Pembrolizumab (Keytruda, Keytruda, MK-3475) is an innovative drug that was approved by the FDA (American Food and Drug Administration) in September 2014, and is currently widely used for the treatment of late-stage melanoma.
In 2014, Keytruda received Priority Review and Breakthrough Medical Designation. This means that Pembrolizumab has been included in a group of medicines that can improve the effectiveness and safety of the treatment of rare and serious diseases. This is why the drug was approved and introduced into clinical practice so quickly - it usually takes much longer.
How does Pembrolizumab work?
Drugs for immunotherapy of melanoma and other malignant tumors have been around for quite some time. But they have always had low efficiency, and until recently scientists did not know how to deal with this problem.
The goal of immunotherapy is to activate the patient’s immune system, causing it to attack and destroy cancer cells. For a long time, the PD-1 protein became an obstacle to achieving this goal.
The PD-1 protein blocks the immune system. It prevents T lymphocytes from recognizing and destroying cancer cells. Keytruda contains monoclonal antibodies that block PD-1. The drug helps remove the “brake”, due to which lymphocytes acquire the ability to attack tumor tissue.
Relevance
On August 31, the US Food and Drug Administration (FDA), based on the results of two recently completed studies, issued warnings about the risks associated with the use of pembrolizumab (Keytruda) in combination with dexamethasone and immunomodulators (lenalidomide or pomalidomide) in patients with multiple myeloma.
This conclusion was a direct result of a review of data from two clinical trials—KEYNOTE-183 and KEYNOTE-185—that examined the efficacy and safety of pembrolizumab in patients with multiple myeloma. On July 3, 2021, the FDA requested discontinuation of treatment in all patients receiving combination therapy (pembrolizumab + immunomodulator) due to increased mortality compared with those in the control group.
However, pembrolizumab can be used in patients with diseases such as melanoma, lung cancer, head and neck cancer, classical Hodgkin lymphoma, uroepithelial carcinoma, and tumors with microsatellite instability.
It is noteworthy that several more clinical trials are currently being conducted to study pembrolizumab in combination with other PD-1/PD-L1 inhibitors and other drugs. The FDA plans to work directly with the companies that manufacture these drugs to determine the safety profile of the therapy.
How effective is Pembrolizumab?
A study was conducted at the University of California, Los Angeles, which involved 173 people diagnosed with advanced melanoma. They were divided into two groups. In one of them, patients received a standard dose of the drug 2 mg per kilogram of body weight every 3 weeks. In the second group, the dose was increased 5 times (10 mg/kg).
In 24% of patients receiving the drug at a dose of 2 mg/kg, the tumor decreased by more than a third. Re-growth of melanoma was not observed, and the effect of the drug lasted from 1.4 to 8.5 months (in some cases longer).
Keytruda®
Security Profile at a Glance
The use of Keytruda® is most often associated with the development of immune-mediated adverse reactions. Most of these, including severe reactions, resolved after initiation of appropriate therapy or discontinuation of Keytruda® (see "Description of Certain Adverse Reactions" below).
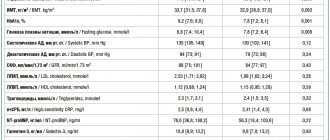
The safety of pembrolizumab when used as monotherapy was studied in clinical trials in 5884 patients with advanced melanoma, stage 3 melanoma after surgery (adjuvant therapy), NSCLC, cHL, urothelial cancer or head and neck cancer in four dosing regimens (2 mg/day). kg every 3 weeks, 200 mg every 3 weeks, or 10 mg/kg every 2 or 3 weeks). Based on all reported adverse drug reactions, the frequency below and in Table 2 are given regardless of the investigator's assessment of the cause-and-effect relationship. In this patient population, the median follow-up time was 7.3 months (range, 1 day to 31 months), and the most common adverse reactions with pembrolizumab were fatigue (32%), nausea (20%), and diarrhea (20%). Most reported adverse reactions when used as monotherapy were grade 1 or 2 in severity. The most serious adverse reactions were immune-mediated adverse reactions and severe infusion reactions (see Precautions).
