What it is
These are drugs that improve performance, memory and learning ability. Piracetam was created first - it appeared in the sixties of the last century. In the seventies, scientist Corneliu Giurgia discovered that this medicine stabilizes the membranes of cells in the central nervous system, improving the functioning of brain cells. They didn’t know the exact mechanism of how piracetam works—they were just guessing. Giurja proposed using it to restore mental abilities after injuries, oxygen starvation of the brain, with senile dementia and congenital dementia in children.
Most nootropics are of animal origin. They are extracted from the brains of pigs and cattle, rich in low molecular weight proteins. The drugs are inexpensive and rarely cause side effects, which is why doctors love them.
Actovegin in the treatment of diseases of the nervous system
Treatment of patients with various neurological diseases with Actovegin has been discussed in a number of reviews [5,8,13,17]. Actovegin is a highly purified hemodialysate obtained by ultrafiltration from the blood of calves. The drug contains organic low-molecular compounds, which eliminates the development of prion diseases, such as Creutzfeldt-Jakob disease. The technology for producing Actovegin excludes the presence of protein components that have antigenic and pyrogenic properties. Actovegin contains amino acids, oligopeptides, nucleosides, intermediate products of carbohydrate and fat metabolism, antioxidant enzymes, electrolytes, and trace elements. There are no exact data on the pharmacokinetics of Actovegin, since it is a multicomponent drug and its composition includes substances originally contained in the human body. Experimental studies have shown that the effect of Actovegin on glucose metabolism begins after 5 minutes, and the peak of action appears after 120 minutes. after intravenous administration of the drug. The antihypoxic effect of Actovegin is associated with its ability to increase the absorption of oxygen by tissues, which increases the resistance of cells to hypoxemia. As a result of normalization of the supply of oxygen and glucose to tissues, the formation of marcroergic phosphates (ATP, ADP) increases and cellular energy imbalance decreases. An increase in oxygen absorption by the vascular wall with the administration of Actovegin leads to the normalization of endothelium-dependent reactions and a decrease in peripheral vascular resistance. The antioxidant effect of Actovegin is ensured by the presence of superoxide dismutase in the drug, which is confirmed by atomic emission spectrometry, as well as magnesium ions, which increase the activity of glutathione synthetase, which converts glutathione into glutamine [6]. It has been shown that Actovegin helps to increase the rate of redox processes in hepatocytes, reduces ultrastructural and functional damage to cardiomyocyte mitochondria, and increases the reduced level of glucose metabolism in chronic alcoholism. Improving the energy capabilities of cells of various organs and tissues, including the nervous system, is associated with Actovegin’s ability to improve the transfer of glucose into the cell by activating its transporters (GluT) and the insulin-like action of one of the components of the drug - inositol phosphooligosaccharide. Due to the fact that Actovegin modulates the activity of intracellular glucose transport [21], lipolysis is activated. The possibility of using Actovegin for the treatment of diabetes mellitus and metabolic syndrome is being considered [12,15]. Simultaneous administration of the antihypertensive drug b-blocker bisoprolol and Actovegin leads to an increase in cerebral perfusion in patients with metabolic syndrome. Actovegin is recommended for widespread use in a wide variety of fields of medicine, for example in the form of a 20% gel, 5% ointment or cream in the treatment of dermatological pathologies. The main task of the external form of the drug is to accelerate tissue healing. However, neurological diseases are the main indication for its use. In neurology, Actovegin is used in the form of intravenous, intramuscular solutions or tablets for oral administration. In intensive care units, Actovegin at a dose of 800–1200 mg is prescribed for the prevention of reperfusion syndrome in patients with acute myocardial infarction, after thrombolytic therapy and balloon angioplasty, in the treatment of various types of shock, after circulatory arrest and asphyxia, and in severe heart failure [14] . The prospects of using Actovegin in the early stages of the formation of persistent vegetative states caused by cerebral hypoxia are considered. At the same time, they proceed from the idea that the leading factor in the preservation of neuroglial structures in conditions of hypoxia and ischemia is the maintenance of stable cerebral blood flow, oxygenation and the creation of conditions for activating the utilization of oxygen and glucose in order to ensure the normal functioning