Chronic lack of iron in the body occurs due to iron deficiency and is characterized by impaired synthesis of hemoglobin, which is contained in red blood cells. The human body receives its first reserves of iron from the mother through the placenta; after birth, iron is replenished through food intake or iron-containing medications. Iron is removed from the body by the urinary and digestive systems, sweat glands and during menstruation in women. About 2 grams of iron are excreted per day, so in order to prevent depletion of reserves, it must be constantly replenished. According to WHO, every 3rd woman and every 6th man in the world suffers from iron deficiency anemia. Pregnant women, children under 3 years of age and teenage girls are at risk.
Causes of iron deficiency anemia (IDA)
- insufficient intake of iron from food: fasting, vegetarianism, or a diet depleted in iron and protein, followed for a long time. In breastfed children, the cause may be iron deficiency anemia of the mother, early transfer to artificial feeding, late introduction of complementary foods
- impaired iron absorption: enteritis (inflammation of the mucous membrane of the small intestine caused by infection or helminthic infestation), gastritis and peptic ulcer of the stomach and duodenum; hereditary diseases (cystic fibrosis and celiac disease); autoimmune damage to the intestinal mucosa and possibly the stomach (Crohn's disease); condition after removal of the stomach and/or duodenum; stomach and intestinal cancer
- chronic blood loss. This is the most basic reason. This includes losses due to: gastric and duodenal ulcers, nonspecific ulcerative colitis, Crohn's disease, hemorrhoids and anal fissures, intestinal polyposis, bleeding from disintegrating tumors of any location and varicose veins of the esophagus; hemorrhagic vasculitis; pulmonary hemorrhages, pulmonary hemosiderosis; chronic pyelonephritis, polycystic disease and cancer of the kidneys and bladder; losses during hemodialysis; uterine fibroids, endometriosis, hyperpolymenorrhea, cervical cancer; nosebleeds
- congenital deficiency of iron in the body (prematurity, birth from multiple pregnancy, severe iron deficiency anemia in the mother, pathological bleeding during pregnancy and childbirth, fetoplacental insufficiency)
- alcoholism (the mucous membrane of the stomach and intestines is damaged, making it difficult to absorb iron)
- use of medications: non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, aspirin) reduce blood viscosity and can promote bleeding, in addition, these drugs can provoke the occurrence of stomach and duodenal ulcers; antacids (Almagel, Gastal, Rennie) reduce the production of hydrochloric acid, which is necessary for effective absorption of iron; iron-binding drugs (desferal), these drugs bind and remove free iron and iron in ferritin and transferrin, and in case of overdose can lead to iron deficiency states
- donation (with donations more than 4 times a year, iron deficiency develops)
- disruption of transferrin synthesis. Transferrin is an iron transport protein that is synthesized in the liver.
Normal hemoglobin level in the blood: in women – 120-140 g/l, in men – 130-160 g/l
Introduction
Anemia is a global problem: approximately 25–30% of people suffer from this disease, and half of all anemia is caused by iron deficiency [1, 2].
Diagnostic criteria for anemia, according to WHO, are hemoglobin levels below 130 g/l in men of all ages and postmenopausal women, for non-pregnant women of reproductive age less than 120 g/l, for pregnant women - less than 110 g/l. These WHO standards are used by physicians in most countries for professional consistency purposes [3, 4]. According to the degree of severity, according to the level of hemoglobin (Hb), anemia is divided into mild (Hb≥90 g/l), moderate (Hb 90–70 g/l), severe (Hb 69–50 g/l) and extremely severe anemia (<50 g/l) [5, 6].
Iron deficiency anemia (IDA) is an acquired disease that is characterized by a reduced iron content in the blood serum, tissue depots, and bone marrow, resulting in the development of hypochromia and trophic disorders in tissues [7–9]. IDA is one of the most common pathological conditions in the world, and in women of childbearing age it is in first place in terms of occurrence [7].
