Unfortunately, pregnancy does not always proceed without complications. In some cases, for the safety of mother and baby, a woman is offered hospitalization in a maternity hospital or in the pathology department. What can be a reason for hospital treatment?
The diagnosis of “oligohydramnios” usually causes anxiety among expectant mothers. How dangerous is this condition for the baby, how can it affect the course of labor and is it possible to fight it?
General information
What is oligohydramnios in pregnancy (medical term oligohydramnios)?
This is a pathological condition in which the amount of amniotic fluid decreases (less than 500 ml) while the membranes are intact and without signs of water leakage. Amniotic fluid (synonymous with amniotic fluid) surrounds the fetus and is the medium that connects it and the mother’s body. Their main function is to ensure the vital activity of the fetus, nutrition and its development, protection from infections and injuries, and facilitating the movements of the developing fetus. The circulation of amniotic fluid is a training factor for the fetal excretory and respiratory system. Oligohydramnios is regarded as a manifestation of pregnancy , which subsequently affects its outcome. It indirectly indicates congenital anomalies, the presence of intrauterine infection and even fetal death, leading to complications of pregnancy and childbirth, which is why it is an urgent problem in obstetrics. We can say that insufficient amniotic fluid is a woman’s body’s response to any changes in her health or the fetus, which may be associated with infections or endocrine pathology. However, only a decrease in water levels below normal without changes in ultrasound, Dopplerography and cardiotocography is not considered as a marker of fetal pathology. Quite often (20-50% of cases) idiopathic oligohydramnios , when no pathology is detected in the woman or the fetus.
Amniotic fluid appears in the third week and normally its volume changes with the duration of pregnancy: at 10 weeks it is 30 ml, then gradually increases and by 37-38 weeks it reaches 1500 ml, and by the end of the period it decreases again. Typically, at the end of pregnancy, moderate oligohydramnios is physiological and does not pose a danger. Most of the water is secreted by the amniotic sac (part of the placenta); the fetus also secretes up to 500 ml of liquid during its life. If the pregnant woman is healthy, then the placenta produces a normal amount of amniotic fluid for the duration of pregnancy. Its normal volume is an indicator of the proper functioning of the membranes and the fetal urinary system. This pathology can appear in any trimester, but more often develops in the third trimester (by 37-38 weeks), which is associated with the aging of the placenta and a decrease in its function. There are cases of the development of oligohydramnios before the 20th week.
Importance of amniotic fluid
Amniotic fluid (medical name) completely provides everything necessary for the proper development of the unborn child. It contains various vitamins, hormonal compounds, oxygen and salt compounds that are very necessary for the fetus, which are the main building materials for the entire small organism.
Amniotic fluid is not only a nutrient medium for the baby, it also protects it in every possible way from various negative factors, gently reducing physical impacts, and neutralizing infectious attacks. As pregnancy progresses, their number should increase, and their composition should be constantly updated, since the needs of the developing body also grow and change. It is very important that the doctor who monitors the patient’s pregnancy monitors all anomalies and failures that may occur, in particular, a decrease in water. This problem can lead to serious complications during pregnancy.
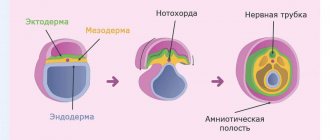
Pathogenesis
The production of amniotic fluid and the maintenance of its volume is a process of formation and absorption that occurs constantly. This process involves the fetal membranes, umbilical cord epithelium, surface of the placenta, lungs, fetal intestines and its urinary system. Up to 5 weeks, water is produced by the chorion , then by the amniotic membrane ; starting from the second trimester, the kidneys (urine) and lungs of the fetus (alveolar fluid) take over the function. The main source of fluid is urine. During a full-term pregnancy, the fetus secretes from 400 to 1200 ml of urine. The lungs of a full-term baby secrete 300–400 ml per day. Amniotic fluid is renewed every three hours, the change of dissolved substances occurs within 5 days.
The volume of liquid is affected by:
- Fetal urination is the main source in the 2nd half of pregnancy, if there are kidney abnormalities, very little amniotic fluid is formed. In a normal full-term pregnancy, the fetus produces 700-900 ml of urine per day.
- Ingestion of water by the fetus. At full term, he swallows 230-750 ml per day.
- Secretion of fluid by the lungs.
- The developed lack of amniotic fluid affects the child - his skin becomes wrinkled and dry, he begins to lag in growth. The walls of the uterus compress it because they fit tightly to the fetal sac, and the fetus itself comes into contact with the amnion. As a result of close contact with the amnion, cords (Simonartian ligaments or constrictions) are formed between the inner surface of the amnion and the fetus. Strands can cause defects or amputation of fingers and, in some cases, amputation of limbs. Club feet and spinal curvature also develop . If Simonart's ligaments compress the umbilical vessels, death occurs.
