose a threat to life also has an effect.
Menopausal hormone therapy: what should a general practitioner know?
More than a third of a modern woman’s life is spent in conditions of deficiency of sex hormones, the decline of which begins after 35 and significantly accelerates after 45 years. Therefore, the first signs of decline in reproductive function and associated clinical manifestations often debut many years before menopause.
Disorders associated with menopause make a woman vulnerable to the development and progression of a wide range of pathological conditions, including therapeutic diseases: various somatoform autonomic dysfunctions (SVD), muscle and joint pain, obesity (AO), cardiovascular diseases (CVD), including coronary heart disease (CHD) and arterial hypertension (AH), type 2 diabetes mellitus (DM), osteoporosis (OP) and a number of others [1, 2].
Family doctors, local therapists, as well as other first-contact doctors can play a significant role both in terms of early detection of menopausal disorders in their patients, and in terms of preventing the medical consequences of hormonal deficiency in the future. Therefore, knowledge of the clinical features of the menopause and the possibilities of their hormonal correction is of great importance for therapists. This knowledge is of particular relevance given the increase in women’s life expectancy, which causes the “accumulation” of diseases in the female population, in the development of which deficiency of sex hormones plays an important role.
In recent years, domestic and international practice has been enriched with agreed upon guidelines regulating the provision of medical care to women during menopause. Among them are clinical recommendations for menopausal hormone therapy (MHT), approved in 2015 by the Ministry of Health of the Russian Federation [1], 2021 recommendations for the health of women of mature age and MHT of the International Menopause Society (IMS) [2, 3 ] and a number of others [4, 5]. These documents contain provisions, the implementation of which requires the active participation of general practitioners. Moreover, their role seems significant at all stages of pre- and postmenopause, including when deciding, together with other specialists (gynecologists, oncologists), indications and contraindications for MHT, which has proven itself in the last decade as an effective means of improving the “quality” of a woman’s life in adulthood. age [2, 3].
Definitions
Menopause (menopause, menopause) is a physiological period of a woman’s life, during which, against the background of age-related changes in the body, involutionary processes in the reproductive system dominate.
Climacteric syndrome (CS) is a pathological condition that occurs in a significant proportion of women (up to 80%) during menopause and is characterized by neuropsychic, vegetative-vascular and metabolic-trophic disorders [6].
Menopause is understood as the last menstruation, the onset of which can be reliably judged a year after the complete cessation of menstrual cycles (MC). In European women, menopause occurs on average at the age of 51 years [2].
If menopause occurs before 40 years of age, it is considered premature, at 40–45 years of age – early, at 46–54 years of age – timely, over 55 years of age – late [1].
Within menopause, along with menopause, the periods of menopausal transition, perimenopause and postmenopause are traditionally distinguished.
Menopausal transition is characterized by variability of the MC, begins at 40–45 years of age and ends with the onset of menopause.
Perimenopause - includes the period of menopausal transition and 1 year after the last independent menstruation.
Postmenopause is the period of a woman’s life after menopause. Some authors limit this period to a certain time frame. For example, up to 65–69 years of age [6] or 10 years after the onset of menopause [7], etc. We are of the opinion that the entire period of a woman’s life after completion of MC should be considered the postmenopausal period, because over time the “load “The problems associated with a deficiency of sex hormones will only increase in them. At the same time, it seems appropriate to distinguish a time frame within each period of menopause: early phase, late phase.
Periods of menopause and stages of reproductive aging of women
In recent years, periods of menopause have begun to be correlated with the stages of aging of a woman’s reproductive system using the STRAW+10 (Stages of Reproductive Aging Workshop+10) scale, developed by a special working group of scientists [4] and approved by expert communities in many countries.
According to the STRAW+10 scale, a woman’s life is divided into 10 stages, designated from –5 to +2. Verification of each stage is based on taking into account the characteristics of the MC (main criteria), hormonal indicators (confirming criteria) and clinical symptoms (descriptive signs).
