Read about the diagnosis and treatment of cholelithiasis at the link.
Get help right away if you develop signs and symptoms of a serious complication related to gallstones, such as:
- Abdominal pain is so severe that you cannot sit still or find a comfortable position
- Yellowing of the skin and whites of the eyes (jaundice)
- High temperature with chills
Number to call an ambulance in Moscow – 103
Prevalence of the disease
Every decade, the number of patients with cholelithiasis is steadily growing. Since the middle of the last century, the number has doubled every ten years. Currently, more than 10% of the world's population suffers from this pathology. In our country, the disease has been diagnosed in 15 million patients; in the United States, more than 30 million patients are registered. Most often, residents of developed countries are susceptible to the disease, and the risk of the disease increases with age. Among people over 45 years of age, every third person develops the disease. The number of operations performed for cholelithiasis in America in the 70s of the last century exceeded 250 thousand; in the 80s, over 400 thousand were performed. By the end of the century, the number of operated patients had already reached 500 thousand. As you can see, the incidence rate is steadily increasing and today in America the number of surgical interventions on the biliary tract and cholecystectomies reaches 1.5 million cases annually; this figure exceeds data for all other abdominal operations, including appendectomy.
Dietary recommendations
- Sugar is a source of endogenous cholesterol and should be avoided.
- Increase your intake of proteins balanced in amino acid composition.
- Increase your intake of plant proteins: oatmeal and buckwheat, seaweed.
- Accustom yourself to regularly eating plant fibers.
- Avoid eating legumes, animal fats, and coffee.
- Skipping breakfast increases the risk of developing gallstones.
- Vitamins E and C reduce the likelihood of gallstone formation.
Unfortunately, in order to forget about gallstone disease in later stages, it is not enough just to follow the correct regimen and diet. Any doctor will tell you that “this is only an additional therapy, not the main treatment.”
Causes
Rice. 1. Pathological anatomy of the biliary tract in cholelithiasis - stones in the gallbladder and obstruction of the cystic duct by one of them (diagram).
Rice. 2. Stages of laparoscopic cholecystectomy - clipping of the cystic duct and artery.
Rice. 3. Stage of laparoscopic cholecystectomy - intersection of the artery and duct and isolation of the gallbladder from the liver bed.
Rice. 4. View of the anterior abdominal wall during open cholecystectomy - suture after laparotomy.
Rice. 5. View of the anterior abdominal wall during laparoscopic cholecystectomy - 4 punctures.
Unfavorable factors that can provoke the appearance of gallstone disease include:
- age;
- overweight;
- pregnancy and childbirth;
- abuse of low-calorie diets, hunger, parenteral nutrition;
- use of certain medications (postmenopausal estrogens, contraceptive steroids, ceftriaxone, fibrate derivatives, octreotide and analogues, etc.)
- heredity (predominance of lithogenic genes, enzymatic defect in the synthesis of solubilizers, cholesterol excretion)
- Crohn's disease, diabetes mellitus, liver cirrhosis, duodenal, choledochal diverticula, infectious diseases of the biliary system, etc.
It should be noted that women are much more common among patients. In addition, there are so-called controllable factors: excess weight, the use of various low-calorie diets in order to reduce weight. For example, in obese individuals, the disease occurs in 33%. Studies conducted in the USA have confirmed that women whose body mass index (BMI) is 25-29 are more likely to get sick. The situation is aggravated by the presence of various diseases (diabetes, coronary heart disease, hypertension). As BMI increases, the likelihood of developing gallstone disease increases. So in women with a BMI above 35, the risk of developing cholelithiasis increases 20 times. It should be noted that low-calorie diets, as well as sudden weight loss (loss of body weight by 1.5 kg per week), weight loss of more than 24% of the initial weight, increase the risk of developing cholelithiasis.
In addition, the biochemical composition of bile is of great importance. Oversaturation with cholesterol, the state of the pronucleating and antinucleating systems, the formation of a crystallization nucleus, and other indicators are very important in the process of stone formation. In addition, a decrease in evacuation function and dysfunction of the enterohepatic circulation of bile acid should be taken into account. The formation of cholesterol stones is based on the hepatic secretion of vesicles that are enriched with cholesterol. However, neither the mechanism of vesicle development itself nor the factors that influence this process are currently not well understood.
