Listeriosis is an infectious disease caused by gram-positive bacteria Listeria monocytogenes in humans and animals, Listeria ivanovii in animals.
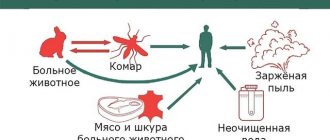
Listeriosis affects humans and animals (rodents, domestic cats and dogs, cows, sheep). Listeria can be infected through food by consuming meat, dairy products, soft cheeses, semi-finished products, seafood, vegetables and fruits, and can multiply in refrigerator conditions at a temperature of +4 - +6ₒ C and remain viable under vacuum packaging. They are stable in the environment: in water, soil. Capable of penetrating into the human body through the mucous membranes of the eyes and respiratory tract when inhaling dust that contains the pathogen. When Listeria crosses the placenta, it can infect the fetus.
Listeriosis is an opportunistic infection that affects people with a weakened immune system (mature people with chronic diseases, HIV-infected people, pregnant women, newborns), and those with congenital immune defects.
Listeriosis as an occupational disease can occur among veterinarians, meat processing and dairy workers, and livestock farms.
Classification and clinical picture of listeriosis
From the moment of infection with Listeria until the appearance of clinical symptoms, it can take from 2 to 4 weeks, sometimes up to two months.
Clinical symptoms are varied: there can be either an asymptomatic course or a severe septic condition.
The following forms of the disease are distinguished:
- Glandular form. Characterized by fever, headache, weakness, and enlarged lymph nodes. There may be plaque on the tonsils, unilateral purulent conjunctivitis.
- The nervous form most often develops in children and the elderly and is manifested by meningitis and meningoencephalitis. Against the background of high temperature, severe headache and impaired consciousness appear.
- Septic form. Muscle and joint soreness, hepatitis, and pneumonia are also present.
- Listeriosis in pregnancy can develop at any stage of pregnancy. It is usually asymptomatic or mild with a favorable outcome. The fetus becomes infected with listeriosis through the placenta with the development of intrauterine infection. If infected in the early stages of pregnancy, developmental defects and intrauterine fetal death may occur.
- Listeriosis in newborns occurs unfavorably, in a severe septic form, the mortality rate reaches 20%.
Listeriosis
Listeriosis is an infectious disease of humans and animals, caused by Listeria, characterized by multiple sources of the infectious agent, a variety of routes and factors of its transmission, polymorphism of clinical manifestations, and high mortality.
According to ICD 10, it is registered under code A32. In the minds of many doctors, listeriosis is a new, rare, recently discovered disease. Meanwhile, the first reliable information about him appeared more than 80 years ago. In 1926, Murray and his co-authors described an outbreak of the disease among rabbits and guinea pigs at the Cambridge University nursery, caused by a previously unknown bacterium that causes a monocytic blood reaction in animals. Three years later, the same microbe was first isolated from a sick person, and in 1940 it was named Listeria monocytogenes in honor of the English surgeon Lister, who proposed the antiseptic method. Since then, the disease has been called listeriosis [9]. Until recently, listeriosis was dealt with primarily by veterinary specialists, because the disease affects many animals, including agricultural ones (sheep, cattle, pigs, horses, etc.), causing their death.
Before 1960, human listeriosis was rare; in 1960–1982 More than 10 thousand cases have already been reported in the world, and subsequently thousands of cases are registered annually. At the end of the last and beginning of the current century, large outbreaks of listeriosis in humans were described in Western Europe (France, Great Britain, Switzerland, Finland) and North America (USA, Canada) with the number of cases ranging from several dozen to 300; they are associated with the consumption of animal products (soft cheeses, semi-finished meat products, vacuum-packed sausages, sausages, butter, etc.), vegetable products (vegetable salads, cabbage), as well as seafood (shellfish, shrimp). The authors of relevant publications always pay attention to the high mortality rate among patients [3, 9, 21, 22, 23]. Currently, listeriosis is considered one of the most important foodborne infections. In this regard, the epidemic situation around the world continues to worsen; and this is due to a number of reasons, including some biological features of Listeria [2, 5, 6, 10, 24].
