Calcemin Advance
Calcemin Advance is a regulator of calcium and phosphorus metabolism. The role of calcium in the public consciousness is often reduced only to the formation of bone tissue. But these functions in the body are far from being exhausted: calcium regulates the permeability of the walls of blood vessels, the conduction of impulses through neurons, participates in the contractions of skeletal muscles, and is one of the components of the blood coagulation system. Normal absorption of calcium is possible only in the presence of active alkaline phosphatase, the activation of which requires vitamin D. Previously, when creating calcium preparations, pharmacologists could not find the optimal amount of vitamin D, because the latter tends to accumulate in the body, which, in turn, is fraught with hypervitaminosis. Vitamin D hypervitaminosis can cause the development of cardiovascular, nervous and hepatic pathologies. In this regard, clinicians were forced to limit the duration of treatment with drugs containing vitamin D in doses above 400 IU, which reduced the risk of developing hypervitaminosis, but at the same time the effectiveness of pharmacotherapy. The latter had a negative effect on individuals with an increased need for calcium, for example, pregnant women. A solution was found by specialists from the pharmaceutical company SAGMEL. In addition to calcium and vitamin D, their Calcemin Advance also contains zinc, copper, manganese and boron, which also promote better absorption of calcium, which made it possible to reduce the dose of vitamin D without losing the effectiveness of treatment.
Zinc activates more than 200 enzymes, including alkaline phosphatase. Copper takes part in the formation of the structural proteins collagen and elastin, preventing a decrease in bone mineral density. Manganese ensures the normal process of formation of mucopolysaccharides necessary for the formation of bones and cartilage. Boron controls the activity of parathyroid hormone, which is involved in calcium-phosphorus metabolism, magnesium and vitamin D metabolism. Calcemin Advance is indicated for the treatment and prevention of osteoporosis (decreased bone mass), other diseases of the musculoskeletal system associated with impaired calcium-phosphorus metabolism, in adolescence - to eliminate lack of calcium and magnesium. The drug is contraindicated in case of individual intolerance to one or more components, nephrolithiasis, increased calcium concentration in the blood plasma, urinary excretion per day of more than 250 (in women) and 300 (in men) mg of calcium. In pediatrics, Calcemin Advance is used starting from the age of 12. The frequency of administration in adults and children is twice a day. Single dose – 1 tablet. It is not recommended to exceed the dose established by the manufacturer, because Excess calcium can impair the absorption of iron, zinc and other trace elements. During pregnancy and breastfeeding, taking the drug should be agreed with your doctor.
Experience with the use of the drug Calcemin Advance in postmenopausal women with osteopenia
One of the achievements of our time is the increase in life expectancy. But longevity is inevitably associated with an increase in the number of diseases. Among the pathologies whose frequency increases with age are diseases of the cardiovascular system, lungs, and oncology. An important place is occupied by osteoporosis (OP), a systemic skeletal disease characterized by a decrease in bone density, a violation of its structural and qualitative characteristics, accompanied by an increased risk of fractures. A fracture of the proximal femur occurs in 1-2 out of 1000 Russian residents aged 50 years and older, and fractures of the forearm are recorded even more often - in every 100 women of the same age group. A year after suffering a hip fracture, only 15% of patients consider themselves to have fully recovered their health.
Considering the above, it becomes clear that there is a need for the prevention and treatment of AP, an important part of which is adequate intake of calcium and vitamin D, which are necessary to maintain a healthy balance in the bones and prevent fractures. Calcium is one of the main components of bone and cartilage tissue, as well as an element necessary to maintain the osmotic and oncotic pressure of blood plasma. The total calcium content in the human body is approximately 1.9% of the total weight of a person, with 99% of all calcium occurring in the skeleton in the composition of microcrystals of carbonate apatite and hydroxyapatite, and only 1% is found in other organs and tissues. Calcium affects the permeability of biological membranes, participates in the regulation of metabolism in cells, and is an important factor in blood clotting.
In addition, calcium is an important cofactor for a number of cytoplasmic, tissue and organ-specific enzymes (for example, for all isoforms of alpha-amylase, pancreatic lipase and other enzymes), and in this role it takes an active part in metabolic processes, regulation of neuromuscular conduction and secretory activity of the stomach, and can also have a significant impact on the functional activity of most organs and systems.
Calcium intake rates vary at different periods of a person's life. Calcium intake in children should continually increase with age, since increased calcium intake during adolescence is associated with increased peak bone mass. A 10% increase in peak bone mass reduces the lifetime risk of osteoporotic fractures in adults by 50%.