of the Krebs cycle. Currently, Actovegin is widely used for the treatment of vascular diseases of the brain and cognitive impairment of varying severity [17]. In a study of the effectiveness of Actovegin’s effect on cognitive functions in elderly and senile people, it was revealed that after 2 weeks of starting drug therapy, a statistically significant improvement in memory, attention and thinking was noted. Clinical improvement in cognitive function, according to neuropsychological testing, is accompanied by normalization of the electroencephalogram and an increase in the amplitude of the evoked cognitive potential P300, and even a single administration of the drug led to an improvement in electrophysiological indicators of brain function [25,26]. Several double-blind, placebo-controlled, randomized studies have studied the effect of Actovegin in patients with mild or moderate dementia. After oral administration of Actovegin at a dose of 2 tablets 3 times a day for 8 weeks, the speed of mental processes significantly increased [24]. A study involving 120 patients with cerebrovascular insufficiency and cognitive deficit showed that during long-term treatment of discirculatory encephalopathy with cognitive impairment syndrome, preference should be given to oral administration of Actovegin [19]. Parenteral administration of Actovegin in this group of patients showed improvement in cognitive functions, primarily memory and attention, reduction in the severity of affective disorders and improvement in social adaptation. It should be especially noted that the effectiveness of the drug increases with increasing time of the course of infusion therapy, not only in vascular dementia, but also in Alzheimer's disease [2,23]. A course of infusion therapy with Actovegin leads to a more pronounced and faster improvement in the condition of patients with cognitive impairment, so it is recommended to start treatment with the parenteral form of the drug, and then switch to taking tablets [3]. The possibility of using Actovegin, given its effect on glucose utilization, in patients with type 2 diabetes with diabetic encephalopathy for the treatment of cognitive impairment is of great interest. In a study of 60 patients with type 2 diabetes mellitus (DM) who had cognitive impairment of varying severity, intravenous administration at a dose of 400 mg for 3 weeks led to an improvement in the sum of scores on the MMSE scale (25.50 ± 2.52 points before treatment and 26 .47±2.50 points after treatment, p<0.05), with memory improving to the greatest extent (Fig. 1) [11]. The improvement in cognitive functions was not accompanied by a significant decrease in depression and anxiety, as well as changes in cerebral hemodynamics according to duplex scanning. Thus, it can be assumed that the clinical effectiveness of Actovegin in patients with type 2 diabetes with cognitive impairment is primarily due to an improvement in cerebral metabolism. In a pilot study carried out on 10 patients with severe traumatic brain injury (TBI), data were obtained on the advisability of using Actovegin in this group of patients. However, the effectiveness of the drug in the treatment of TBI needs to be confirmed by the results of double-blind placebo-controlled randomized studies [4]. There is much less data on the possibility of treating diseases of the peripheral nervous system with Actovegin. However, a vascular component is present in many mononeuropathies, including radiculopathies, multiple mononeuropathies and polyneuropathies. Works on the treatment of elderly patients with discogenic radiculopathies who have intense pain syndrome with Actovegin, Xefocam and indomethacin are presented. When using Actovegin, patients experienced a more rapid regression of pain syndrome compared to groups of patients receiving only Xefocam or indomethacin [16]. In addition, as a follow-up study showed, patients in the group of patients receiving combination therapy with Actovegin were 43% less likely to have a need for re-hospitalization due to relapse of pain. The severity of neurological deficit was significantly lower in the group of patients receiving Actovegin than in other groups. In addition, in the group of patients treated with Actovegin, a significant improvement in well-being, motor activity and sleep was noted. It was concluded that the inclusion of Actovegin in the complex therapy of elderly patients with discogenic radiculopathy allows for faster relief of pain, accelerates regression of neurological disorders and improves the well-being of patients. Significantly more studies evaluating the effectiveness of Actovegin have been carried out in diabetic lesions of peripheral nerves - diabetic distal symmetric sensory-motor polyneuropathy (DPN) [5,18,22], which is predetermined by the mechanisms of pharmacological action of the drug. Reduced blood flow in endoneural vessels caused by microangiopathy underlies the formation of DPN. One can agree with the point of view