Rash due to secondary syphilis
Secondary syphilis is characterized by the appearance of a rash on the skin and mucous membranes - secondary syphilides. The rash with secondary fresh syphilis is abundant and varied (polymorphic): spotted, papular, vesicular and pustular. The rash can appear on any part of the skin and mucous membranes.
- The most abundant rash at the first rash, often symmetrical, the elements of the rash are small in size, always brightly colored. Often against its background one can detect residual signs of primary syphiloma (chancre), regional lymphadenitis and polyadenitis.
- Secondary recurrent syphilis is characterized by less profuse rashes. They are often grouped to form fancy patterns in the form of garlands, rings and arcs.
- The number of rashes in each subsequent relapse becomes less and less. At the end of the second stage of syphilis, monorelapses occur, when the clinical picture is limited to a single element.
Elements of the rash in secondary syphilis have some features: high prevalence at the beginning of the secondary period, sudden appearance, polymorphism, clear boundaries, peculiar coloring, lack of reaction of surrounding tissues, peripheral growth and subjective sensations, benign course (often the rash disappears spontaneously without scarring and atrophy), high contagiousness of the elements of the rash.
Rice. 2. Manifestations of secondary syphilis - syphilitic seizure.
How is it transmitted?
Syphilis is caused by Treponema pallidum, which lives in the external environment for only 3 minutes. Therefore, the main route of transmission of the disease is sexual. Infection of the fetus is possible in utero (vertical route) or intrapartum, when the child passes through the mother’s birth canal.
The household route of transmission is uncommon; infection is possible from persons with the tertiary stage of syphilis, when treponema pallidum gets on dishes, linen, towels, etc. from decaying gums. Hematogenous transmission of syphilis through blood transfusion cannot be ruled out.
Cases of infection of medical workers through contact with the blood of a patient are not that rare. It is possible to become infected through “bloody” objects: a shared toothbrush, razor, manicure set, etc.
Syphilitic roseola
Syphilitic roseola of the skin
Syphilitic roseola (spotted syphilide) is the most common form of damage to the mucous membranes and skin in early secondary syphilis. It accounts for up to 80% of all rashes. Syphilitic roseola is spots from 3 to 12 mm in diameter, from pink to dark red in color, oval or round in shape, do not rise above the surrounding tissues, there is no perifocal growth and peeling, the spots disappear with pressure, there is no pain and itching.
Roseola is caused by vascular disorders. In the dilated vessels, over time, the breakdown of red blood cells occurs with the subsequent formation of hemosiderin, which causes the yellowish-brown color of old spots. Roseolas that rise above the skin level often peel off.
The main locations for roseola are the trunk, chest, limbs, abdomen (often the palms and soles) and sometimes the forehead. Roseola are often located on the mucous membrane of the oral cavity, rarely on the genitals, where they are hardly noticeable.
Elevated, papular, exudative, follicular, confluent - the main forms of spotted syphilide. With relapses of the disease, the rash is more sparse, less colored, and tends to group with the formation of arcs and rings.
Spotted syphilide should be distinguished from pubic lice bites, pityriasis versicolor and pityriasis versicolor, infectious roseola, measles, rubella and tartaric skin.
Rice. 2. Rash due to secondary syphilis - syphilitic roseola.
Rice. 3. Signs of secondary syphilis - syphilitic roseola on the skin of the body.
Syphilitic roseola of the mucous membranes
Syphilitic roseola in the oral cavity is located isolated, sometimes the spots merge, forming continuous areas of hyperemia in the tonsils (syphilitic tonsillitis) or soft palate. The spots are red, often with a bluish tint, sharply demarcated from the surrounding tissue. The general condition of the patient rarely suffers.
When localized on the mucous membrane of the nasal passages, dryness is noted, and crusts sometimes appear on the surface. On the genitals, syphilitic roseola is rare and always inconspicuous.
Rice. 4. Syphilitic roseola in the oral cavity - erythematous sore throat.
