Pharmacological properties of the drug Tracrium
A peripherally acting muscle relaxant of the non-depolarizing competitive type. Blocks H-cholinergic receptors in the terminal plates of skeletal muscle fibers and prevents the depolarizing effect of acetylcholine, resulting in inhibition of neuromuscular transmission at the level of the postsynaptic membrane. After intravenous administration, it is spontaneously metabolized by Hoffman elimination (a non-enzymatic process that occurs at physiological values of blood pH and body temperature of the patient), as well as by ether hydrolysis with the participation of nonspecific esterases in blood plasma. This leads to the formation of laudanosine and other metabolites. Metabolites do not have muscle relaxant properties. The binding of atracurium besylate to plasma proteins is about 80%, the half-life is 20 minutes. Excreted in urine and bile, mainly in the form of metabolites.
Use of the drug Tracrium
Adults Administration by injection Tracrium is administered by intravenous bolus injection. The dosage regimen for adults is 0.3–0.6 mg/kg body weight, depending on the required duration of complete neuromuscular blockade and provides adequate relaxation for 15–35 minutes. Endotracheal intubation can be performed during the first 90 s after intravenous administration of the drug at a dose of 0.5–0.6 mg/kg body weight. If it is necessary to enhance the blocking effect, the drug is additionally administered at a dose of 0.1–0.2 mg/kg body weight. Correct additional dosing does not increase the cumulative effect of neuromuscular blockade. Restoration of normal neuromuscular transmission occurs after 35 minutes. Neuromuscular blockade caused by the use of Tracrium can be quickly neutralized by the use of anticholinesterase drugs in standard doses. Administration by infusion After the initial administration of a bolus dose of the drug 0.3–0.6 mg/kg body weight, further maintenance of neuromuscular blockade during prolonged surgery is carried out by long-term intravenous infusion of the drug in the mode of 0.3–0.6 mg /kg/h. The drug can be used by intravenous infusion during coronary artery bypass grafting. If body hypothermia is necessary to a temperature of 25–26 °C, the level of inactivation of atracurium besylate is reduced, therefore, to maintain complete neuromuscular blockade in this case, the rate of infusion of the drug can be reduced by 2 times. Compatibility with other solutions and the period of stability of the drug are given below:
Solution for intravenous infusion | Period of stability |
| Sodium chloride solution (0.9%) | 24 hours |
| Glucose solution (5%) | 8 hours |
| Ringer's solution | 8 hours |
| Sodium chloride solution (0.18%) and glucose solution (4%) | 8 hours |
| Hartmann solution | 4 hours |
When diluted in the above solutions to achieve a concentration of atracurium besylate at a concentration of 0.5 mg/ml or higher, the resulting solution will remain stable in daylight during the specified period at a temperature not exceeding 30 °C. Children The drug is used in children over 1 month of age in the same dose as in adults, the dose is calculated according to the child’s body weight. Elderly patients Used in standard dosage, however, it is recommended to prescribe the initial dose at the lower limit of the dose range and administer the drug more slowly. Renal and liver failure The drug is prescribed in standard doses for any level of renal or liver failure, including terminal stages. Patients with cardiovascular diseases In patients with clinically significant manifestations of cardiovascular diseases, the initial dose of the drug should be administered over a period of at least 60 s. Patients in intensive care units After administration of the required initial bolus dose of the drug in the range of 0.3–0.6 mg/kg body weight, further maintenance of the neuromuscular blockade is ensured by a constant IV infusion of the drug at a rate of 11–13 mcg/kg/ min (0.65–0.78 mg/kg/h). However, there is wide individual variability in the dosage regimen of the drug, which may also change over time. Some patients may require a low dosage level of 4.5 mcg/kg/min (0.27 mg/kg/h), while others may require a high dose of 29.5 mcg/kg/min (1.77 mg/kg). /h). The rate of restoration of neuromuscular transmission in patients does not depend on the duration of use of the drug and, according to clinical studies, is in the range of 32–108 minutes. Monitoring In order to individualize the dosage regimen, as with the use of other drugs that block neuromuscular transmission, its function should be constantly monitored.
