“The number of leprosy cases has increased in Russia”, “More than 6 cases of leprosy in 2021” - such news headlines have excited people. After all, it seemed to many that such a disease had long since sunk into the past. And they often know little about it, and often more of something from the “mythological” category.
About what this disease is, how it is defined and whether it is possible to protect against it, AiF.ru was told by Ph.D., dermatovenerologist, associate professor of the Department of Hospital Pediatrics named after. Academician V. A. Tabolin, Faculty of Pediatrics, Federal State Autonomous Educational Institution of Higher Education, Russian National Research Medical University named after. N.I. Pirogov Alexandra Botkina.
Article on the topic Leprosy: a history of the disease and medieval misconceptions
Leprosy - what kind of disease is it?
Leprosy
(or leprosy) is a chronic infectious disease. It affects the skin and nerves located on the surface. The cause of leprosy is prolonged contact with the skin of a sick person. According to some experts, infection can also occur by air. Contrary to existing myths about the disease, occasional touching of the affected areas of the skin cannot cause leprosy. Prejudices also include the idea that leprosy is incurable and has an unfavorable prognosis (death). It should also be noted that there is a low threshold for the incidence of leprosy among people at risk, for whom there is a real risk of infection. No more than 10% of people do not have sufficient immunity and cannot resist the penetration of the pathogen, therefore it is believed that the pathogenicity of microorganisms that cause leprosy is relatively low.
The disease is not very contagious. No more than 7% of people worldwide suffer from it. The remainder of the population (about 95%) has immunity to this disease. It prevents infection from entering the body. Leprosy cannot be inherited and the child does not get the infection from the mother.
Leprosy peaked between the 12th and 16th centuries. Most of the inhabitants of Europe suffered from it. At that distant time, leprosy was considered a disease from which there was no cure. People affected by the infection were exiles. They were expelled from the city, forced to wear a crow's foot around their necks, and also to ring a bell if they were going to approach a healthy person.
Now the peak incidence has subsided, but cases of leprosy infection are still being diagnosed. Therefore, doctors need to be attentive to patients with characteristic complaints. In Russia, the last time the disease was officially registered was in a migrant from Tajikistan. This happened in 2015. The man worked in the capital at a construction site.
Facts from history:
- The disease in past centuries spread during the Crusades. When sick warriors and knights became infected and infected residents of other countries.
- Leprosy was stopped by the plague. During the epidemic, people with weak immune systems who suffered from leprosy fell ill first.
- In France there was a decree. According to it, all people with leprosy were subjected to a “religious tribunal.” They were taken to church, had a funeral service, and then were laid in a coffin. When the coffin was lowered into the grave, they said the phrase: “You are dead to us, not alive.” Then several shovels of earth were thrown onto the coffin. After this, the person was taken out of the grave and sent to the leper colony. He couldn't return to the house. He remained in a specialized institution until the end of his days. At the same time, his relatives considered him dead.
- People with leprosy were deprived of all social rights. They were not allowed to go to church, entertainment venues, or fairs. Infected people were prohibited from swimming in bodies of water, drinking running water, eating with healthy people, and even talking to them.
- Catholics allowed couples to divorce if one spouse had leprosy, although the Catholic Church rejects divorce as such.
- In the Middle Ages, leprosy was called by different terms, including: Phoenician disease, black sickness, lazy or slow death, mournful disease. The name "leprosy" was coined in Russia. This word comes from the Old Russian “kazit”, that is, to disfigure or distort.
Content:
General information
Leprosy - what kind of disease is it?
Leprosy disease - syn. Hansen's disease (Hansen) is an infectious chronic disease (mycobacteriosis), characterized by a long incubation period, systemic nature and relapsing course (Wikipedia). It is characterized by damage to ectoderm derivatives, namely the skin, peripheral nervous system, mucous membranes and, much less frequently, internal organs, the musculoskeletal system, and eyes. Leprosy is a relatively less contagious infection. The disease has a centuries-old history. In the Middle Ages, those infected with leprosy were considered “lepers” and, since there was no effective treatment, they were subjected to lifelong isolation in leper colonies (specialized medical institutions).
According to WHO statistics, today the number of leprosy patients in the world is estimated at 10-15 million. At the same time, 96% of all new cases of leprosy occur in 22 countries, the main ones being India, Brazil, Indonesia, Ethiopia, Angola, Sudan, Congo . And only 4% comes from other countries. In Europe, leprosy has been reported among refugees/migrants from the Middle East and Africa. The main regions in the world where leprosy is endemic are shown below.