Syphilitic roseola is a typical manifestation of early secondary syphilis.
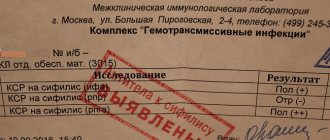
Diagnostics
Syphilis is diagnosed by examination, characteristic signs and laboratory tests:
- Examination by a dermatovenerologist. He asks the patient in detail about the course of the disease, examines the skin, genitals, and lymph nodes.
- Detection of treponema or its DNA in the contents of gummas, chancre, syphilides using dark-field microscopy, direct immunofluorescence reaction, and PCR.
- Instrumental studies: search for gummas using ultrasound, MRI, CT, X-rays, etc.
- Carrying out various serological tests: Non-treponemal - search for antibodies against treponema membrane lipids and phospholipids of tissues destroyed by the pathogen (Wassermann reaction, VDRL, rapid plasma reagin test). The result obtained may be false positive, i.e. show syphilis where there is none. Treponema - search for antibodies to Treponema pallidum (RIF, RPHA, ELISA, immunoblotting, RIBT).
Remember that for such a serious disease you cannot diagnose yourself “on the Internet” by reading about syphilis and its symptoms. The fact is that the rash and other changes can visually copy those of completely different diseases, so that even doctors are periodically misled.
Papular syphilide
Papular syphilide is a dermal papule that is formed as a result of an accumulation of cells (cellular infiltrate) located under the epidermis in the upper dermis. The elements of the rash have a round shape, are always clearly demarcated from the surrounding tissues, and have a dense consistency. Their main locations are the trunk, limbs, face, scalp, palms and soles, oral mucosa and genitals.
- The surface of the papules is smooth, shiny, and smooth.
- The color is pale pink, copper or bluish red.
- The shape of the papules is hemispherical, sometimes pointed.
- They are located in isolation. Papules located in skin folds tend to grow peripherally and often merge. Vegetation and hypertrophy of papules leads to the formation of condylomas lata.
- With peripheral growth, the resorption of papules begins from the center, resulting in the formation of various figures.
- Papules located in the folds of the skin sometimes erode and ulcerate.
- Depending on the size, miliary, lenticular and coin-shaped papules are distinguished.
Papular syphilides are extremely contagious, as they contain a huge number of pathogens. Particularly contagious are patients whose papules are located in the mouth, perineum and genitals. Handshakes, kisses and close contact can cause transmission of infection.
Papular syphilides resolve within 1 to 3 months. When the papules dissolve, peeling is observed. Initially, it appears in the center, then, like a “Biette collar,” on the periphery. In place of the papules, a pigmented brown spot remains.
Papular syphilide is more typical for recurrent secondary syphilis.
Rice. 5. Rash due to secondary syphilis - papular syphilide.
Miliary papular syphilide
Miliary papular syphilide is characterized by the appearance of small dermal papules - 1 - 2 mm in diameter. Such papules are located at the mouths of the follicles; they are round or cone-shaped, dense, covered with scales, sometimes with horny spines. The trunk and limbs are their main places of localization. Resolution of papules occurs slowly. A scar remains in their place.
Miliary papular syphilide should be distinguished from lichen scrofulous and trichophytosis.
Miliary syphilide is a rare manifestation of secondary syphilis.
Lenticular papular syphilide
Lenticular papules form in the 2nd to 3rd year of the disease. This is the most common type of papular syphilis, occurring in both early and late secondary syphilis.
The size of the papules is 0.3 - 0.5 cm in diameter, they are smooth and shiny, round in shape with a truncated apex, have clear contours, pink-red color, and are painful when pressed with a button probe. As the papules develop, they become yellowish-brown in color, flatten, and become covered with transparent scales. A marginal appearance of peeling (“Biette’s collar”) is characteristic.