In table For ease of perception, in a simplified form, Figure 1 presents a generalized description of the periods of menopause and the stages of aging of a woman’s reproductive system in accordance with generally accepted criteria and the STRAW+10 scale.
The first clinical signs of a decrease in the level of sex hormones appear during the transition period, especially in its late phase, when a woman is likely to have neuropsychic and vegetative-vascular disorders. The most significant clinical consequences of hormonal deficiency “accumulate” and are fully realized in postmenopause. It is generally accepted that its early phase lasts 5 years, and the late phase lasts until the end of life [8].
“Therapeutic” manifestations and consequences of menopausal syndrome
Following a decrease in the content of sex hormones in a woman’s body, a train of neurovegetative and metabolic disorders is formed, which, based on the nature and time of occurrence, are conventionally divided into early (can debut in the transition period and last several years in postmenopause), medium-term (occur 1–3 years after menopause) and late (manifest 5 or more years after menopause) menopausal disorders [6].
Early manifestations of CS include neurovegetative (vasomotor), psychoemotional disorders, dyslipidemia (DLP), medium-term manifestations include urogenital disorders, deterioration of the skin and its appendages, late manifestations include CVD, postmenopausal AP and neurodegenerative changes in the central nervous system (up to Alzheimer's disease) [7, 9, 10].
At all stages of peri- and postmenopause, a woman is highly likely to experience symptoms of CS, which may be a reason for her to see a therapist.
At the initial stages, this, along with vasomotor disturbances (hot flashes), can be numerous conditions interpreted within the framework of SVD. Women may begin to complain of heart failure, instability of blood pressure (BP), breathing problems, intestinal problems, sweating, poor sleep, which, coupled with increased anxiety, causes her to frequently consult a therapist.
In the early phase of postmenopause, neurovegetative changes are accompanied by urogenital disorders, which can also be a reason to contact a therapist due to inflammatory changes in the urine. The latter can occur both due to degenerative changes in the mucous membrane of the vagina and bladder, and as a result of an ascending infection involving the renal collecting system (pyelitis, pyelonephritis).
As the length of time the female body has been in conditions of deficiency of sex hormones increases, late (metabolic) disorders begin to manifest, among which CVD and AP have the greatest medical and social significance. Without manifesting themselves clinically for many years, these diseases may subsequently contribute to increased morbidity and mortality among women [5].
Other hormonal disorders are also associated with a deficiency of sex hormones, which contribute to the general range of metabolic disorders of menopause. Thus, insulin resistance, hyperinsulinemia, decreased growth hormone, changes in the renin-aldosterone system and a number of other disorders in pre- and postmenopause make a woman vulnerable to the development of metabolic syndrome (MS) [11].
The principles of management of patients with MS are currently well developed [12]. The solution to many issues related to the diagnosis and treatment of MS is, of course, within the competence of therapists. The components of this syndrome (abdominal coolant, hypertension, DLP and hyperglycemia) and the conditions associated with it (non-alcoholic fatty liver disease, hyperuricemia, atherosclerosis, etc.) have always been and are in the area of “interest” of general practitioners.
Goals and principles of menopausal hormone therapy
The goal of MHT is to partially compensate for the deficiency of sex hormones, using such minimally optimal doses of hormonal drugs that can actually improve the general condition of patients and ensure the prevention of late metabolic disorders [13]. As a result of MHT, two main effects should be achieved: increasing life expectancy and improving its quality
Indications for prescribing MHT are [1]:
- vasomotor symptoms with mood changes, sleep disturbances;
- symptoms of urogenital atrophy, sexual dysfunction;
- prevention and treatment of AP;
- low quality of life associated with menopause, including arthralgia, muscle pain, memory loss;
- premature and early menopause;
- oophorectomy.