The safety of pembrolizumab when used in combination with chemotherapy was studied in clinical trials in 1067 patients with NSCLC or HNSCC at dosing regimens of 200 mg, 2 mg/kg, or 10 mg/kg every three weeks. Based on all reported adverse drug reactions, the frequency below and in Table 2 are given regardless of the investigator's assessment of the cause-and-effect relationship. In this patient population, the most common adverse reactions were anemia (50%), nausea (50%), fatigue (37%), constipation (35%), diarrhea (30%), neutropenia (30%), decreased appetite (28%). ) and vomiting (25%). The incidence of grade 3-5 adverse reactions in patients with NSCLC was 67% when using pembrolizumab in combination with chemotherapy and 66% when using chemotherapy alone; in patients with HNSCC it was 85% when using pembrolizumab in combination with chemotherapy and 84% when using chemotherapy in combination with cetuximab.
The safety of pembrolizumab when used in combination with axitinib was studied in a clinical trial in 429 patients with advanced RCC using a dosing regimen of 200 mg pembrolizumab every three weeks and 5 mg axitinib twice daily. In this patient population, the most common adverse reactions were diarrhea (54%), increased blood pressure (45%), fatigue (38%), hypothyroidism (35%), decreased appetite (30%), and palmoplantar erythrodysesthesia syndrome (28%). ), nausea (28%), increased ALT (27%), increased AST (26%), dysphonia (25%), cough (21%) and constipation (21%). The incidence of grade 3-5 adverse reactions was 76% when using pembrolizumab in combination with axitinib and 71% when using sunitinib monotherapy.
The safety of pembrolizumab when used in combination with lenvatinib was studied in 94 patients with endometrial cancer at a dosing regimen of pembrolizumab 200 mg every three weeks and lenvatinib 20 mg orally once daily until evidence of unacceptable toxicity or disease progression as determined by the investigator. In this patient population, the most common adverse events were increased blood pressure (64%), diarrhea (63%), fatigue (54%), decreased appetite (51%), hypothyroidism (49%), nausea (48%), vomiting ( 39%), stomatitis (36%), weight loss (36%), arthralgia (33%), headache (33%), constipation (32%), dysphonia (29%), urinary tract infection (29%), abdominal pain (27%), hypomagnesemia (27%), palmoplantar erythrodysesthesia syndrome (26%), dyspnea (25%), cough (21%), myalgia (21%) and back pain (20%). Among the most frequently reported adverse events, which occurred in more than 2% of patients, the following grade 3-4 adverse events were noted: increased blood pressure, fatigue, abdominal pain, nausea, diarrhea, urinary tract infection, weight loss, hypomagnesemia, palmoplantar erythrodysesgesia syndrome and dyspnea.
Tabular list of adverse reactions
Adverse reactions observed in clinical studies of pembrolizumab when used as monotherapy, or in combination with chemotherapy, or with other antineoplastic agents, or reported during post-marketing use of Keytruda®, are listed in Table 2. Adverse reactions occurring with pembrolizumab alone or with pembrolizumab alone. chemotherapy may occur when they are used together, even if these reactions were not reported in clinical trials of combination therapy.
These reactions are presented by system-organ classes and frequency. Frequencies are listed in the following categories: very common (≥ 1/10); frequent (≥ 1/100 to < 1/10); uncommon (≥ 1/1000 to < 1/100); rare (≥ 1/10000 to < 1/1000); very rare (< 1/10000) and unknown (frequency cannot be estimated from available data). Within each frequency group, adverse reactions are arranged in descending order of severity.