that “diabetes begins as a metabolic disease and ends as a vascular pathology” [1]. According to the modern point of view, the development of DPN is associated with oxidative stress resulting from disorders of glucose metabolism, as well as the weakness of one’s own antioxidant systems [20]. Metabolic disorders, causing changes in the content of phosphate energy substrates in the cytoplasm of cells, lead to the development of the phenomenon of “pseudohypoxia”. Thickening of the vascular wall of endoneurial vessels and changes in the rheological properties of blood in diabetes form true hypoxia. This understanding of the metabolic and vascular processes underlying the development of DPN makes it advisable to use Actovegin, which affects the development of hypoxia and glucose metabolism, for the treatment of DPN. W. Jansen and E. Beck studied the effect of Actovegin in patients with DPN in a controlled study: one group of 35 patients received placebo, another group of 35 patients received Actovegin at a dose of 600 mg (2 tablets) 3 times a day for 24 weeks [22]. The criteria for assessing the effectiveness of the drug were clinical characteristics of polyneuropathy (tendon reflexes, superficial and deep sensitivity, intensity of pain) and EMG indicators of peripheral nerve function (velocity of propagation of excitation (RPV), as well as the distance that patients could walk without pain. Improvement in the condition of patients in Actovegin treatment group was observed in the majority of patients 8 weeks after the start of treatment, and the optimal effect was achieved after 16 weeks of treatment.Significant improvement compared with the placebo group was shown in almost all clinical indicators: pain-free walking distance, tendon reflexes, superficial and deep sensitivity (p <0.01).SRV significantly (p<0.001) increased in the Actovegin group compared to the placebo group. Patients in the Actovegin group felt better and had fewer complaints about disturbances in psycho-emotional status, which correlated with an improvement in their physical condition. In the work of Yavorskaya V.A. et al. [18] in an open study, Actovegin was used for the treatment of DPN in 24 patients with type 1 and 2 diabetes in the form of daily infusions for 20 days. The effectiveness criteria were clinical indicators, data from peripheral blood flow studies, and the results of an EMG examination. An improvement in the clinical condition of patients was noted in the form of a decrease in pain, improved sensitivity and tendon reflexes, and an increase in muscle strength. Rheovasography showed an improvement in blood flow in the legs, and an EMG examination showed an increase in the amplitude of the M-response and SRV when stimulating the nerves of the legs. The use of Actovegin in the complex treatment of 33 patients with diabetic foot syndrome of varying severity according to the Wagner classification showed that the connection of the drug to traditional treatment contributed to the rapid relief of pain and the acceleration of the processes of granulation and epithelization of ulcerative defects with their healing [7]. In the study by Morgoeva F.E. et al. The effectiveness of intravenous monotherapy with Actovegin in patients with type 2 diabetes was studied [5]. The group of 30 patients who received Actovegin once a day intravenously at a dose of 400 mg, in 200 ml of physiological solution for 3 weeks (15 infusions) included patients with diabetes duration of at least 10 years at the age of 58.94 ± 1.29 years (9 men and 21 women). The presence of DPN was determined based on neurological examination, EMG results, quantitative sensory and autonomic testing. The group included patients who had stages 2a and 2b of DPN according to the PJ Dyck classification and an HbA1C level of no more than 10%. The assessment of positive neuropathic symptoms (unpleasant sensations of patients) was carried out using the TSS scale (Total Symptom Score - a general score of symptoms of neuropathy) with an analysis of the severity of pain, burning, numbness and paresthesia. Negative neuropathic symptoms (neurological deficits) were assessed using the NISLL scale (Neuropathy Impairment Score - a score of neuropathic disorders for the legs) with testing of muscle strength, reflexes and sensitivity of various modalities. The study of the functional state of the peripheral nerves of the legs was carried out using EMG stimulation with testing of the motor (n. peroneus) and sensory (n. suralis) nerves. Quantitative assessment of superficial and deep sensitivity, as well as autonomic cardiac innervation was carried out using a CASE-IV device (Medical Electronics, USA) with determination of thresholds of cold, temperature, pain and vibration sensitivity. The level of oxidative stress was assessed by the content of malondialdehyde in blood serum and erythrocyte hemolysate. The state of microcirculation was studied in the nail bed of the second finger of the hand using a GY-0.04 computer