The next important stages, when an increase in calcium intake to 1200-1500 mg per day is again required, are periods of pregnancy, lactation, and the onset of menopause in women. However, as previous studies have shown, calcium intake from food among women aged 50 years and older is insufficient, so additional medications are required to ensure adequate levels of calcium intake.
The main regulator of the active absorption of calcium in the body is the active metabolite of vitamin D - calcitriol. Under physiological conditions, the level of intestinal absorption of calcium does not exceed 20-30%, the use of vitamin D increases it to 60-80%. After being absorbed into the blood, calcium is distributed among systems and organs, primarily entering the bones, where it participates in the mineralization process, as well as the kidneys. Under physiological conditions, calcium excretion from the body is approximately 250-300 mg/day. In children and adolescents, the transport and utilization of calcium in the bones is 2-3 times higher than in adults, which is due to the active formation of the skeleton and bone growth. In healthy adults, the process of bone formation and resorption is balanced. In old age, due to increased resorption processes against the background of the development of vitamin D deficiency, this balance is disturbed and the removal of calcium from the bone often exceeds its entry into the skeleton. It is known that a lack of vitamin D can lead to secondary hyperparathyroidism, which, in turn, increases bone turnover, which entails increased bone loss. The concentration of 25(OH)D in the blood, which is one of the best clinical indicators of sufficient intake of vitamin D in the body, should ideally be at least 50 nmol/l, but, as research results show, vitamin D insufficiency and deficiency occur in almost all populations regardless of the time of year.
Numerous studies have shown that calcium and/or vitamin D supplementation reduces bone loss and fracture rates among postmenopausal women. In studies aimed at studying the effect of calcium and vitamin D therapy on reducing the incidence of fractures, a significant reduction in the risk of hip fracture was found by 18% [(RR 0.82 (95% CI 0.71-0.94), p = 0, 0005] and the risk of non-vertebral fractures by 12% [(RR 0.88 (95% CI 0.78-0.99), p=0.036] in groups receiving combination therapy compared with groups without treatment. In studies where Vitamin D supplementation of 700-800 IU per day had a greater effect on hip fracture risk than 400 IU (21% and 18%, respectively).In studies in which patients received vitamin D alone or placebo (4 RCTs with a total of of 9083 patients), there was no reduction in the risk of non-vertebral fractures: both when using a dose of 400 IU (RR 1.14 [95% CI 0.87-1.49]) and when using 700-800 IU (RR 1. 04 [95% CI 0.75-1.46]), which confirms previously reported data that vitamin D without added calcium does not reduce the risk of fractures. Combining calcium with vitamin D reduces the risk of fractures only in the case of 75-80% compliance patients.
Currently, calcium preparations are widely used for the prevention of AP - single preparations or combined with vitamin D. However, in Russia, doctors also have at their disposal complex calcium preparations, which are a combination of calcium and vitamin D with individual microelements. One of these drugs is Calcemin Advance, which, in addition to calcium (in the form of carbonate and citrate), includes magnesium, zinc, copper, manganese and boron.
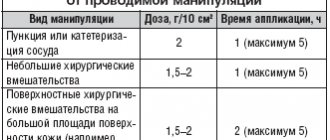
An open clinical trial was conducted at the Research Institute of Rheumatology of the Russian Academy of Medical Sciences to evaluate the effectiveness and tolerability of the complex drug Calcemin Advance for osteopenia in postmenopausal women. 100 women aged 45-65 years with osteopenia in the spine and/or femoral neck were examined. The patients were randomly divided into 2 groups: Group I - 50 people received Calcemin Advance (1 tablet 2 times a day, which amounted to 1000 mg of calcium per day, 400 IU of cholecalciferol, 80 mg of magnesium, 15 mg of zinc, 2 mg of copper, 3 .6 mg manganese and 500 µg boron); Group II (control) – 50 women who did not receive drug treatment, who were given nutritional recommendations.
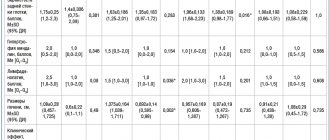
Patients of the 2 groups were comparable in age, height, weight, body mass index, duration of the reproductive period, age at menopause and duration of the postmenopausal period, BMD indicators in the lumbar spine and proximal femur. There were significant differences in the intensity of pain in the lumbar spine. Thus, in the group that subsequently received the drug, more pronounced pain syndromes were noted. In both groups, there was an insufficient daily intake of calcium from food, the deficiency of which reached 65% of the recommended standards for postmenopausal women, while no differences were found between the groups in this indicator. There were no significant differences in the state of calcium-phosphorus metabolism in both groups and in the indicators of markers of bone resorption and formation. The duration of the study was 12 months.