Regions where leprosy is most endemic are shown in red.
In the Russian Federation, the Astrakhan region is one of the regions endemic for leprosy. Significantly fewer patients are identified in regions such as the Far East, Siberia, and the North Caucasus. However, in general, the incidence of leprosy in the Russian Federation is sporadic, which is due to the introduction of complex anti-leprosy measures into practice. The main contingent of sick people are people who have been in contact with the patient: family members, relatives of the patient, people living in leprosy foci for a long period and migrants.
Today, despite the universal availability of specific treatment (antibiotic therapy) and the downward trend in the number of patients, new cases of leprosy are reported annually, and the prospect of its complete elimination in the world remains doubtful.
Leprosy occupies a special position as a factor influencing the physical and psycho-emotional state of the patient. Specific clinical manifestations, frequent complications, a high risk of disability, and forced lifestyle changes, in particular limiting contacts against the background of a pronounced cosmetic defect, contribute to the development of a feeling of inferiority, depression and difficulty adapting to society.
Below are photos of people with leprosy.
Geography and features of the spread of leprosy
Today, no more than 2 million people live with leprosy worldwide. A decrease in the number of infected people occurred in the nineties; before that time there were about 12 million of them. In Russia, as of 2007, 600 people with leprosy were registered, 35% of them were treated in a hospital, and the rest were treated at home.
Leprosy today practically does not occur in regions characterized by cold climates; it is mainly common in the tropics and subtropics. The disease is observed in Asian and African countries (India, countries of the former USSR, Japan, Korea and several others), as well as in Central and South America.
Leprosy is not a widespread disease, but nevertheless it affects approximately 11 million people worldwide (according to WHO). According to statistics, men are three times more likely to get leprosy, but if we take into account the age of those infected, then among children there is a higher susceptibility to microorganisms than among adults.
The infection is spread by a sick person. It can also be carried by armadillos and monkeys. Leprosy bacteria are found in soil and water, but the likelihood of infection through them is extremely low.
The bacterium that causes leprosy cannot exist outside the human body. It quickly breaks down in air. At the same time, bacteria can exist in human corpses for a long time.
The size of the population suffering from leprosy largely depends on the economic status of the country. What matters is the level of sanitary and hygienic skills of people and their financial well-being.
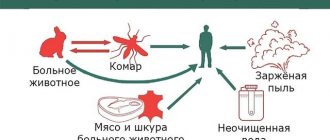
The infection can spread in 2 ways:
- By airborne droplets. Bacteria are released when you cough, sneeze or talk. At the same time, a lot of pathogenic microorganisms enter the air.
- In case of violation of the integrity of the skin. The infection can be acquired through tattooing, or through the bite of insects that feed on blood.
The longer the contact with a sick person, the higher the risk of infection. Thus, the likelihood of infection increases if a person is intimate with a leprosy patient or lives next door to him. Although statistics indicate that even if there is a person with leprosy in the family, close relatives get sick no more than in 12% of cases.
The incidence is high among children, since their protective forces are not yet fully formed. It has been established that black men suffer from leprosy more often than women. Among white-skinned people such a trend is not observed.
If a person with leprosy lived in the apartment, then after his departure the premises must be disinfected.
Features of its implementation:
- First of all, linen and dishes are disinfected, as well as those places where mucus and sputum secreted by a person may be located.
- All objects are boiled in a 2% concentration of soda solution. You can also soak them for an hour in a 1% chloramine solution.
- The walls and floors in the living room are sprayed with chloramine at a concentration of 0.5%, or bleach at a concentration of 0.2%.
Prevention
Preventive measures boil down to:
- Isolation of patients in leper colonies until bacterioscopic negativity, after which treatment continues on an outpatient basis.
- Regular examination of all family members of a leprosy patient, as well as persons living in leprosy-endemic regions.
- To carry out chemoprophylaxis with special (anti-leprosy) drugs for persons who are in long-term contact with the patient (in the family) and for persons who have been identified as having isolated the causative agent of leprosy.
- To carefully comply with the requirements of antiseptics during childbirth in women with leprosy. Transferring a child to artificial feeding immediately after birth from mothers with leprosy.
- Administration of the BCG vaccine to enhance anti-leprosy immunity.
- Control/mandatory examination of all foreign citizens for leprosy arriving in the country from areas where this disease is endemic.
Causes of leprosy
The causative agent of leprosy, Mycobacterium leprae, was discovered by Hansen in 1874. From the moment of infection until the first symptoms of leprosy appear, it can take from two to 20 years, with an average of 3–10 years.
