Chronic pancreatitis (CP) is a long-term inflammatory disease of the pancreas, with manifestations in the form of irreversible changes in the structure of the organ, which cause pain and/or a persistent decrease in its function.
The pancreas performs important functions:
- secretion of most digestive enzymes
- production of insulin (a hormone whose deficiency develops diabetes mellitus)
There is a worldwide trend toward an increase in the incidence of acute and chronic pancreatitis, more than doubling over the past 30 years.
Reasons for the development of pancreatitis
The most common cause of chronic pancreatitis is alcohol consumption, and the quality and raw materials from which the drink is made do not matter.
Other reasons
- Toxins and metabolic factors:
- alcohol abuse
- smoking
- increased calcium levels in the blood (develops in patients with a tumor of the parathyroid glands)
- overeating and eating fatty foods
- protein deficiency in food
- effects of medications and toxins
- chronic renal failure
- Blockage of the pancreatic duct:
- stones in this channel
- due to dysfunction of the sphincter of Oddi
- blocking of the duct by a tumor, cysts
- post-traumatic scars of the pancreatic ducts (complication of endoscopic procedures: papillosphincterotomy, stone removal, etc.)
- Pathology of the gallbladder and biliary tract.
- Pathology of the duodenum.
- Consequences of acute pancreatitis.
- Autoimmune mechanisms.
- Heredity (gene mutations, 1-antitrypsin deficiency, etc.).
- Helminths.
- Insufficient oxygen supply to the pancreas due to atherosclerosis of the vessels supplying blood to this organ.
- Congenital anomalies of the pancreas.
- Idiopathic chronic pancreatitis (the cause cannot be determined).
Causes
The disease occurs under the influence of such factors:
- in 60% of cases, the cause of pancreatitis is alcohol consumption; however, the disease develops only in 5–7% of drinkers, which is due to a genetic predisposition to it;
- cholelithiasis, chronic cholecystitis and other conditions accompanied by stagnation of bile;
- cicatricial deformation of the duodenum, tumor of the papilla of Vater, that is, mechanical obstacles to the release of pancreatic juice into the intestine;
- cystic fibrosis is a genetic disease with a violation of the secretory activity of the glands, accompanied by damage to the respiratory system;
- lipid metabolism disorders, manifested by repeated episodes of acute inflammation;
- autoimmune diseases (primary pancreatic disease, Sjogren's syndrome, primary biliary cirrhosis, sclerosing cholangitis);
- some medications - azathioprine, furosemide, tetracyclines, estrogen preparations, prednisolone, metronidazole and others.
Pancreatitis in children is often associated with pathology of the structure of the biliary tract and pancreas, both congenital and acquired (opisthorchiasis). Often the cause of illness in a child is blunt trauma to the abdomen. Infections play a certain role - herpes, mononucleosis, mumps, salmonellosis.
Symptoms of pancreatitis
- abdominal pain: usually the pain is localized in the epigastrium and radiates to the back, increasing after eating and decreasing when sitting or bending forward
- nausea, vomiting
- diarrhea, steatorrhea (fatty stool), increased stool volume
- bloating, rumbling in the stomach
- weight loss
- weakness, irritability, especially on an empty stomach, sleep disturbance, decreased performance
- the symptom of “red drops” is the appearance of bright red spots on the skin of the chest, back and abdomen.
If such symptoms appear, it is recommended to undergo examination to exclude chronic pancreatitis.
Pancreatitis in children
In young children, pancreatitis is usually a consequence of congenital malformations of the digestive system or enzyme deficiency. It can also be a complication of mumps (mumps). In older children, the development of the disease may be associated with poor nutrition (including abuse of sweets and carbonated drinks) or caused by intestinal parasites.
Children are often unable to clearly formulate their complaints, what and how they hurt. Therefore, at the first signs of the disease (the child’s complaints of abdominal pain, nausea, vomiting, unstable stool with impurities of undigested food), you should immediately consult a doctor. Infants with pancreatitis cry hysterically and quickly lose weight. Their tummy is swollen.