MHT should be strictly individualized and take into account the patient’s preferences, her personal risk factors (age, duration of postmenopause, risk of venous thromboembolism, stroke, ischemic heart disease, AP, etc.), the presence or absence of a uterus. It is important if a woman has pathology of the gastrointestinal tract (GIT), cholelithiasis (GSD), hypertriglyceridemia (HTG). In this case, the prescription of MHT to relieve symptoms or prevent AP and IHD should be part of an overall strategy, including recommendations regarding lifestyle, diet, physical activity, smoking cessation and alcohol abuse [3].
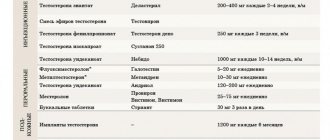
MHT was initially focused on reaping the benefits of replenishing a woman's estrogen deficiency. The use of estrogens in MHT, which are close to natural hormones, and the possibility of flexible use of various ways of administering them (Table 2) ensured their widespread use and the accumulation of convincing data on the beneficial effects of this component of MHT on a woman’s body during the pre- and postmenopausal periods. However, the use of estrogen monotherapy to achieve systemic effects is possible only when the uterus has been removed; in other cases, the mandatory inclusion of progestogens in MHT is required [1, 2].
In some cases, progestogens can be used as the only component of MHT (for example, during the menopausal transition or perimenopause to regulate the cycle and treat hyperplastic processes), but much more often - as a component of combined (in combination with estrogens) MHT. The combination of estrogens with progestogens makes it possible to protect the endometrium from hyperplastic processes with an intact uterus [1].
If previously some undesirable effects of MHT were associated with the progestogen component - an increase in the risk of thrombosis, an adverse effect on the plasma lipid profile [14], then now, thanks to the expansion of the line of progestogens, it has become possible to derive an additional therapeutic effect from the use of this component as part of MHT. For example, the presence of antimineralocorticoid action in drospirenone actualizes its use in MHT in women with hypertension and abdominal obesity [15]. Dydrogesterone does not reduce the protective effect of estrogens on the cardiovascular system, which creates an advantage for regimens that include this progestogen in MHT in women with diabetes and obesity [16].
Therapeutic aspect of the positive effects of MHT
The study of benefit/risk profiles when summarizing the results of numerous studies on the use of MHT has demonstrated the positive impact of this treatment on numerous aspects of the health of women of mature age [2], some of them are in the area of direct interest of doctors of therapeutic specialties, including local therapists and doctors general practice.
The following provisions on MHT have an evidence base today [3]:
- MHT is the most effective treatment for vasomotor disorders;
- quality of life, sexual function and other menopause-related complaints, such as joint and muscle pain, mood changes and sleep disturbances, may improve with MHT;
- MHT is effective in preventing menopausal AP and has shown a significant reduction in the risk of hip, spine, and other fractures in postmenopause;
- Estrogen-only MHT (at a standard dose) may reduce the risk of myocardial infarction and overall mortality;
- observational studies show that MHT administered to women with spontaneous or iatrogenic menopause before age 45 and especially before age 40 is associated with a reduced risk of CVD, increases life expectancy, and reduces the risk of dementia;
- MHT may be useful in improving mood in early postmenopausal women with depressive and/or anxiety disorders.
More and more information is emerging about the positive properties of MHT, such as the ability to prevent the development of type 2 diabetes in women, abdominal obesity, and inhibit age-related deterioration of cognitive abilities [1, 2].
When should MHT be prescribed and for how long?
Based on numerous data assessing the risk/benefit ratio of MHT in different (in terms of time of initiation and duration of treatment) groups of women, the concept of a “window of therapeutic opportunity” was formed [17]. It is recommended to start MHT between the ages of 45 and 60 years (with timely menopause) and no later than 10 years after menopause. During this period, MHT is not accompanied by the risk of cardiovascular and metabolic disorders [11].
In case of premature menopause (before 40 years), the feasibility of using combined oral contraceptives can be discussed [1].
For women with premature ovarian failure, MHT is recommended until the average age of menopause [17], i.e., until the age of 50–52 years.