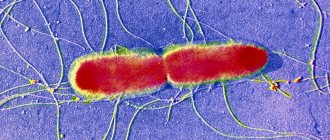
Etiology. The causative agent of human listeriosis, Listeria monocytogenes, belongs to the genus Listeria, is a short, gram-positive, non-spore-forming rod of regular shape, facultative anaerobes. Listeria can transform into L-forms and parasitize intracellularly, which causes insufficient effectiveness in some cases of antibacterial therapy, explains the tendency of listeriosis to have a protracted and chronic course, the possibility of a latent form and bacterial carriage. Highly stable in the external environment, grow in a wide range of temperatures (from 1 to 45 ° C) and pH (from 4 to 10), tolerate low temperatures well and are able to reproduce at temperatures of 4–6 ° C in soil, water, on plants, in organs of corpses. They multiply in various food products (milk, butter, cheese, meat, etc.) at the temperature of a household refrigerator. At 70°C they die in 20–30 minutes, at 100°C in 3–5 minutes; are inactivated by solutions of formalin (0.5–1%), chloramine (3–5%) and other conventional disinfectants [9, 13]. Listeria is sensitive to penicillins, tetracyclines, aminoglycosides, glycopeptides, new generation fluoroquinolones; resistant to cephalosporins [2, 3, 9, 20, 21, 23, 25].
The most important factor in the pathogenicity of Listeria is listeriolysin O, which has hemolytic activity and determines the virulence of the microbe; less significant ones include phosphatidylinazitol, internalin A, internalin B, ActA protein, etc. [7, 8, 9].
Epidemiology. Previously, listeriosis was considered a typical zoonosis, in which the source of the causative agent of infection are various animals, but now it is classified as a sapronoses, and the main source and reservoir of the pathogen are recognized as environmental objects, natural substrates in which listeria is able to multiply - primarily soil. Listeria is also isolated from plants, silage, dust, water bodies and wastewater.
The main route of human infection with listeriosis is through food, through the consumption of various food products (see above) without preliminary heat treatment. Soft cheeses, as well as fast food products - hot dogs, hamburgers, etc. are of increased danger. Contact routes of infection (from infected animals and rodents), aerogenous (indoors when processing skins, etc.) are also possible. wool, as well as in hospitals), transmissible (from insect bites, in particular ticks). Of particular importance is the possibility of transmission of Listeria from a pregnant woman to the fetus, either during pregnancy (transplacentally) or through contact of the newborn with the birth canal of the mother (intrapartum) [2, 3, 5, 9, 21, 23]. Listeria can cause nosocomial infections, in particular in maternity hospitals; outbreaks that arise in this case are described both in domestic and foreign literature. In the human population, asymptomatic carriage of Listeria is 2–20%; listeria is isolated from the feces of healthy people in 5–6%.
There is no data in the literature on the possibility of infection from a person with listeriosis or a carrier of the bacteria. The exception is pregnant women, who can transmit the infection to the fetus.
In Russia, official registration of listeriosis began in 1992; since then, from 40 to 100 patients are identified annually in the country. Obviously, these figures do not reflect the true incidence and will increase as doctors of different specialties become more familiar with the variants of clinical manifestations and subject to the improvement of laboratory diagnostics.
The current and predicted future increase in the incidence of listeriosis is due to several reasons, namely the high adaptive ability of listeria, their ability to reproduce in an abiotic environment, including in food products during their production (cheese ripening, preparation of meat, fish and chicken semi-finished products for “quick food”) and storage; an increase in the proportion of people with various immunodeficiencies in the human population who are most susceptible to this infection; predominance of the food route of infection.