Table 2: Adverse reactions in patients treated with Keytruda®*
| Monotherapy | In combination with chemotherapy | In combination with axitinib | |
| Infectious and parasitic diseases | |||
| Frequent | pneumonia | pneumonia | pneumonia |
| Blood and lymphatic system disorders | |||
| Very frequent | anemia | anemia, neutropenia, thrombocytopenia | |
| Frequent | thrombocytopenia, lymphopenia | febrile neutropenia, leukopenia, lymphopenia | anemia, neutropenia, leukopenia, thrombocytopenia |
| Infrequent | neutropenia, leukopenia, eosinophilia | lymphopenia, eosinophilia | |
| Rare | immune thrombocytopenic purpura, hemolytic anemia, true erythrocyte aplasia, hemophagocytic lymphohistiocytosis | eosinophilia | |
| Immune system disorders | |||
| Frequent | infusion reactiona | infusion reactiona | infusion reactiona |
| Infrequent | sarcoidosis | ||
| Unknown | solid organ transplant rejection | ||
| Endocrine system disorders | |||
| Very frequent | hypothyroidismb | hyperthyroidism, hypothyroidismb | |
| Frequent | hyperthyroidism | hypothyroidism, hyperthyroidism | hypophysitisd, thyroiditis, adrenal insufficiencyc |
| Infrequent | adrenal insufficiencyc, hypophysitisd, thyroiditis | hypophysitisd, thyroiditis, adrenal insufficiencyc | |
| Metabolic and nutritional disorders | |||
| Very frequent | loss of appetite | hypokalemia, loss of appetite | loss of appetite |
| Frequent | hyponatremia, hypokalemia, hypocalcemia | hyponatremia, hypocalcemia | hypokalemia, hyponatremia, hypokatcyemia |
| Infrequent | diabetes mellitus type 1f | type 1 diabetes mellitus | diabetes mellitus type 1f |
| Mental disorders | |||
| Frequent | insomnia | insomnia | insomnia |
| Nervous system disorders | |||
| Very frequent | headache | dizziness, headache, peripheral neuropathy, dysgeusia | headache, dysgeusia |
| Frequent | dizziness, peripheral neuropathy, lethargy, dysgeusia | lethargy | dizziness, lethargy, peripheral neuropathy |
| Infrequent | epilepsy | epilepsy | myasthenic syndrome |
| Rare | encephalitis, Guillain-Barreg syndrome, myelitis, myasthenic syndrome, meningitis (aseptic)j | ||
| Violations of the organ of vision | |||
| Frequent | dry eyes | dry eyes | dry eyes |
| Infrequent | uveitisk | uveitisk | |
| Rare | Vogt-Koyanagi-Harada syndrome | ||
| Heart disorders | |||
| Frequent | abnormal heart rhythm†(including atrial fibrillation) | abnormal heart rhythm†(including atrial fibrillation) | abnormal heart rhythm† (including atrial fibrillation) |
| Infrequent | pericardial effusion, pericarditis | pericardial effusion | myocarditis |
| Rare | myocarditis | myocarditis, pericarditis | |
| Vascular disorders | |||
| Very frequent | increased blood pressure | ||
| Frequent | increased blood pressure | increased blood pressure | |
| Respiratory, thoracic and mediastinal disorders | |||
| Very frequent | shortness of breath, cough | shortness of breath, cough | shortness of breath, cough, dysphonia |
| Frequent | pneumonitis | pneumonitis | pneumonitis |
| Gastrointestinal and cervical tract disorders | |||
| Very frequent | diarrhea, abdominal pain, nausea, vomiting, constipation | diarrhea, nausea, vomiting, constipation, abdominal pain | diarrhea, abdominal pain, nausea, vomiting, constipation |
| Frequent | colitis, dry mouth | colitis, dry mouth | colitis, dry mouth |
| Infrequent | pancreatitis, ulceration of the wall of the gastrointestinal tractq | pancreatitis, ulceration of the wall of the gastrointestinal tractq | pancreatitis, ulceration of the wall of the gastrointestinal tractq |
| Rare | small intestinal perforation | ||
| Disorders of the liver and biliary tract | |||
| Frequent | hepatitis | ||
| Infrequent | hepatitis | hepatitis | |
| Skin and subcutaneous tissue disorders | |||
| Very frequent | rash, itching | rash, alopecia, itching | palmoplantar erythrodysesthesia syndrome, rash, itching |
| Frequent | severe skin reactions, erythema, dry skin, vitiligo, eczema, alopecia, acneiform dermatitis | severe skin reactions, erythema, dry skin | severe skin reactions, acneiform dermatitis, dermatitis, dry skin, alopecia, eczema, erythema |
| Infrequent | lichenoid keratosis, psoriasis, dermatitis, papule, hair color changes | psoriasis, acneiform dermatitis, dermatitis, vitiligo, eczema | hair color changes, lichenoid keratosis, papule, psoriasis, vitiligo |
| Rare | toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema nodosum | hair color changes, lichenoid keratosis, papule | |
| Musculoskeletal and connective tissue disorders | |||
| Very frequent | musculoskeletal pain, arthrathgia | musculoskeletal pain, arthralgia | musculoskeletal pain, arthralgia, limb pain |
| Frequent | limb pain, myosity, arthritis | myositis, limb pain, arthritis | myosity, arthritisz, tenosynovitisa |