During early syphilis, lenticular papules can appear on different parts of the body, but most often they appear on the face, palms and soles. During the period of recurrent syphilis, the number of papules is smaller, they tend to group, and bizarre patterns are formed - garlands, rings and arcs.
Lenticular papular syphilide should be distinguished from guttate parapsoriasis, lichen planus, vulgar psoriasis, and papulonecrotic tuberculosis of the skin.
On the palms and soles, papules are reddish in color with a pronounced cyanotic tint, without clear boundaries. Over time, the papules acquire a yellowish color and begin to peel off. A marginal appearance of peeling (“Biette’s collar”) is characteristic.
Sometimes the papules take on the appearance of calluses (horny papules).
Palmar and plantar syphilides should be distinguished from eczema, athlete's foot and psoriasis.
Lenticular papular syphilide occurs in both early and late secondary syphilis.
Rice. 6. Lenticular papules in secondary syphilis.
Rice. 7. Palmar syphilide with secondary syphilis.
Rice. 8. Plantar syphilide with secondary syphilis
Rice. 9. Secondary syphilis. Papules on the scalp.
Coin-shaped papular syphilide
Coin-shaped papules appear in patients during the period of recurrent syphilis, in small quantities, bluish-red in color, have a hemispherical shape, measuring 2 - 2.5 cm in diameter, but can be larger. When resorption occurs, pigmentation or an atrophic scar remains in place of the papules. Sometimes there are many small ones around the coin-shaped papule (bursant syphilide). Sometimes the papule is located inside a ring-shaped infiltrate; between it and the infiltrate there remains a strip of normal skin (a type of cockade). When coin-shaped papules coalesce, plaque syphilide is formed.
Rice. 10. A sign of syphilis of the secondary period is psoriasiform syphilide (photo on the left) and nummular (coin-shaped) syphilide (photo on the right).
Wide type of papular syphilide
The broad type of papular syphilide is characterized by the appearance of large papules. Their size sometimes reaches 6 cm. They are sharply demarcated from healthy areas of the skin, covered with a thick stratum corneum, and dotted with cracks. They are a sign of recurrent syphilis.
Seborrheic papular syphilide
Seborrheic papular syphilide often appears in places with increased sebum secretion - on the forehead (“the crown of Venus”). On the surface of the papules there are fatty scales.
Rice. 11. Seborrheic papules on the forehead.
Weeping papular syphilide
Weeping syphilide appears in areas of the skin where there is increased humidity and sweating - the anus, interdigital spaces, genitals, large folds of skin. Papules in these places undergo maceration, become wet, and acquire a whitish color. They are the most contagious form among all secondary syphilides.
Weeping syphilide must be distinguished from folliculitis, contagious molluscum, hemorrhoids, chancroid, pemphigus and epidermophytosis.
Rice. 12. Secondary syphilis. Weeping and erosive papules, condylomas lata.
Erosive and ulcerative papules
Erosive papules develop in the event of prolonged irritation of their localization sites. When a secondary infection occurs, ulcerative papules are formed. The perineum and anal area are common places for their localization.
Condylomas lata
Papules that are subject to constant friction and weeping (anal area, perineum, genitals, inguinal, less often axillary folds) sometimes hypertrophy (increase in size), vegetate (grow) and turn into condylomas lata. Vaginal discharge contributes to the appearance of condylomas.
Rice. 13. When papules grow, condylomas lata are formed.
Third stage of the disease
Nowadays, stage three syphilis is not often encountered. This is very good news not only for doctors, but also for the patients themselves. Due to the fact that the infection is diagnosed in time, doctors prescribe the optimal treatment, which allows stopping the disease in the initial stages. If the disease is not treated, it may not make itself felt for the first couple of years, slowly affecting the body from the inside.
In no more than five years, syphilis will slowly but surely enter its third stage. During this period, internal organs and the endocrine system are seriously damaged. The disease greatly affects the senses. Even at this stage, the patients' bodies are covered with small tubercles called syphilides. When they are opened, pus is released. Sometimes syphilides appear only on the body, but with advanced disease they can form on internal organs, which in turn is fatal.