Pathogenesis. Not being highly pathogenic microbes, Listeria causes clinically manifest disease in humans only when the immune defense factors are weakened [2, 6, 8, 17, 18, 20]. L.monocytogenes are facultative intracellular parasites; immune responses during this infection are carried out using cellular mechanisms. Any congenital or acquired dysfunction of T-lymphocytes creates the preconditions for the development of the disease. Listeriosis is usually classified as an opportunistic infection; people with various immunodeficiencies are at greatest risk of the disease (pregnant women, newborns, elderly and senile people, HIV-infected people, cancer patients, patients with diabetes mellitus, renal or heart failure, chronic alcohol intoxication, drug addiction and etc.). According to some foreign sources, listeriosis occurs 150–300 times more often in HIV-infected people than in the general population, but others do not confirm this [26]. Listeria enters the human body through the mucous membranes of the gastrointestinal tract, respiratory organs, eyes, damaged skin, and is transmitted through the placenta of a pregnant woman to the fetus. With an adequate immune response of the body, production of a sufficient number of subpopulations of T-lymphocytes, activation of macrophages, further promotion of Listeria does not occur. Otherwise, from the “entry gate” microbes can spread hematogenously and lymphogenously, penetrate into the reticuloendothelial system (liver, spleen, lymph nodes), into the central nervous system, kidneys, etc., where further reproduction of listeria occurs with the formation listerioma-granulomas, consisting of reticular, monocytic cells, cellular detritus, altered polymorphonuclear leukocytes. Listeria is able to overcome the blood-brain barrier, affecting both the membranes and the substance of the brain, where an inflammatory reaction develops and subcortical abscesses are often formed [1, 11, 22]. The granulomatous process in congenital listeriosis is generalized and is interpreted as granulomatous sepsis.
Clinic. The duration of the incubation period ranges from 1–2 days to 2–4 weeks, occasionally up to 1.5–2 months.
The clinical manifestations of listeriosis are varied depending on the route of penetration of the microbe into the human body, the reaction of the immune system and a number of other cofactors (age, gender, concomitant diseases, etc.).
The main forms of listeriosis are: glandular; gastroenteric; nervous; septic; bacterial carriage.
Listeriosis of pregnant women and newborns is distinguished separately.
Depending on the duration of the disease, acute (1–3 months), subacute (3–6 months) and chronic (longer than 6 months) listeriosis are distinguished.
The glandular form occurs in two variants: anginal-glandular and oculoglandular. The first of them is characterized by an increase in body temperature, intoxication, tonsillitis (ulcerative-necrotic or membranous), enlargement and soreness of the submandibular, less often cervical and axillary lymph nodes. Enlargement of the liver and spleen is also possible. The febrile period is 5–7 days. The hemogram shows monocytosis (“monocytic tonsillitis”). The disease resembles infectious mononucleosis.
For the oculoglandular variant, unilateral purulent conjunctivitis is typical; There is pronounced swelling of the eyelids, narrowing of the palpebral fissure. Nodular rashes are detected on the transitional fold of the conjunctiva. Visual acuity decreases; The parotid and submandibular lymph nodes on the corresponding side become enlarged and painful.
The gastroenteric form is characterized by an acute onset, a rapid increase in body temperature to high levels, and severe intoxication (chills, headache, arthralgia and myalgia). After a few hours, gastrointestinal symptoms appear in the form of nausea, repeated mild vomiting, cramping abdominal pain, frequent loose stools, sometimes mixed with mucus. Characterized by bloating and pain on palpation, especially pronounced in the right iliac region. The duration of fever is 5–7 days or more. This form of listeriosis is clinically similar to many acute intestinal infections and cannot be identified without laboratory confirmation. The high mortality rate characteristic of this form (20% and above) is caused either by the development of infectious toxic shock (ITS) or by the transition to more severe forms—nervous, septic forms [9, 16].
The nervous form is one of the most common, occurring most often (according to previous ideas) in children under three years of age and in adults over 45–50 years of age, usually manifesting itself in the form of meningitis or meningoencephalitis. The incidence of listeria meningitis is about 1–5% of all bacterial meningitis, but among some categories, particularly patients with cancer, it is the most common form of meningitis.
We have our own observations of 53 patients with listeriosis, 32 of whom were diagnosed with meningitis; the majority were young and middle-aged people without concomitant and background diseases that could cause immunosuppression.