| Infrequent | tenosynovitis | tenosynovitis | Sjögren's syndrome |
| Rare | Sjögren's syndrome | Sjögren's syndrome | |
| Renal and urinary disorders | |||
| Frequent | nephritisbb, acute kidney injury | acute kidney injury, nephritisbb | |
| Infrequent | jadebb | ||
| administration site disorders | |||
| Very frequent | fatigue, asthenia, edema, increased body temperature | fatigue, asthenia, increased body temperature, edema | fatigue, asthenia, increased body temperature |
| Frequent | flu-like illness, chills | chills, flu-like illness | edema, influenza-like illness, chills |
| Laboratory and instrumental data | |||
| Very frequent | increased creatinine concentration in the blood | increased alt activity, increased act activity, increased creatinine concentration in the blood | |
| frequent | increased act activity, increased alt activity, hypercalcemia, increased alkaline phosphatase activity in the blood, increased bilirubin concentration in the blood, increased creatinine concentration in the blood | hypercalcemia, increased alt activity, increased act activity, increased alkaline phosphatase activity in the blood | increased activity of alkaline phosphatase in the blood, hypercalcemia, increased concentration of bilirubin in the blood |
| infrequent | increased amylase activity | increased bilirubin concentration in the blood, increased amylase activity | increased amylase activity |
*The incidence of adverse reactions listed in Table 2 may be associated not only with the use of pembrolizumab as monotherapy, but also with the underlying disease or with other drugs used in combination therapy.
†Based on standard queries to the database of adverse reactions, including bradyarrhythmias and tachyarrhythmias.
The following terms represent a group of related events that describe a medical condition rather than a single event:
a. infusion reactions (drug hypersensitivity, anaphylactic reaction, anaphylactoid reaction, hypersensitivity and cytokine release syndrome);
b. hypothyroidism (myxedema);
c. insufficiency of adrenal function (primary adrenal insufficiency, acute adrenal insufficiency, secondary adrenal insufficiency);
d. hypophysitis (hylopituitarism);
e. thyroiditis (autoimmune thyroiditis and thyroid disease);
f. diabetes mellitus type 1 (diabetic ketoacidosis);
g. Guillain-Barré syndrome (axonal neuropathy and demyelinating polyneuropathy);
h. myelitis (including transverse myelitis);
i. myasthenic syndrome (myasthenia gravis, including exacerbation);
j. aseptic meningitis (meningitis, non-infectious meningitis);
k. uveitis (inflammation of the iris and iridocyclitis);
l. myocarditis (autoimmune myocarditis);
m. pneumonia (interstitial lung disease and organizing pneumonia);
n. abdominal pain (stomach discomfort, upper abdominal pain, lower abdominal pain);
O. colitis (microscopic colitis, enterocolitis, hemorrhagic enterocolitis and autoimmune colitis);
R. pancreatitis (autoimmune pancreatitis and acute pancreatitis);
q. ulceration of the wall of the gastrointestinal tract (stomach ulcer and duodenal ulcer);
r. hepatitis (autoimmune hepatitis, immune-mediated hepatitis, drug-induced liver injury and acute hepatitis);
s. rash (erythematous rash, follicular rash, generalized rash, macular rash, maculous-papular rash, papular rash, pruritic rash, vesicular rash and genital rash);
t. itching (urticaria, papular urticaria, generalized itching and genital itching);
u. severe skin reactions (bullous dermatitis, exfoliative dermatitis, generalized exfoliative dermatitis, erythema multiforme, exfoliative rash, pemphigus, skin necrosis, toxicoderma and any of the following ≥ grade 3: acute febrile neutrophilic dermatosis, bruise, bedsore, psoriasiform dermatitis, drug rash , jaundice, pemphigoid, pruritus, generalized pruritus, rash, erythematous rash, generalized rash, maculopapular rash, pruritic rash, pustular rash and skin lesions);
v. vitiligo (skin depigmentation, skin hypopigmentation and eyelid hypopigmentation);
w. lichenoid keratosis (lichen planus and lichen sclerosus);
x. musculoskeletal pain (musculoskeletal discomfort, back pain, musculoskeletal stiffness, musculoskeletal chest pain and torticollis);
y. myositis (myalgia, myopathy, rheumatic polymyalgia and rhabdomyolysis);
z. arthritis (joint swelling, polyarthritis and joint effusion);
ah. tenosynovitis (tendinitis, synovitis and tendon pain);
bb. nephritis (autoimmune nephritis, tubulointerstitial nephritis and renal failure, acute renal failure or acute kidney injury with signs of nephritis, nephrotic syndrome and membranous glomerulonephritis);
ss. edema (peripheral edema, generalized edema, hypervolemia, fluid retention, eyelid edema and lip edema, facial edema, localized edema and periorbital edema).