Tracrium, 10 mg/ml, solution for intravenous administration, 5 ml, 5 pcs.
IV.
Adults and children over 1 month.
Bolus administration
Recommended doses for adults are 0.3–0.6 mg/kg (depending on the required duration of neuromuscular blockade), which provides adequate myoplegia within 15–35 minutes.
Tracheal intubation can be performed within 90 s after intravenous administration of Trakrium at a dose of 0.5–0.6 mg/kg.
The duration of complete neuromuscular blockade can be increased by introducing additional doses at the rate of 0.1–0.2 mg/kg, which is not accompanied by cumulation of the effect of the drug. Spontaneous restoration of conduction after complete neuromuscular blockade is observed after approximately 35 minutes (determined by the restoration of tetanic contraction to 95% of the original). Neuromuscular conduction can be quickly restored with the administration of anticholinesterase drugs (neostigmine, etc.) in combination with atropine without the appearance of signs of recurarization.
Infusion administration
After an initial bolus of 0.3–0.6 mg/kg Tracrium can be administered by continuous infusion at a rate of 0.3–0.6 mg/kg/hour to maintain neuromuscular blockade during prolonged surgical procedures. This method of administration can be recommended for operations on the heart and lungs.
With artificial hypothermia, accompanied by a decrease in body temperature to 25–26 °C, the rate of inactivation of atracurium decreases, therefore, to maintain complete myoplegia, the infusion rate should be reduced by approximately 2 times.
Elderly patients
Tracrium is prescribed in standard doses, but it is preferable to use the lower end of the recommended dosage range and administer the drug slowly.
If liver and/or kidney function is impaired,
incl. for end-stage liver or kidney failure, Tracrium is prescribed in standard doses.
Use for diseases of the cardiovascular system.
In patients with severe cardiovascular pathology, the initial dose should be administered over at least 60 seconds.
Use in intensive care units.
To maintain myoplegia after an initial bolus dose of 0.3–0.6 mg/kg, Tracrium can be administered by continuous infusion at a rate of 11–13 mcg/kg/min (0.65–0.78 mg/kg/h). The dose is not the same for different patients and may change over time. Some patients may require doses as low as 4.5 mcg/kg/min (0.27 mg/kg/hour) and doses as high as 29.5 mcg/kg/min (1.77 mg/kg /h). Spontaneous recovery of neuromuscular conduction (T4/T1>0.75) usually occurs approximately 60 minutes (in clinical trials, this period ranged from 32 to 108 minutes) after Tracrium infusion and its rate does not depend on the duration of drug administration.
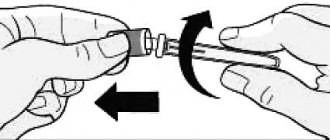
Instructions for use
Tracrium is compatible with the following infusion solutions.
| Infusion solution | Stability period, h |
| Sodium chloride solution for intravenous infusion (0.9%) | 24 |
| Glucose solution for intravenous infusion (0.9%) | 8 |
| Ringer's solution for injection | 8 |
| Solution of sodium chloride (0.18%) and glucose (4%) for intravenous infusion | 8 |
| Hartmann's solution for injection | 4 |
Tracrium solution, when diluted with compatible infusion solutions to obtain an atracurium besylate concentration of at least 0.5 mg/ml, remains stable for a specified period of time under normal lighting and temperatures up to 30 °C.