According to Russian recommendations [1], the average duration of combined hormonal therapy is 5 years, estrogen monotherapy is 7 years. However, in recent years, the possibility of continuing systemic hormonal therapy in late postmenopausal women has been increasingly discussed [13, 17].
Contraindications to MHT
A significant proportion of Russian women have a rather restrained attitude towards MHT, which is largely due to an obsessive fear of hormones as such [14]. Meanwhile, the range of contraindications to MHT includes a fairly limited list of conditions [1], among them:
- breast and endometrial cancer;
- acute hepatitis, liver tumors;
- acute deep vein thrombosis;
- acute thromboembolism;
- allergy to MHT ingredients;
- cutaneous porphyria.
Relative contraindications include: uterine fibroids, endometriosis, migraine, history of venous thrombosis and embolism, familial hyperthyroidism, cholelithiasis, epilepsy, history of ovarian cancer.
In general, the proportion of women with CS for whom MHT is contraindicated is quite modest and amounts to about 16.8% [18].
When talking with women of mature age, as an argument in favor of MHT, data should be cited according to which timely prescribed MHT not only effectively relieves menopausal symptoms and improves the quality of life at the moment, but also reduces the risk of developing diseases of aging in the long term [19].
Therapeutic spectrum of examinations before MHT
According to modern requirements, before MHT, a woman should be consulted by a therapist and undergo appropriate examination [1, 11].
When collecting anamnesis, it is necessary to assess the risk of thrombosis (strokes or myocardial infarction suffered at a young age in oneself or close relatives, a history of thrombosis and thromboembolism, recurrent miscarriage, stillbirth, periods of immobility for more than a day in the last 2 weeks, as well as planning in the near future surgical operation). It is important to clarify the history of porphyria, AP (fractures), CVD, gastrointestinal pathology, diabetes, and to gain an understanding of the woman’s bad habits (smoking, alcoholism) and lifestyle (physical activity and nutrition).
It is imperative that the therapist evaluate the body mass index, blood pressure, and refer the woman for a general blood and urine test, a study of the lipid spectrum, and determination of glucose and thyroid-stimulating hormone in the blood.
If necessary (if there are appropriate suspicions), the therapist should prescribe an ultrasound examination of the liver, colonoscopy, densitometry of the lumbar spine and femoral neck, recommend blood tests for liver enzymes, hemostasiogram and D-dimer, determine the level of vitamin D and send blood samples to identify thrombophilic diseases. mutations [1].
Conclusion
Thus, MHT is an effective measure to preserve the health of mature women. The decision to conduct MHT should be made by a well-informed woman with the participation of a gynecologist and other specialists, among whom the therapist plays an important role.
Literature
- Menopausal hormone therapy and maintaining the health of mature women. Clinical guidelines (Treatment protocol). Letter of the Ministry of Health of the Russian Federation dated October 2, 2015 No. 15–4/10/2–5804.
- Baber R. J., Panay N., Fenton A. and the IMS Writing Group NS 2016 IMS Recommendations on women's midlife health and menopause hormone therapy // Climacteric. 2016; 19 (2): 109–150.
- De Villiers TJ, Hall JE, Pinkerton JV, Cerdas Perez S., Rees M., Yang C., Pierroz DD Revised Global Consensus Statement on Menopausal Hormone Therapy // Climacteric. 2016; 19: 313–315.
- Harlow SD, Gass M, Hall JE et al. Executive summary of the Stages of Reproductive Aging Workshop+10: addressing the unfinished agenda of staging reproductive aging // Climacteric. 2012; 15: 105–114.
- Chazova I. E., Smetnik V. P., Balan V. E. et al. Management of women with cardiovascular risk in peri- and postmenopause: consensus of Russian cardiologists and gynecologists // Practical Medicine. 2009; 2:5–18.
