Typhoid is the general name for a group of diseases caused by infection, the symptoms of which are impaired consciousness combined with high fever and intoxication.
The disease is dangerous, so it is important to have an idea of the mechanism of infection, symptoms, treatment and prevention.
What is typhoid fever
Typhoid fever is an infectious disease that affects the gastrointestinal tract and adjacent lymph nodes and is caused by the Salmonella bacterium.
Salmonella typhi has a complex structure, is resistant to environmental factors, and can be present for a long time in soil layers, water bodies, on vegetables and fruits, and in dairy products.
Infection occurs through the fecal-oral route: the microorganism enters the body through the mouth along with water or food (meat and dairy products are especially dangerous). The bacterium is also shed in the stool of both an infected person and a salmonella carrier. A child can become infected through contact or household contact.
After entering the oral cavity, salmonella enters the intestine and invades the ileum; after entering the lymph, the infectious agent begins to actively multiply and migrate into the blood. As a result, intoxication and the first signs of infection appear.
An increase in incidence is observed in summer and autumn; high ambient temperatures and flies contribute to the proliferation of typhoid fever.
The prevalence depends on the level of socio-economic development of the state. During periods of war, outbreaks of the disease were recorded; currently no more than 30 cases are registered in Russia annually, mostly imported from other countries. Children and young people who actively travel and eat outside the home are at risk.
Diagnosis methods
The most reliable methods for diagnosing typhoid fever today are laboratory tests.
- Agglutination reaction to detect antibodies to the Salmonella typhi antigen. This test is carried out two weeks after infection. Its disadvantage is the possibility of a false positive result if another Salmonella bacterium is present in the body.
- Indirect hemagglutination. The test can detect typhoid fever during the first week of illness.
- ELISA. This method is highly accurate and allows you to determine the presence of any antibodies to bacterial antigens. Its advantage is the ability to conduct the test at all stages of the disease, including during the recovery period.
For general clinical and bacteriological studies, samples of the patient’s blood, feces and urine are taken. During the last phase of the disease, duodenal intubation is performed, during which a sample of the contents of the duodenum is taken.
Why is he dangerous?
The seriousness of the disease is that after the stick enters the blood, it spreads throughout the body and penetrates the organs and systems. The most dangerous presence of salmonella is in the heart, liver, kidneys, and spleen.
Damage to the heart by a toxin can provoke inflammation of the heart muscle, a decrease in heart rate and blood pressure, and hypoxia.
When an infection enters the kidneys, a disruption of all functions develops, urine output becomes less frequent or stops, and urea and creatinine begin to accumulate in the body, causing intoxication.
The lungs stop performing their functions, they fill with fluid and begin to swell, and it becomes more difficult for the patient to breathe.
Typhoid fever is dangerous due to complications: intestinal perforation and peritonitis, bleeding in the intestines, infectious-toxic shock, thrombosis of intestinal vessels, pneumonia, pyelonephritis, meningitis, abscess.
How to cure
Since the infection is extremely virulent, and the disease is severe and often complicated, treatment of typhoid fever must be carried out in the infectious diseases department of the hospital, in conditions of complete isolation. During illness, the patient remains in bed and does not leave the infectious disease ward. Therapy continues until the patient's body temperature returns to normal for ten consecutive days and includes:
- taking antibiotics (orally or by injection);
- replacement of fluid losses (orally or intravenously);
- a gentle diet with a high content of protein products;
- in case of intestinal perforation - surgical removal of a section of intestine with multiple injuries or closure of a single perforation with drainage of the peritoneum.
Taking antibacterial drugs continues for several months. Constant monitoring of patients' condition allows for timely detection of complications and prevention of their development. After discharge from the hospital, the patient is monitored at the dispensary for a certain time.
Classifications of the disease
Typhoid fever can occur in a typical form (with obvious signs) and atypical (when the disease develops back or has mild symptoms), with or without complications.
According to bacterial carriage, the disease can be primary or secondary, acute, chronic or temporary.