According to clinical signs, listeriosis meningitis does not differ from bacterial meningitis of other etiologies. The most common symptoms are high body temperature, impaired consciousness and increasingly intense headache. However, in some cases the temperature is low-grade or does not rise at all. Compared with other bacterial meningitis, listeria meningitis is less likely to have meningeal signs (including neck stiffness), and the cerebrospinal fluid (CSF) is less likely to have a neutrophilic composition and a high protein content [1, 11, 14, 15, 20, 22]. Thus, among the 32 adult patients with listeria meningitis we observed, lymphocytes predominated in the CSF in 5 of them. This fact deserves special attention from clinicians, since lymphocytic pleocytosis of the CSF usually gives grounds to assume a viral etiology of meningitis and not to prescribe antibacterial therapy, which is certainly indicated for meningitis of listeriosis etiology. One of the notable features of the described meningitis is severe complications: hydrocephalus, rhombencephalitis, encephalopolyneuritis, dementia, etc. In addition to the brain, damage to the spinal cord is possible in the form of intramedullary abscesses, cysts, arachnoiditis, myelitis, etc.
The course of the nervous form is usually severe, mortality reaches 30% or higher, and relapses occur in approximately 7% of cases.
Listeriosis meningitis (meningoencephalitis), tonsillitis, conjunctivitis can be both independent forms of listeriosis, and one of the manifestations of the septic form or precede it.
The septic form is characterized by repeated chills, fever with sharp fluctuations in body temperature, intoxication (headache, weakness, loss of appetite, muscle aches, etc.), enlarged liver and spleen. A large-spotted rash may appear on the skin, mainly around large joints; on the face the rash may be in the form of a “butterfly”. Hepatitis with jaundice often occurs, there may be polyserositis, pneumonia. The hemogram reveals anemia and thrombocytopenia. The development of the septic form is sometimes gradual or subacute; the first signs of the disease in these cases are either catarrhal symptoms (sore or sore throat, pain in the eyes) or dyspeptic symptoms (nausea, vomiting, stool disorders).
Severe septic form of listeriosis is more common in newborns, persons with severe immunodeficiencies, patients with liver cirrhosis, chronic alcoholism; mortality reaches 60%. The cause of death may be ITS, massive bleeding due to the development of disseminated intravascular coagulation (DIC), acute respiratory and acute renal failure [9, 14, 15].
With all the above-described forms of listeriosis, leukocytosis (up to hyperleukocytosis), band shift, and sometimes monocytosis are observed in the blood. However, contrary to the name of the microbe, pronounced monocytosis is not often recorded in the hemogram: in 30–40% according to the literature [9], in isolated cases according to our observations [14].
In addition to those listed, such rare forms of listeriosis as endocarditis, dermatitis, arthritis, osteomyelitis, abscesses of various organs, mumps, urethritis, prostatitis, etc. have been described.
Listeria hepatitis can occur in a septic form, and in some cases it is accompanied by jaundice. It is extremely rare that hepatitis with severe hyperenzymeemia, signs of hepatic cellular failure, and symptoms of acute hepatic encephalopathy (AHE) dominates the clinical picture of listeriosis. We observed a case of listeria sepsis with a fatal outcome in a 19-year-old patient without any signs of immunodeficiency. The clinical picture was dominated by fulminant hepatitis syndrome. Similar descriptions are given in the literature [12].
Listeriosis in pregnant women. A decrease in the level of cellular immunity during pregnancy causes increased susceptibility to listeria infection. In the United States, listeriosis in pregnancy accounts for more than a quarter of the total number of cases of this infection and more than half of the cases in people aged 10–40 years.
Listeriosis can develop at any stage of pregnancy, although most cases occur in the second half. Acute listeriosis in pregnant women is either completely asymptomatic or mild, with erased polymorphic symptoms, so the correct diagnosis is often established retrospectively after the death of the fetus or newborn. A pregnant woman may have fever, muscle pain, catarrhal symptoms from the upper respiratory tract, conjunctivitis; in these cases, influenza or ARVI is suspected. Some patients show symptoms of gastroenteritis, others have urinary tract inflammation. Damage to the nervous system, the most common clinical form of listeriosis, is, oddly enough, extremely rare in pregnant women [3, 10, 15].