capillaroscope (Russia). Digital image analysis made it possible to determine the speed of blood flow, the number of “sludge phenomena,” and the amount of perivascular edema. The patients were examined before and after the course of treatment with Actovegin. Before treatment, in the group of patients with diabetes with DPN, a significant increase in the level of lipid peroxidation in plasma and erythrocyte membranes was observed compared with a group of 15 healthy volunteers of the same age, which indicated the severity of oxidative stress. Treatment with Actovegin led to a decrease in the level of malondialdehyde (MDA) in plasma and erythrocyte membranes, followed by its normalization. Thus, Actovegin had an undoubted antioxidant effect, acting on the pathogenetic mechanisms of the development of DPN. The state of the rheological properties of blood was assessed by computer capillaroscopy before and after treatment with Actovegin. After treatment with Actovegin, a significant improvement was noted in the main characteristics of capillary blood flow, not only reflecting the rheological properties of the blood, but also the state of permeability of the capillary wall (Fig. 2). Before treatment, the severity of positive neuropathic symptoms on the TSS scale was significant (7.79 points). After treatment, there was a significant decrease in both the sum of scores on the TSS scale and the scores of each sensory symptom separately (p<0.001) (Table 1). The decrease in the severity of painful sensations in patients after treatment with Actovegin was not associated with psycho-emotional disorders, since no dynamics in the severity of depression and anxiety were noted after treatment (Table 2). When assessed before treatment, the severity of negative neuropathic symptoms was insignificant (sum of points on the NISLL scale – 2.27 points), and disturbances of sensitivity and reflexes were mainly detected. After treatment with Actovegin, a significant decrease in the severity of neurological deficit was noted (p<0.05), but not in individual groups of symptoms (muscle strength, reflexes, sensitivity) (Fig. 3). When studying the functional state of the motor nerve, no significant changes in the main electrophysiological characteristics were revealed after treatment with Actovegin. When studying the functional state of the sensory nerve, a significant increase in the amplitude of the sensory response was revealed (3.87 ± 2.43 μV before treatment and 6.19 ± 3.16 μV after treatment, p < 0.05) with the SRT unchanged (Table 3). A study of temperature and pain sensitivity thresholds using quantitative sensory testing showed that after treatment with Actovegin, there is a decrease in sensitivity thresholds associated with the state of thin nerve fibers (p < 0.05). There was no significant increase in the threshold of vibration sensitivity (thick fibers), although an EMG examination revealed a significant increase in the amplitude of the sensory response. Heart rate variability, according to the study of R-R intervals at rest and during the deep breathing test, did not significantly change after treatment with Actovegin, although a tendency towards normalization was noted. Thus, the study showed that anti -ovegin treatment, reducing the severity of oxidative stress and improving the condition of the microcirculation system, leads to patients with type 2 diabetes to regression of the clinical manifestations of DPN, which is confirmed by an improvement in the functional state of the peripheral nerves (EMG and quantitative sensory testing). Despite the fact that all studies of the effectiveness of Actovegin in DPN showed the feasibility of its use, there is a need to conduct a large -scale controlled study with a large number of patients in the treatment group and the placebo group. In 2007–2008 Under the patronage of the pharmaceutical, a multicenter randomized double -centered placebo -controlled study was carried out with the planned inclusion of 550 patients (“Actovegin against placebo in patients with diabetic polyneuropathy”). Currently, the results are statistically processed and will be allegedly published at the end of 2008. It is hoped that this study will finally solve the issue of the effectiveness and safety of the use of Actovegin for the treatment of DPN. From a pathophysiological point of view, there is no doubt that the Actovegin with an anti -hyponsant and antioxidant effect can be used for a wide range of neurological diseases of the central and peripheral nervous system, in the pathogenesis of which hypoxia, ischemia and oxidative stress play the role of hypoxia. The drug can be used for vascular diseases of the brain, for cognitive disorders caused by vascular or vascular -deigenerative factors. Diseases of the peripheral nervous system, for example, ischemic neuropathies, tunnel and radicular syndromes, in the genesis of which the vascular factor plays an important role, is also a possible goal for the use of actovengin.