description of some adverse reactions
Data for the following immune-mediated adverse reactions are based on information from patients receiving pembrolizumab in clinical studies at four dosing regimens (2 mg/kg every 3 weeks, 10 mg/kg every 2 or 3 weeks, or 200 mg every 3 weeks). Recommendations for the management of patients with these adverse reactions are described in the “special instructions” section.
immune-mediated adverse reactions
(see "special instructions")
immune-mediated pneumonitis
253 (4.3%) patients who received pembrolizumab developed pneumonitis, including grade 2, 3, 4 or 5 in 106 (1.8%), 69 (1.2%), 13 (0.2 %) and 9 (0.2%) patients, respectively. The median time to onset of pneumonitis was 3.3 months (range, 2 days to 26.8 months). median duration was 1.9 months (range, 1 day to 25.3+ months). Pneumonitis occurred more frequently in patients with a history of chest radiation therapy (8.1%) than in patients with no prior chest radiation therapy (3.4%). Discontinuation of pembrolizumab therapy due to pneumonitis was required in 98 (1.7%) patients. Pneumonitis resolved in 138 patients, complications were observed in 2 cases.
patients with NSCLC developed pneumonitis in 160 (5.7%) cases, including grade 2, 3, 4 or 5 in 62 (2.2%), 47 (1.7%), 14 (0.5 %) and 10 (0.4%) patients, respectively. In patients with NSCLC who had a history of radiation therapy, pneumonitis developed in 8.9% of cases.
immune-mediated colitis
107 (1.8%) patients receiving pembrolizumab developed colitis, including grade 2, 3, or 4 in 31 (0.5%), 62 (1.1%), and 3 (<0.1%) ) patients respectively. The median time to onset of colitis was 4.3 months (range, 7 days to 24.3 months). median duration was 0.9 months (range, 1 day to 8.7+ months). Discontinuation of pembrolizumab therapy due to colitis was required in 29 (0.5%) patients. Colitis resolved in 84 patients, complications were observed in 2 cases.
immune-mediated hepatitis
50 (0.8%) patients receiving pembrolizumab developed hepatitis, including grade 2, 3, or 4 in 8 (0.1%), 31 (0.5%), and 8 (0.1%) patients accordingly. The median time to onset of hepatitis was 3.6 months (range, 8 days to 21.4 months). median duration was 1.1 months (range, 1 day to 20.9+ months). Discontinuation of pembrolizumab therapy due to hepatitis was required in 19 (0.3%) patients. hepatitis resolved in 36 patients.
immune-mediated nephritis
22 (0.4%) patients who received pembrolizumab as monotherapy developed nephritis, including grade 2, 3, or 4 in 5 (0.1%), 14 (0.2%), and 1 (<0). .1%) patients respectively. The median time to onset of nephritis was 5.0 months (range, 12 days to 21.4 months). median duration was 2.6 months (range, 6 days to 12.0 months). Discontinuation of pembrolizumab therapy due to nephritis was required in 10 (0.2%) patients. nephritis resolved in 13 patients, complications were observed in 3 cases. In patients with non-squamous NSCLC treated with pembrolizumab in combination with chemotherapy including pemetrexed and platinum (n=488), the incidence of nephritis was 1.4% (all grades) with an incidence of 0.8% for grade 3 and 0 .4% for grade 4 severity.
immune-mediated endocrinopathies
46 (0.8%) patients receiving pembrolizumab developed adrenal insufficiency, including grade 2, 3 or 4 in 19 (0.3%), 20 (0.3%) and 3 (0.1%) %) of patients, respectively. The median time to onset of adrenal insufficiency was 5.4 months (range, 1 day to 17.7 months). median duration was not reached (range 3 days to 26.2+ months). Discontinuation of pembrolizumab therapy due to adrenal insufficiency was required in 4 (0.1%) patients.
Adrenal insufficiency resolved in 16 patients, complications were observed in 4 cases.