Maternal listeriosis can lead to transplacental infection of the fetus, and the development of intrauterine infection can be quite intense, and therefore the sick mother and fetus seem to exchange infection: first the mother infects her fetus, then the fetus infects the mother a second time, causing her to have a secondary wave of the disease, in the form of fever of unknown etiology. Due to this feature, listeriosis is sometimes called a “ping pong” infection.
A characteristic clinical feature of listeriosis in pregnant women is a critical decrease in body temperature after termination of pregnancy; subsequently the fever usually does not recur.
Acute and chronic listeriosis in a pregnant woman can cause severe obstetric pathology: early termination of pregnancy at different stages, recurrent miscarriage, fetal malformations, intrauterine death, etc.
Listeria infection can persist in a woman’s body for quite a long time, in particular in the kidneys, and become more active during pregnancy, against the background of declining immunity. Screening studies revealed that listeria is isolated from women who have had urogenital diseases in 16–17% of cases. Almost all women who fell ill with listeriosis had a “rich” obstetric and gynecological history: cervical erosion, adnexitis, pyelonephritis, induced and spontaneous abortions, etc. [12].
Listeriosis of newborns. Unlike pregnant women, in whom listeriosis usually has a benign course and clinical recovery occurs even without treatment, listeriosis in newborns is a severe generalized disease with high mortality (more than 20%), occurring as sepsis. The share of listeriosis in perinatal mortality is 25%. The timing of the onset and clinical manifestations of listeriosis in newborns depend on the time and route of infection (antenatal or intrapartum, transplacental or aspiration infection).
In the case of transplacental infection of the fetus, if intrauterine death has not occurred, a child with congenital listeriosis is usually born prematurely, with reduced body weight. After a few hours, sometimes after 1-2 days, his condition sharply worsens, body temperature rises, papular, sometimes hemorrhagic exanthema appears, anxiety, shortness of breath, cyanosis, convulsions occur, and in most cases death occurs, the cause of which may be pneumonia, purulent pleurisy, hepatitis, meningoencephalitis, damage to other organs, intrauterine sepsis [10, 12, 15].
With intrapartum infection, the child looks healthy immediately after birth; clinical signs of listeriosis in the form of sepsis appear after the 7th day of the child’s life.
Fetal aspiration of infected amniotic fluid can result in severe lung damage; the mortality rate reaches 50%.
In some newborns, listeriosis develops 10–12 days after birth and in these cases usually occurs in the form of meningitis with a mortality rate of up to 25%. This form is most typical for nosocomial outbreaks of listeriosis in maternity hospitals [6].
Specific laboratory diagnostics. It is extremely difficult to establish a diagnosis of listeriosis based on clinical and epidemiological data due to the polymorphism of clinical manifestations and the impossibility in some cases of identifying the source of infection. Moreover, laboratory diagnostics acquires essentially decisive importance. A preliminary conclusion can be given based on the results of bacterioscopic examination of Gram-stained smears of CSF sediment and amniotic fluid.
A final diagnosis is only possible using a bacteriological method [3, 10, 13, 15] or polymerase chain reaction (PCR).
Listeria can be isolated from patients from various clinical samples: blood, CSF, tonsil smears, lymph node punctures, vaginal and cervical smears, feces, purulent discharge from the eyes, etc. If listeria sepsis is suspected, a blood culture is performed, for meningitis and meningoencephalitis, CSF is performed, and for newborn disease, meconium is cultured. In a woman who gave birth to a stillborn child or with signs of listeriosis, the amniotic fluid, placenta, and discharge from the birth canal are examined.
In addition, it is possible to isolate Listeria in smears from the oropharynx and from the feces of healthy people, which is regarded as asymptomatic carriage.
Methods for serodiagnosis of listeriosis have not been developed in detail. When determining specific antibodies using currently available methods, both false-negative and false-positive research results occur.