- Gynecology. National leadership / Ed. V. I. Kulakova, G. M. Savelyeva, I. B. Manukhina. M.: GEOTAR-Media. 2011: 1088 (National Guidelines Series).
- Endocrinology. National leadership. Brief edition / Ed. I. I. Dedova, G. A. Melnichenko. M.: GEOTAR-Media. 2013: 752 p.
- Reese M. et al.: Menopause / Trans. from English edited by V. P. Smetnik. M.: GEOTAR-Media. 2011. 240 p.
- Serov V.N., Prilepskaya V.N., Ovsyannikova T.V. Gynecological endocrinology. M.: MEDpress-inform, 2006. 528 p.
- Tumilovich L. G., Gevorkyan M. A. Handbook of gynecologist-endocrinologist. M.: Practical Medicine, 2009. 202 p.
- Mychka V. B., Tolstov S. N., Prokhorova Yu. V., Salov I. A., Vertkin A. A. A woman at an outpatient appointment: what should a therapist know? // Doctor.Ru. 2014; 55 (9): 67–75.
- Recommendations for the management of patients with metabolic syndrome: clinical guidelines. M.: RMOAG, 2013. 43 p.
- Ovsyannikova T.V., Kulikov T.V. Individual choice of menopausal hormonal therapy // Gynecology 2016; 4:59–62.
- Ilovayskaya I. A., Voitashevsky K. V. Rejuvenating apples of the XXI century. Menopausal hormone therapy: possibility and risks // Status Praesens. 2015; 5:80–86.
- Baranova E. I., Bolshakova O. O., Zazerskaya I. E., Yusipova T. Kh. Effect of replacement therapy with drospirenone on the structural and functional parameters of the cardiovascular system in postmenopausal women with hypertension and abdominal obesity // Arterialnaya hypertension. 2015; 4: 372–377.
- Grigoryan O. R. Menopausal syndrome in women with diabetes mellitus // Diabetes mellitus. 2013; 3: 103–108.
- De Villiers TJ, Pines A, Panay N et al. Updated 2013 International Menopause Society recommendations on menopausal hormone therapy and preventive strategies for midlife health // J. Climacteric. 2013; 16: 316–337.
- Pestrikova T. Yu., Yurasova E. A., Yachinskaya T. V., Kovaleva T. D. Menopausal hormonal therapy or non-hormonal treatment: a rational choice // Gynecology. 2015; 3:94–39.
- Yureneva S.V., Ilyina L.M., Yakushevskaya O.V. Menopausal hormonal therapy in postmenopause: quality of life today and in the long term // Gynecology. 2016; 1:24–29.
I. V. Madyanov*, 1, Doctor of Medical Sciences, Professor T. S. Madyanova**
* GAU DPO Institute for Advanced Training of Physicians of the Ministry of Health of the Chechen Republic, Cheboksary ** Medical LLC, Cheboksary
1 Contact information
When to start hormone replacement therapy?
There are no clear recommendations. The period for prescribing special drugs depends on the severity of age-related manifestations. The imbalance of sex hormones increases gradually and becomes more noticeable after 40 years (in both women and men). Deteriorating health is often explained by the aging of the body and a bunch of medications are prescribed that do not solve the problem, while it is enough to do a special analysis to understand the cause of the changes.
In women, the following signs indicate a lack of estrogen and testosterone, and therefore the need for hormone replacement therapy:
- menstrual irregularities;
- the appearance of papillomas, dry skin and mucous membranes;
- decreased sexual desire;
- decreased self-confidence;
- development of atherosclerosis, increased blood pressure, increased cholesterol and blood sugar levels;
- inability to lose weight even on strict diets;
- laxity of the inner sides of the shoulders.
Similar symptoms are observed in men. Often these are accompanied by depressive conditions, the appearance of fat folds in the waist area, swelling of the mammary glands, cardiovascular diseases, and prostate pathologies. Hypertension, osteoporosis, diabetes, heart attack, obesity are mostly consequences of a lack of specific hormones.