36 (0.6%) patients receiving pembrolizumab developed hypophysitis, including grade 2, 3, or 4 in 13 (0.2%), 19 (0.3%), and 1 (<0.1%) ) patients respectively. The median time to onset of hypophysitis was 5.9 months (range, 1 day to 17.7 months). median duration was 3.3 months (range, 3 days to 18.1+ months). Discontinuation of pembrolizumab therapy due to hypophysitis was required in 8 (0.1%) patients. hypophysitis resolved in 17 patients, complications were observed in 8 cases. 244 (4.1%) patients receiving pembrolizumab developed hyperthyroidism, including grade 2 or 3 in 64 (1.1%) and 7 (0.1%) patients, respectively. The median time to onset of hyperthyroidism was 1.4 months (range, 1 day to 22.5 months). median duration was 1.8 months (range, 4 days to 29.2+ months). Discontinuation of pembrolizumab therapy due to hyperthyroidism was required in 3 (0.1%) patients. hyperthyroidism resolved in 191 (78.3%) patients, complications were observed in 5 cases.
645 (11.0%) patients receiving pembrolizumab developed hypothyroidism, including grade 2 or 3 hypothyroidism in 475 (8.1%) and 7 (0.1%) patients, respectively. The median time to onset of hypothyroidism was 3.5 months (range, 1 day to 19.6 months). median duration was not reached (range 2 days to 32.6+ months). Discontinuation of pembrolizumab therapy due to hypothyroidism was required in 2 patients (<0.1%). hypothyroidism resolved in 153 (23.7%) patients, complications were observed in 10 cases. in patients with coli (n=241), the incidence of hypothyroidism was 14.1% (all severity levels) with a frequency of 0.4% for severity grade 3. In patients with HNSCC (n=909) who received pembrolizumab as monotherapy, the incidence of hypothyroidism was 16.1% (all grades) with a rate of 0.3% for grade 3. in patients with HNSCC (n=276) who received pembrolizumab in combination with chemotherapy, including platinum and 5-fu, the incidence of hypothyroidism was 15.2%, all cases were grade 1 or 2.
immune-mediated cutaneous adverse reactions
89 (1.5%) patients receiving pembrolizumab experienced immune-mediated severe skin reactions, including grade 2, 3, or 5 in 10 (0.2%), 65 (1.1%), and 1 (<0 .1%) patients respectively. The median time to onset of severe skin reactions was 3.3 months (range, 3 days to 19.4 months). median duration was 1.6 months (range, 1 day to 27.3+ months). Discontinuation of pembrolizumab therapy due to severe skin reactions was required in 9 (0.2%) patients. severe skin reactions resolved in 64 patients.
Rare cases of Stevens-Johnson syndrome and toxic epidermal necrolysis have been observed, some of them fatal (see sections "Dosage and Administration" and "Special Instructions").
other malignant tumors
monotherapy
Adverse events in patients with SCLC, gastric cancer, malignancies with high levels of microsatellite instability, HCC, or cervical cancer were generally similar to those in patients with melanoma or NSCLC.
complications of allogeneic hematopoietic stem cell transplantation for coronary artery disease
Of 23 patients with CC who underwent allogeneic hematopoietic stem cell transplantation after treatment with Keytruda®, 6 patients (26%) developed graft-versus-host disease, one fatal, and 2 patients (9%) severe obliterative endophlebitis of the hepatic veins developed after reduced-intensity conditioning, in one case with a fatal outcome. In 23 patients, the median follow-up period after allogeneic hematopoietic stem cell transplantation was 5.1 months (range: 0-26.2 months).
combination therapy
adverse events in previously untreated patients with NSCLC who received pembrolizumab in combination with carboplatin and paclitaxel or albumin-stabilized nanoparticulate paclitaxel in the keynote-407 study were generally similar to those in patients in the keynote-189 study, with the exception of alopecia (46% ) and arthralgia (21%).