Mycobacterium leprae, considered the cause of leprosy, has much in common with Mycobacterium tuberculosis, but, unlike them, they are cultivated only on the skin of experimental animals and do not grow on nutrient media of artificial origin.
Mycobacteriaceae are a family of actinomycetes. The only genus is Mycobacterium. Some members of the genus Mycobacterium (e.g. M. tuberculosis, M. leprae) are pathogenic for mammals
The bacterium looks like a stick, which has a straight or curved shape. Its ends are rounded. It does not exceed 7.0 microns in length and 0.5 microns in diameter. The bacterium is resistant to treatment with alcohol compounds. It is classified as an obligate intracellular parasite that invades tissue macrophages.
The source of the spread of the bacterium is humans. He releases it into the environment. Pathogenic flora is present in breast milk, saliva, nasal mucus, urine, feces and semen, and discharge from wounds. The mycobacterium enters the mucous membranes or damaged areas of the skin, and then reaches the nerve fibers and blood vessels. Along with blood and lymph, pathogens spread throughout the body.
If a person is healthy, then he has immunity to the bacterium and infection will not occur. At risk are children, people who abuse alcohol, patients with chronic diseases and those with weak immunity.
List of sources
- Yushchenko A.A., Irtuganova O.A., Duiko V.V. and others. Modern methods of diagnosis, treatment and prevention of leprosy (a manual for doctors). Astrakhan, 1997. 33 p.
- Grigorieva Yu.G., Belopasov V.V. Pathogenetic mechanisms and the role of serum markers in the development of leprosy neuropathies // Current issues in clinical and experimental leprology: Proceedings of the International Scientific and Practical Conference. Astrakhan, 2011. pp. 53–67.
- Belopasov V.V. Leprosy. Chronic neuroinfections. 2nd ed. M.: GEOTAR-Media, 2021. pp. 392–415.
- Leprosy. Fact Sheet No. 101. World Health Organization (October 2016).
- Duiko V.V. Quality of life and features of management of patients with leprosy. Russian Journal of Skin and Venereal Diseases 2013; 2. P.54-57.
Leprosy symptoms
The incubation period of the disease is quite long and ranges from 3 to 7 years, although sometimes it can be shortened to six months or extended for 15-20 years. There is evidence that leprosy existed for 40 years in the incubation period. However, the person did not show any symptoms of the disease. Even after leprosy has left the incubation period, the patient may not have any symptoms of infection for a long time.
Leprosy primarily affects tissues that come into contact with air. Symptoms of leprosy include damage to the skin, mucous membranes of the mouth and sinuses, as well as nerves located on the surface. In advanced cases, leprosy penetrates into the deep layers of the skin and causes destruction of nerve fibers, as a result of which deformities occur and the usual appearance of a person is distorted.
The causative agents of leprosy are not the direct cause of death of the toes. If the infection is not treated in a timely manner, it leads to tissue necrosis in the arms and legs. On fingers deprived of blood supply, a secondary infection quickly develops, caused by bacteria that enter the injured skin, thus, it is because of the bacterial infection that the fingers and toes ultimately die.
There are two types of leprosy:
- Tuberculoid leprosy
- Lepromatous form
Tuberculoid leprosy
This infection has the most favorable prognosis. In humans, the skin is affected, as well as the nerve fibers passing along the periphery. Sometimes visceral internal organs are affected.
If the disease is of the tuberculin type, the symptoms of leprosy are flat spots with a red or white tint or covered with scales. When the disease has just begun to develop, several spots resembling erythema are found on the dermis. Their boundaries are clearly defined. They grow quickly and coalesce, forming plaques that rise above the surface of the skin. In the affected areas of the skin, the sheaths of nerve fibers become denser, their thickening gradually leads to loss of sensitivity of individual tissues. Then the plaque in the middle becomes dense, the dermis begins to atrophy. Over time, its dimensions reach 15 mm in diameter. The lesions are multiple and can be found on the chest, lower back, and back.
With this form of the disease, the nail plates suffer, they lose their natural color, begin to break, peel and collapse. The nails become gray and streaks appear on them.
Neurological symptoms develop early. In those places where there are skin defects, sensitivity worsens, hair falls out, the color of the dermis changes, and the glands responsible for the production of sebum and the secretion of sweat suffer. The skin becomes dry and rough patches appear on it. When the disease has just begun to develop, skin sensitivity either decreases or increases for a short period of time. Then it decreases and disappears completely.