Treatment. It is necessary to prescribe antibacterial therapy as early as possible. For a localized (glandular, gastroenteric) form, one of the following drugs is used: ampicillin, amoxicillin, co-trimoxazole, erythromycin, tetracycline, doxycycline, chloramphenicol in medium therapeutic doses orally [10, 19, 23].
For generalized infection (nervous, septic forms), listeriosis in newborns, a combination of ampicillin (adults 8–12 g/day; children 200 mg/kg/day) or amoxicillin with gentamicin (5 mg/kg/day) or amikacin is recommended throughout the febrile period. period and another 3–5 days, and in severe cases up to 2–3 weeks from the moment the temperature normalizes. If such therapy is ineffective, it is necessary to change the antibiotic, taking into account the sensitivity of the Listeria strain isolated from the patient. In recent years, vancomycin and meropenem have been reported to be effective.
If necessary, infusion detoxification, as well as desensitizing and symptomatic therapy, and treatment of concomitant diseases are carried out.
Ampicillin is used to treat pregnant women. A woman who has given birth to a child with listeriosis is given a course of antibiotic therapy with ampicillin or doxycycline in two cycles of 7–10 days with an interval of 1.5 months.
Prevention of listeriosis. Includes control over food products provided for by relevant regulatory documents [13]; sanitary educational work among the population, especially risk groups.
Fast food products that have not undergone long-term heat treatment (for example, hamburgers), as well as feta cheese, soft cheeses and raw milk should be excluded from the diet of pregnant women.
To prevent listeriosis in newborns, it is necessary to examine women with a burdened obstetric and gynecological history, as well as those who have constant contact with soil and/or animals. Women with identified listeriosis, clinically manifest or asymptomatic, are subject to specific therapy.
Thus, in Russia, as in many other countries of the world, there is currently an increase in the incidence of listeriosis, and not only elderly patients with various concomitant diseases are affected, but also young, previously healthy individuals. Listeriosis is characterized by polymorphic clinical symptoms, so patients can consult doctors of different specialties (general practitioners, gastroenterologists, neurologists, obstetricians-gynecologists, etc.). In sporadic cases, diagnosis of listeriosis is impossible without bacteriological confirmation or DNA detection by PCR. With timely initiation and adequate antibiotic therapy, the disease is curable.
Literature
- Dekonenko E. P., Kupriyanova L. V., Golovatenko-Abramov K. V. et al. Listeriosis meningitis and its complications // Neurological Journal, 2001; 2:23–26.
- Krasovsky V.V., Vasiliev N.V., Derkach N.A., Pokhil S.I. Results of a five-year study of listeriosis in Ukraine // Journal. microbiol., 2000; 3:80–85.
- Pokrovsky V.I., Godovannyy B.A. Listeriosis In the book: Pokrovsky V.I. (ed.) Infectious diseases. M: Medicine; 1996, 291–296.
- Practical guide to anti-infective chemotherapy. Ed. L. S. Strachunsky, Yu. B. Belousov, S. N. Kozlov. Smolensk, MAKMAH, 2007. 464 p.
- Rodina L.V., Manenkova G.M., Tsvil L.A. Epidemic situation of listeriosis in Moscow // Epidemiol. and infectious b-ni, 2000; 6:15–18.
- Rodina L.V., Manenkova G.M., Timoshkov V.V. Factors and routes of infection of the population of Moscow with listeriosis // Epidemiol. and infectious b-ni, 2002; 4:48–50.
- Sereda A. D., Kotlyarov V. M., Vorobyov A. A., Bakulov I. A. Immunity in listeriosis // J-l microbiol., 2000; 5:98–102.
- Sorokina M. N., Ivanova V. V., Skripchenko N. V. Bacterial meningitis in children. M.: Medicine, 2003. 320 p.
- Tartakovsky I. S. Listeria: role in human infectious pathology and laboratory diagnostics // Klin. microbiol. and antimicr. Chemoter., 2000; 2:20–30.
