Iron deficiency anemia in children is one of the types of anemia, which is characterized by iron deficiency, leading to impaired hemoglobin synthesis. On average, about 80% of cases of anemia in children are due to iron deficiency. The pathology is quite common: its incidence rate is about 40% among young children.
Treatment of iron deficiency anemia in children can be done at the CELT multidisciplinary clinic. We employ highly qualified specialists who will accurately diagnose and prescribe appropriate treatment. Symptoms and treatment of anemia in children will be discussed in this article. Don't forget: the sooner you seek professional medical help, the more effective the treatment will be.
What is iron deficiency anemia in a child?
Pediatricians around the world deal with this disease every day.
This group of diseases includes those associated with a decrease in the content of hemoglobin and/or red blood cells per unit volume of blood, which negatively affects the oxygen supply to the body’s tissues. Iron deficiency anemia is the most common of all anemias, accounting for 80% of all cases. In our country and Europe, the prevalence of iron deficiency anemia in young children is approximately 50%, and in older children - 20% or more.
Iron deficiency anemia in a child is a syndrome characterized by a lack of iron in the body. It develops against the background of pathological processes and is manifested by signs of anemia and sideropenia.
Iron is one of the main microelements in the body of both children and adults. The body has hemoproteins, which contain about 70% of the total amount of iron, which is associated with porphyrin. Iron is contained in hemoglobin, myoglobin, peroxidases, cytochromes, catalases, etc.
This element is stored in the body in the form of ferritin (the majority) and hemosiderin. In babies, most of the iron is stored in erythroid cells and very little in the muscles.
Iron deficiency conditions are very widespread. 3.6 billion people on Earth have signs of latent iron deficiency, and another 1.8 billion suffer from iron deficiency anemia. Maternal mortality in the world associated with anemia is 500 thousand cases per year. Iron deficiency conditions are responsible for approximately 1/5 of perinatal deaths and 1/10 of maternal deaths.
Important medical problem
Iron deficiency conditions (IDC) include iron deficiency anemia (IDA) and latent iron deficiency (LDI).
IDA, according to experts from the authoritative scientific organization Micronutrient Initiative (USA):
► leads to a decrease in mental development in almost 40% of growing infants;
► leads to health problems and decreased performance in approximately 500 million women;
► responsible for more than 60 thousand newborn deaths in the world every year.
Experts believe that properly organized prevention allows:
► prevent 4 out of 10 child deaths;
► reduce maternal mortality by 1/3;
► increase efficiency by 40%;
► increase intelligence quotient (IQ) by 10–15 points;
► increase the country's gross national product by 5%.
They also talk about replenishing iron deficiency (ID) as the most important medical problem in the world.
The average adult human body contains about 3–5 g of iron. Risk groups for ID include women, especially pregnant and lactating women, young children and teenage girls.
From mother to child
IDA is associated with lower weight and height of the child, delayed sexual development, immune system disorders and, therefore, can lead to an increase in the incidence of acute respiratory diseases, otitis media, intestinal infections, and protracted and complicated bacterial infections.
According to the literature, the prevalence of IDA in pregnant women ranges from 21% to 80% of cases, judging by the level of hemoglobin, and from 49% to 99%, if we take into account such signs of iron deficiency as a decrease in serum ferritin and iron in the blood serum, hypochromia of erythrocytes and microcytosis. In the third trimester, IDA of varying severity is found in almost 90% of patients (LDD in all), which suggests a high incidence of anemia in the postpartum period.
ID has an adverse effect on the course of pregnancy and childbirth, the postpartum period, and the condition of the fetus and newborn. It has been proven that the most common complications of IDA during pregnancy are:
- premature birth - in 20–42%;
- preeclampsia - 40%;
- placental insufficiency - in 25%;
- bleeding in the postpartum period - in 47%;
- purulent-septic complications - in 12% of cases.
An examination of newborns from mothers with IDA revealed the presence of ID in 48% of cases, and during further observation these children had delays in psycho-emotional and mental development, frequent acute respiratory infections and allergic diseases. In the postpartum period, many, even after acceptable blood loss during vaginal delivery, and even more so during surgical delivery, have a significantly reduced iron supply.
In patients who had ID before childbirth, the condition worsens, which can negatively affect overall well-being and contribute to the development of other complications, including purulent-inflammatory processes, venous thrombosis and thromboembolism, hypogalactia, and a decrease in the reparative capabilities of tissues. It has been established that postpartum women with ID have decreased cognitive abilities and physical activity, including mental disorders, which worsens the quality of life and the ability to care for the child.