Side effects of the drug Tracrium
The following side effects are classified by organ, system and frequency of occurrence. Classification of the frequency of side effects: very often (1/10); often (1/10, but ≤1/100); uncommon (1/100, but ≤1/1000); rare (1/1000, but ≤1/10,000); very rare (≤1/10,000). The definition of “ unknown ” refers to those side effects when it is impossible to determine the frequency of their occurrence from available sources. Data obtained from clinical studies Vascular disorders Often: skin hyperemia*, arterial hypotension (moderate, transient)*. Respiratory and thoracic disorders Uncommon : bronchospasm *. *These symptoms may be due to an increase in histamine release. Data obtained from post-licensing use Immune system Very rare: anaphylactic, anaphylactoid reactions. When Tracrium is used in combination with other anesthetic drugs, there are isolated reports of severe anaphylactoid or anaphylactic reactions. CNS Convulsions (frequency unknown ). There are isolated reports of the occurrence of seizures in patients undergoing intensive treatment when using Trakrium in combination with other drugs. These patients, as a rule, had one or more factors causing convulsive syndrome (head injury, cerebral edema, viral encephalitis, hypoxic encephalopathy, uremia). A causal relationship with the action of laudanosine has not been established. According to clinical studies, a correlation between the level of laudanosine in the blood plasma and the occurrence of seizures has not been established. Musculoskeletal system and connective tissue Myopathy, muscle weakness (the frequency of their occurrence is unknown ). With long-term use of muscle relaxants in critically ill patients in intensive care units, cases of muscle weakness and/or myopathy have been reported. The majority of these patients received concomitant treatment with corticosteroids. Such reports were infrequent, and a causal relationship with the use of Tracrium has not been established.
Special instructions for the use of the drug Tracrium
Like all other neuromuscular blockers, atracurium besilate causes paralysis of the respiratory muscles in the same way as other skeletal muscles, without affecting consciousness. Therefore, the use of the drug is possible only against the background of adequate general anesthesia under the supervision of an experienced anesthesiologist and in the presence of equipment for endotracheal intubation and mechanical ventilation. In sensitive patients, there is a potential for histamine release during the use of atracurium besylate, so caution should be exercised when administering it to patients with allergic diseases and hypersensitivity to histamine. Because there are reports of cross-sensitivity between various neuromuscular blocking agents, atracurium besylate should be administered with caution to patients with hypersensitivity to other drugs in this group. When used in recommended doses, Tracrium does not have a significant vagal or ganglion-blocking effect and is not contraindicated in bradycardia associated with the use of many anesthetics or vagal stimulation during surgery. As with other non-depolarizing muscle relaxants, patients with myasthenia gravis, neuromuscular diseases and severe electrolyte disturbances may experience increased sensitivity to Tracrium. In patients at risk of a significant decrease in blood pressure, for example with hypovolemia, Tracrium should be administered over 60 s. Atracurium besylate is inactivated at a high pH value of the solution, so it cannot be mixed in the same syringe with sodium thiopental or any other alkaline solution. After introducing Tracrium into a peripheral vein or when introducing other drugs into the same needle or cannula, the infusion system should be flushed with an adequate amount of isotonic sodium chloride solution. Tracrium is a hypotonic solution and cannot be used in the same infusion system with blood products or during blood transfusion. In patients sensitive to malignant hyperthermia, it was found that the drug does not contribute to the appearance of this hyperthermia syndrome. As with the use of other non-depolarizing muscle relaxants, patients with burns may develop resistance to Tracrium, which may require increasing its dose depending on the period that has passed since the burn and the area of the burn surface. The results of experimental and clinical studies conducted on animals indicate that when atracurium besylate is used in high doses, its metabolite laudanasine can cause arterial hypotension, and sometimes the effect of cerebral excitation. A reliable reason for the relationship between the seizures observed in patients receiving Tracrium and the action of the laudanasine metabolite has not been established. During pregnancy and breastfeeding. During pregnancy, Tracrium should be used with caution and only if the expected benefit to the mother outweighs the potential risk to the fetus. In obstetric practice, Tracrium can be used as a muscle relaxant during cesarean section, since when used in recommended doses it does not cross the placenta in a clinically significant concentration. It is not known whether atracurium besylate and its metabolites are excreted in breast milk. Ability to drive vehicles and operate other machinery . No data.
Tracrium®
The table of pharmaceutical compatibility of Trakrium with some infusion solutions is given in the section “Interaction with other drugs and other interactions”.
Patient groups
— Injection use in adults
Tracrium is administered intravenously as injections. For adults, the dose range is about,
3-0.6 mg/kg (depending on the required duration of complete blockade), which provides adequate myoplegia within 15-35 minutes.
After intravenous administration in doses of 0.5-0.6 mg/kg, endotracheal intubation can usually be performed after 90 seconds.