Cartilage and other soft tissues will undergo severe deformation. They can degenerate into tumors, which are called gummas.
Syphilis is not only a serious, but also a very dangerous disease. The danger lies in the fact that for many years it may not manifest itself, proceeding exclusively in a latent form. Sometimes external signs appear only at the third stage. To protect yourself from troubles and identify the infection at the earliest stages, you need to undergo a routine examination with a doctor.
Vesicular syphilide
Vesicular syphilide occurs in severe syphilis. The main places of localization of syphilides are the skin of the extremities and torso. On the surface of the formed plaque, which is red in color, many grouped small vesicles (bubbles) with transparent contents appear. The vesicles quickly burst. In their place, small erosions appear, and when they dry, crusts form on the surface of the rash. When cured, a pigment spot with many small scars remains at the site of the lesion.
The rashes are resistant to therapy. With subsequent relapses they appear again. Vesicular syphilide should be distinguished from toxicerma, simple and acute herpes.
Prevention
Disease prevention measures:
- Due to the fact that the main route of transmission of syphilis is sexual, the most important aspect of prevention is avoiding sexual contact with infected people.
- There is also preventive treatment that is given to pregnant women who have previously had syphilis; newborns whose mothers have not received a full course of treatment for syphilis.
- Also, special therapy is prescribed for people who have had sexual or personal contact with an infected person, if no more than 60 days have passed since the contact.
Pustular syphilide
Pustular syphilide, like vesicular syphilide, is rare, usually in weakened patients with low immunity and has a malignant course. When the disease occurs, the general condition of the patient suffers. Symptoms such as fever, headache, severe weakness, joint and muscle pain appear. Often, classical tests for syphilis give negative results.
Acne, smallpox, impetiginous, syphilitic ecthyma and rupiah are the main types of pustular syphilide. Rashes of this type are similar to dermatoses. Their distinctive feature is a copper-red infiltrate located along the periphery in the form of a roller. The occurrence of pustular syphilide is promoted by diseases such as alcoholism, toxic and drug addiction, tuberculosis, malaria, hypovitaminosis, and trauma.
Acne-like (acneiform) syphilide
The rashes are small pustules of a rounded conical shape with a dense base, located at the mouths of the follicles. After drying, a crust forms on the surface of the pustules, which falls off after a few days. A depressed scar remains in its place. The scalp, neck, forehead, and upper half of the body are the main locations for acne syphilide. Elements of the rash appear in large numbers during the period of early secondary syphilis, and scanty rashes appear during the period of recurrent syphilis. The general condition of the patient suffers little.
Acne syphilide should be distinguished from acne and papulonecrotic tuberculosis.
Rice. 14. Rash due to syphilis - acne syphilide.
Smallpox syphilide
Smallpox syphilide usually occurs in weakened patients. Pea-sized pustules are located on a dense base, surrounded by a copper-red ridge. When the pustule dries out it becomes like a smallpox element. In place of the fallen crust, brown pigmentation or an atrophic scar remains. The rashes are not abundant. Their number does not exceed 20.
Rice. 15. The photo shows manifestations of secondary syphilis - smallpox syphilide.
Impetiginous syphilide
With impetiginous syphilide, a dark red papule the size of a pea or more appears first. After a few days, the papule festeres and shrinks into a crust. However, the discharge from the pustule continues to be released to the surface and dries out again, forming a new crust. The layering can become large. The formed elements rise above the skin level. When syphilides merge, large plaques are formed. After peeling off the crusts, a juicy red bottom is exposed. Vegetative growths resemble raspberries.
Impetiginous syphilide, located on the scalp, nasolabial fold, beard and pubis, is similar to a fungal infection - deep trichophytosis. In some cases, the ulcers merge, forming large areas of damage (corrosive syphilide).