The most unpleasant thing for representatives of the stronger sex is the inability to maintain their previous physical shape. In addition to deterioration in appearance, there is a drop in vitality and fatigue even with minor exertion. This is extremely painful for people accustomed to an active lifestyle and regular exercise. Therefore, it is important to follow the recommendations of experts who advise taking hormone tests twice - after turning 35-45 years old, as well as when any signs of imbalance appear. The results of the study will help make a decision about the need to start HRT or postpone it to a later period.
Pros and cons of hormone replacement therapy
Of course, HRT is not a panacea for all diseases and not a harmless “indulgence in vitamins.” In addition to the pronounced benefits, it has side effects that should not be forgotten. But if you approach the prescription of hormone replacement drugs thoughtfully, the negative consequences will be minimal, and the quality of life as a result of such therapy will improve several times. People who scare themselves and those around them with “horror stories” about hair growth, kilograms of excess weight, and cancerous lesions caused by HRT actually know nothing about it.
In order to have a good idea of what awaits a patient who has been prescribed hormonal medications or a bodybuilder who wants to improve performance in sports, it is important to clearly distinguish between the pros and cons of replacement therapy. This approach, combined with the recommendations of a competent specialist, will give the most complete picture and help you make a decision.
The benefits of hormone replacement therapy
Many endocrinologists, in particular Leonid Vroslov, candidate of medical sciences, believe that timely administration of HRT can prevent many diseases. A course of replacement medications, started at the first signs of hormonal imbalance, will prevent ischemic heart disease, diabetes mellitus, hypertension, atherosclerosis, muscle atrophy, and other pathologies associated with aging. The effectiveness of HRT in the prevention of osteoporosis has also been proven, as confirmed by Professor Marina Tarasova. Special therapy may not prolong life, but it will significantly improve its quality.
In women, taking hormonal medications is aimed at eliminating estrogen deficiency. Replacement therapy will provide relief from the painful manifestations of menopause:
- irritability, fatigue, insomnia;
- regular headaches, joint, lumbar pain;
- hot and cold flashes;
- mood instability;
- digestive disorders, urination;
- problems with memory, attention;
- increased heart rate, decreased libido, etc.
In men, drug correction of hormonal levels can be considered as an effective alternative to antidepressants. Increasing testosterone levels with the help of replacement therapy will restore their stamina, strength, sexuality, improve their appearance, allow them to achieve serious results in sports, and prevent the formation of abdominal fat deposits.
Medical research confirms that the level of “male hormone” is responsible for:
- quality of metabolism, the body's sensitivity to oxygen;
- blood sugar balance, cholesterol removal;
- support of cardio- and neurological functions;
- immune system function, muscle mass;
- stable mood, libido.
Testosterone controls a number of vital processes and affects a man’s well-being. Therefore, it is so important to prevent a significant drop in its level, which is why hormone replacement therapy is prescribed. For many patients with cardiac disorders, it helps them stop taking expensive medications to stimulate cardiac activity.
What is HRT aimed at?
In older women, hypoestrogenism causes memory loss, which affects work. And HRT helps solve the problem of deteriorating mental abilities. Due to a lack of bone mass, older people are susceptible to fractures. In women, this risk increases sharply after menopause. Trying to take tons of calcium is useless: it is not absorbed against the background of a hypoestrogenic state. If a woman has a predisposition to osteoporosis, then HRT is vital for her. Classic osteoporosis type: blonde secretary with a cup of coffee in front of the computer. This is exactly the image that is drawn for students at the department for ease of memorization. In other words, this is a woman with low body weight, she has a sedentary job, she drinks a lot of coffee and smokes.
The second type - the northern peoples (Evenks, Chukchi) - have genetically thin bones that break easily in old age. And there are also families where fractures occur in several generations among elderly and senile people. If these risk groups begin to take estrogens, their bone mass will be restored, which means that the possibility of fractures will be delayed for a considerable time. In addition to osteoporosis, older women face no less dangerous traps: coronary heart disease, myocardial infarction, hypertension.
