Secondary syphilis
The development of secondary syphilis often begins with general symptoms similar to those of acute respiratory viral infection or influenza. This is malaise, fever, chills, headache. A distinctive feature of secondary syphilis is arthralgia and myalgia, which worsen at night. Only a week after the appearance of these prodromal symptoms do skin manifestations of secondary syphilis occur.
Rashes of secondary syphilis - secondary syphilides - are characterized by significant polymorphism. At the same time, they have a number of similar characteristics: a benign course without peripheral growth and destruction of surrounding tissues, a rounded shape and clear demarcation from the surrounding skin, the absence of subjective symptoms (occasionally slight itching is noted) and acute inflammatory signs, healing without scar formation. Secondary syphilides contain a high concentration of pale treponema and cause a high infectious danger for a patient with secondary syphilis.
The most common form of rash associated with secondary syphilis is syphilitic roseola.
or spotted syphilide, manifested by rounded pale pink spots with a diameter of up to 10 mm. They are usually localized on the skin of the limbs and torso, but can be on the face, feet and hands. Roseolas with secondary syphilis appear gradually, 10-12 pieces per day for a week. Typically, roseola disappears when pressure is applied to it. Rarer forms of roseola rash in secondary syphilis include scaly and raised roseola. The first has a small depression in the center and is covered with lamellar scales, the second rises above the general level of the skin, which makes it look like a blister.
The second most common cause of secondary syphilis is papular syphilide.
. Its most typical form is lenticular, having the appearance of densely elastic papules with a diameter of 3-5 mm of pink or copper-red color. Over time, peeling begins in the center of the papules of secondary syphilis, which spreads to the periphery. A “Biette collar” is characteristic - peeling along the edge of the papule while in the center it has already ended. Resolution of papules ends with the formation of long-lasting hyperpigmentation. Rarer forms of papular syphilide include seborrheic, coin-shaped, psoriasiform, weeping syphilide, papular syphilide of the palms and soles, as well as condylomas lata.
A rare form of secondary syphilis rash is pustular syphilide.
. Its appearance is usually observed in weakened patients (tuberculosis patients, drug addicts, alcoholics) and indicates a more severe course of secondary syphilis. Pustular syphilide is characterized by the presence of purulent exudate, which dries to form a yellowish crust. The clinical picture resembles manifestations of pyoderma. Pustular syphilide of secondary syphilis can have the following forms: impetiginous, acne-like, ectymatous, smallpox, rupoid.
With recurrent secondary syphilis, pigmentary syphilide
(syphilitic leukoderma), appearing on the side and back of the neck in the form of rounded whitish spots, called the “necklace of Venus”.
Skin manifestations of secondary syphilis are accompanied by generalized enlargement of the lymph nodes (lymphadenitis). Enlarged cervical, axillary, femoral, and inguinal lymph nodes remain painless and are not fused with the surrounding tissues. Impaired nutrition of the hair roots in secondary syphilis leads to hair loss with the development of diffuse or focal alopecia. Lesions of the mucous membranes of the oral cavity (oral syphilis) and larynx are often observed. The latter cause characteristic hoarseness in patients with secondary syphilis.
On the part of the somatic organs, mainly functional changes are observed, which quickly disappear during treatment and are absent during periods of latent secondary syphilis. Liver damage is manifested by its soreness and enlargement, and impaired liver function tests. Gastritis and gastrointestinal dyskinesia are often observed. From the kidneys, proteinuria and the occurrence of lipoid nephrosis are possible. Damage to the nervous system is manifested by irritability and sleep disturbances. Some patients with secondary syphilis experience syphilitic meningitis, which is easily treatable. Damage to the skeletal system is possible with the development of osteoperiostitis and periostitis, manifested by night pain mainly in the bones of the extremities and occurring without bone deformities. In some cases of secondary syphilis, otitis media, dry pleurisy, retinitis, and neurosyphilis may occur.