Clinical manifestations of IDA
Anemic syndrome - occurs due to a decrease in the level of red blood cells and hemoglobin in the blood, reducing the saturation of cells and tissues with oxygen. The signs of anemic syndrome are difficult to recognize, but they help to suspect the presence of anemia and, in combination with the data of other examinations, make a diagnosis. These are general weakness, high fatigue and decreased performance, dizziness, tinnitus and flashing “spots” before the eyes, periodic palpitations, shortness of breath with little physical exertion, and fainting. Upon examination, pallor of the skin and visible mucous membranes, slight swelling of the legs, feet, face (mainly the area around the eyes), tachycardia, various types of arrhythmia, moderate heart murmurs, and muffled heart sounds are revealed.
Sideropenic syndrome - caused by iron deficiency in tissues, which causes a decrease in the activity of many enzymes (protein substances that regulate many vital functions), manifested by numerous symptoms:
- change in taste (desire to eat unusual foods: sand, chalk, clay, tooth powder, ice, as well as raw minced meat, unbaked dough, dry cereals)
- tendency to eat hot, salty, spicy foods
- distortion of the sense of smell (attracted by the smell of gasoline, acetone, the smell of varnishes, paints, lime)
- decreased muscle strength and atrophy
- dry, flaky skin; fragility and hair loss; dullness, transverse striations, spoon-shaped concavity of nails; Minor injuries and abrasions do not heal for a long time
- dryness and cracks in the corners of the mouth in 10-15% of patients
- feeling of tongue fullness, redness and atrophy, frequent periodontal disease and caries
- dryness of the esophageal mucosa, which causes pain when swallowing and difficulty swallowing solid food, the development of atrophic gastritis and enteritis
- urgency to urinate, inability to hold urine when coughing, laughing, sneezing, episodes of bedwetting
- the symptom of “blue sclera” is characterized by a bluish coloration of the sclera
- prolonged increase in body temperature to subfebrile levels (37.0-37.9°C) for no apparent reason
- frequent ARVI
What is ZhDA
IDA is a condition in which the body is deficient in iron, which causes a decrease in the number of red blood cells. As a result, various disturbances in the functioning of the body develop, primarily associated with inadequate gas exchange. Therefore, iron deficiency anemia is characterized by weakness, dizziness and even loss of consciousness, as well as a number of other changes in the condition. This may be a consequence of both insufficient intake of iron from food, and a violation of its absorption in the body or excessive consumption.
Therefore, iron deficiency anemia cannot be a primary disease. It is always a consequence of the occurrence of certain violations. At the same time, it accounts for about 80% of all anemia, which requires careful attention to this problem and its detailed consideration.
WHO statistics show that more than 2 billion people worldwide suffer from iron deficiency anemia. But this is only according to official data. In reality, their number is significantly higher.
Normally, iron enters the body along with plant and animal foods. In plant sources it is found in the form of ferric iron, and in animal sources - ferrous. These forms of iron differ in different rates and degrees of absorption. Iron from animal food sources, or heme, is easily absorbed. But trivalent or non-heme iron obtained from plant foods must first be transformed under the action of hydrochloric acid of the stomach into divalent, and after entering the initial parts of the small intestine with the food bolus, it must again transform into the trivalent form.
Some of the iron accumulates in the mucous membrane of the small intestine, and the rest is absorbed into the blood. Moreover, no more than 2.5 mg of iron can be absorbed per day. In the blood it is bound by the protein transferrin, the production of which is responsible for the liver. The amount of iron absorbed and deposited in the intestines is regulated depending on its level in the body. If excess iron comes from food, it is retained in a larger volume in the cells of the mucous membrane of the small intestine, which are subsequently naturally exfoliated and excreted along with feces.
Iron absorbed into the bloodstream is transported by transferrin in two main directions:
- through the portal vein it enters the liver, where it is deposited in the form of the protein ferritin;
- is delivered to red bone marrow cells, where it is used for the synthesis of hemoglobin and takes part in tissue redox reactions.
If disturbances occur at any of these stages, the body develops iron deficiency. Thus, with a decrease in the acidity of gastric juice, which may be a consequence of atrophic gastritis, the use of antacids, or gastric resection, the body’s ability to convert ferrous iron into ferric iron decreases. This means that it cannot be fully absorbed and subsequently participate in biochemical transformations.
With the development of chronic pathologies affecting the intestinal mucous membranes, their ability to absorb iron also decreases. Therefore, it cannot enter the blood in sufficient quantities.