It is necessary to diagnose the disease promptly and begin treatment to prevent loss of the pancreas.
More information about pancreatitis in children
Complications of chronic pancreatitis
If left untreated, possible complications of chronic pancreatitis include:
- diabetes
- vitamin deficiency (mainly A, E, D)
- increased bone fragility
- cholestasis (with and without jaundice)
- inflammatory complications (inflammation of the bile ducts, abscess, cyst, etc.)
- subhepatic portal hypertension (fluid accumulation in the abdominal cavity, enlarged spleen, dilation of the veins of the anterior abdominal wall, esophagus, liver dysfunction)
- effusion pleurisy (fluid accumulation in the membranes of the lungs)
- compression of the duodenum with the development of intestinal obstruction
- pancreas cancer.
First aid for an attack of pancreatitis
To reduce pain, you can use a heating pad filled with cold water. It needs to be applied to the abdominal area, namely to the epigastric region (the area under the xiphoid process, corresponding to the projection of the stomach onto the anterior abdominal wall). This allows you to reduce the intensity of pain, slightly reduce swelling and inflammation.
The patient must comply with the hospital regime. This will reduce blood flow to the organ, and therefore reduce inflammation.
Eating is prohibited. The digestion process can cause more severe pain, nausea and vomiting. And the diet will reduce the production of enzymes that increase the inflammatory response and pain. You need to fast for 3 days. You can drink clean water without gases.
It is imperative to call a doctor for an examination, even if the patient is not exactly sure that this is an attack of acute pancreatitis. As we already know, this pathology can subside and then rapidly recur. At this time, you can take a painkiller to reduce discomfort.
Severity of chronic pancreatitis
There are three degrees of severity of chronic pancreatitis:
Mild degree
- exacerbations are rare (1-2 times a year), short-lived
- moderate pain
- no weight loss
- no diarrhea, no fatty stools
- Coprological examination of stool is normal (no neutral fat, fatty acids, soaps)
With mild severity of chronic pancreatitis, long courses of medication are usually not required, since lifestyle changes and giving up bad habits often prevent relapses.
Average degree
- exacerbations 3-4 times a year, occur with prolonged pain syndrome
- There may be an increase in amylase and lipase in the blood
- periodic loose stools, greasy stools
- there are changes in the coprogram
With moderate severity of chronic pancreatitis, a strict diet, longer courses of therapy, and constant supervision by the attending physician are necessary.
Serious condition
- frequent and prolonged exacerbations with severe, prolonged pain syndrome
- frequent loose stools, fatty stools
- loss of body weight, up to exhaustion
- complications (diabetes mellitus, pseudocysts, etc.)
In severe cases of chronic pancreatitis, constant maintenance therapy, stronger medications and a strict diet are required. Often, patients need careful monitoring not only by a gastroenterologist, but also by doctors of other specialties (endocrinologist, surgeon, nutritionist). Emerging exacerbations, as well as complications of the disease, pose a threat to the patient’s life and, as a rule, are an indication for hospitalization.
The presence of chronic pancreatitis, regardless of severity, requires immediate consultation with a doctor, since without treatment and lifestyle changes, the process will steadily progress.
Treatment Basics
The approach to treating pancreatitis varies depending on the form of the disease. In acute severe form of pancreatitis, when there is pain and constant vomiting, the patient is hospitalized. In case of a chronic disease and in the absence of relapses, hospitalization is not required; doctors fight the cause of the disease with the help of drugs.
Acute pancreatitis on a CT image. Photo: Hellerhoff / (Creative Commons Attribution-Share Alike 3.0 Unported license)
After admission to the hospital with acute pancreatitis, the patient is not fed, as a rule, for the first 48 hours. A tube is inserted into the stomach to remove its contents. If there are complications (bleeding, acute intestinal obstruction, suppuration, etc.), the patient is referred for surgery.
Next, the doctor prescribes various medications to reduce the load on the gland, reduce pain and prevent the development of infection.