Treatment of syphilis
Syphilis is perhaps the most feared disease. It is caused by a bacterial pathogen - a spirochete. Syphilis is transmitted from person to person through sexual contact. The possibility of becoming infected through everyday life - through a handshake, contact with a towel, door handle, etc. – practically equal to zero.
- Story
It is believed that syphilis arrived in Europe from America. It was brought by the sailors of Christopher Columbus, and at the turn of the 15th – 16th centuries the first pandemic of this disease broke out in Europe; you can read more about it in this historical essay
. Today, when personal protective equipment is available to everyone, and everyone knows about the dangers of STDs, syphilis still affects 3-4 people out of 1000 people.
- First stage
Approximately 3-4 weeks after unprotected sexual intercourse, a man develops an ulcer on his penis. It's called chancre - if you touch it, it's hard at the base. Sometimes it looks like a pimple, sometimes like a sore with a crater. It is painless and does not bother you. Usually a person thinks that it is a rub, or a bite, or an allergy. Classically, sexual contact is considered vaginal. But besides it, there can be anal contact and oral. With oral infection, a chancre forms on the lip or palate. Patients often confuse chancre in the anus with an acute form of hemorrhoids and do not always realize to get tested. Following the appearance of chancre, the lymph nodes enlarge, but the person may not feel this. If the patient discovers a chancre and consults a doctor, syphilis can be cured at the first stage.
- Second stage
After some time, the chancre goes away on its own, and the lymph nodes become smaller. But after about six months - and given the widespread use of antibiotics, it can take a year or a year and a half - a person develops nonspecific skin rashes. Even doctors can sometimes mistake them for an allergic reaction, and by that time the patient had already forgotten about that ulcer (chancre), which did not bother him at all. Papules appear on the palms - red nodules. Leucoderma appears around the neck - what was previously called the “necklace of Venus”. Today, there are many erased forms of secondary syphilis; instead of the classic “necklace of Venus”, 2-3 incomprehensible spots appear, which even a doctor cannot always identify. If the diagnosis has not been made, syphilis develops further.
- Third stage
Tertiary syphilis is characterized by gummous changes in tissues. Gumma (syphilitic granuloma) is a tissue node in which spirochetes are concentrated. Most often, gummas occur in the liver, soft tissues, and in the wall of the aorta. The tissues are irreversibly destroyed and rough knots are formed. If the spirochete enters the trunks of the nervous system, an extremely dangerous condition develops - neurophysilis. However, tabes dorsalis (a form of late neurosyphilis characterized by damage to the central nervous system) now practically does not occur. The artist Mikhail Vrubel suffered from tabes dorsalis - this is where his demons came from. more about the tragedy of Vrubel and his doctors in this article.
- Condylomas lata
Lata condylomas should not be confused with genital warts, which occur with the human papillomavirus. Previously, broad-pointed condylomas occurred at stages 2 and 3 of syphilis. But now, either due to the widespread use of antibiotics, or for some other reasons, condylomas can occur in the first stage. Due to the difference in the anatomy of the genital organs, men find condylomas more easily than women. If you see or feel that a condyloma has appeared on the genitals, do not try to determine on the Internet whether it is wide-ended or not, go to the doctor immediately.
- Test for syphilis
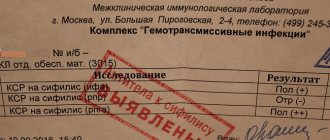
3 weeks after casual unprotected sexual intercourse (including oral and anal intercourse), it is necessary to take a specific RW test (Wassermann reaction, or simply “syphilis test”). There is no point in getting tested earlier, since the body’s immune response has not yet developed, and the test may give a false negative answer. A test for syphilis can be taken in any private laboratory, but it is best to go to a dispensary at your place of residence.