If the binding process of iron by transferrin is disrupted, it cannot be transported effectively throughout the body. Therefore, it does not enter the red brain cells in the required quantities.
In any of these cases, the consequence is a decrease in the ability to form hemoglobin and other iron-containing proteins, i.e., the development of iron deficiency anemia and other metabolic disorders. As a result of a decrease in hemoglobin production, the resulting young red blood cells are smaller in size, and their total number decreases.
Diagnosis of IDA
- clinical blood test: decreased level of hemoglobin, red blood cells, decreased hemoglobin content in one red blood cell, often increased ESR
- biochemical blood test: decrease in serum iron level, increase in total iron-binding capacity of serum, decrease in ferritin content in blood serum
If an iron deficiency is detected in the patient’s body using tests, then the next step will be to search for the causes of this deficiency. To identify the cause of iron deficiency, a comprehensive examination is carried out, including esophagogastroduodenoscopy, sigmoidoscopy, colonoscopy, bronchoscopy, chest x-ray, ultrasound examination of the abdominal organs, pelvis and kidneys, examination by a gynecologist, urologist, hematologist, stool analysis for occult blood and eggs. helminths, as well as examination of red bone marrow from the sternum or ilium (sternal puncture, trephine biopsy).
"We live because we breathe..."
...and iron plays a huge role in this, and at the cellular level. The adult body contains an average of 5 grams of iron. Most of it is found in hemoglobin, which transports oxygen to all organs and tissues, up to 10% is in myoglobin, the “oxygen cushion” for skeletal muscles and myocardium. Our body keeps approximately a quarter of the total amount of iron in reserve - in the liver, muscles, spleen, and bone marrow. And 1% of the mineral is contained in special enzymes that ensure the processes of cellular “respiration”. Iron's position is more than privileged. He even has his own personal “taxi” - the protein transferrin, which “carries” the metal directly to the places of use.
Complications of IDA
Complications arise with prolonged anemia without treatment and reduce the patient’s quality of life: decreased immunity, increased heart rate, which leads to heart failure; in pregnant women, the risk of premature birth and fetal growth retardation increases; in children, iron deficiency causes retarded growth and development; a rare and severe complication is hypoxic coma; hypoxia due to iron deficiency complicates the course of existing cardiopulmonary diseases (coronary artery disease, bronchial asthma, chronic cerebral ischemia, etc.) until the development of emergency conditions, such as acute or repeated myocardial infarction and acute cerebrovascular accident (stroke).
Causes of iron deficiency and increased need for it
- Heavy or prolonged periods. They lead to increased blood loss and depletion of iron reserves.
- Pregnancy and breastfeeding. During pregnancy and childbirth, the need for iron increases on average by 2 times, and during lactation even more.
- Pathological chronic blood loss.
- Passion for vegetarianism, veganism or raw food eating. Non-heme iron from plant foods is less absorbed than heme iron from animals and requires the presence of vitamin C.
- Frequently eating fast food, which is poor in useful components, including minerals.
- Consumption of foods that bind iron and reduce its absorption in the intestines. For example, this is how salts of phytic acid act in unleavened dough made from whole grain flour and in cereals; oxalates of fresh vegetables, especially rhubarb, spinach, sorrel; phosphoproteins of eggs, polyphenolic compounds of coffee and tea, milk lactoferrin, EDTA preservative in carbonated drinks, seasonings, sauces and mayonnaise.
- Taking certain medications (for example, some antibiotics, antacids, proton pump blockers, H2 blockers).
- Diseases of the gastrointestinal tract (celiac disease, peptic ulcer, inflammatory bowel disease, tumors, diverticulosis, parasitic infestations, etc.).
- Pathology of the urinary system (hemorrhagic cystitis, urolithiasis, glomerulonephritis).
- Overweight and obesity. In this condition, there is an increased production of pro-inflammatory substances that negatively affect the absorption and bioavailability of iron.
- Regular exercise. They significantly increase the need not only for proteins, but also for vitamins and minerals, including iron.
Iron chelate, 60 tablets, Evalar
375 ₽
Dietary supplement NOT A MEDICINE
Treatment of IDA
The basic principles of treatment for iron deficiency anemia include eliminating the cause of iron deficiency, correcting the diet, and replenishing iron deficiency in the body.