In patients with HNSCC who received Keytruda® in combination with chemotherapy (platinum and 5-fu), the following adverse reactions were more severe (grade 3-4) and occurred more often (≥ 2% difference) compared with cetuximab in combination with chemotherapy (platinum and 5-fu): fatigue (7% versus 4.9%), mucosal inflammation (10% versus 5%), and stomatitis (8% versus 3.5%).
increased activity of liver enzymes during therapy with pembrolizumab in combination with axitinib for RCC
In a clinical trial in previously untreated patients with RCC treated with pembrolizumab in combination with axitinib, a higher than expected incidence of grade 3 and 4 alt elevations (20%) and grade 3 and 4 act elevations was observed. The median time to onset of ALT elevation was 2.3 months (range, 7 days to 19.8 months). in patients with an increase in ALT activity above UL ≥ 3 times (grade 2-4 severity, n=116), in 94% of cases the adverse reaction decreased to grade 0-1 severity. 59% of patients with increased ALT activity received systemic corticosteroids. if resolved, 92 patients (84%) were re-treated with pembrolizumab (3%) or axitinib (31%) monotherapy or combination therapy (50%). Among these patients, 55% did not experience a re-increase in ALT activity above UL > 3 times; all patients with a re-increase in ALT activity > 3 times UL experienced resolution. No grade 5 liver events were recorded.
deviation of laboratory values
among patients receiving pembrolizumab as monotherapy, the percentage of patients whose laboratory parameters had a grade 3 or 4 deviation from baseline was: a decrease in the number of lymphocytes 10.9%, a decrease in sodium concentration 8.2%, a decrease in hemoglobin concentration 6 ,3%, decrease in phosphate concentration 5.2%, increase in glucose concentration 4.8%, increase in act activity 2.8%, increase in alkaline phosphatase activity 2.7%, increase in alt activity 2.7%, decrease in potassium concentration 2, 2%, increased calcium concentration 1.8%, decreased neutrophil count 1.8%, increased potassium concentration 1.8%, increased bilirubin concentration 1.7%, decreased platelet count 1.7%, decreased albumin concentration 1.6% , decreased calcium concentration 1.5%, increased creatinine concentration 1.3%, decreased leukocyte count 0.8%, increased magnesium concentration 0.7%, decreased glucose concentration 0.6%, decreased magnesium concentration 0.2%, increased sodium concentration 0.2%.
among patients receiving pembrolizumab in combination with chemotherapy, the proportion of patients who had a deviation of laboratory parameters from baseline values to grade 3 or 4 was: a decrease in the number of neutrophils 26.7%, a decrease in the number of lymphocytes 23.9%, a decrease in hemoglobin concentration 19.1%, decreased leukocyte count 17.9%, decreased platelet count 12.2%, decreased sodium concentration 10.2%, decreased phosphate concentration 8.9%, increased glucose concentration 7.4%, decreased potassium concentration 6, 5%, increased creatinine concentration 3.3%, increased alt activity 3.1%, increased act activity 3.1%, decreased calcium concentration 3.1%, increased potassium concentration 3.0%, decreased albumin concentration 2.9% , increased calcium concentration 2.3%, increased alkaline phosphatase activity 1.2%, decreased glucose concentration 0.8%, increased bilirubin concentration 0.7%, increased sodium concentration 0.3%.
among patients receiving pembrolizumab in combination with axitinib, the proportion of patients who had deviations in laboratory parameters from baseline values to grade 3 or 4 was: increased alt activity 20.1%, increased act activity 13.2%, decreased lymphocyte count 10.8%, increased glucose concentration 8.9%, decreased sodium concentration 7.8%, decreased phosphate concentration 6.4%, increased potassium concentration 6.2%, increased creatinine concentration 4.3%, decreased potassium concentration 3, 6%, increased bilirubin concentration 2.1%, decreased hemoglobin concentration 2.1%, increased alkaline phosphatase activity 1.7%, increased INO 1.5%, decreased leukocyte count 1.4%, decreased platelet count 1.4% , prolongation of activated partial thromboplastin time 1.2%, decrease in the number of neutrophils 1.2%, increase in sodium concentration 1.2%, decrease in calcium concentration 0.7%, increase in calcium concentration 0.7%, decrease in albumin concentration 0.5% , decreased glucose concentration 0
,
2
%.
immunogenicity
in 36 (1.8%) of 2034 evaluable patients treated with Keytruda® in clinical trials at doses of 2 mg/kg every three weeks, 200 mg every three weeks, or 10 mg/kg every two or three weeks as monotherapy , the results of testing for antibodies to pembrolizumab were positive, among which 9 (0.4%) patients had neutralizing antibodies against pembrolizumab, there was no evidence of a change in the pharmacokinetic profile or safety profile after the appearance of binding or neutralizing antibodies against pembrolizumab.