It is important to understand that if syphilis infection has occurred, the RW test will always be positive. In only 1 out of 10 patients, the syphilis marker disappears after treatment. The presence of a marker (positive RW analysis) may raise unnecessary questions during hospitalization, obstetrics, and professional examinations at work. Therefore, a sick person needs to undergo only legal treatment in a government medical institution licensed to treat syphilis. Such an institution will issue the patient a certificate stating that there was syphilis, the patient completed a course of treatment, was registered and deregistered, and is healthy. No private clinic has the right to treat syphilis and issue such certificates! A private clinic can only make a diagnosis and refer the patient to a public medical institution.
- Treatment of syphilis
Today, all over the world, syphilis is easily treated with long-acting penicillin antibiotics, which until recently were available in Russia. Treatment of syphilis with long-acting antibiotics is only 4 injections of extencillin. But now this drug is not available in Russia, and bicillin or penicillin is used in the treatment of syphilis - 6 injections daily for 10 days, the treatment is complex. The task of the state is to make the patient not infectious to society. Everywhere in the world, when syphilis is detected, the patient is given the first injection of the long-acting antibiotic extencillin - after which he is no longer contagious. Treatment with bicillin or penicillin does not give such a quick effect and the person continues to pose a danger to sexual partners until the end of the course of treatment with bicillin. If you are allergic to penicillin, treatment with second-line drugs, such as tetracyclines, is possible.
- What to do if accidental unprotected sexual intercourse occurs
Specific antibodies to syphilis and HIV appear in the blood 3 to 4 weeks after infection. But you should consult a doctor 1 week after suspicious sexual contact. You should not take any medications before consulting a doctor. The doctor will prescribe a special laboratory test called immunoblot. This is a highly specific and highly sensitive method that allows you to detect traces of developing antibodies to the causative agent of syphilis.
For patients who have had syphilis in the past, it is important to understand the difference between a total test for immunoglobulins M and G and their determination in the blood separately. Their total analysis will always be positive, because immunoglobulin G remains in the blood of those who have previously had syphilis. Only immunoglobulin M indicates a new infection. This is a rather complex question; you should not solve it yourself using the Internet.
After suspicious unprotected sexual intercourse, a blood test is required for syphilis, an HIV test (this is also taken no earlier than 3-4 weeks after contact) and hepatitis C, which is easily transmitted through sexual contact. At the same time, a scraping is taken from the urethra or from the vagina and cervix for markers of diseases that are predominantly sexually transmitted. Their pathogens include gonococcus, trichomonas, ureaplasma, metaplasma, chlamydia, candida, gardnerella. The only correct approach to suspicious unprotected sexual intercourse is to take the entire set of tests.
- How to protect yourself from sexually transmitted diseases
A good condom guarantees protection against STDs, provided that it is put on correctly, that it does not burst, and that extragenital contacts - oral and anal - were also carried out in a condom. Today, there is no better protection against STDs than a condom. Treating the genitals with drugs like Miramistin is not effective!
What is clinical relapse of syphilis?
Relapse is usually called the return of the disease after treatment.
But there is also the concept of clinical relapse.
This is the return of symptoms in a patient who has not received treatment.
The secondary and tertiary periods sometimes proceed in waves.
They distinguish two clinical periods, alternately replacing each other:
- latent phase
- clinical relapse
During the latent phase there are no symptoms.
They appear in the relapse phase.
These may be rashes, central nervous system lesions, etc., depending on the stage of the disease.
Incorrect treatment as a cause of relapse of syphilis
Relapse occurs often after treatment.
It can occur both through the fault of the doctor and the patient.
If a non-specialized specialist takes on the treatment of a syphilitic infection, he may prescribe the wrong treatment regimen.
Only a venereologist or syphilidologist should do this.
The following treatment features reduce the risk of relapse:
- therapy takes place in a hospital
- Intermediate or short-acting penicillins are used
- the doses are sufficient
- the course duration is sufficient
- there may be several courses
- there may be more than one antibiotic
Errors that can lead to incomplete destruction of bacteria and subsequent relapse:
1. Treatment of late stages of syphilis at home.
Patients should be hospitalized in a hospital.