- The diet for iron deficiency anemia consists of eating foods rich in iron. Patients are advised to have a nutritious diet with the obligatory inclusion in the diet of foods containing heme iron (veal, beef, lamb, rabbit meat, liver, tongue). Plant foods rich in iron include beans, beans, lentils, peas, spinach, cauliflower, potatoes, carrots, beets, bananas, apricots, peaches, apples, blueberries, raspberries, strawberries, almonds and walnuts. It should be remembered that ascorbic acid, which is found in bell peppers, cabbage, rose hips, currants, citrus fruits, sorrel, enhances the absorption of iron in the gastrointestinal tract, and oxalates and polyphenols (coffee, tea, soy protein, milk, chocolate) worsen the absorption of iron. calcium, dietary fiber and other substances. However, no matter how much meat we eat, only 2.5 mg of iron will enter the bloodstream per day - this is exactly how much the body can absorb. And 15-20 times more is absorbed from iron-containing complexes - that’s why the problem of anemia cannot always be solved with the help of diet alone, and therefore iron-containing drugs are prescribed
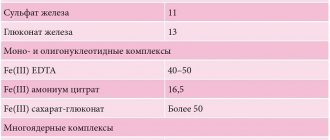
- Oral iron supplements differ from other medications by special rules of administration: - short-acting iron-containing preparations are not taken immediately before or during meals. The medicine is taken 15-20 minutes after meals or in the pause between doses; prolonged medications (sorbifer durules, tardiferron-retard, etc.) can be taken before meals and at night (1-2 times a day); - iron supplements are not taken with milk and milk-based drinks (kefir, fermented baked milk, yogurt) - they contain calcium, which will inhibit the absorption of iron - tablets (except for chewable ones), dragees and capsules are not chewed, are swallowed whole and washed down with plenty of water, rosehip decoction or clarified juice without pulp Oral iron supplements (in tablets, drops, syrup, solution) are the initial treatment for mild to moderate anemia; if there is pregnancy, the intake is agreed with an obstetrician-gynecologist. The duration of treatment is 4–8 weeks until hemoglobin levels normalize, then the drug is taken for 4–6 weeks at half the dose. The most commonly prescribed: - sorbifer durules/fenuls 100 mg, 1-2 tablets 1-2 times a day until hemoglobin levels are restored (in pregnant women, for prevention, 1 tablet 1 time a day, for treatment, 1 tablet 2 times a day) - ferretab comp . 1 capsule per day, up to a maximum of 2-3 capsules per day in 2 divided doses, minimum period of use is 4 weeks - maltofer/actiferrin comes in three dosage forms (drops, syrup, tablets), intake 40-120 drops/10-30 ml syrup / 1-3 tablets per day in 1-2 doses - tardiferron 80 mg, 1-2 tablets per day, pregnant women 1 tablet per day, II-III trimester - totema (combined preparation of iron, copper and manganese) 2- 4 ampoules per day, solution diluted in 1 glass of water, taken for 3-6 months - ferlatum 15 ml 1-2 bottles per day in 2 divided doses
- Injectable iron preparations (venofer, likfer, cosmofer, ferrinject) are used exclusively in the hospital (it is necessary to have the ability to provide anti-shock care), contraindicated during pregnancy and lactation
- Hemotransfusion (transfusion of red blood cell-containing blood components) is performed in case of severe anemia, according to strict indications and in a hospital setting.
Iron metabolism
It is known that iron is an important trace element, which is used mainly as a component of heme in erythrocytes for oxygen transport, and is present in smaller quantities in muscles in the form of heme-myoglobin and in the liver in the form of ferritin [10]. Its sufficient level is necessary to maintain physiological homeostasis [11]. However, excess iron levels can lead to cell death through the formation of free radicals and lipid peroxidation of biological membranes, toxic damage to proteins and nucleic acids. It is important that both iron deficiency and overload can have catastrophic consequences for the body, therefore the content of this microelement is strictly regulated [7, 9, 12–14].