The main end point of the study was the dynamics of BMD during densitometric examination: analysis of BMD after 12 months of observation showed that in the group receiving Calcemin Advance therapy, a stable state of BMD was noted, while in the control group, mineral density decreased in all assessed areas, which is especially was expressed in the lumbar spine (0.865±0.06 g/cm compared with 0.853±0.067 g/cm), and this decrease was significant p<0.013.
When comparing both groups in terms of BMD dynamics (as a percentage of the initial data), a significant difference was revealed between the increase in BMD in the lumbar vertebrae in the drug intervention group and the decrease in BMD in this area in the control group, while in both areas of measurement of the proximal femur there were significant differences between groups were not obtained (Fig. 1).
Analysis of the dynamics of pain in the thoracic and lumbar spine showed a significant decrease in the severity of pain after 3, 6 and 12 months in both parts of the spine in women receiving therapy, compared with its severity at the study inclusion visit and compared with the control. The control group also showed a slight decrease in pain, but it was not statistically significant.
The quality of life of patients was assessed using a visual analogue scale (VAS) before the start of the study and after 12 months. To study the indicators of daily physical activity and limitation of movements, a questionnaire was filled out, which recorded the ability of women to perform various activities and the physical activity performed. During the study, on average across groups, we did not obtain changes in quality of life indicators, as well as range of motion and functional activity in patients, as in the comparison between groups (Table 1). However, among patients in the treatment group, there were significantly more patients who significantly improved their quality of life than in the control group (32 and 14%, respectively, p = 0.032).
Evaluating the results of biochemical studies over time, we identified an average increase in the calcium/creatinine index in the urine of patients receiving Calcemin Advance, but these indicators did not go beyond the reference values, i.e. were within normal limits and did not require discontinuation of the drug in any of the patients. Other indicators of calcium homeostasis remained within normal limits in both groups during observation.
The study of the dynamics of bone turnover markers showed similar changes in both groups: a statistically insignificant decrease in the level of osteocalcin and a significant decrease in bone alkaline phosphatase (markers of bone formation), a significant increase in type I collagen c-telopeptide (CTX - a marker of bone resorption). However, a comparative analysis between the groups revealed that in the drug intervention group the decrease in bone alkaline phosphatase levels after 3 months was on average 5% less compared to the group without treatment, and after 12 months the difference between the groups was already 26.7% (p <0.001). The average increase in serum CTX levels in patients receiving the drug after 3 months was 21% lower than in the control group, and after 12 months the differences between the groups were 26.1% and were significant (p = 0.03) ( Fig. 2).
98 people completed the study, 2 people dropped out from the control group. Adverse events associated with taking the drug occurred in 10% of people and were as follows: nausea (4%), flatulence (2%), constipation (2%), cramps in the calf muscles (2%).
Thus, the use of the drug Calcemin Advance for a year in postmenopausal women with osteopenia has a stabilizing effect on the mineral density of the skeleton and reduces pain in the spine. Its long-term use does not cause hypercalcemia and increased urinary calcium excretion. The drug is well tolerated. Due to the fact that about 80% of postmenopausal women do not take enough calcium from food, an assessment of its intake should be carried out in all postmenopausal women, and if a deficiency is detected, preventive medication in the form of pharmacological drugs in combination with vitamin D, which increases its absorption, should be prescribed. Gastrointestinal tract. The study allows us to recommend Calcemin Advance for the prevention of postmenopausal osteoporosis.
Figure and table are in the appendix
How is ankylosing spondylitis diagnosed?
As with arthrosis of the knee, shoulder or hip, this disease involves changes in the articular cartilage. The pathology takes many years to develop, and the first symptoms appear when the joints have already significantly degraded. To clarify the diagnosis, a rheumatologist may prescribe the following examinations:
- X-ray;
- MRI;
- test for histocompatibility antigen, which is responsible for predisposition to this disease;
- Ultrasound of hands and feet;
- laboratory tests - ESR, C-reactive protein (the most informative in determining the current stage of the inflammatory process);
- examinations of other systems (fluorography, electrocardiography, consultation with an ophthalmologist, etc.).