In extreme cases, this could be a day hospital, where the patient comes daily to receive injections and the necessary medical procedures.
Drugs for the treatment of syphilis are used in injections.
Patients at home without medical supervision can:
- do not give injections;
- buy an alternative drug in tablets and not tell the doctor about it;
- giving injections incorrectly;
- do not administer the entire dose;
- forgetting to give an injection from time to time;
- not being treated completely, etc.
Outpatient 100% control of treatment is not provided.
While in a hospital, the doctor can be sure that the patient has received the full dose of the required antibiotic.
2. Use of one antibiotic.
This is acceptable in the initial stages of syphilis.
But in “experienced” patients, 2 drugs with different mechanisms of action are often used.
The first drug is one of the forms of benzylpenicillin, which the doctor considers appropriate in this particular clinical case.
The second is an antibiotic of a different group, for example, a macrolide or tetracycline.
An important condition: it must have a different mechanism of action, different from penicillin drugs.
Why is this necessary?
We have already said that bacteria are able to “hide” from drugs by turning into L-forms.
These forms lack a cell wall completely or partially.
Penicillins act by affecting the cell wall.
If it is not present, the bacterium is immune to this drug.
It would seem, why then use penicillin at all?
Because only some pale spirochetes change into the L-form.
Most of them are in their usual spiral state.
They die under the influence of penicillin.
While another antibiotic, which inhibits protein synthesis, “finishes off” the remaining L-forms so that they do not cause a relapse in the future.
3. Use of short- or medium-acting drugs.
It is always better for the patient if he:
- visits the doctor less often;
- gives injections less often;
- spends less time on treatment.
Therefore, convenient forms of penicillin have been developed that accumulate in the body and are then gradually released.
They act on the causative agent of syphilis with a gradually weakening effect over 2 weeks or more.
Injections of such drugs are given once a week, which is very convenient for the patient.
But such drugs are less effective.
Therefore, they can only be used in the initial stages of syphilis.
The order of the Ministry of Health provides for the possibility of using durable penicillins not only in the primary, but also in the secondary period.
But many doctors don't want to take risks.
From the secondary period, they refuse such drugs, giving preference to penicillins, used once or several times a day.
This therapy is less well tolerated by the patient and requires hospitalization or frequent visits to the clinic.
But the likelihood of successful treatment is higher, and the risk of relapse is lower.
4. Insufficient control of cure.
You cannot treat a patient and send him home.
He is always being watched.
And for quite a long time - at least 3 months, if treatment is prescribed literally immediately after infection or the appearance of the first symptoms.
The observation period can reach 3 years or more if there were severe forms of syphilis.
Some patients receive additional treatment during this time.
If there is no proper control, then relapses occur very often.
Special forms of bacteria that cause syphilis
In the human body, the causative agent of syphilis exists in different morphological forms.
Not all of them are amenable to the action of antibiotics and antibodies.
In the infectious stage, the bacterium is in a spiral shape.
It is transmitted from person to person, but quickly dies under the influence of antibacterial therapy.
Less contagious and at the same time less vulnerable forms:
- cysts
- L-shape
They appear in the later stages of the disease.
It is for this reason that early syphilis is easier to treat than late syphilis.
These forms are the main way the infection persists in unfavorable conditions.
Cysts are distinguished by the presence of a protective shell.
They have:
- several layers of membrane coating
- capsule-shaped mucopolysaccharide substance
The cyst has antigenic properties.
Therefore, positive serological reactions are preserved if they are present in the body.
An increase in encysted forms of pale spirochetes occurs over time.
The longer a person suffers from syphilis, the more cysts there are in his body.
Their presence is explained by:
- seroresistance
- long-term asymptomatic course of syphilitic infection, which can result in damage to internal organs and the nervous system after a few years
- relapse of the disease after therapy
The L-form is characterized by the loss of the cell wall.