The body of a healthy person contains about 3–5 g of iron, most of which, 2100 mg, is found in blood cells and bone marrow. Approximately 2.5 g of this iron is present in hemoglobin for oxygen transport, and another 2 g is stored as ferritin, mainly in the bone marrow, liver and spleen [9]. In the bone marrow, iron is used to form hemoglobin, liver iron is the main reserve of the microelement, and reticuloendothelial cells of the spleen remove old red blood cells. Finally, relatively small amounts of iron (approximately 400 mg) are present in cellular proteins such as myoglobin and cytochromes, and approximately 3–4 mg is bound to transferrin in the circulation [10, 15]. Almost all metabolically active iron is bound to proteins, and free iron ions can be present in extremely low concentrations.
Under natural conditions, no more than 0.05% (<2.5 mg) of the total amount of iron is lost daily due to exfoliating epithelium of the skin and gastrointestinal tract (GIT), as a result of sweating [12, 13, 16, 17]. The processes of absorption, recycling and storage of iron reserves are regulated by a special hormone - hepcidin, which is produced by liver cells. Under physiological conditions, hepcidin production is controlled by a complex interaction of signals, primarily the level of iron in the blood and the degree of oxygenation of liver tissue. Under pathological conditions, its production is regulated by proinflammatory cytokines, of which interleukin-6 plays a major role [7, 12, 13, 18].
Iron deficiency is detected in people of all age and social groups, but more often in women of reproductive age, young children and the elderly [5, 6]. The main reasons for the development of iron deficiency include decreased food intake, decreased absorption and blood loss. In developed, resource-rich countries, adult diets are almost always adequate, and the most common cause of iron deficiency is blood loss [2, 6].
Forecast and prevention of iron deficiency anemia
In most cases, iron deficiency anemia can be successfully corrected. However, if the cause is not addressed, iron deficiency may recur or progress. Iron deficiency anemia in infants and young children can cause delayed psychomotor and intellectual development.
In order to prevent iron deficiency anemia, annual monitoring of clinical blood test parameters, nutritious nutrition with sufficient iron content, and timely elimination of sources of blood loss in the body are necessary. Persons at risk may be advised to take prophylactic iron supplements.
Prevalence of IDA
Iron deficiency anemia in women is a common pathological condition. Thus, according to WHO (2015), severe iron deficiency is observed in every third woman of reproductive age and in every second pregnant woman, being an important cause of chronic fatigue and poor health, and the third most common cause of temporary disability in women aged 15– 44 years old [12, 19]. In the Russian Federation, despite active preventive and therapeutic measures, the prevalence of IDA remains very high. For example, in Moscow, anemia occurs in almost 38% of gynecological patients [20, 21] and is the most common concomitant pathological process and the first manifestation of the underlying disease, determining the severity of its course and treatment tactics. The main reasons for the development of IDA in women are heavy menstrual bleeding, pregnancy, childbirth (especially repeated ones) and lactation. Anemia often accompanies uterine fibroids, adenomyosis, hyperplastic processes in the endometrium, and ovarian dysfunction. During normal menstruation, 30–40 ml of blood is lost (which is equivalent to 15–20 mg of iron). The critical level corresponds to a blood loss of 40–60 ml, and with a blood loss of more than 60 ml, iron deficiency develops. In women suffering from abnormal uterine bleeding of various origins, the amount of blood lost during one menstruation can reach 200 ml (100 mg of iron) or more. In such situations, the loss of iron exceeds its intake and IDA gradually forms [20].
The most important medical and social problem is anemia in pregnant women, which, according to WHO, is detected in 24–30% of women in economically developed countries and in more than 50% of women in countries with low economic levels [3, 22].
A survey of pregnant women conducted as part of clinical studies in the 2000s showed a high incidence of anemia even among residents of prosperous European countries. Thus, in Belgium (n=1311), Switzerland (n=381) and Germany (n=378) iron deficiency was diagnosed in 6% and 23% (serum ferritin (SF) <15 μg/l) in the first and third trimesters, respectively, of Belgian women; in 19% (SF<12 µg/l) - in Switzerland and Germany. The prevalence of IDA (Hb <110 g/L, SF <15 μg/L) was 16% in Belgium and 3% in Switzerland, although 65–66% of Belgian and Swiss women received dietary iron supplementation during pregnancy. In Germany, IDA was diagnosed in 12% of women [23].