There are three degrees of severity:
- Light. Characteristic: an increase in temperature no higher than 38°C for no longer than a week, loose stools no more than five times in 24 hours, persistence of symptoms for no more than 7 days, no complications.
- Moderate severity. Characteristic: an increase in temperature to 39°C for no longer than two weeks, vomiting, loose stools no more than ten times in 24 hours, persistence of symptoms for up to 20 days, moderate enlargement of the spleen and liver, complications may occur.
- Severe degree. The temperature rises to 40°C and lasts up to three weeks, vomiting is present for about a week, loose stools more than 10 times for more than 1.5 weeks. The spleen and liver are significantly enlarged, complications are present.
Symptoms of typhoid fever depending on the stages
The latent period of the disease is 7-25 days, then a gradual increase in symptoms begins. The main signs of typhoid fever:
- infectious intoxication;
- roseola-like rashes on the skin in the abdomen, sides of the chest, inner surfaces of the shoulders;
- enlarged spleen and liver;
- inflammation of the small intestine and constipation;
- typhoid bronchitis;
- inflammatory process in the intestinal lymph nodes.
Symptoms of the disease increase depending on the stages:
- At the initial stage, the patient experiences weakness, loss of appetite, fever, and clouded consciousness. Then a cough, bloating, and diarrhea appear. The doctor may detect an enlarged spleen and liver, pain in the abdomen when pressed, a brown coating on the tongue, and redness of the oropharynx.
- At the peak of the disease, a rash appears; in rare cases, the palms and soles may acquire a yellowish tint. The febrile state and signs of toxin poisoning reach the limit of severity, hallucinations are possible. The heart beats slower, and wheezing is heard in the lungs. The phase lasts 1.5 weeks.
- At the final stage, the symptoms fade: intoxication is alleviated, consciousness returns, the temperature normalizes, the liver and spleen shrink.
Publications in the media
Typhoid fever (BT) is an acute infectious disease (generalized salmonellosis), characterized by ulcerative lesions of the lymphatic system of the small intestine, bacteremia; manifested by intoxication, typical fever, roseola rashes on the skin, enlarged liver and spleen. Incidence : 0.12 per 100,000 population in 2001
Classification • According to clinical forms •• Typical form (classical clinical variant) •• Atypical forms: ••• Erased ••• Subclinical ••• With a predominance of damage to individual organs and systems (colotif, meningotif, pneumotyphoid, etc.) • By severity: •• Mild form •• Moderate form •• Severe form • By course: •• Uncomplicated •• With complications and relapses.
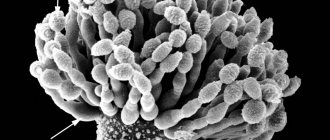
Etiology . Salmonella typhi is an aerobic gram-negative rod of the Enterobacteriaceae family.
Epidemiology • BT is an anthroponotic disease. Sources of infection are sick people and bacteria carriers. The greatest epidemiological danger is posed by bacteria carriers and patients with erased and mild forms of the disease. Chronic bacteria carriers are the main reservoir of infection in nature • Summer-autumn seasonality is typical • The mechanism of infection is fecal-oral. The water factor is of primary importance in the occurrence of epidemic outbreaks of BT. Contact-household and food transmission routes cause sporadic cases of the disease.
History • Contact with a patient with BT or a bacteria carrier 1 month before the onset of the first symptoms of the disease • Stay of the patient in a region that is epidemiologically unfavorable for BT.
Clinical picture
• Periods of the course •• Incubation (7–25 days, on average 12–14) •• Initial (4–7 days) •• Height of the disease (1–2 weeks) •• Resolution of the disease (up to 1 week) •• Reconvalescence ( 2–4 weeks).