After menopause, atherosclerosis progresses sharply. The only thing that can protect a woman in this situation is estrogens, which will slow down the development of these diseases. It has been clearly proven that with a high concentration of estrogen in the blood, the risks of Alzheimer's disease and intestinal cancer are significantly reduced. HRT solves the problems of urinary incontinence, vaginal dryness, which makes sexual life difficult, even making it impossible. But most of all, a woman suffers from autonomic dysfunction, from hot flashes, when the face turns crimson-red in a second, from irritability, and night sweats. These menopausal symptoms make being in society uncomfortable, even unbearable. There are women who suffer from severe menopause for 6–10 years. And all their suffering is relieved by HRT.
Sports and hormones
For professional athletes, the use of HRT is not aimed at correcting well-being, but at improving physical fitness. In sports, preference is given to a combination of hormone replacement therapy with anabolic drugs, which can be combined in different ways to achieve better results. However, regardless of the purpose of their use, it is important to monitor your health status. With reasonable consumption, testosterone will only bring benefits: it will increase the volume of muscle tissue, reduce body fat, provide a surge of strength, rejuvenate the body, and increase achievements in sports.
However, you should not thoughtlessly increase the dosage of the drug, so that in the future you do not have to reduce its level with other medications. During administration, you need to constantly monitor the lipid profile, general clinical blood parameters, and the content of estradiol and prolactin in it. Before prescribing the course, you should undergo an examination and take tests.
Is hormone replacement therapy harmful?
Like any drug treatment, HRT has side effects. But they are not as terrible as hormonephobes try to imagine. For men, the main fear that keeps them from adjusting their testosterone levels is the fear of developing prostate cancer. However, most studies refute the connection between this disease and HRT.
As for women, the risk of malignant tumors of the breast and pelvic organs does exist. But it increases only with long-term use of hormone replacement drugs - with continuous therapy for over 15 years. The risk of any complications increases in heavy smokers and overweight patients.
The disadvantage of hormonal treatment is a significant deterioration in the quality of life after their withdrawal. The body, accustomed to the supply of active substances from the outside, is rarely able to return to their natural production.
Contraindications for hormone replacement therapy
Before prescribing medications, the doctor will definitely refer the patient for examination. It is necessary to undergo an ultrasound of the reproductive organs (for women also a mammogram), check the blood for clotting, determine the glucose level, find out the cause of excess weight (if any), and take tests for basic hormones. It is not necessary to examine the liver (if there are no problems on its part), but it is advisable. After treatment is prescribed, it is necessary to check your health once a year.
Testosterone hormone replacement therapy is not used for benign and malignant prostate tumors, breast cancer, neoplasms in the pituitary gland, and some blood diseases. Lung pathologies and heavy smoking are considered relative contraindications to the course.
In women, hormone replacement therapy is not used for malignant tumors in the reproductive organs or mammary gland, or vaginal bleeding of unknown etiology.
General contraindications are:
- thromboembolic complications;
- liver pathologies;
- severe forms of diabetes mellitus;
- disorders of fat metabolism.
Risks of using HRT
There are contraindications to HRT, and complications with their use exist. Estrogens increase the risk of endometrial cancer if taken without progestins. To prevent this, a second component, gestagen, is added to hormone replacement therapy drugs. The patient is prescribed drugs with pure estrogens only if the uterus is removed.
Very severe obesity, in which there is increased blood clotting, operated breast cancer, renal failure - all these are good reasons for refusing HRT. But chronic pyelonephritis does not interfere with HRT. As for hypertension, in some forms HRT can form the basis for a woman’s treatment, but in others it cannot be used. Therefore, the doctor must conduct a comprehensive examination and only after that decide on HRT.
How do estrogens affect blood vessels?