Healing of syphilide is long. Pigmentation remains at the site of the lesion, which disappears over time.
Impetiginous syphilide should be distinguished from impetiginous pyoderma.
Rice. 16. In the photo, a type of pustular syphilide is impetiginous syphilide.
Syphilitic ecthyma
Syphilitic ecthyma is a severe form of pustular syphilide. Appears 5 months after infection, earlier in weakened patients. Deep pustules are covered with thick crusts up to 3 or more centimeters in diameter; they are thick, dense, and layered. Elements of the rash rise above the surface of the skin. They have a round shape, sometimes irregular oval. After the crusts are rejected, ulcers with dense edges and a bluish rim are exposed. The number of ecthymas is small (no more than five). The main places of localization are the limbs (usually the lower legs). Healing occurs slowly, over 2 or more weeks. Ecthymas can be superficial or deep. Serological tests sometimes give negative results. Syphilitic ecthyma should be distinguished from vulgar ecthyma.
Rice. 17. Secondary syphilis. A type of pustular syphilide is syphilitic ecthyma.
Syphilitic rupee
A type of ecthyma is syphilitic rupee. The rashes range in size from 3 to 5 centimeters in diameter. They are deep ulcers with steep, infiltrated edges, covered with dirty and bloody discharge, which dry to form a cone-shaped crust. The scar heals slowly. It is often located on the shins. It spreads both peripherally and deeply. Combines with other syphilides. It should be distinguished from rupoid pyoderma.
Rice. 18. Rash due to secondary syphilis - syphilitic rupee.
Rice. 19. In the photo, the symptoms of malignant syphilis of the secondary period are deep skin lesions: multiple papules, syphilitic ecthymas and rupees.
Primary signs of the disease
Before you begin treatment for syphilis, it is worth knowing how syphilis manifests itself. So the most important sign of syphilis in a patient manifests itself in the form of a hard, dense chancre and a significant increase in the size of the lymph nodes.
Chankra - Photo of the initial stage
Chancre is an ulcerative neoplasm or a focus of erosion, regular rounded in shape, with clear edges, filled with liquid and most often occurs at the site of contact with the carrier of the disease.
Syphilis also manifests itself with the following additional signs:
- insomnia and increased body temperature in the patient;
- attacks of headache, aches in joints and bones;
- swelling of the genitals and the appearance of such a symptom as a syphilitic rash.
Characteristics of the pathogen: external structure
Treponema pallidum resembles a corkscrew in appearance. It has 8 - 14 equal-sized curls, the height of which decreases at the ends. The spiral shape of the pathogen is preserved in all cases and under all conditions. The length of the microorganism is from 5 to 15 microns, the width is 0.2 microns.
Rice. 4. The photo shows the causative agent of syphilis Treponema pallidum (view under an electron microscope).
"End" formations
The ends of most treponemes are pointed. They contain disc-shaped outgrowths (blepharoplasts) with 10-11 fibrils attached to them.
The fibrils stretch along the body of the treponema and wrap around it, providing the bacteria with a spiral shape. From each end there are 2 independent bundles of fibrils. They are located under the outer wall, passing above the cytoplasmic membrane. Fibrils were also found under the cytoplasmic membrane. They are thinner and more numerous. The fibrils of the external bundle ensure movement of the treponema; they are twice as thick. They are long tubes consisting of flagellin protein, which is quite resistant to the action of a number of enzymes. The fibrils of the inner layer play the role of a framework.
At one end of the bacterium there are two round structures (corpus spongiosum). It ensures active penetration of bacteria into host cells.
Treponema pallidum can perform translational (back and forth), rotational, flexion, wave-like (convulsive) and helical movements.
Rice. 5. The photo shows treponema pallidum (cultured form).
Rice. 6. The photo shows pale treponema with a magnification of 3000 times (dark-field microscopy). This type of research allows you to record the shape and movement of living bacteria.