How are the bile ducts arranged and how do they work?
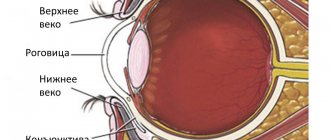
The bile ducts are a system of ducts that originate from hepatocytes and gradually gather into interlobular, segmental and right and left lobar ducts, which unite into the common hepatic duct.
One of the stages of bile removal is its accumulation in the reservoir - the gallbladder. The main function of the gallbladder is to concentrate bile and release it into the lumen of the duodenum during digestion. The volume of this organ is about 80 ml.
The gallbladder is located on the lower surface of the liver. It is a hollow muscular organ, externally covered with a serous membrane and internally lined with mucous membrane. The structure of the gallbladder is divided into the bottom, body and neck of the bladder, which passes into the cystic duct.
Clinical picture and symptoms of the disease
Most often, the first sign that forces the patient to see a doctor is pain in the right hypochondrium, of varying intensity. Cutting or stabbing in nature, the pain is most often constant, often radiating to the right shoulder blade, lower back, and forearm. In some cases (with cholecystocoronary Botkin's symptom), it can radiate beyond the sternum, resembling an attack of angina. It should be borne in mind that the intensity of pain is in no way an indicator of the severity of the process. For example, in some cases, severe pain may disappear, but mild pain does not mean a mild form of the disease.
Often the patient’s condition worsens after eating spicy or fatty foods; their consumption increases the need for bile to process food, which leads to contraction of the gallbladder. In any form of the disease, there is an increase in body temperature. In the form of short rises, the temperature rises to 37-38°C, and the patient often experiences pain. However, during an acute attack accompanied by chills, the temperature can rise to 38-40°C.
How are gallstones formed?
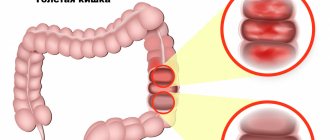
The process of stone formation is quite well studied. The key links are:
- An increase in the lithogenicity of bile (the ability to form stones) means an increase in the content of cholesterol and bilirubin in it.
- Impaired contractile function of the gallbladder.
- Increased pressure in the bile duct system.
Mucin is a natural gel, constantly secreted by the wall of the gallbladder; when lithogenicity increases, it begins to “absorb” cholesterol crystals, thereby forming a “fossilization nucleus.” The formed suspension, with impaired contractile function, continues to attach salt crystals encrusted with calcium salts. Thus, gallstones can grow up to 5-7 mm per year.
Diagnostics
The diagnosis is based on the results of instrumental studies and anamnesis data.
- Ultrasound examination (ultrasound) of the upper abdominal cavity is performed to diagnose cholelithiasis and calculous cholecystitis. During the study, in addition to stones in the gall bladder or ducts, the size of the gallbladder, the condition of its walls, and pathology of the liver or pancreas are determined.
- gastroduodenoscopy - allows you to determine diseases of the stomach, esophagus and duodenum.
- retrograde cholangiography (x-ray examination using a contrast agent) is performed in the presence of complications.
- transgastric ultrasound of the ducts is necessary when diagnosing choledocholithiasis.
Consequences of choledocholithiasis
After treatment and following the doctor’s recommendations, the patient quickly returns to his normal life. However, if you do not seek medical help promptly, complications may arise.
- The presence of stones provokes inflammatory processes that are severe and painful.
- Since the bile and pancreatic ducts connect before entering the duodenum, if the mouth is blocked by a stone, the ducts become swollen and damage to the pancreas is possible. Acute pancreatitis can result in the death of the patient.
- Communicating with the liver, the inflamed biliary system disrupts the functional activity of this organ (and the liver participates in digestion, hematopoiesis, deposits necessary substances, utilizes and deactivates unnecessary ones, and so on). As a result, there is an imbalance in the functioning of almost all body systems.