When pathogens penetrate large nerve trunks, destructive changes occur in bones and joints, most often the limbs are affected. The person begins to move his fingers with difficulty, and contractures appear. Trophic ulcerative defects form on the legs. Subsequently, the fingers, hands and nose atrophy and are rejected. This process is called mutilation.
If the facial nerve is affected, the facial muscles stop moving and the eyelids do not close completely.
In medicine, there are cases of spontaneous disappearance of symptoms of tuberculin-type leprosy.
Lepromatous form of leprosy
In this form, mycobacteria quickly multiply in the skin and cause the formation of nodules (lepromas) or plaques with a characteristic scaly structure. Over time, the skin becomes thicker and deep folds appear on it. Most often they can be seen on the patient's face, which resembles a lion's muzzle - a characteristic symptom of leprosy.
This disease has a severe course. First of all, the patient’s skin and mucous membranes are affected. After which the pathological process spreads to the internal organs and the nervous system.
The main symptoms of lepromatous form of leprosy:
- Skin damage.
Symmetrically located spots appear on the skin, which look like erythromatous rashes. Each such spot contains a huge number of mycobacteria leprosy. The spots do not have clear outlines. They can appear on the palms, face, legs, buttocks and forearms. At first the spots have a glossy sheen, but on top they are smooth. As the pathology progresses, the spots turn from red to rusty or brown. In this case, there is no deterioration in sensitivity in the area of their concentration. In this form, stains can persist for many years. Sometimes they disappear, and sometimes they transform into lepromas and infiltrates. In the latter case, the spots have the appearance of plaques without a clear boundary. If vascular paresis occurs, the spots become brown in color.
- Loss of skin function.
If skin infiltration occurs, the sebaceous glands begin to work in enhanced mode. Therefore, the dermis becomes greasy and acquires shine. The vellus hair follicles and sweat gland ducts become wider. Therefore, the skin resembles the appearance of an orange peel. As the pathology progresses in the area of infiltrate formation, sweat ceases to be released. First, vellus hair stops growing, and then the person’s mustache, beard and eyebrows begin to fall out.
- Facial lesion.
The face with infiltrates that appear on it begins to resemble a “lion’s face.” All skin folds and wrinkles deepen, the brow ridges protrude forward, the nose and cheeks become thicker, the lips and chin are divided into segments.
- Formation of leprosy.
When the disease has just begun to develop, infiltrates form on the patient’s skin. They are not found on the scalp, eyelids, elbow creases or armpits. Then, at the site of the infiltrates, lepromas are formed, which can reach 3 cm in size. There are especially many of them on the face, ears, hands, forearms, legs, back and buttocks. Lepromas do not hurt, have a smooth surface, and can peel off. Most often, over time, lepromas become soft, but sometimes, on the contrary, they harden. It happens that they resolve on their own. After them, a depigmented spot remains on the skin, which slightly sinks inward. If a person does not receive proper therapy, then ulcers form on leprosy, which are very painful. After they disappear, scars remain on the skin.
- Damage to mucous membranes.
The nasal mucosa is especially often affected. If the disease is severe, the damage affects the mouth, lips and tongue. The patient experiences nosebleeds and nasal breathing worsens as lepromas begin to grow in the nasal cavity. The organ itself undergoes deformation. Sometimes a person loses the ability to speak. This happens when the disease affects the vocal cords.
- Other symptoms.
In addition to the symptoms of the disease described above, a person’s visual organs may suffer. Keratitis, blepharitis, iridocyclitis, lens opacity, and conjunctivitis are often diagnosed. The pathological process may involve nerve fibers, lymph nodes, blood vessels, testicles and liver. As the disease progresses, a person develops paralysis and paresis, and trophic ulcers form. When the liver suffers, the patient is diagnosed with chronic hepatitis. Men may develop orchitis and epididymitis orchitis. Subsequently, the patient’s mammary glands begin to increase in size according to the female type, and symptoms of infantilism develop, which is associated with hormonal imbalance.
Leprosy of dimorphic and undifferentiated type
If a patient develops a dimorphic type of leprosy, then the clinical picture will combine symptoms of tuberculoid and lepromatous types of leprosy.
The undifferentiated form of the disease may be accompanied by damage to nerve fibers. The peroneal, auricular and ulnar nerves are primarily affected. On the skin of patients, areas with altered pigmentation appear; in these places, sensitivity decreases or completely disappears, and the sweat glands stop working. The more severely the nerve fibers are affected, the more intense the symptoms of polyneuritis. Patients often experience paralysis and paresis, and deformities of the arms and legs may occur. Areas of ulceration appear on them, which do not heal for a long time.