- Tartakovsky I. S., Maleev V. V., Ermolaeva S. A. Listeria: role in human infectious pathology and laboratory diagnostics. M.: Medicine for everyone; 2002. 200 p.
- Chestnova T.V. Two cases of listeriosis with unusual clinical manifestations. Materials of the international scientific and practical conference. Pokrov: VNIIV ViM, 2001; 120–123.
- Chestnova T.V. Diagnosis of listeriosis in newborns // Epidemiol. and infectious b-ni, 2001; 3:45–47.
- Epidemiology and prevention of listeriosis. Method. instructions. M.: Federal TsGSEN Ministry of Health of Russia, 2002. 12 p.
- Yushchuk N.D., Karetkina G.N., Klimova E.A. et al. Listeriosis: variants of the clinical course // Ter. archive, 2001; 11:48–51.
- Yushchuk N.D., Karetkina G.N., Dekonenko E.P. et al. Listeriosis with damage to the nervous system // Ter. archive, 2007; 11:57–60.
- Carrique-Mass JJ, Hokeberg I, Andersson V et al. Febrile gastroenteritidis after eating on-farm manufactured fresh cheese— an outbreak of listeriosis? // Epidemiol. Infect. 2003; 130(1):79–86.
- Doganay M. Listeriosis: clinical presentation // Immunol. Med. Microbiol. 2003; 31(3):173–175.
- Gierowska-Bogusz B., Nowicka K., Drejewicz H. Clinical and laboratory diagnosis of listeria monocytogenes on the basis of own investigations// Med. Wieku Rozwoj. 2000; 4 (2 Suppl 3): 89–96.
- Girmenia C., Iori AP, Bernasconi S., Testy AM et al. Listeriosis in recipientof allogeneic bone marron transplants from unrelated donors // Eur. J. Clin. Microbiol. Infect. Dis. 2000; 19 (9):711–714.
- Gordon RS Listeria monocytogenes infections // Indian. J. Pediatr. 1995; 62(1):33–39.
- Mead PS, Slutsfeer L., Dietz V. et al. Food-related illness and death in the United States // Emerging Infect. Dis. 1999; 5:607–626.
- Mylonakis E., Hohmann EL, Calderwood SB Central nervous system infection with listeria monocytogenes. 33 years'experience at a general hospital and review of 776 episodes from the literature// Medicine (Baltimore). 1998; 77(5):313–336.
- Rainis T., Potasman I. Listeria monocytogenes infections—ten years'expirience // Harefuah 1999; 137(10):436–440.
- Rocourt J., Jacguet C., Reilly A. Epidemiology of human listeriosis and seafoods // Int. J. Food Microbiol. 2000; 62(3):197–209.
- Temple ME, Nahata MC Treatment of listeriosis. Ann. Pharmacoter. 2000; 34(5):656–661.
- Valencia Ortega M.E., Enriques Crego A., Laguna Cuesta F. et al. Listeriosis: an infrequent infection in patient with HIV // An.Med. Interna. 2000; 17 (12): 649–651.
G. N. Karetkina , Candidate of Medical Sciences, Associate Professor MGMSU , Moscow
Laboratory diagnosis of listeriosis
Laboratory diagnosis is based on identifying listeria from biological material: blood, cerebrospinal fluid, eye discharge, oropharynx, nasopharynx, feces. For diagnosis, the bacteriological method and the polymerase chain reaction (PCR) method are used.
But it must be taken into account that listeria can be detected in stool in healthy individuals, so detection of it in stool by PCR without clinical symptoms does not serve as a basis for diagnosis. But pregnant women who are found to have listeria in their stool and urine, even in the absence of symptoms of disease, are subject to treatment.
- Microbiological (cultural) study on Listeria (Listeria monocytogenes) with determination of sensitivity to antimicrobial drugs.
- Listeria (Listeria monocytogenes), qualitative determination of DNA (CSF, AF) - allows you to detect listeria in the cerebrospinal fluid or amniotic fluid.
- Listeria (Listeria monocytogenes), qualitative determination of DNA (whole blood).
- Listeria (Listeria monocytogenes), qualitative determination of DNA (feces)