Classification
Forms of polyhydramnios:
- Early, developing from 16 to 20 weeks and associated with inadequate function of the membranes. May indicate fetal developmental abnormalities.
- Later, detected in the II-III trimester (after 26 weeks). This form develops against the background of maternal diseases, pathology of the placenta and pathology of pregnancy. It may also be caused by partial prenatal rupture of the membranes.
By duration:
- Chronic - forms slowly and progresses. To confirm it, ultrasound and other studies are carried out over a period of 1-2 months. With progression, a final diagnosis is made.
- Acute (transient) - occurs acutely and temporarily, develops after a respiratory infection , sore throat or poisoning . This form is benign and disappears after the pregnant woman recovers.
By severity:
- Mild severity (IAP - amniotic fluid index 5-10 cm).
- Moderate severity (amniotic fluid index 2-5 cm).
- Severe (IAP less than 2 cm).
Moderate oligohydramnios during pregnancy (amniotic fluid is determined in the amount of 400-500 ml) is detected by chance on an ultrasound scan, since moderate oligohydramnios is not accompanied by any objective symptoms. Severe oligohydramnios is diagnosed if the lack of fluid exceeds 700 ml. Severe oligohydramnios is already accompanied by symptoms - pain when the fetus moves, dizziness , nausea or vomiting, and there may be dry mucous membranes.
How does oligohydramnios affect the development of pregnancy and the condition of the fetus? In any trimester, it is associated with risks for the pregnant woman and the fetus. Oligohydramnios during pregnancy 20 weeks is often associated with fetal death. The prolonged presence of oligohydramnios during this period increases the risk of chest abnormalities, underdevelopment of the pulmonary artery and limb deformities. Typically, in this period, oligohydramnios develops after infectious and inflammatory diseases and is combined with placental insufficiency and developmental abnormalities. Pregnant women have a history of cytomegalovirus infection , herpes infection or parainfluenza . If oligohydramnios, inflammation of the placenta and membranes, and embryogenesis disorders are detected, the question of the advisability of continuing the pregnancy is decided.
If oligohydramnios is detected at 32 weeks of pregnancy, it is prolonged. Moderate oligohydramnios at this stage is not dangerous, but to clarify the condition of the fetus, cardiotocography is performed at 32-33 weeks of gestation and monthly ultrasound monitoring. In cases of severe oligohydramnios and increased uterine tone, hospitalization is indicated at 34 weeks. Treatment includes sedatives, antispasmodics, drugs that improve placental blood flow, and, if indicated, hormones . The efforts of doctors are aimed at prolonging pregnancy and maturing the baby, so the pregnant woman is offered hospitalization in order to maintain the pregnancy.
At 36 weeks - 37, the fetus continues to be actively monitored, treatment is prescribed to improve metabolism in the placenta and gas exchange, as well as vitamins. For hypertension, tocolytics are prescribed. If conservative treatment does not produce results, the amount of amniotic fluid continues to decrease, and the condition of the fetus worsens, delivery is recommended regardless of the gestational age. Given the high risk of complications during childbirth, preference is given to caesarean section.
38 or 39 weeks is the period at which a pregnant woman can give birth, so a planned caesarean section . Oligohydramnios at 40 weeks and 41 is associated with post-term pregnancy, since by 40 weeks the amount of water normally decreases to 0.6 l - this is an indication for delivery.
Is it possible to prevent oligohydramnios?
Symptoms, causes, diagnosis, treatment are very important factors, but is it possible to predict the occurrence of a problem in advance and ensure that the woman remains healthy? Unfortunately, such preventive measures do not exist. But there are special rules, following which, you can minimize the development of a variety of pathologies. These include avoiding excessive physical activity and carrying heavy objects.
It is important to pass all tests and undergo timely examinations that help to exclude various ailments that can later cause oligohydramnios during pregnancy. The causes and consequences of past diseases are negative. Therefore, it is better to take measures in advance and undergo a course of treatment that will improve the health of both the expectant mother and the child.
To improve your well-being, you need to eat right. Doctors and nutritionists recommend eating smaller meals, eating food at least five times a day, but in small portions. This will have a beneficial effect on the health of both the woman and the baby.
Causes of oligohydramnios during pregnancy
In most cases, the cause of insufficient amniotic fluid is:
- Underdevelopment of the amniotic epithelium, as a result of which the production of fluid in the required quantity is impaired.