Manifestations of the disease in both sexes
In men, syphilis most often affects the penis and scrotum - it is on the external genitalia that the disease primarily manifests itself in the form of negative symptoms.
In women , the disease most often affects the labia minora, vagina and mucous membranes. If sexual partners practice oral or anal sex, infection and subsequent damage to the circumference of the anus, oral cavity, mucous membrane of the throat and skin in the chest and neck area occurs.
The course of the disease is long-term, if it is not treated in a timely manner, it is characterized by a wave-like manifestation of negative symptoms, a change in both the active form of the pathology and the latent course.
Internal structure of Treponema pallidum (ultrastructure)
Mucoprotein "case"
The body of the bacterium is surrounded by a mucus-like structureless substance (microcapsule). This mucopolysaccharide substance protects treponemes from phagocytes and antibodies. The capsular substance is produced by the treponema itself.
Cytoplasmic membrane
The cytoplasmic membrane of bacteria performs a number of vital functions: transport, protective, is the site of localization of antigens and enzymes, it takes an active part in cell division, L-transformation and sporulation. The cytoplasmic membrane has a three-layer structure. Its inner layer forms numerous outgrowths in the protoplasmic cylinder, due to which the active transfer of nutrients from the outside occurs. The vital activity of bacteria depends on the state of the cytoplasmic membrane.
Protoplasmic cylinder
The protoplasmic cylinder is located under the outer wall. The structure of the cytoplasm of Treponema pallidum is finely granular. Ribosome granules and many lamellar structures are immersed in the transparent hyaloplasm. Ribosomes provide protein synthesis in the bacterial cell. The cytoplasm also contains a nucleotide that does not have a limiting membrane. It stretches along the entire length of the protoplasmic cylinder.
Mesosomes
Mesosomes are derivatives of the cytoplasmic membrane. They occupy half or the entire axis of the diameter of the treponema. Mesosomes supply energy to the bacterial cell at points of increased growth during sporulation and division. Their function is similar to mitochondria. Mesosomes differ in the nature of their structure, but their number is always very large.
Rice. 7. Ultrastructure of Treponema pallidum. Mucoprotein cover on top, then a three-layer cell wall, inside there is a cytoplasmic membrane and a cylinder with nucleotide, mesosomes, ribosomes and other inclusions. The photo clearly shows the fibrils running along the body of the bacterium.
Damage to the lower leg areas (saber shins)
The pathology typically manifests itself in the child’s infancy.
It accounts for 70% of all pathologies associated with late syphilitic manifestations.
A large proportion of the damage occurs in the periosteum and tibia - osteoperiostitis, osteochondritis (damage to the cartilage itself involving a small area of the bone itself),
Due to the weight of the child, the bones simply bend forward.
The child grows and learns to walk, his legs resemble a saber blade.
The bones become thicker and longer.
At the same time, the child begins to sleep restlessly, as he is bothered by night pain in his legs.
In this case, damage to the bones of the forearm is not observed.
To confirm this diagnosis, an x-ray examination is necessary.
In addition to the saber-shaped manifestation of syphilis, there is a similar symptom with Paget's disease or rickets, when the bones bend outward.
Stability of pathogens in the external environment
- Treponema pallidum is resistant to low temperatures. Can withstand freezing for up to one year. Pathogenic strains of pathogens are stored in an oxygen-free environment at low temperatures (20 - 70 ° C) or dried from a frozen state.
- Treponemas retain their virulence on environmental objects until they dry out. At temperatures up to 42°C, the activity of bacteria first increases, and then they die. When heated to 60°C, treponemes remain active for 15 minutes. For more than 3 days, syphilis pathogens retain their pathogenic properties in cadaveric material.
- Outside the human body, bacteria quickly die. At a temperature of 100°C they die instantly. Treponema pallidum is sensitive to disinfectants and some antibiotics.
Rice. 2. To identify bacteria, an immunofluorescence reaction is used.