It is known that the required daily dose of 18 mg of iron for non-pregnant women is in very rare cases covered only by nutrition. Therefore, almost half of women have very small iron reserves at the beginning of pregnancy. According to the latest data, its deficiency at the end of pregnancy develops in all women without exception in a latent or overt form.
Pregnancy is accompanied by additional loss of iron: 320–500 mg is spent on an increase in hemoglobin and increased cellular metabolism, 100 mg on the construction of the placenta, 50 mg on an increase in the size of the uterus, 400–500 mg on the needs of the fetus, 100–500 mg on blood loss during childbirth, 200–300 mg for breastfeeding. The iron balance during this period is on the verge of deficiency and requires correction.
It has been established that in pregnant women in the third trimester, when the hemoglobin level is closer to the lower limit of normal, hypochromia and microcytosis are detected, and the content of serum ferritin and hematocrit decreases, that is, clear signs of ID are revealed. Under these conditions, even taking into account that the growing fetus takes iron from its mother against the concentration gradient (literally “sucks it out”), it cannot receive it in sufficient quantities due to deficiency. In this case, there is no risk of manifestations of hemochromatosis in a pregnant woman against the background of corrective ferrotherapy, since during this period the woman gives the fetus from 1/3 to 1/2 of her iron pool with all the ensuing consequences for her. And it is necessary to help her make up for these losses both during pregnancy and during lactation.
The consequences of ID for the development of the fetus and after the birth of the child are also known, and they must be prevented with the help of ferroprophylaxis for pregnant and lactating women.
It has been proven that the growing fetus is especially sensitive to ID. There are disturbances in the growth of brain mass and the process of myelination, the conduction of nerve impulses through synapses. These changes are irreversible and cannot be corrected with iron supplements prescribed after the birth of the child. Subsequently, the child may experience delayed mental and motor development and impaired cognitive functions.
Thus, life cycle in a growing fetus and newborn depends on the timely fulfillment of the needs of a pregnant woman and then a nursing mother. Naturally, an interested party in the prevention of VDD during pregnancy is not only an obstetrician-gynecologist, but also a pediatrician due to the known consequences of VDD in the fetus and young child.
In 2018–2019, we surveyed a large group of children to determine the prevalence of IDA and LVID. It was found that there is a fairly high percentage of IDA and LID in young children, namely 1–2 years of age. And we associate this with the shortcomings of prevention.
What is ID prevention?
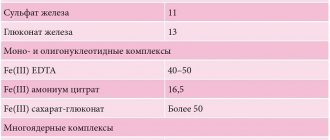
In a number of countries, government measures are being taken to fortify the most commonly consumed food products, for example, flour for baking bread, with iron compounds (USA, Canada, Western Europe, some CIS and Asian countries). Medical preventive measures (WHO expert recommendations) include the need for women to take iron supplements throughout the second half of pregnancy at a dose of 50–60 mg of elemental iron per day.
Obstetricians and gynecologists of Belarus mainly carry out the prevention of IDA in pregnant women depending on the level of hemoglobin in the blood, guided by the recommendations of WHO experts and the developments of the head of the Department of Clinical Hematology and Transfusiology of BelMAPO, Professor Lyudmila Smirnova, presented in the instructions of the Ministry of Health “Comprehensive prevention of iron deficiency anemia in children” (2011 ). However, for the group of patients whose hemoglobin does not decrease during pregnancy, some obstetricians and gynecologists do not prescribe iron supplements. The fallacy of this tactic is obvious.
It has been established that 60% of iron in the body is in the form of iron hemoglobin and myoglobin, 20% in the form of ferritin and hemosiderin (reserve iron) and another 20% in enzymes (dehydrogenase, catalase, peroxidase, cytochrome, etc.). With a negative iron balance that occurs during pregnancy, as is known, the reserve fund is first consumed - ferritin and hemosiderin, then the iron of enzyme systems and only after that the iron of hemoglobin. Therefore, in a pregnant woman in the 2nd and, of course, the 3rd trimester, even if the level of hemoglobin in the blood is at a minimum level from the norm, iron deficiency is already present in the body, and the woman cannot supply the growing fetus with a sufficient amount of iron.