Literature 1. Efimov A.S. Diabetic angiopathies // M. "Medicine" - 1989. 2. Kammerer S. Early initiation of therapy in patients with dementia // Russian medical journal. – 2003 – No. 10 – p.583–585. 3. Kunz G., Schumann G. The use of Actovegin in moderate dementia: results of a multicenter double-blind placebo-controlled randomized trial // Neurological Journal - 2004 - No. 1 - pp. 40–44. 4. Mihalovich N., Hack J. Antihypoxants in emergency treatment of traumatic brain injuries // Russ. honey. magazine – 2004 – No. 10 – p.621–625. 5. Morgoeva F.E., Ametov A., Strokov I.A. Diabetic encephalopathy and polyneuropathy: therapeutic possibilities of Actovegin // Russ. medical journal – 2005 – No. 6 – p.302–304. 6. Nordvik B. Mechanism of action and clinical use of the drug Actovegin // In collection. “Actovegin. New aspects of clinical application” – M. – 2002 – p. 18–24. 7. Obolensky V.N. Complex treatment of patients with diabetic foot syndrome // In collection. “Experience in the clinical use of Actovegin in endocrinology” – M., 2005 – pp. 39–46. 8. Piradov M.A., Rumyantseva S.A. RMJ – 2005 – No. 15 – p.980–983. 9. Rumyantseva S.A. Pharmacological characteristics and mechanism of action of Actovegin // In collection. “Actovegin. New aspects of clinical application” – M. – 2002 – p. 3–9. 10. Rumyantseva S.A., Benevolenskaya N.G., Evseev V.N. Antihypoxants in resuscitation and neurology // Russ. medical journal – 2004 – No. 22 – pp. 302–304. 11. Strokov I.A., Morgoeva F.E., Strokov K.I. and others. Therapeutic correction of diabetic polyneuropathy and encephalopathy with Actovegin // Russ. medical journal – 2006 – No. 9 – p.698–703. 12. Sych Yu.P., Zilov A.V. Possibilities of using Actovegin in the treatment of diabetes mellitus // Problems of endocrinology – 2003 – No. 3 – pp. 51–53. 13. Chugunov A.V., Kamchatnov P.R., Kabanov A.A. and others. Possibilities of metabolic therapy in patients with chronic cerebrovascular disorders // Consilium medicum – 2006 – No. 2. 14. Shilov A.M. Antihypoxants and antioxidants in cardiological practice // Russ. honey. journal – 2004 – No. 2 – pp. 112–114. 15. Shishkova V.N. Prospects for using the drug Actovegin in patients with metabolic syndrome and prediabetes. Modern ideas about disorders of carbohydrate metabolism // RMJ – 2007 – No. 27. 16. Shmyrev V.I., Bobrova T.A. Actovegin and Xefocam in combination therapy of vertebrogenic pain syndromes in the elderly // Treatment of nervous diseases - 2002 - No. 1 - pp. 37–39. 17. Shmyrev V.I., Ostroumova O.D., Bobrova T.A. Possibilities of the drug Actovegin in the prevention and treatment of dementia // Russian medical journal. – 2003 – No. 4 – pp. 216–220. 18. Yavorskaya V.A., Egorkina O.V., Mashkin O.N. and others. Clinical experience with the use of Actovegin in diabetic polyneuropathy // In the collection. “Experience in the clinical use of Actovegin in endocrinology” – M. – 2005 – art. 27–30. 19. Jansen V., Bruckner G.V. Treatment of chronic cerebrovascular insufficiency using Actovegin forte tablets (double-blind placebo-controlled study) // Russ. medical journal – 2002 – No. 12–13 – pp. 543–546. 20. Brownly M. Biochemistry and molecular cell biology of diabetic complications // Nature – 2001 – Vol.414 – P.813–820. 21. Jacob S., Dietze GJ, Machicao F. et al. Improvement of glucose metabolism in patients with type II diabetes after treatment with hemodialysate // Arzneimittelforschung – 1996 – No. 3 – P.269–272. 22. Jansen W., Beck E. Treatment of diabetic polyneuropathy. Controlled double-blind study // In collection. “Experience in the clinical use of Actovegin in endocrinology” – M., 2005 – pp. 11–20. 23. Kinzler E., Lehmann E., Groth J. et al. Actovegin in der Behandlung geriatrischer Patienten mit hirnorganischem psychosyndrom // Munch Med Wochenschr – 1988 – Vol. 130 – P.644–646. 24. Oswald WD, Steger W, Oswald B et al. Die Verbesserung fluider kognitiver Leistungen als Indikator fur die klinische Wirksamkeit einer nootropen Substanz.Eine placebokontrollierte Doppelblind–Studie mit Actovegin // Z. Gerontopsychol.–psychiatrie. – 1991 – Vol.4 – P.209–220. 25. Saletu B., Grunberger J., Linzmayer L. et al. EEG brain mapping and psychometry in age-associated memory impairment after acute and 2-week infusions with the hemoderivative Actovegin: double-blind, placebo-controlled trials // Neurophychobiol. – 1990/1991 – Vol.24 – P.135–148. 26. Semlitsch HV, Anderer P, Saletu B et al. Topographic mapping of cognitive event-related potentials in a double-blind, placebo-controlled study with the hemoderivative Actovegin in age-associated memory impairment // Neurophychobiol. – 1990/1991 – Vol.24 – P.49–56.
When to use them
Most often, nootropics appear in the prescriptions of neurologists. They are prescribed for everything - from neurosis and OCD, from VSD, which does not exist, and dementia. In hospitals, nootropic drugs are administered intravenously to speed up tissue recovery after a stroke or transient ischemic attack - as prescribed by clinical recommendations. But they do not recommend using some nootropics during the acute period of ischemic stroke due to possible neuronal depletion and steal syndrome. Therefore, focusing only on them is not enough.