If it is necessary to prolong complete neuromuscular blockade, Tracrium is additionally administered at a dose of 0.1-0.2 mg/kg. Correct administration of additional doses of the drug does not lead to accumulation of the muscle relaxant effect.
Spontaneous restoration of conduction after complete neuromuscular blockade occurs after approximately 35 minutes, as determined by the restoration of tetanic contraction to 95% of normal neuromuscular function. The neuromuscular blockade caused by atracurium can be quickly reversed by the use of anticholinesterase agents in standard doses, such as neostigmine and edrophonium, in combination with simultaneous or preliminary administration of atropine (without signs of recurarization).
Infusion use in adults
After an initial bolus dose of 0.3-0.6 mg/kg, Tracrium can be used to maintain neuromuscular blockade during prolonged surgery by continuous infusion at a rate of 0.3-0.6 mg/kg/hour.
Tracrium can be administered by infusion during cardiopulmonary bypass surgery at the rate recommended for infusion. With induced hypothermia with a body temperature of 25° to 26°C, the rate of inactivation of Tracrium decreases, thus, to maintain complete muscle relaxation at low temperatures, the infusion rate is reduced by approximately 2 times.
Children
For children aged 2 years and older, Tracrium is prescribed in the same doses as adults, based on body weight.
The initial dose of Tracrium used in children aged 1 month to 2 years under halothane anesthesia is 0.3 - 0.4 mg/kg. Children may require more frequent maintenance doses than adults.
Elderly patients
Tracrium can be used in standard doses in elderly patients. However, it is recommended to use an initial dose that is less than the lower value of the dose range and to administer the drug slowly.
Use in patients with impaired renal and/or liver function.
Tracrium can be used in standard doses for any degree of liver or kidney dysfunction, including end-stage failure.
Use in patients with cardiovascular diseases
In patients with cardiovascular diseases with severe clinical symptoms, the initial dose of Tracrium should be administered within 60 seconds.
Use of BIT in patients
After administration, if necessary, Tracrium in an initial bolus dose of 0.3-0.6 mg/kg, the drug can be used to maintain neuromuscular blockade by performing a continuous infusion at a rate of 11-13 mcg/kg/min (0.65-0. 78 mg/kg/h). However, there is wide interindividual variation in dosage regimen. The dosage regimen may change over time. Some patients may require either a low infusion rate of 4.5 mcg/kg/min (0.27 mg/kg/h) or a high infusion rate of 29.5 mcg/kg/min (1.77 mg/kg/h).
The rate of spontaneous recovery after neuromuscular blockade at the end of the Trakrium infusion in BIT patients does not depend on the duration of administration. Spontaneous recovery of neuromuscular conduction (ratio of quarter height to first twitch in the train-of-four test T4/Ti>0.75) usually occurs after approximately 60 minutes. In clinical studies, this period ranged from 32 to 108 minutes after infusion of Tracrium, and its speed does not depend on the duration of drug administration.
Monitoring
As with the use of other muscle relaxants, monitoring of neuromuscular function is recommended throughout the entire period of use of Trakrium to determine the dosage regimen in each individual case.
Interactions of the drug Tracrium
The neuromuscular blockade caused by Tracrium can be enhanced by the use of inhaled anesthetics such as halothane, isoflurane, and enflurane. When Tracrium is administered, the intensity of neuromuscular blockade and/or its duration may increase when used in combination with:
- antibiotics, including aminoglycosides, polymyxins, spectinomycins, tetracyclines, lincomycin and clindamycin;
- antiarrhythmic drugs: propranolol, calcium channel blockers, lidocaine, procainamide, quinidine;
- diuretics: furosemide, possibly with mannitol, thiazide diuretics, acetazolamine;
- magnesium sulfate;
- ketamine;
- lithium salts;
- ganglion blockers (trimethorphan, hexamethonium).