With pancreatitis, control of the production of pancreatic digestive enzymes is vital. Lack of oral nutrition in the first week after the attack is over is the most effective way of such control. Therefore, parenteral nutrition is used, that is, intravenous infusion through a dropper, or enteral nutrition, in which nutritional mixtures are administered through a tube.
Pancreatitis can occur with a complication in the form of death of part of the pancreas or the entire organ (pancreatic necrosis). In this case, doctors adhere to a conservative method of treatment with the help of medications. In case of infected pancreatic necrosis, the use of antibiotics is mandatory. If conservative treatment does not help and the patient progresses to multiple organ failure, suppuration, pancreatic necrosis or pancreatic cancer, surgery is prescribed.
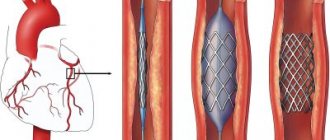
At the first stage, doctors prefer to minimize surgical intervention in the body. First, puncture and drainage of the pancreas and retroperitoneum are performed. To do this, using small incisions, special tubes (drains) are inserted inside, which remove excess liquid and wash the cavity with special solutions.
In case of a more severe condition of the patient and widespread damage to the gland, they resort to alternative treatment tactics, which include:
- laparotomy, that is, external drainage, in which incisions are made in the abdominal wall,
- resection of the gland or removal of it entirely.
Removing the gland is an extreme measure; it is resorted to in a situation where the organ can no longer be restored. It is possible to live without a gland, but you will have to artificially maintain its functions: take insulin, enzyme preparations and follow a very strict diet.
How to cope with an attack of pancreatitis?
The main task when severe pain occurs is to provide the gland with cold, hunger and peace. You should not eat anything and consult a doctor immediately. To relieve inflammation, you need to put a cold compress on your stomach.
Diagnosis of pancreatitis
The EXPERT Clinic has an algorithm for diagnosing chronic pancreatitis, which includes:
Laboratory methods:
- A clinical and biochemical blood test is performed (of particular importance is the level of pancreatic enzymes in the blood - amylase, lipase)
- coprogram - the presence of certain substances in the stool (fats, soaps, fatty acids, etc.) is assessed. Normally, they should be absent, but in chronic pancreatitis, due to insufficient production of enzymes by the gland to break down these substances, they remain undigested and are detected in the feces
- fecal elastase is an enzyme of the pancreas, the level of which decreases when it is not working enough
- in certain cases, it is important to determine cancer markers
- If a hereditary genesis of the disease is suspected, a genetic examination of the patient is carried out.
Instrumental studies
- Ultrasound of the abdominal cavity. Signs of inflammation of the pancreatic tissue, the presence of stones in the ducts, calcifications, cysts, and tumors of the pancreas are assessed. Additionally, changes in other organs of the gastrointestinal tract are determined to exclude complications of the disease, as well as concomitant pathologies.
- Elastography of the pancreas.
Allows you to determine whether there is fibrosis (hardening) of the pancreas, which is a criterion for the severity of structural changes in the organ. Ultrasound with elastography of a healthy pancreas - FGDS. Visualization of the duodenum is necessary to assess the presence of inflammation in it, as well as indirect signs of pancreatitis. It is necessary to exclude inflammation and pathological formations (tumor, diverticulum) in the area of the large duodenal nipple (through it, pancreatic secretions enter the duodenum; when it is blocked, the outflow of this secretion is disrupted, which leads to inflammation of the gland tissue). Visualization of the stomach and esophagus is necessary to exclude erosions, ulcers, and inflammation in them. Pathological changes in these organs are often combined with chronic pancreatitis, being mutually aggravating conditions.
- Additionally, CT and MRI of the abdominal cavity with cholangiography and RCHP may be prescribed. They are necessary to confirm the diagnosis, and are also prescribed if there is a suspicion of the presence of pathological formations in the pancreas, blockage of the gland ducts with a stone, tumor or cyst.
Diagnostics
To confirm the diagnosis of pancreatitis, in addition to analyzing complaints, medical history, and examining the patient, doctors use laboratory and instrumental diagnostic methods.