Conservative methods of therapy
To identify cholelithiasis, determine the degree of inflammation in the wall of the gallbladder, as well as select the correct individual tactics for surgical treatment, you can send me a complete description of an ultrasound of the abdominal organs, preferably a gastroscopy, to my personal email address, you must indicate your age and main complaints. In rare cases, if stones in the ducts are suspected, it is necessary to perform an endoscopic ultrasound examination of the ducts and pancreas. If I provide the above research, I will be able to advise you by email.
In the absence of pronounced manifestations, or in case of a single attack of biliary colic, conservative treatment is carried out aimed at reducing inflammation, improving the motility of the bile ducts and bladder, and the outflow of bile. In addition, it is necessary to correct metabolic processes, as well as eliminate concomitant diseases. However, the tactics of therapy depend on the phase of the process, whether it is an exacerbation, biliary colic or remission. The patient can receive treatment either on an outpatient basis or in a hospital (therapeutic department or surgery). During the period of remission, patients are recommended drug therapy, diet, physiotherapy, and sanatorium-resort treatment is also indicated.
For repeated attacks of biliary colic, which are accompanied by pain, surgical methods for the treatment of cholelithiasis are recommended - only in this way can the development of complications be prevented: peritonitis when the gallbladder ruptures, the development of obstructive jaundice and biliary pancreatitis when the stone enters the hepatic duct, which will lead to obstruction of the biliary tract .
Some categories of patients use traditional medicine methods in the treatment of cholelithiasis. As a result, according to the patients themselves, stones come out of the gallbladder with feces. However, the opening of the sphincter of Oddi, which separates the small intestine from the common bile duct, is no more than 3 mm in diameter. In this case, stones visible to the naked eye simply cannot enter the intestinal lumen. In fact, the patient may find “stones,” which are nothing more than clots of bile that enter the intestines in large quantities. Stone-like formations the size of a walnut, greenish-yellow in color can come out under the influence of various choleretic agents: decoctions and infusions of St. John's wort, flaxseed, immortelle flowers, dandelion root, stelina, peppermint, trefoil, etc. Thus, folk remedies have only a choleretic effect, but the stones are still in the patient’s gall bladder. It should be borne in mind that uncontrolled use of folk remedies can lead to undesirable consequences. Thus, as a result of increased peristalsis, stones in the gallbladder can move, blocking the duct, which will lead to edema, the development of an attack of acute cholecystitis, which, in turn, will cause obstructive jaundice and the development of acute pancreatitis.
In cases where the inflammatory process is pronounced, as well as with long-term stones, with the development of reactive changes in organs located nearby (duodenitis, pancreatitis, cholangitis, hepatitis), as well as with stone obstruction of the neck of the gallbladder, conservative treatment may be useless.
How does the liver work?
The liver is the largest gland in humans. It is located in the upper floor of the abdominal cavity on the right. It consists of two main lobes - right and left, which in turn are divided into 8 segments.
In an adult, it weighs about 1/40 of the total body weight (approximately 1.6 kg in men and 1.2 kg in women). The liver has a dual blood supply: approximately 80% of the blood entering the liver comes from the portal vein (venous blood collected from all unpaired abdominal organs), the rest (oxygenated arterial blood) comes from the hepatic artery. Having entered the portal of the liver, both vessels give rise to multiple branching smaller vessels. At the exit from the liver, 3-4 hepatic veins are formed, which flow into the inferior vena cava.
The main structural unit of the liver is the hepatic lobule, which consists of liver cells - hepatocytes. This cell is one of the most important biochemical laboratories of the body. The hepatocyte takes part in the metabolism of proteins, carbohydrates, fats, bile acids, and vitamins. Neutralizes toxic substances coming from the intestines, followed by the release of associated products into the intestinal lumen. An important function of the hepatocyte is the synthesis of bile, which is involved in digestion.
Surgical methods of treatment
Today there are two main methods of surgical treatment for cholelithiasis:
- Laparoscopic cholecystectomy
- with this method, the intervention is performed using laparoscopic equipment through small incisions on the anterior wall of the peritoneum, through a puncture in the umbilical area or transvaginally. Today, laparoscopy is recognized as the “gold” standard in abdominal surgery. Among the advantages of this method, it is worth noting the excellent cosmetic result: only small incisions remain on the skin. The rehabilitation period is much shorter than with traditional surgical treatment. The patient begins to walk on the first day, and on the second day he is allowed to take liquid food. The operated patient usually leaves the clinic on the 2nd or 3rd day after the operation. A person can usually start work within 10-14 days. - Traditional cholecystectomy
is an open operation, performed manually, with a 15-20cm incision made on the anterior abdominal wall. Currently, surgical intervention using this method is performed only for complications of cholelithiasis (peritonitis, gallbladder perforation).