Rarely, when administered simultaneously with certain drugs that increase the manifestations of myasthenia gravis (including during its latent course) and provoke the development of myasthenic syndrome, increased sensitivity to atracurium besilate is possible. These drugs include various antibiotics, β-adrenergic blockers (propranolol, oxprenolol), antiarrhythmics (procainamide, quinidine), antirheumatic drugs (chloroquine, D-penicillamine), trimetaphan, chlorpromazine, steroids, phenytoin and lithium. In patients receiving long-term anticonvulsants, a later onset and shorter duration of neuromuscular blockade caused by Trakrium are possible. Administration of non-depolarizing neuromuscular blocking agents in combination with atracurium besylate may cause greater neuromuscular blockade than would be expected with an equivalent total dose of atracurium besylate. The synergistic effect may vary depending on the combination of drugs. Depolarizing muscle relaxants should not be administered to increase the duration of neuromuscular blockade caused by non-depolarizing muscle relaxants, as this may lead to the development of prolonged and deep relaxation, which is difficult to eliminate with anticholinesterase drugs.
Tracrium
Ethyl ether, and to a lesser extent fluorotane, hexenal, and sodium thiopental enhance and prolong the effect of atracurium besylate.
Aminoglycosides and polypeptide antibiotics (polymyxin), spectinomycin, capreomycin, amphotericin B, trimetaprim, tetracyclines, lincomycin, clindamycin, antiarrhythmic drugs (propranolol, BMCC, lidocaine, procainamide, quinidine), procaine (iv), diuretics (furosemide, ethacrynic acid , indapamide, mannitol, thiazide, acetazolamide), corticosteroids, mineralocorticoids, magnesium sulfate, ketamine, Li+ salts, ganglion blockers (trimetaphane camsilate, hexamethonium), depolarizing muscle relaxants, citrates enhance neuromuscular blockade.
Reduces the effect of anticholinesterase drugs, edrophonium chloride (dosage adjustment may be required).
Antibiotics, beta-blockers (propranolol, oxprenolol), antiarrhythmic drugs (procainamide, quinidine), antirheumatic drugs (chloroquine, D-penicillamine), trimetaphane camsilate, chlorpromazine, steroids, phenytoin, Li+ drugs can enhance or unmask latent myasthenia or cause myasthenic syndrome, which can lead to the development of hypersensitivity to the drug.
Opioid analgesics increase respiratory depression. High doses of sufentanil reduce the need for high initial doses of nondepolarizing muscle relaxants. Underpolarizing muscle relaxants prevent or reduce muscle stiffness caused by high doses of opioid analgesics (including alfentanil, fentanyl, sufentanil), while the risk of developing bradycardia and lowering blood pressure caused by opioid analgesics is not reduced (especially in patients with impaired myocardial function and/or or against the background of the prescription of beta-blockers), moreover, it increases the risk of arterial hypotension (the use of H1- or H2-histamine receptor blockers can prevent the development or reduce the severity of these adverse effects). Increases histamine-dependent side effects caused by opioid analgesics (with the exception of alfentanil, fentanyl and sufentanil, which do not cause histamine release)
Inhaled anesthetics (including enflurane, isoflurane) enhance the effect (the dose of peripheral muscle relaxants should be reduced to 1/3-1/2 of the usually recommended).
Ca2+ drugs reduce the effect. Doxapram temporarily masks the residual effects of muscle relaxants.
Compatible with the following solutions for infusion (at a concentration of 0.5-0.9 mg/ml in daylight and temperatures up to +30 degrees C): 0.9% NaCl solution for intravenous administration - for at least 24 hours, 5% dextrose solution for intravenous administration - 8 hours, Ringer's solution for injection - 8 hours, solution of NaCl 0.18% and dextrose 4% for intravenous administration - 8 hours, sodium lactic acid solution (Hartmann solution) for intravenous administration - 4 hours .
Do not mix in the same syringe with sodium thiopental or other alkaline solution (inactivation).
Tracrium drug overdose, symptoms and treatment
Symptoms : prolonged paralysis of skeletal muscles and its consequences are the main signs of overdose. Treatment : maintain unobstructed air access along with positive pressure ventilation until spontaneous breathing is restored. At this time, it is necessary to ensure complete sedation of the patient. When the first signs of spontaneous respiratory recovery appear, it can be accelerated by the administration of anticholinesterase drugs in combination with atropine.