Analyzes
In a blood test during a severe inflammatory process in the gland, nonspecific changes are revealed: an increase in the number of leukocytes, an increase in ESR. Such disorders are recorded in acute cases and in a third of cases of exacerbation of the disease. There were no changes in blood tests in the remaining patients.
The main biochemical sign of the disease is the appearance in the blood and urine of a large amount of the enzyme necessary to break down starch. This is the enzyme amylase; when examined in urine, it is called diastasis. In addition, the concentration of other pancreatic enzymes increases: lipase, phospholipase A2, trypsin, elastase.
Additional biochemical signs of pancreatitis:
- increased levels of bilirubin and transaminases;
- an increase in fibrinogen levels is a sign of increased blood clotting;
- increased concentrations of glucose and urea.
Detection of enzymes in the blood is observed during the acute course of the disease and exacerbation of the chronic form of the pathology. In many patients, tests remain normal. Therefore, the main role in diagnosing the disease, especially its chronic forms, belongs to instrumental studies.
Of additional importance for identifying exocrine insufficiency, that is, a lack of digestive enzymes, is a coprogram - stool examination. Muscle fibers, neutral fats, and starch grains are found in feces.
Instrumental methods
For the diagnosis of acute pancreatitis, computed tomography or magnetic resonance imaging is advantageous. They make it possible to detect the destruction of glandular cells and tissue swelling. The diagnosis is confirmed by laparoscopy.
Methods for diagnosing chronic inflammation of the pancreas:
- X-ray: small accumulations of calcium are detected in the pancreatic ducts;
- Ultrasound: in 70% of patients, an increase in tissue density, uneven outlines, changes in size, and deformed ducts are detected;
- computed tomography: useful for pseudotumor and cystic forms of the disease and for diagnosing a malignant tumor;
- MRI: helps in diagnosing fibrosis of the gland, that is, diffuse growth of connective tissue in it;
- magnetic resonance cholangiopancreatography: a non-invasive method without radiation exposure, which allows you to create a detailed image of the common bile and pancreatic ducts, useful for detecting stones and malformations;
- ERCP (endoscopic retrograde cholangiopancreatography) is a study that includes filling the gland ducts with contrast through an endoscope and a thin catheter inserted into the duodenum; indicated only in severe cases of the disease and suspected cancer;
- endoscopic ultrasonography is a modern ultrasound method in combination with endoscopy, informative for the diagnosis of small stones and tumors;
- EGDS - endoscopic examination of the esophagus, stomach and duodenum to identify concomitant diseases - reflux esophagitis, peptic ulcer, duodenitis;
- angiography - the introduction of contrast to study the vascular network of an organ, usually performed with simultaneous enlargement of the spleen to exclude portal hypertension.
Treatment of pancreatitis
The main treatment for chronic pancreatitis is diet and giving up bad habits, lifestyle changes, as well as medications:
- drugs that reduce the production of hydrochloric acid by the stomach (proton pump inhibitors)
- enzyme preparations
- antispasmodics
- in the presence of pain - analgesics, NSAIDs; if the pain is extremely severe and is not eliminated by these drugs, narcotic analgesics are prescribed.
It is necessary to identify during the initial examination the pathology of other organs of the gastrointestinal tract (cholelithiasis, chronic cholecystitis, gastritis, duodenitis, peptic ulcer, hepatitis, bacterial overgrowth syndrome, intestinal dysbiosis, kidney disease, etc.), since these diseases may be the cause and/or aggravating factors of chronic pancreatic inflammation. In this case, treatment of other gastrointestinal diseases is necessary. The decision on the urgency and procedure for treating a particular concomitant disease is made by the attending physician.
If medications taken by a patient for other diseases may contribute to the development of the disease, the issue of replacing medications is decided.
All types of drug therapy should be prescribed and monitored by a gastroenterologist.
If any mechanical obstruction to the outflow of bile is detected, surgical treatment is indicated for the patient.
Other medications for pancreatitis
Depending on the form and phase of the disease in each individual case, based on symptoms and test results, the doctor prescribes additional medications.