In 2018–2019, we analyzed the state of affairs with the prevention of IDA by interviewing over 300 mothers of sick young children treated at the 3rd State Children's Clinical Hospital and the Minsk State Children's Clinical Hospital. It turned out that during the lactation period ferroprophylaxis is not prescribed at all (99%) to nursing mothers, as well as to young children, which is recommended in the previously mentioned instructions, complies with the recommendations of WHO experts and is even included in textbooks. At the same time, ferrotherapy for a nursing mother is necessary, on the one hand, to restore a significant amount of iron given to the fetus during pregnancy, on the other hand, to restore after blood loss during childbirth, as well as to maintain normal iron content in breast milk.
According to modern approaches, nursing mothers are recommended to take iron supplements during the entire period of lactation in a daily dose of 50–60 mg of elemental iron per day or vitamin-mineral complexes with a similar iron content.
Who is most appropriate to implement this preventive measure in our republic? In our opinion, first of all, this can be done by a local pediatrician by providing patronage to a newborn. It is he who will justify this as an event to compensate for the loss of iron during pregnancy and childbirth, as well as to improve the quality of breast milk and provide the growing child with iron, and reduce morbidity.
It is well known that after 4–5 months of life, a full-term breastfed baby completely uses up the iron supply obtained during pregnancy, therefore a widespread recommendation: from 4 months, prescribe iron supplements at a dose of 1 mg/kg per day until 1 year or until introducing complementary foods fortified with iron.
For premature infants, taking into account the degree of prematurity, from 1–2 months it is recommended to prescribe iron supplements at a dose of 2 mg/kg per day for at least 1 year. Children from multiple pregnancies and with the presence of other risk factors (low socio-economic status of the family; acute blood loss in the ante- and intrapartum periods (including hemorrhages and hematomas); hemorrhagic disease of the newborn; intrauterine infection; large birth weight or excess weight gain; low birth weight; nutritional disorders (delayed introduction of complementary foods, irrational and unbalanced nutrition, lack of vitamins and essential microelements); atopic dermatitis; maternal anemia, acute infectious diseases during pregnancy) it is recommended to take iron supplements in a dose of 2 mg/ kg from 4 months before the introduction of complementary foods containing iron.
To summarize, it should be noted that the introduction into practice of these generally accepted preventive measures (in the form of a mandatory protocol) will improve the health of both women after childbirth and young children.
Pathogenesis (what happens?) During iron deficiency anemia in a child:
Iron leaves the body through urine, feces, sweat, as well as through nails, hair and skin. Losses do not depend on gender. In children, about 0.1–0.3 mg is released into the external environment per 24 hours. In adolescents, the loss is a maximum of 0.5–1.0 mg. The child needs to receive 0.5–1.2 mg of iron per day. There is an increased need for infants and preschoolers. In order for a child to develop normally, the diet should contain 1.5 mg of iron per day in newborns, and at least 10 mg in children from 1 to 3 years old.
Iron deficiency provokes a tendency to infectious diseases of the baby's gastrointestinal tract and respiratory system. Without iron, brain structures cease to function normally. With a lack of iron, disruptions occur in the neuropsychic development of the baby. In children who were diagnosed with iron deficiency anemia in infancy, at the age of 3-4 years, disturbances in the transmission of nerve impulses from the centers of the brain to the organs of hearing and vision are found due to impaired myelination and, as a consequence, impaired nerve conduction.
Clinical manifestations
The symptoms of iron deficiency anemia in children are very diverse; manifestations of the disease can be presented in the form of syndromes:
- astheno-vegetative - caused by hypoxia of the brain, tissues and internal organs and is characterized by symptoms such as child retardation in physical and psychomotor development, irritability, general weakness, frequent dizziness, fainting, enuresis and muscle hypotension;
- epithelial - characterized by dry skin, thickening of the stratum corneum on the knees and elbows, the appearance of cracks in the corners of the mouth, intense hair loss, brittle nail plates;
- dyspeptic - characterized by deterioration of appetite, up to anorexia, constipation or diarrhea, flatulence, changes in taste and olfactory sensations;
- cardiovascular - characterized by shortness of breath, heart murmur, tachycardia, myocardial dystrophy and occurs with severe disease;
- immunodeficiency - characterized by frequent acute respiratory viral infections, as well as low-grade fever;
- hepatolienal - caused by compensatory changes in internal organs (enlargement of the liver and spleen primarily) and occurs with severe anemia.