• Clinical symptoms •• Fever is the most consistent objective symptom. BT is characterized by 3 types of temperature curves ••• Trapezoidal Wunderlich temperature curve - classic, with a sequential change of stages of increasing body temperature, constantly high values and decline; their duration corresponds to the initial period of the disease, its height and resolution ••• Botkin’s wavy temperature curve with a sequential alternation of 3-4-day episodes of febrile and subfebrile body temperature ••• Kildyushevsky’s temperature curve with a short (1-2 days) stage of constantly high temperature and a long (2–2.5 weeks) decline stage; typical for children • • Intoxication (anorexia, headache, insomnia) - at altitude the development of delirium, psychotic states and disorders of consciousness (status typhosus) is possible • • Damage to the gastrointestinal tract - thickened tongue coated with a gray-brown coating with tooth marks on the lateral surfaces ( typhoid tongue), shortening of percussion sound over the ileocecal area (Padalka's symptom), pain and infiltration determined by palpation of this area (Obraztsov-Gausman symptom), symptoms of enterocolitis (flatulence, diarrhea with stool in the form of pea puree or constipation), colotyphoid • • Hepatosplenomegaly (determined by palpation from the end of the first or beginning of the second week) • • Skin lesions - pallor of the skin, roseola rash protruding above the surface of the skin (roseola elevata), not abundant, discrete, appears on the 8-12th day of illness, localized on the skin of the chest and abdomen, persists for 3–4 days and disappears without a trace. During the period of resolution, elements of prickly heat (crystallina miliaria) and yellow discoloration of the skin of the palms and feet (Fillipovich's symptom) may appear. • Damage to the cardiovascular system - bradycardia and dicrotia of the pulse, moderate arterial hypotension. With the development of complications - collapse, tachycardia • • Damage to the central nervous system - meningitis and meningoencephalitis of a serous and purulent nature, meningotif • • Damage to the respiratory system - infiltrative forms of pneumonia, pneumotyphoid • • Damage to the kidneys - symptoms of nephritis or hemolytic-uremic syndrome, nephrotyphoid.
Laboratory studies • Isolation of the pathogen or detection of its Ag •• Bacteriological method: sowing and isolation of the pathogen from blood (hemoculture), feces (coproculture), urine (urinoculture), bile (bilinoculture), bone marrow (myeloculture); positive results of pathogen isolation are an absolute diagnostic sign of BT •• Immunofluorescent analysis methods for detecting pathogen Ag in biological fluids • Detection of antibodies to pathogen Ag in the RNGA •• AB to O-Ag (thermostable lipopolysaccharide, endotoxin) is detected in the first week of the disease •• AT to H-Ag (heat-labile, flagellated) is recorded in convalescents and vaccinated people, appears on days 6–8 of the disease and persists during the period of convalescence; a simultaneous positive result of the reaction with O- and H-Ag with a predominance of O-agglutinin titers indicates an actively ongoing process •• Antibodies to Vi-Ag (heat-labile, somatic) do not have diagnostic or prognostic value, the reaction is used to identify carriers (positive reaction - 1:5 and higher) and vaccinated (Vi-Ag is included in vaccines) • CBC - leukopenia, relative lymphocytosis, aneosinophilia; an increase in the number of eosinophils in peripheral blood is a prognostically favorable sign.
Differential diagnosis is carried out with all diseases with a gradual increase in body temperature during the first 5–7 days and with high body temperature that persists for more than a week, especially if no other causes of its occurrence are identified. Wunderlich's rule: the diagnosis of BT is unlikely if on the 1st or 2nd day a body temperature of 40 °C is noted, and on the 4th day the body temperature does not reach 39 °C.
TREATMENT
• Mandatory hospitalization.
• Bed rest until the 10th day of normal body temperature.
• Diet with mechanical, thermal and chemical sparing; diet No. 2, complex of vitamins.
• Causal treatment - antibiotic therapy, does not prevent the development of relapses, complications and chronic bacterial carriage • • Chloramphenicol. Treatment regimen for adults: 0.5 g 4 times a day until the 4th day of normal body temperature, 0.5 g 3 times a day until the 8th day and 0.5 g 2 times a day until the 12th day of normal body temperature. The treatment regimen for children is the same, but the initial dose is 75–80 mg/kg/day, followed by a dosage reduction by 25% and 50%, respectively. The drug is recommended to be taken 1 hour before or 2 hours after meals, washed down with plenty of water • • Ceftriaxone 30 mg/kg/day IV or IM in 2 divided doses (1 g every 12 hours) or cefoperazone 60 mg/ kg/day IV in 2 doses for 14 days • • Ampicillin 1.5 g orally 4 times a day or amoxicillin 2 g 3 times a day until the 10th day of normal body temperature (for 4–6 weeks during carriage) • • Co-trimoxazole, ciprofloxacin, ofloxacin.