- Damage to the membranes due to infectious and inflammatory diseases: vulvovaginitis , adnexitis , endometritis . When oligohydramnios is detected in pregnant women, a history of chlamydia , trichomoniasis , HPV infection , mycoplasmosis , gonorrhea or syphilis is noted.
- Extragenital pathology of women - chronic kidney disease, collagenosis , cardiovascular diseases.
- Metabolic disorders in a pregnant woman ( obesity , diabetes mellitus ). Women with this pathology constitute a risk group, and insufficient production of amniotic fluid is noted from the first trimester.
- Primary placental insufficiency associated with malformations or infarctions .
- Abnormal attachment, premature detachment, premature aging of the placenta.
- Anomalies in the development of the urinary system in the fetus ( polycystic kidney disease , underdevelopment of the kidneys, various types of atresias and obstructions of the urinary system).
- Delayed fetal development or death, chromosomal pathologies (trisomy 13,21,18).
- Post-term pregnancy, which is the cause in 20-30% of cases. The volume of fluid increases until 36-37 weeks, and then begins to decrease and goes to a minimum during post-term pregnancy.
- Oligohydramnios is often observed in one of the twins if the other develops polyhydramnios at the same time. This is due to the fact that the blood circulating in the common placenta is distributed unevenly.
- The use of non-steroidal anti-inflammatory drugs by a pregnant woman, which increases the risk of kidney pathology in the fetus. In this case, oligohydramnios can develop quickly (within two days of use) or within several weeks from the start of NSAID treatment. Usually this condition is reversible and disappears when the drug is discontinued.
- In 25%, idiopathic oligohydramnios for no apparent reason.
In the first trimester, insufficient water supply is a rare finding, but is associated with an unfavorable prognosis (threat of miscarriage). The reasons for the development of this pathology during this period: heart abnormalities, chromosome number abnormalities, rupture of membranes and intrauterine fetal death. An iatrogenic cause—medical manipulation (chorionic villus biopsy)—cannot be ruled out.
Oligohydramnios in the second trimester is most often associated with obstruction , rupture of membranes, placental abruption and early fetal growth restriction. Sometimes it is possible to detect deviations in the amount of water only in the third trimester: in the prenatal period (37-38 weeks) oligohydramnios is detected in 3%-5% of cases, and in 40-41 weeks - in 5%-11%.
Causes of oligohydramnios in the 3rd trimester of pregnancy:
- premature rupture of membranes;
- intrauterine growth retardation;
- placental abruption;
- Iatrogenic causes (pregnant women taking ACE inhibitors or non-steroidal anti-inflammatory drugs).
Oligohydramnios in the later stages, at 30, 32, 38, 40 weeks
Late moderate and severe oligohydramnios is a pathology during pregnancy, which is characterized by insufficient function of the membranes of the amniotic sac or various disorders during the development and growth of the fetus. It is usually diagnosed in the third trimester of pregnancy, at 32-38 weeks, but can sometimes be detected after 20 weeks.
Oligohydramnios in the first trimester
Oligohydramnios in the early stages of pregnancy indicates serious, life-threatening pathologies of the fetus. Most often, this problem leads to forced or spontaneous termination of pregnancy. One of the serious causes of oligohydramnios is the improper development or functioning of the fetal urinary system. For example, if the child does not have kidneys, the mother develops oligohydramnios before the second trimester of pregnancy. Since a fetus without kidneys will not be viable, the pregnancy must be terminated.
Oligohydramnios in the second trimester
Oligohydramnios is detected more often after 20 weeks of pregnancy than in the early stages. In the period from 18 to 25 weeks, there is still a lot of room in the uterus for the fetus to grow, so the volume of amniotic fluid should be at a sufficient level. With severe oligohydramnios in the second trimester of pregnancy, we can talk about severe intrauterine abnormalities. Oligohydramnios in the second trimester during pregnancy can develop due to clubfoot, deformation of the skull, and intrauterine dislocation of the femur.
Symptoms
Clinical signs of moderate oligohydramnios are not expressed and pathology can only be determined by ultrasound. Signs of severe oligohydramnios include:
- poor fetal movement;
- pain or discomfort when moving;
- lower abdominal pain;
- morning sickness and dry mouth;
- restless sleep;
- weakness and apathy;
- spontaneous miscarriage.
Upon examination, the size of the uterus is insufficient in terms of time, its consistency is dense, the fetus is inactive and its position is incorrect.