Antibiotics
To combat inflammation and pus, as well as to prevent serious consequences in the form of necrosis, sepsis and abscess, antibiotics and antimicrobial agents are needed. The duration of the course usually does not exceed 7–14 days. Carbapenems, cephalosporins, fluoroquinolones, and metronidazole are usually used. In the hospital, such drugs are administered parenterally (intramuscularly or intravenously).
Vitamins
Digestive insufficiency is usually accompanied by a lack of vitamins. Before prescribing vitamin preparations, doctors always send for analysis to find out which vitamins are missing. As a rule, fat-soluble vitamins A, D, E and K are prescribed, since they are responsible for the metabolism of proteins, fats and carbohydrates. They also help enzymes function and protect against pancreatic cancer.
Anti-inflammatory drugs for pancreatitis
In addition to antibiotics, doctors prescribe non-steroidal anti-inflammatory drugs and analgesics. In particular, non-narcotic analgesics (diclofenac, piroxicam, meloxicam, metamizole sodium, etc.). They relieve inflammation and pain.
Is it possible to take choleretic drugs?
Gallstone disease is one of the main causes of pancreatitis. Therefore, choleretic substances, which help prevent stagnation of bile and reduce the load on the pancreas, are on the list of drugs to combat this disease. It must be borne in mind that in acute pancreatitis and exacerbation of the chronic form, choleretic drugs are contraindicated. They are taken only during the period of remission.
Iron supplements
The use of iron supplements in the treatment of pancreatitis is not common practice. In some cases, taking enzyme preparations can lead to a deterioration in the absorption of iron and, consequently, its deficiency in the body. According to other data, the consumption of iron supplements by patients after acute pancreatitis affected carbohydrate metabolism.
Preparations for restoring intestinal microflora
In addition to the basic treatment complex, bifidobacteria and lactobacilli are prescribed. They are designed to restore microflora especially after taking antibiotics. Such drugs are the prevention of dysbiosis, in which the microbial composition of the intestine is disrupted.
What drops are falling
Infusion solutions are prescribed in the form of droppers. This therapy is aimed at maintaining water and electrolyte composition. This includes colloidal and crystalline solutions. They replenish lost energy, protein and plasma.
Plasmapheresis
Plasmapheresis is used to cleanse the body of toxins. During this procedure, blood is taken, the patient's plasma, which contains toxins, is filtered, and donor plasma is returned.
Forecast
Chronic pancreatitis is a serious disease. However, if you follow the recommendations of the supervising physician for the prevention of exacerbations (compliance with dietary recommendations, preventive courses of treatment, etc.), chronic pancreatitis proceeds “calmly”, without frequent exacerbations and has a favorable survival prognosis.
If the diet is violated, alcohol intake, smoking and inadequate treatment, degenerative processes in the gland tissue progress and severe complications develop, many of which require surgical intervention and can be fatal.
Classification and types
Many classifications of pancreatitis have been created according to various criteria.
In accordance with the international classification of diseases, there are:
- acute pancreatitis (ICD-10 code K85);
- chronic pancreatitis of alcoholic origin (ICD-10 code K86.0);
- other chronic pancreatitis (ICD-10 code K86.1).
Variants of acute pancreatitis:
- edematous with rapidly developing dysfunction of the gland;
- necrotic (pancreatic necrosis) - a more severe form, accompanied by the breakdown of organ tissue under the influence of its own enzymes.
Types of chronic inflammatory process of the pancreas:
| Variety | Cause | Peculiarities |
| Calcifying (calcifying) | Alcohol consumption | Chronic damage to the smallest pancreatic ducts causes the formation of plugs in them, which gradually calcify |
| Obstructive | Gallstone disease, tumor, scar deformity | Occurs when large ducts are compressed; cells are damaged secondary to increased intraductal pressure |
| Parenchymal-fibrous | Autoimmune process, recurrent inflammation | Rarely occurs, accompanied by widespread damage to glandular cells |
Chronic pancreatitis can be asymptomatic, but more often there is an alternation of remissions and exacerbations. During remission the patient has no complaints. Exacerbation of the chronic inflammatory process is accompanied by the appearance of symptoms of the disease.