These operations are performed under general anesthesia, and the gallbladder is removed along with the stones according to the same procedure. If there is a single large or several small stones, the gallbladder is completely removed. Some patients ask about the possibility of removing only stones while preserving the gallbladder. It is possible to perform such surgical intervention. However, at this time there is no definite guarantee that the stones will not reappear. Today, specialists from all over the world are working on this problem, but stones often reappear within six months.
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
Transvaginal laparoscopic cholecystectomy using the NOTES method
Rice. 6. Scheme of laparoscopic transvaginal cholecystectomy using NOTES technology
Rice. 7. View of the anterior abdominal wall during laparoscopic cholecystectomy using SILS technology.
Since 2007 in France, and since 2008 in the Russian Federation, a unique method of removing the gallbladder has been practiced - transvaginal cholecystectomy using NOTES technology. The operation is performed without any punctures of the abdominal wall, therefore, there are no postoperative scars. The essence of the surgical intervention is access to the affected organ through a small puncture (1 cm) of the posterior vaginal fornix. The intervention is performed using laparoscopic instruments and optics introduced into the peritoneal cavity through this access. After removing the gallbladder through the same access, one suture is placed on the puncture. The synthetic suture material used in this case dissolves within 3-4 weeks.
The advantages of this method are:
- in the absence of pain after surgery;
- the patient's motor activity is not impaired;
- short rehabilitation period, patient hospitalization lasts only one day;
- excellent cosmetic effect;
After 7-10 days after surgery, a person can begin to work, and they can play sports on the 14th day. Among the restrictions in the postoperative period should be the need to exclude intimate relationships for a month. At the same time, the genital organs (uterus, appendages, etc.) are not affected during transvaginal cholecystectomy, so their functionality remains unchanged.
Single-port laparoscopic cholecystectomy SILS
The use of the NOSE technique is technically impossible in cases where patients have undergone many surgical interventions on the pelvic organs in the past. Therefore, an equally effective method of minimally invasive cholecystectomy was developed, which has been used in America since 2008, and since 2009 such operations have been performed by domestic surgeons. We are talking about removing the gallbladder through a puncture in the navel area (SILS technology).
Single-port laparoscopic cholecystectomy
consists of performing an operation using a special device (port), which is a soft plastic apparatus that is inserted into the abdominal cavity through a puncture. Port diameter 23-24 mm. It is through this that laparoscopic instruments are inserted; the diameter of the laparoscope does not exceed 5 mm. Upon completion of the operation, a cosmetic suture is applied to the small wound. Surgical intervention using SILS technology (single-port surgery), in contrast to conventional laparoscopic access (multi-puncture), has a number of advantages:
- fewer punctures on the abdominal wall;
- less pain after surgery;
- shorter rehabilitation period;
- better cosmetic effect;
The advantages of this method of surgery are especially noticeable when there are multiple stones in the gallbladder - with the usual method, the surgeon must increase the puncture to remove stones and the diseased organ.
The choice of the appropriate surgical treatment method depends on the individual characteristics and health status of the patient. Visiting a clinic with qualified and experienced specialists guarantees the highest possible treatment results.
Why is it important to consult a doctor at the first symptoms?
Since choledocholithiasis often has an asymptomatic course, the onset of the inflammatory process can be missed. Trying to get rid of pain or other symptoms on their own, a person wastes time, and this is absolutely forbidden to do, in order to avoid the development of irreversible processes. This is especially true for patients with a removed gallbladder. Timely diagnosis and treatment ensures a favorable outcome.
The Yusupov Hospital has all the conditions for high-quality diagnostics and treatment. Here you can conduct a preventive examination if you have had a cholecystectomy in the past or if there are cases of cholelithiasis in the family.