Complications
Among the complications of leprosy are the following conditions:
- damage to the skin beyond recognition;
- serious disturbances in the functioning of the nervous system;
- blindness, glaucoma;
- muscle weakness;
- deformation of the hands and feet, loss of fingers;
- infertility;
- renal failure;
- erectile disfunction;
- chronic damage to the inner surface of the nose;
- loss of sensation in different parts of the body.
Diagnosis of leprosy
The disease can be suspected based on its manifestations. When leprosy is in an advanced stage of development, the diagnosis will be obvious to the doctor. Patients have no eyebrows, lepromas form on the body and face, limbs are paralyzed, fingers and hands may be missing, the nose is severely deformed, etc.
If the disease has just begun to develop, the absence of obvious symptoms of leprosy may present difficulties in making a correct diagnosis. In this case, the patient can be referred for consultation to a neurologist, dermatologist, infectious disease specialist or other specialist, since the manifestations of the disease are quite diverse.
To confirm leprosy, it will be necessary to conduct a bacteriological examination of scrapings taken from the fingers, earlobes, and nasal mucosa. Lepromas, the contents of lymph nodes, or discharge from areas of ulceration can be taken for histological analysis. Mycobacterium leprosy will be found in the collected materials.
To clarify the degree of loss of skin sensitivity, functional tests are performed. They are carried out with Minor's reagent, with nicotinic acid, with mustard plaster and with histamine.
The lepromin test is also used. If his reaction is positive, then the patient develops leprosy of the tuberculoid type, and if it is negative, then the lepromatous or borderline form can be diagnosed. When the test gives a weak positive reaction, an undifferentiated variant of the disease is suspected.
Undifferentiated type of leprosy
The undifferentiated (borderline) type of leprosy develops when the patient has not yet developed a type of immunological activity. With a favorable course, the tuberculoid type of leprosy subsequently develops; with a low degree of immunological reactivity, the lepromatous type of leprosy develops. The lepromine reaction, depending on the direction of the pathological process, can be negative or positive. The undifferentiated (borderline) type of leprosy combines the clinical manifestations of 2 main types of the disease, but with a milder course.
Rice. 19. The undifferentiated (borderline) type of leprosy develops in cases where the type of immunological activity has not yet formed.
Treatment of leprosy
For several centuries, leprosy was treated with haulmugra oil, which was replaced by sulfone drugs. Diaphenylsulfone (dapsone) has become the main treatment for leprosy since 1950. Its therapeutic effect can only be noticed after a long period of time. While not a specific treatment for leprosy, sulfone drugs inhibit the development of the disease. In mild cases, recovery occurs within two years; in more severe situations, leprosy treatment requires about eight years.
With the emergence in the 1980s of strains resistant to the main treatment for leprosy, dapsone, complex regimens came into medical practice. Clofazimine is currently widely used for the lepromatous type of leprosy.
Today, leprosy is a curable disease. It is important to identify it at an early stage of development, before it leads to disability. A sick person is placed in a leper colony or treated at home.
Now only those people who have severe skin defects are hospitalized. Inpatient treatment is also indicated for primary therapy. Patients with relapse of leprosy are hospitalized. People who have had a negative bacteriological test and have few skin rashes can be treated at home.
Patients are prescribed 2 or 3 drugs at once that have pathological activity against leprosy bacteria. Be sure to carry out therapy aimed at increasing immunity. Drug correction can be implemented using drugs such as: Methyluracil, Dapsone, Rifampicin, Pyrogenal, gamma globulin. Patients are advised to take vitamin-mineral complexes.
Main directions of drug therapy:
- Sulfone drugs:
Solusulfone, Diaphenylsulfone, Diucifon.
- Antibacterial agents:
Rifampicin, Lampren, Clofazimine, Ofloxacin, Ethionamide.
The drugs are prescribed for up to six months. If a person tolerates the treatment well, then there are no breaks between courses. The patient is prescribed one sulfone drug and two antibiotics. To prevent bacteria from developing resistance, medications must be alternated every 2 courses. In general, therapy should last at least a year, and sometimes it takes about 3 years. Some patients require lifelong treatment.
If a patient is diagnosed with multibacillary leprosy, he is prescribed Rifampicin, Dapsone and Clofasamine. The drugs are given to patients free of charge.