In Russia, according to the Ministry of Health, the incidence of anemia in pregnant women varies from 39% to 44%, in postpartum women - from 24% to 27% [24]. A 2021 systematic review and meta-analysis found that in low- and middle-income countries, pregnancy anemia increases the likelihood of preterm birth by 63%, low birth weight by 31%, perinatal mortality by 51%, and neonatal loss by 2 ,7 times [25].
During pregnancy, there is a significant physiological increase in the need for iron for the normal functioning of the placenta and fetal growth. The total amount of iron required for a normal pregnancy is 1000–1200 mg. To complete a normal pregnancy without developing iron deficiency, a woman must have iron stores in the body at conception of ≥500 mg, which corresponds to an SF concentration of 70–80 μg/L [20, 23].
Symptoms
IDA can manifest itself differently in different people. In general, this disease is characterized by the development of 2 syndromes: sideropenic and anemic.
Sideropenic syndrome is caused by the occurrence of disturbances in the condition of the skin and mucous membranes against the background of a lack of iron in the body, i.e., a disturbance in the course of metabolic processes. Therefore, with IDA, the following may occur:
- dryness, decreased skin tone, peeling and cracking;
- fragility and separation of nails, the formation of transverse stripes on them, the development of onychodystrophy with flattening or acquisition of a concave shape by the nail;
- cracks and ulcers in the corners of the mouth (cheilitis);
- development of stomatitis (ulceration of the oral mucosa);
- deterioration of hair condition, including loss of shine, hair loss, increased fragility, which leads to split ends;
- disorders of taste preferences with the appearance of a tendency to eat chalk, lime, coal, earth, paint, etc.;
- pathological desire to inhale unpleasant and even downright toxic odors of solvents, paints and varnishes, gasoline, fuel oil, exhaust gases, etc.;
- diseases of the gastrointestinal tract, including damage to the tongue (glossitis, cracking), gums (gingivitis, periodontal disease), teeth (caries), stomach and intestines (enteritis, gastritis);
- unproductive cough, sensation of a foreign body in the throat, difficulty swallowing;
- discomfort during sexual intercourse, increased incidence of infectious urological diseases;
- disruption of the functioning of the sphincters (circular muscles that close the intestines, urethra, etc.), which leads to stress urinary incontinence, for example, when coughing, nocturnal enuresis, etc.
The most characteristic symptom that occurs in most patients with iron deficiency anemia is pale skin. Often it even takes on a greenish tint. In this case, the sclera (whites) of the eyes may become bluish.
Anemic syndrome develops as a result of impaired gas exchange against the background of a drop in hemoglobin levels. Its main manifestations are:
- weakness;
- fast fatiguability;
- the appearance of drowsiness during the day;
- attacks of dizziness;
- loss of consciousness;
- frequent headaches;
- noise in ears;
- flashing spots before the eyes;
- attacks of shortness of breath during physical exertion;
- increased heart rate (tachycardia);
- discomfort in the heart area;
- lowering blood pressure levels.
Sometimes with iron deficiency anemia there is a persistent increase in body temperature to subfebrile levels, and this may be the only symptom of the pathology. While taking iron supplements, the temperature normalizes.
Quite often, the decrease in the level of iron in the body, and therefore the hemoglobin produced, proceeds smoothly. Therefore, many organs and systems manage to adapt to the changed conditions of existence. During this time, the patients’ well-being gradually deteriorates, but since this happens slowly, they do not notice pronounced changes in their condition and attribute the symptoms that appear to overwork. Therefore, often at the moment when they undergo examination or go to the doctor, a severe form of IDA is already observed.
Diagnosis of anemia
To diagnose anemia at CITILAB you can undergo the following tests:
- 11-10-001 – General blood test
- 95-13-211 – Vitamin B12
- 33-20-038 – Folic acid (folates)
- 26-20-100 – Serum iron
You can also run profile 99-00-026 - “Chronic Anemia”, which includes additional parameters for diagnosing and determining the type of anemia. For example, ferritin, which reflects how much ferric ions are deposited; total serum binding capacity, haptoglobin, transferritin and other important indicators.