Childbirth with oligohydramnios is complicated: contractions are painful and ineffective, there is a slow opening of the cervix, weak labor and fetal hypoxia . Compression by the umbilical cord often results in fetal death during childbirth. When the amniotic sac is opened, a small amount of thick liquid colored by feces is released. Bleeding is often observed in the afterbirth period. Childbirth is carried out with early artificial rupture of the bladder. Fetal cardiac monitoring is performed continuously. oxytocin , methylergometrine is mandatory . When hypoxia begins during labor, delivery by cesarean section is indicated. In newborns there is a decrease in adaptation.
Pregnant women often turn to a forum dedicated to this topic at 32-33 weeks, when oligohydramnios is most often detected, they ask questions and share their experience. Many people report that they always do cardiotocography and if the examination results are poor, then hospitalization is prescribed. If there is significant oligohydramnios and severe fetal growth retardation, then a cesarean section is performed despite the gestational age.
Signs
Moderate oligohydramnios is very rarely accompanied by certain symptoms, but women can still sometimes experience some discomfort. Below they will be discussed in more detail:
1. First of all, pain in the lower abdomen should alert you. 2. Tremors and nausea may occur when the fetus moves. 3. In the second trimester, there is an increase in the child’s activity. If the amniotic sac is deficient in fluid, movements will cause severe discomfort to the mother. 4. The doctor can point out the described problem based on the small size of the uterus, as well as the diameters of the abdominal circumference that do not correspond to the norms. 5. Slight fetal mobility.
Tests and diagnostics
- An external obstetric examination is carried out - the abdominal circumference and the position of the fundus of the uterus are measured. Due to a decrease in amniotic fluid, these indicators are deviated downward, and fetal mobility is limited.
- On vaginal examination, the uterus is toned and the amniotic sac is flat.
- An important study is ultrasound assessment of amniotic fluid. The amniotic fluid index is calculated: the uterine cavity is mentally divided into 4 quadrants and the depth of the amniotic fluid pocket is determined in each. The sum of the values in the four quadrants is the amniotic fluid index. If the pocket depth is less than 2 cm and the index is less than 5 cm, then this indicates oligohydramnios.
- Examination of a pregnant woman for the presence of infections (examination of urine, blood, smears for pathogenic flora, PCR testing for infections).
- Assessment of the length of the cervical canal (determines the risk of premature birth).
- Ultrasound of the fetus, which allows you to determine developmental anomalies.
- Cardiltocography. Assess the condition of the fetus by its heartbeat. The study is carried out only in the third trimester (after 32 weeks).
Diet
Diet 15 table
- Efficacy: therapeutic effect after 2 weeks
- Timing: constantly
- Cost of food: 1600-1800 rubles per week
It goes without saying that during pregnancy, a balanced and healthy diet with sufficient calories, vitamins and minerals, and protein is important. In this regard, a pregnant woman can adhere to dietary Table No. 15 , but increase the content of protein, foods rich in calcium, iron, zinc, omega-3 fatty acids (fatty fish, flaxseed oil, nuts). The positive effect of antioxidants and methionine in the normal development and functioning of the placenta has been proven. Methionine is found in Brazil nuts, milk, meat, fish, powdered eggs, Parmesan cheese, beans, red caviar, beans, almonds, lentils, sesame seeds, and soybeans.
A balanced diet for this pathology is more prevention than treatment, so from the first days of pregnancy a woman should reconsider her diet. Animal fats and simple carbohydrates (sweets, baked goods, confectionery) are significantly limited in the diet.
Medicines
Photo: tvoymalysh.com.ua
The following medications can be used:
- Vasodilators are medications that help expand the lumen of blood vessels. These drugs are necessary to improve uteroplacental blood flow;
- antiplatelet agents - inhibit the aggregation of red blood cells and platelets, reduce their ability to stick together and adhere to the vascular wall. In addition, antiplatelet agents, by reducing the surface tension of red blood cell membranes, facilitate changes in their shape as they pass through capillaries. Capable of not only preventing aggregation, but also causing disaggregation of already aggregated blood platelets;
- Tocolytics are drugs that are used in the presence of uterine hypertonicity. The effect of the drugs is to weaken the contractile activity of the myometrium;
- antibacterial agents - used to treat infectious diseases of bacterial etiology. As a rule, preference is given to broad-spectrum antibiotics, which have an effect on both gram-positive and gram-negative microflora;
- vitamin and mineral complexes, the purpose of which helps to saturate a woman’s body with all the necessary vitamins and minerals, thereby enhancing the body’s protective properties.
Prevention
- Timely registration with a gynecologist and compliance with all doctor’s recommendations (rational nutrition, avoidance of stress and hard work at work).