All arterial vessels are lined from the inside with a thin layer of endothelial cells. Their task is to expand or narrow the vessel in a timely manner, as well as protect it from cholesterol and blood clots. The endothelium depends on estrogens: if it is suddenly damaged, estrogens help it recover. When there are few of them, endothelial cells do not have time to recover. The vessels “age”: they lose elasticity, become overgrown with cholesterol plaques, and narrow. And since the vessels cover all organs, it turns out that estrogens affect the functioning of the heart, kidneys, liver, lungs... Estrogen receptors are found in all cells of a woman’s body.
Principles of hormone replacement therapy
HRT is a whole complex of measures, the purpose of which is to restore unbalanced body functions. Therefore, hormone replacement therapy is combined with lifestyle correction, normalization of weight, and psycho-emotional state. It is very important to establish proper nutrition, as it directly affects the production of active substances. It is recommended to include more vegetables and fruits, lean meat, fish, vegetable oil, nuts, and seeds in the menu. You need to move a lot, exercise regularly, and stick to a daily routine.
Hormone dosages will vary at different ages. For example, women before menopause are prescribed drugs with a higher content of active substances, gradually reducing their level as they age.
After 65 years of age, hormonal treatment is usually not prescribed because it will no longer be effective. However, if the correction is started on time, it can be continued for as long as desired. If there are no contraindications. The main principle of replacement therapy speaks for itself: “the last pill is on the last day of life.”
When is HRT prescribed?
For different ages, the dosages of hormones vary: there are drugs for women under 45 years old, from 45 to 50, from 51 and older. During perimenopause (before menopause), high doses are prescribed, then they are gradually reduced. Unfortunately, you may be late to jump into the last carriage of the departing train. If, for example, atherosclerosis has already developed, then it has managed to close the estrogen receptors, and no dose of the hormone will make them act. That is why it is so important to start taking sex hormones as early as possible, even if the menopausal syndrome is not yet pressing: you do not suffer from hot flashes, bouts of sweating, insomnia, irritability, hypertension.
There is a term “therapeutic window”. After 65 years, hormone therapy, as a rule, is not prescribed: sex hormones will no longer be able to properly engage in the functioning of the human mechanism. But if HRT is started on time, then it can be continued as long as the heart beats. If there are no contraindications. You need to understand that HRT is not an elixir of immortality; it will not give you extra years of life, but it will greatly improve your quality of life.
Will herbs help with menopause?
Recently, phytohormones have been actively promoted as the best and safest remedy against menopausal syndrome. And many gynecologists advise drinking dietary supplements with phytoestrogens during perimenopause. Plant hormone-like substances really work and help cope with hot flashes, insomnia, and irritability. But few people know that against their background, endometrial hyperplasia (proliferation of the inner layer of the uterus) is more common. This property of estrogen and estrogen-like substances in standard HRT is compensated by gestagen - it does not allow the endometrium to grow. Exclusively estrogen (without gestagen) is prescribed to women if the uterus has been removed. True, recent studies show a beneficial effect of gestagen on both the central nervous system and the mammary glands - it prevents the development of tumors. Unfortunately, unlike real estrogens, phytoanalogues have no effect on metabolism, calcium absorption, or the condition of blood vessels. Plant hormones are a compromise and salvation for those for whom real HRT is contraindicated. But doctor's supervision and regular examinations are also necessary.
Hormones and beauty
Any hormonal changes affect the condition of the skin. Cosmetic procedures themselves are effective only up to 40 years of age. After this, injections of hyaluronic acid, botulinum toxin, peelings are only half the battle; first of all, you need to normalize the hormonal status. When a circumferential lift is performed, excess tissue is cut off, but the quality of the skin remains the same. If there is no estrogen, the skin will be dry, dehydrated, without the proper amount of collagen and elastin. Wrinkles will appear again and again. If you replace the level of estrogen with the help of HRT, the emerging wrinkles will not disappear, but will stop getting deeper. And the weight will not increase.