children
The safety of pembrolizumab when used as monotherapy at a dosing regimen of 2 mg/kg every 3 weeks was assessed in the phase I/II study keynote-051 in 154 pediatric patients with advanced melanoma, lymphoma, or advanced, relapsed or refractory pd-positive solid tumors. l1. The safety profile in pediatric patients was similar to that in adult patients receiving pembrolizumab. The most common adverse reactions (reported with an incidence of at least 20% in pediatric patients) were fever (31%), vomiting (26%), headache (22%), abdominal pain (21%), anemia (21). %) and constipation (20%). Most reported adverse reactions when used as monotherapy were grade 1 or 2 in severity. 69 (44.8%) patients had one or more grade 3-5 adverse reactions, of which 6 (3.9%) patients had one or more adverse reactions that resulted in death. the frequency is based on all registered adverse drug reactions, regardless of the investigator's assessment of the cause-and-effect relationship.
reporting suspected adverse reactions
reporting suspected adverse reactions after state registration of a drug is important. this allows continuous monitoring of the benefit/risk ratio of the drug. Healthcare professionals are encouraged to report any suspected adverse reactions.
Is Keytruda safe?
The second study was conducted on 411 patients who had advanced melanoma and were taking Keytruda. However, severe side effects from the intestines, lungs and liver were rarely observed.
Most often, patients experienced side effects such as increased fatigue, cough, nausea, rash, itching, loss of appetite, constipation, diarrhea, and joint pain (source).
The information is for reference only. Euroonko cooperates with Israeli, European and American doctors who have accumulated significant experience with the drug Keytruda.
Book a consultation 24 hours a day
+7+7+78
KEYNOTE-185 Study
The KEYNOTE-185 (phase 3) trial assessed the efficacy and safety of lenalidomide in combination with low-dose dexamethasone with or without pembrolizumab in patients with multiple myeloma who are not eligible for autologous stem cell transplantation.
- Of 301 randomized patients, 19 died in the pembrolizumab group, compared with 9 patients in the control group (hazard ratio, 2.06 (95% CI: 0.93-4.55)).
- There was a 22% increased risk of severe toxicity (grade 3-5) in the pembrolizumab group, as well as a higher incidence of serious adverse events (54% vs. 39%).
- The causes of death in patients from the pembrolizumab group, not associated with disease progression, were pulmonary embolism, intestinal ischemia, myocarditis, heart failure, sudden death, pneumonia.
Source:
FDA. Drug Safety and Availability. August 31, 2017
Release form
Concentrate for the preparation of solution for infusion. Transparent or opalescent solution from colorless to light yellow.
1 bottle contains:
active ingredient: pembrolizumab 100.0 mg;
excipients: L-histidine 1.2 mg; L-histidine hydrochloride monohydrate 6.8 mg; polysorbate – 80 0.8 mg; sucrose 280 mg; water for injection up to 4.0 ml.
4 ml of the drug in a type I flint glass bottle (European Pharm., US Pharm.), sealed with a chlorobutyl rubber stopper, crimped with an aluminum cap and protected with a plastic cap.
Interaction with other drugs
Specific studies of the pharmacokinetic interaction of Keytruda with other drugs have not been conducted. Since pembrolizumab is eliminated from the circulation by catabolism, metabolic drug interactions should not be expected.
The use of systemic corticosteroids or immunosuppressants should be avoided before initiating Keytruda therapy, given their possible effect on the pharmacodynamic activity and efficacy of Keytruda. However, systemic corticosteroids or other immunosuppressants may be used after initiation of pembrolizumab treatment for the treatment of immune-mediated adverse reactions (see Precautions).
Side effects
From the blood and lymphatic system
: anemia, lymphopenia.
From the nervous system
: headache.
From the gastrointestinal tract:
nausea, diarrhea, constipation, vomiting, abdominal pain.
Metabolism and nutrition
: decreased appetite.
From the respiratory system, chest and mediastinal organs:
shortness of breath, cough.
From the skin and subcutaneous tissues
: itching, rash, vitiligo.
From the musculoskeletal and connective tissue side
: arthralgia, back pain.
From the laboratory parameters
: hypocalcemia, hyperglycemia, hyponatremia, hypoalbuminemia, increased alkaline phosphatase activity,
hypertriglyceridemia, increased ALT activity, increased AST activity, hypercholesterolemia, decreased bicarbonate concentration,
General and administration site disorders
: fatigue, fever, peripheral edema, asthenia.