Prevention and recommendations
Prevention is based on eliminating risk factors that provoke the disease:
- timely treatment of diseases that provoke pancreatitis
- eliminating the possibility of chronic intoxication that contributes to the development of this disease (industrial, as well as alcoholism)
- ensuring a balanced diet and daily routine.
Nutrition for chronic pancreatitis
For pancreatitis, all dishes are made from lean meat and fish - and then only in the boiled version. Fried foods are prohibited. You can consume dairy products with a minimum percentage of fat content. It is advisable to drink only natural juices, compotes and tea from liquids.
The following should be completely excluded:
- all types of alcohol, sweet (grape juice) and carbonated drinks, cocoa, coffee
- fried foods
- meat, fish, mushroom broths
- pork, lamb, goose, duck
- smoked meats, canned food, sausages
- pickles, marinades, spices, mushrooms
- white cabbage, sorrel, spinach, lettuce, radishes, turnips, onions, rutabaga, legumes, raw ungrated vegetables and fruits, cranberries
- pastries, black bread
- confectionery, chocolate, ice cream, jam, creams
- lard, cooking fats
- cold food and drinks
A qualified nutritionist will help you think through the basics of nutrition for chronic pancreatitis, create a diet and take into account the wishes and habits of the patient.
Features of taking medications for pancreatitis
For pancreatitis, any self-medication is strictly contraindicated, even taking painkillers. The doctor determines the method of treatment, selects medications and their dosage strictly individually for each patient. The duration of treatment depends on the form of the disease, its severity, as well as on the patient’s body’s response to a particular drug. It is important not to forget about the medicine: take medications regularly and at the strictly designated time.
Photo: pressfoto / freepik.com
FAQ
Does the pancreas die in chronic pancreatitis?
Chronic pancreatitis is a disease characterized by inflammation and dystrophy with subsequent development of connective tissue in the organ and disruption of digestive and endocrine function. The “death” of the gland is called pancreatic necrosis and occurs in acute pancreatitis, being a deadly condition
Why does pancreatitis develop if I don’t drink?
Indeed, in most cases, the development of pancreatitis is caused by the effect of alcohol, but there are other factors: cholelithiasis, liver diseases characterized by impaired formation and outflow of bile, diseases of the stomach and duodenum, heredity, a malfunction in the immune system, impaired blood supply to the organ, background diseases: viral hepatitis, hemochromatosis, cystic fibrosis, etc.
Can pancreatitis be cured?
Chronic pancreatitis is called chronic because it cannot be completely cured, but correct medical tactics can achieve long-term remission.
Can pancreatitis lead to the development of diabetes?
Yes, a long course of pancreatitis can lead to the development of not only a violation of the digestive function of the pancreas, but also a change in the endocrine function with the development of diabetes mellitus, especially in the presence of a hereditary predisposition to diabetes mellitus.
Is it important to follow a diet for pancreatitis?
Diet is a fundamental factor in achieving remission.
Pathogenesis of the disease
Inflammatory phenomena in the pancreas gradually lead to degenerative changes in its structure, tissue sclerosis and obliteration of the ductal system. This process usually occurs in waves. The exacerbation is replaced by remission, instead of the glandular tissue that produces enzymes, connective tissue appears. Gradually, enzymes become insufficient; first of all, the exocrine function of the pancreas (production of digestive enzymes) decreases, and then the endocrine function (decreased insulin production).
Symptoms of pancreatic enzymatic insufficiency appear when normal pancreatic tissue is damaged by 90%.
Triad of symptoms of chronic pancreatitis
- pancreatic calcification;
- diabetes;
- steatorrhea is characteristic of an advanced stage of the disease. Steatorrhea occurs when lipase production by the pancreas falls below 16% of its normal level.
Impaired processing and absorption of nutrients in chronic pancreatitis leads to poor absorption of proteins, fats and vitamins. As a result, exhaustion, asthenia, and metabolic disorders of bone tissue and the blood coagulation system may develop.