- Careful monitoring of pregnant women at risk - women with a history of oligohydramnios, urogenital infection, obesity and diabetes.
- Prenatal diagnosis includes early detection of defects of the musculoskeletal and genitourinary systems.
- In case of postterm pregnancy, urgent delivery is indicated.
- The complex of measures for predicting oligohydramnios should include medical genetic consultation.
- If oligohydramnios develops, a pregnant woman should avoid physical activity, eat right and visit a gynecologist.
Can a baby be born healthy?
If treatment for oligohydramnios was started on time, and the child began to feel normal as a result of therapy, pregnancy continues up to 38 weeks. In this case, the woman has every chance of giving birth to a healthy child.
Treatment of pathology that occurs late in pregnancy (in the second or third trimester), especially when the child has problems with intrauterine development, may have an unfavorable outcome. These problems may well cause a serious developmental delay in the baby or even his death.
Is it possible to avoid the condition of amniotic fluid deficiency? Yes, if even at the stage of pregnancy planning the woman is examined for diseases of the internal organs and, if necessary, undergoes their treatment. You should also protect your pregnancy from stressful situations, exclude serious physical activity and the impact of any negative phenomena and factors on the body. It is important to carefully plan your menu and adhere to a balanced diet, including vitamins and microelements.
If oligohydramnios was diagnosed already during pregnancy, then you should carefully listen to all the recommendations of the gynecologist, undergo diagnostic procedures and tests in a timely manner.
Consequences of oligohydramnios during pregnancy and complications
Why is oligohydramnios dangerous? When considering the consequences, it is necessary to indicate the consequences for the mother and for the fetus. For a woman, oligohydramnios is dangerous:
- threat of abortion;
- premature birth;
- anemia;
- premature placental abruption;
- preeclampsia;
- weakness of labor;
- bleeding.
This condition threatens the development of the fetus:
- defects of the musculoskeletal system (congenital pathology of the feet, muscular torticollis , curvature of the spine, various bone deformities);
- genitourinary system (bilateral renal underdevelopment, polycystic kidney disease );
- congenital heart disease ;
- chronic hypoxia ;
- growth retardation.
Treatment regimen for oligohydramnios
The doctor determines how to treat oligohydramnios after a complete examination. In the absence of reasons such as illness, expectant management is chosen, during which the condition of the mother and child is carefully monitored.
If the problem is dehydration of the pregnant woman’s body, it is necessary to increase the amount of fluid consumed per day to 2 liters.
In the presence of congenital fetal defects, treatment of oligohydramnios consists of surgical intervention. After a comprehensive examination, the doctor makes a decision: to perform an operation to artificially terminate the pregnancy or to monitor the further development of the situation.
If the reason for the decrease in water is an infectious lesion, medications with antibacterial or antiviral action are used.
Forecast
The prognosis for this pathology and the outcome of childbirth depend on the severity and time of development. An unfavorable prognosis for the fetus occurs with the development of oligohydramnios in the second trimester, since there is a possibility of the development of multiple anomalies and the possible death of the child. In this regard, it is important to resolve the issue of the possibility of prolonging pregnancy. Prolonging pregnancy is problematic with the development of oligohydramnios at the very beginning of the third trimester and developmental delay. If the condition of the fetus is normal and there is no growth retardation, then with oligohydramnios in the third trimester it is possible to carry the pregnancy to 37-38 weeks and have a favorable birth outcome.
List of sources
- Kaganova M. A, Spiridonova N. V. Analysis of the characteristics of the course of labor and perinatal outcomes in isolated oligohydramnios/Postgraduate Bulletin of the Volga Region. - 2021. - issue 5-6, pp. 39-43.
- Sidorenko V.N., Bugrov V.Yu. Modern view on the etiopathogenesis of oligohydramnios and polyhydramnios, and ways to solve them for polyhydramnios of an infectious nature/Medical news. - 2021. - No. 4. pp. 53-57.
- Voevodin S.M., Shemanaeva T.V., Serova A.V. Modern aspects of the diagnosis and pathogenesis of oligohydramnios/Gynecology. — 2021, VOLUME 19, No. 3
- Alieva L.I., Alieva E.M., Mamedova S.N. Efficacy of complex pathogenetic therapy for pregnant women with oligohydramnios/Medical news. — 2021. — No. 1, pp. 77-79
- Prytkov A.N., Zakharov L.V., Karkusova A.V. The occurrence of congenital malformations of the fetus with pathological content of amniotic fluid in the mother during pregnancy / Medical genetics. - 2004. - No. 11. — P.529-532.