Treatment regimen:
- 600 mg Rifampicin + 300 mg Clofazimine orally once a month under medical supervision. At home, a person should take Dapsone 100 mg + Clofazimine 50 mg once a day. The course of therapy lasts a year. Such recommendations are given by WHO.
- In America, the treatment regimen is somewhat different. There, patients are offered 600 mg of Rifampicin + 100 mg of Dapsone + 100 mg of Clofazimine once a day. The course lasts a year. If a person is diagnosed with a borderline form of the disease, then he is prescribed Dapsone for 10 years. In the lepromatous form of leprosy, this drug will need to be taken for life.
If a person is diagnosed with oligobacillary leprosy, WHO recommends that such patients take 600 mg of Rifampicin once a month and 100 mg of Dapsone every day. The course of treatment according to this regimen lasts 6 months. If the patient has a single skin lesion, then he is offered a single dose of Ofloxacin 400 mg + Rifampicin 600 mg + Myocycline 100 mg.
In America, patients are prescribed 600 mg of Rifampicin + 100 mg of Dapsone once a day. The course of therapy lasts a year. If a patient is diagnosed with an indeterminate or tuberculoid form of leprosy, he is prescribed Dapsone for 3 years. In case of a borderline form of the disease, the drug will need to be taken for 5 years.
Dapsone is an inexpensive and safe drug used to treat leprosy. Occasionally, patients develop hemolysis and mild anemia, allergic dermatosis. The latter complication can be severe. Dapsone syndrome develops even less frequently.
Rifampin is even more active against leprosy bacteria than Dapsone. However, treatment with its use is more expensive. Side effects include: liver damage, flu-like syndrome, thrombocytopenia, renal failure.
Clofazimine is a safe drug. Its only side effect is a change in skin color, but after completion of the course of therapy, the color of the dermis is restored.
If the patient develops mild skin erythema (the first or second episode of inflammation), then patients are offered Aspirin. For severe erythema, Prednisone 40-60 mg is prescribed once a day. Complement treatment with an antibiotic. When skin lesions occur again, patients are advised to take Thalidomide 100-300 mg once a day. However, this drug is prohibited for use by women who are planning a pregnancy. Its side effects are leukopenia and constipation.
While antibacterial agents can stop the progression of the disease, they do not allow one to get rid of existing deformities or correct existing damage to nerve fibers. Therefore, it is so important to begin treatment in the early stages of the disease. The drugs are used in a complex regimen, since mycobacterium leprosy can quickly develop resistance to one antibiotic.
Answers to popular questions
- What is the prognosis for leprosy?
If a person begins to receive treatment at an early stage of the disease, the prognosis is favorable. When leprosy is in an advanced form, there is a high probability that the patient will become disabled.
- Are there leper colonies in Russia?
Yes, in Russia there are 4 leper colonies, which are located in Astrakhan, Krasnodar Territory, Stavropol Territory and Sergiev Posad. Sick people in leper colonies have their own houses and run their households. Doctors live next to the leper colony.
- After recovery, are already formed deformities reversible?
No, if a person has lost his hands or fingers, they will not grow back. Treatment is aimed at eliminating leprosy bacteria in the body. To cope with paralysis, paresis and contractures, the patient is recommended physiotherapy, exercise therapy, and sometimes surgery is performed.
- What are the complications of leprosy?
The main complications include: trophic ulcers, damage to the organs of vision with the development of complete blindness, loss of voice, deformation of the nose, loss of fingers, paralysis. If there is no therapy, the person dies from cachexia, asphyxia or amyloidosis.
- Is it possible to get vaccinated against leprosy? What are the measures to prevent the disease?
There is no vaccine for leprosy. There is evidence that BCG placement significantly reduces the likelihood of infection with Mycobacterium leprosy. To prevent infection, you need to support your immune system and also avoid contact with sick people. If a person with leprosy lives in a family, then he should have his own personal belongings, from a comb to dishes. All family members should be regularly examined for detection of Mycobacterium leprosy in their body, and also carefully observe the rules of personal hygiene.
Forecast
The prognosis of leprosy is determined by such factors as the clinical form of the disease, the duration of its course, and the time of initiation of treatment. In most cases, with timely early diagnosis of the disease (within a year from the onset of characteristic symptoms), it is possible to minimize the risk of developing disabling consequences. With late diagnosis of the disease, paresis, sensory disturbances, and disfiguring deformities that are difficult to treat may develop and persist. In the absence of specific therapy, there remains a high risk of death of patients from asphyxia , intercurrent diseases , leprosy cachexia , and amyloidosis .