Diagnosing ankylosing spondylitis is very difficult
How is ankylosing spondylitis treated?
As in the treatment of osteoarthritis, a rheumatologist selects an individual treatment regimen - combines medicinal and non-medicinal methods. The goal of treatment is to eliminate pain and inflammation and slow down the progression of the disease. For this purpose, they resort to medications, physical therapy, recommend special exercises, and in severe cases, surgical intervention (joint replacement, fixation of vertebrae or straightening of a deformed spine).
The best physiotherapy for this diagnosis is UV irradiation, UHF therapy of joints, electrophoresis of novocaine or Parfenov's liquid. You can also get a certain improvement after a course of ultraphonophoresis with hydrocortisone, after taking salt and hydrogen sulfide baths. In the inactive stage of the disease, balneotherapy is indicated.
In case of ankylosing spondylitis, the patient is given an individual exercise therapy program. It includes exercises for stretching the spine, bending, Nordic walking and swimming, yoga or complexes with a gymnastic stick. The main thing is not to experience discomfort, otherwise you can harm the affected joints.
In case of ankylosing spondylitis, you can perform the following complex of exercise therapy, which over time will alleviate the general condition:
Why does ankylosing spondylitis develop?
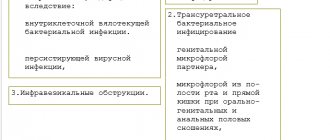
No one knows the exact cause, but it is assumed that the disease develops due to malfunctions of the immune system, especially in the presence of provoking factors:
- too low birth weight;
- infectious disease at the age of 5-12 years (infections of the genitourinary system and intestines are of particular danger);
- hypothermia;
- spinal and pelvic injuries;
- the presence in the body of enterobacteria that cause arthritis, etc.
The HLA-B27 gene is present in almost everyone who has been diagnosed with ankylosing spondylitis
Forms of ankylosing spondylitis
Depending on the location, the disease has the following forms:
- central – only the spine is affected (accounts for about half of all cases);
- rhizomelic - the shoulders and hip joints are also affected;
- peripheral – affects, in addition to the spine, the knee, elbow and ankle joints (diagnosed mainly at the age of 10-16 years);
- Scandinavian - similar in symptoms to rheumatoid arthritis, affects all joints, including small ones;
- visceral - inflammation also extends to blood vessels, kidneys, eyes and other organs.
The earlier ankylosing spondylitis is detected, the better it is treated
What medications can be prescribed
Depending on the manifestations, the rheumatologist may include the following drugs in the treatment regimen:
- nonsteroidal anti-inflammatory drugs, such as indomethacin and diclofenac, for pain relief;
- hormonal;
- immunosuppressants (if the cause is immune in nature);
- inhibitors of TNF-alpha and B-cell activation;
- chondroprotectors (in the early stages they stop the degradation of joints, accelerate the restoration of cartilage and reduce pain).
As with other joint diseases, ankylosing spondylitis can have different development scenarios. If it is detected too late and left untreated, it can result in disability. In the early stages, a person has every chance to take control of the disease and continue to lead a full life.
What is ankylosing spondylitis
This term refers to chronic progressive joint disease. In 80% of cases it begins with back pain (intervertebral joints are damaged), much less often with peripheral arthritis in the joints. The inflammation begins where tendons and ligaments attach to bone and spreads to the small joints between the vertebrae. Gradually the bones fuse and the spine slowly turns into one solid bone.
Since even the ligaments ossify, the person completely loses flexibility and cannot move. The inflammatory process spreads to the peripheral joints, which may already be affected by arthrosis, as well as to the eyes, lungs, kidneys and heart. Without timely treatment, the prospects are very sad.
Features of symptoms
The most common symptom is back pain, which worsens during sleep and improves with exercise. In addition, a person may feel:
- moderate pain in the groin, sacrum;
- stiffness of movements;
- curvature of the spine and stoop;
- feeling of chest tightness;
- dizziness and tinnitus;
- swelling of the joints.
With ankylosing spondylitis, the temperature may also rise at the end of the day, weight may decrease, and the person will quickly get tired. The eyes may become inflamed, sometimes heart valve failure develops and difficulty breathing occurs. Complications in the functioning of the nervous system are not uncommon. Similar symptoms occur with arthrosis, osteochondrosis, spondylosis, rheumatoid arthritis, so it is very important to make a correct diagnosis.
Ankylosing spondylitis has symptoms similar to arthrosis