• Symptomatic therapy - relief of intoxication (infusion detoxification therapy), improvement of repair processes of the intestinal mucosa and correction of metabolic disorders (infusions of immunoglobulins and other blood products, vitamins).
• Treatment of emergency conditions •• For infectious-toxic shock - infusion of plasma replacement drugs (for example, polyglucin), GC in high doses (prednisolone up to 30 mg/kg IV or dexamethasone for 48 hours, first 3 mg/kg IV, then 1 mg/kg every 6 hours), dopamine, sodium bicarbonate • • For intestinal bleeding - strict bed rest, cold on the stomach, fasting for 8-10 hours, infusions of blood products, fibrinolysis inhibitors; if possible - abstain from surgery • • In case of perforation of the intestinal wall - emergency surgery.
Complications can develop with mild or even erased forms of BT • Intestinal bleeding develops at 2–3 weeks of illness, accompanied by a sudden decrease in body temperature (“incision” of the temperature curve), increased heart rate, disappearance of its dicrotia, decreased blood pressure, clearing of consciousness (apparent well-being) , tarry stools (sometimes mixed with scarlet blood). With massive bleeding, death is possible • Typhoid perforation of the intestine occurs at 3–4 weeks of illness, and can be single or multiple. Symptoms: abdominal pain localized in the right iliac region (the first few hours), symptoms of peritoneal irritation, sudden decrease in body temperature, tachycardia, increased leukocytosis • Infectious-toxic shock is typical for severe forms, observed during the first week of the disease.
Current and prognosis . The course of BT is relapsing. Relapses in typhoid-paratyphoid diseases mean the return of the main symptoms of the disease during periods of resolution and convalescence against the background of normal body temperature. Relapses appear in the first 1.5-3 weeks of the convalescence period, and sometimes later - after 2-3 months of normal body temperature; there can be several of them - from 1 to 9 (usually one). Each relapse is accompanied by bacteremia, and its clinical picture does not differ from that during the main wave of the disease. The fundamental difference is the short duration of manifestations (7–10 days). With timely and adequate treatment of BT and its complications, the prognosis is favorable.
Prevention • Prescription of convalescents no earlier than 21 days from the moment of normalization of body temperature and receipt of negative results of a three-time bacteriological examination of feces, urine and a single study of bile (bile is examined on the 10th day of normal body temperature) • The first collection of material is carried out on the 5th day of normal body temperature , and then at 5-day intervals • Convalescents are subject to 3-month dispensary observation to identify possible relapse and bacterial carriage • Active prevention is carried out in regions with high incidence rates (25 or more cases per 100,000 population) using combined chemical vaccines • Children up to Typhoid bacteriophage is prescribed for 7 years • Disinfection is carried out at the source of TB • Contact persons are placed under medical observation for 25 days with daily thermometry and mandatory bacteriological examination of feces and urine • General measures: strict control of the quality of drinking water and the activities of production, processing and sales enterprises food products.
Features of BT in children • Infants, due to their dietary habits and relative isolation from potential sources of infection, rarely get sick • With age, the risk of the disease increases • Predominance of symptoms of gastrointestinal tract damage - frequent vomiting, diarrhea, up to the development of intestinal toxicosis • Temperature curve or the wrong type, or Kildyushevsky type • Intoxication is manifested by central nervous system excitation (restlessness, psychomotor agitation, convulsive seizures, meningism) • Complications are rarely observed • Absence of characteristic bradycardia • Favorable course.
Reduction . BT - typhoid fever
ICD-10 • A01 . 0 Typhoid fever