Treatment stories
Story No. 1
Patient X., 52 years old, came to the EXPERT Clinic with complaints of girdling pain after eating fatty foods and a small amount of alcohol, nausea, and loose stools. From the anamnesis it is known that discomfort in the area above the navel with loose stools was observed for several years due to dietary errors, but after following a strict diet they disappeared without a trace. The woman was not examined for this reason. This is the first time that real complaints have arisen. In addition, 20 years ago, during pregnancy, the patient was told about the presence of thick bile on ultrasound. The patient was not examined further, as nothing bothered her. During a laboratory and instrumental examination, changes in blood tests were revealed: increased ESR, pancreatic amylase activity, and ultrasound revealed multiple stones in the gall bladder. After pain relief, the patient was referred for planned surgical treatment - removal of the gallbladder. After a successful operation, the patient continues to be monitored by a gastroenterologist, follows dietary recommendations, has no complaints, and her indicators have returned to normal.
Story No. 2
Patient B., 56 years old, applied to the EXPERT Clinic with complaints of periodic intense pain syndrome of a shingles nature for no apparent reason, accompanied by nausea and diarrhea. At the previous stage of the examination, diffuse changes in the structure of the pancreas were identified, which was regarded as chronic pancreatitis. The patient led a healthy lifestyle, did not drink alcohol or fatty foods. The prescribed treatment with enzyme preparations did not have a significant effect. When trying to find out the cause of the development of pancreatitis, the gastroenterologist at the EXPERT Clinic ruled out a number of diseases that could lead to the development of chronic pancreatitis (gastrointestinal tract disease, peptic ulcer, iron metabolism disorder, etc.) and drew attention to an immunological shift in laboratory tests. This served as the basis for an in-depth immunological examination, which made it possible to establish that the cause of damage to the pancreas was a malfunction of the immune system - autoimmune pancreatitis. A pathogenetic treatment was prescribed that influenced the mechanism of development of the disease - glucocorticosteroids according to a regimen, against the background of which, during a control examination, the signs of immune inflammation were eliminated. Currently, the patient is receiving long-term maintenance therapy under the supervision of a supervisor and has no complaints. During control ultrasound of the abdominal organs, no signs of pancreatic edema were detected.
Symptoms
The leading symptom of pancreatitis is pain in the upper abdomen of varying intensity. It may appear suddenly or develop gradually. Often this symptom appears some time after eating or drinking alcohol.
Signs of acute inflammation of the gland:
- sudden pain in the upper abdomen radiating to the lower back, interscapular region;
- severe nausea and persistent vomiting;
- increased pain after eating;
- sensitivity of the abdominal wall to touch;
- fever, chills, feeling unwell, weakness.
Symptoms of chronic pancreatitis:
- intermittent pain in the upper abdomen, intensifying 2 to 6 hours after eating; after drinking alcohol, an attack of pancreatitis may develop within 2 to 3 days;
- gradual weight loss, first caused by a decrease in food intake due to fear of pain, and then associated with a deterioration in the absorption of nutrients;
- oily stool with an unpleasant odor associated with the release of undigested proteins and fats.
When 80% of glandular cells are destroyed, secondary diabetes mellitus develops.
Prevention
The main way to prevent pancreatitis in adults is to limit the consumption of alcoholic beverages. To prevent illness in children, proper nutrition is recommended, limiting irritating foods, fast food, and preventing injuries.
Secondary prevention, that is, prevention of relapses, exacerbations and complications, includes:
- refusal to drink alcohol;
- treatment of cholecystitis, cholelithiasis;
- constant use of enzyme preparations and diet.
If such conditions are met, pancreatitis does not lead to serious consequences, and its prognosis for life is favorable.
Important: before use, read the instructions or consult your doctor.