Since it is the target for the action of antibiotics and immunoglobulins, this form is more resistant to treatment.
Metabolism in the bacterial cell is reduced.
It retains its spiral shape.
Has a high reproductive capacity.
At the same time, it retains the ability to convert back into the pathogenic form of the pale spirochete.
Unlike cysts, the L-form has no antigenic properties.
Since most antigens are located precisely on the cell wall of bacteria.
If patients have only L-forms of spirochetes left in their bodies, tests for syphilis will be negative.
Penicillin has no effect on these forms of bacteria.
But some other antibiotics that don't target the cell wall still work.
Therefore, late syphilis is often treated not with one, but with two antibacterial drugs with different mechanisms of action.
This reduces the risk of relapse.
In the presence of L-forms, the immobilization reaction of Treponema pallidum and RIF remains positive.
They do not grow on nutrient media.
Malignant syphilis
If a syphilitic infection returns after therapy, it may develop a malignant form.
The cause can be either relapse or reinfection (re-infection).
The resulting hard chancre is prone to necrosis and peripheral growth.
The initial period in case of infection lasts only 3-4 weeks, and then a rash appears on the body.
In addition to spots, rupee, ecthyma, and impetigo (pustular syphilide) appear.
The eruptions become ulcerated.
Serological tests may be negative.
But they become positive after the start of penicillin therapy.
General symptoms of relapse of syphilis appear if it occurs in a malignant form:
- fever
- weakness
- intoxication
The disease does not go into a latent state for months.
If this happens, remissions are very short.
Clinical relapses follow one after another.
Patient mistakes as a cause of relapse of syphilis
The patient's mistakes begin only after the doctor makes a mistake.
Namely, he will send a patient with syphilis home for treatment.
At home, a person can make many mistakes.
Basically they are the following:
- replacing an expensive drug with a cheap one because the pharmacy said it was “the same thing”
- refusal to use antibiotics due to personal belief that all diseases, including syphilis, can be treated with pickles, pine cones or propolis
- skipping injections due to lack of discipline
- use of incorrect doses (the name of the drug is the same as prescribed by the doctor, but the dose at the pharmacy was given differently)
- incorrect frequency of drug use (either I forgot how to inject, or did not consider it necessary to follow the doctor’s instructions in full)
- not all medications are purchased and used (the patient considers some medications important, but for some reason does not take others)
The most common mistake a patient makes is that he is not treated completely.
He tells the doctor that he continues to inject antibiotics.
But he refuses them because:
- symptoms have passed;
- the person considers himself healthy;
- fears the harm of antibiotics to health;
- the injections are painful, and there is no longer a living place on the “soft spot”;
- does not want to spend any more money on treatment.
All these factors combine.
Of course, if a person considers himself sick, he is ready to spend money on treatment and endure painful injections.
But if he believes that he has already been cured, and the doctor prescribes further injections just to be on the safe side, he can stop using the drugs.
Not in 100% of cases, but sometimes this results in relapses.
They can happen even several years after the end of therapy.
And all because the person was lazy or did not consider it necessary to complete the course, as a result of which a “handful” of bacteria remained in his body.
Causes of relapse of syphilis
Syphilis can be fresh or recurrent.
Recurrent can be treated or untreated.
If a person has manifested secondary syphilis, after a few months the symptoms disappeared, but after a certain time they appeared again - this is a relapse.
If the patient underwent treatment, normalization of serological parameters was observed, but then tests again showed an increase in antibody titer - this is also a relapse, but serological.
It can be difficult to distinguish from reinfection.
That is, from re-infection with a syphilitic infection.
For differential diagnosis, several different antibody tests are performed.
In particular, the determination of immunoglobulins M is informative.
Causes of relapse of syphilitic infection:
- weak immunity, HIV
- inadequate treatment
- long-term syphilis
- transition of the pale spirochete into special forms