Toxic (drug-induced) pancreatitis
Drug-induced pancreatitis occurs in less than 5% of cases. The prognosis for this pancreatitis is generally good and the mortality rate is low. The pathogenetic mechanism of drug-induced pancreatitis includes:
- immunological reactions (6-mercaptopurine, aminosalicylates, sulfonamides);
- direct toxic effects (diuretics, sulfonamides);
- accumulation of toxic metabolites (valproic acid, didanosine, pentamidine, tetracycline), ischemia (diuretics, estrogens);
- increased viscosity of pancreatic juice (diuretics and steroids).
Demonstrating interactions between pancreatitis and drugs is usually difficult. Pancreatitis may develop within a few weeks of starting treatment. Rash and eosinophilia may occur. Meanwhile, patients taking valproic acid, pentamidine or didanosine do not develop pancreatitis until many months later due to chronic accumulation of the drug's metabolite.
When restarting treatment, patients should be closely monitored. If symptoms recur, the drug should be discontinued.
What else is important to know about enzyme preparations?
The minimum starting dosage is Creon® 25,000 units, which is stated in Russian recommendations for the treatment of chronic pancreatitis and exocrine pancreatic insufficiency2,5. The number indicates the amount of the enzyme lipase, which helps digest fats. If necessary, the doctor can increase the dosage; in European practice, the required dose per single dose can reach up to 80,000 units8. By comparison, the pancreas of a healthy person produces up to 720,000 of these units during each meal9.
Therapy should be taken seriously, since high-quality “nutrition” of the body is the key to its functioning. How long can a person live without energy from food? With chronic pancreatitis, the body must be supplied with enzymes at every meal, even with a snack. Thus, in accordance with the instructions for the drug Creon®, a full dose is required for a meal (for example, 25,000 units), and half for a snack. Creon® capsules are convenient to use: you can open them and add minimicrospheres to food, thereby selecting the desired dose10. More information about the admission rules can be found here.
Treatment
Inflammation of the pancreas can be caused by different reasons, have different symptoms and treatment. To find out how to treat pancreatitis in each case, you need to be examined by a gastroenterologist.
Diet
All patients with pancreatitis are prescribed therapeutic nutrition.
During an exacerbation, it is recommended to abstain from food for 1–2 days, then gradually introduce unsweetened tea, crackers, liquid porridge with water, cream soup, and omelet.
During remission, it is useful to limit the content of fats and carbohydrates in the diet. Preference is given to baked or steamed dishes. You need to eat warm food 6 times a day.
Healthy foods:
- lean meat, poultry, fish;
- oatmeal;
- omelette;
- soy products;
- potato.
What foods should be excluded for pancreatitis:
- causing bloating (brown bread, legumes, grapes);
- containing coarse fiber (raw vegetables and fruits, whole grain cereals);
- stimulating the production of digestive enzymes (rich soups, fried foods, spices, herbs, smoked, salty foods).
Treatment of acute pancreatitis
Acute pancreatitis requires hospitalization. Treatment is often carried out in the intensive care unit. Intensive infusion therapy (intravenous administration of solutions to relieve intoxication) and pain relief are carried out. The duration of the attack is several days.
In the necrotic form, a surgical operation is performed to remove dead tissue. If the attack is caused by gallstones, surgeons remove the gallbladder. As a result, inflammation of the pancreas subsides.
Treatment of chronic pancreatitis
Therapy uses drugs that replace the enzymatic function of the gland. Micrasim is a modern medicine containing pancreatin. This substance replaces the missing enzymes - lipase, amylase, protease. Protecting drug microparticles from the acidic environment of the stomach allows the drug to quickly penetrate the duodenum. Enzyme therapy is carried out over a long period of time, which allows the body to absorb nutrients normally. At the same time, the patient must follow a diet and stop drinking alcohol.
When an exacerbation of pancreatitis develops, drugs that inhibit pancreatic function are prescribed.
If the disease is associated with obstruction of the excretory ducts of the gland, surgical intervention may be required to eliminate it. Indications for surgery for chronic pancreatitis:
- constant, unrelieved pain;
- pseudocyst or blockage of the common bile duct that is not amenable to endoscopic treatment;
- suspicion of gland cancer;
- constant vomiting, persistent weight loss.