“First, the doctor makes a generally accepted diagnosis,” says GMS Clinic neurologist Sergei Makarov. — If we are talking about vascular cognitive impairment, then first of all the risk factors are corrected: diabetes mellitus, atherosclerosis and arterial hypertension. Not all diseases require medication."
But many neurologists and psychiatrists, who are not interested in new research, prescribe nootropics to people with impaired memory, attention and learning ability, focusing only on clinical recommendations. For example, Cerebrolysin is recommended for the prevention of dementia at the initial signs of Alzheimer's disease. Also, many doctors believe that nootropics will help you stay sane and memory longer in case of chronic vascular disorders of the brain.
“When a child has a disorder of psychoneurological development, the doctor is tempted to give something to “improve brain function,” says Varvara Khaletskaya, MD, neurologist at the Fantasy children’s clinic. “After all, sometimes there is no effective method leading to a complete recovery. Therefore, the doctor and the parent are trying to invest bit by bit: pedagogical correction, physiotherapy and medications.
It’s another matter when there is an effective treatment protocol, but the doctor continues to treat in his own way. It turns out ugly: instead of pedagogical correction, a child with psycho-speech disorders is given nootropic drugs, and they are advised to “wait” with classes. Or in the case of sensorineural hearing impairment, for which hearing aids are possible, they are referred to a neurologist to “feed” the auditory nerve. In this case, time is simply wasted. Before prescribing a treatment with insufficient evidence base, the doctor should make sure that there is a more effective solution.”
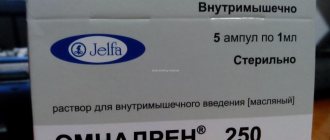
Actovegin
Actovegin belongs to the group of antihypoxants, i.e. drugs that help body cells store oxygen and reduce the need for it. The pharmaceutical raw material for the production of Actovegin is calf blood serum extract. By activating the cellular metabolism of oxygen and glucose and optimizing their consumption, the drug significantly increases the energy capabilities of cells and their resistance to oxygen starvation. When using Actovegin, the synthesis of ATP, the main energy “fuel” of the body, increases 18 times. Thus, all energy-consuming processes in cells are intensified (regeneration). At the same time, Actovegin increases the body's concentration of amino acids aspartate, glutamate, and gamma-aminobutyric acid, which promotes, for example, the rapid healing of wounds and other skin damage.
The method of using Actovegin is determined by its release form. Tablets are taken three times a day before meals along with a small amount of water, 1-2 pieces. Duration of treatment is 1-1.5 months. Actovegin solution is injected into a vein, muscle or artery. The initial dose is 10-20 ml per day, then the dose is reduced to 5-10 ml. The duration of treatment depends on the specific disease, for example, for disorders of cerebral circulation and metabolism it is at least a month, for ischemic stroke - 3 weeks, for poorly healing ulcers and burns, they focus mainly on the speed of the healing process.
As for the external forms of release of Actovegin - cream, gel and ointment - in this case the drug is used externally: applied twice a day (this is the established minimum, more often is possible) for at least 12 days. For ulcers, wounds and inflammatory skin diseases, treatment begins with 20% gel and 5% cream, then moves on to 5% ointment (the so-called three-step treatment). In order to prevent bedsores, external forms of Actovegin are rubbed into the skin in the most disadvantaged places in this regard.
When using Actovegin in the form of an injection solution, you should be aware of a number of important circumstances. Thus, when using the drug intramuscularly, it is allowed to administer no more than 5 ml of solution. To prevent allergies, it is recommended to do a test injection (2 ml of solution intramuscularly). No preservatives are used in the production of injectable Actovegin, so injections must be carried out in strict compliance with all aseptic conditions. And most importantly: the opened drug is not stored, and if not all of the solution was used from the open ampoule, then the remaining drug must be disposed of.
Do they have any effect?
Until the 2000s, the actual mechanism of action and effectiveness of nootropics was not particularly studied. Doctors prescribed them, and people drank them. There was a myth circulating among medical students that a month-long course of nootropics before exams improves memorization of the material, and to be sure, you need to inject it into a muscle or vein.
Now the proof of the drug’s effectiveness is not the doctor’s word, but research data. There must be at least three thousand participants, and they must be divided into at least two groups, one of which is a control group with a placebo. At the same time, neither the doctor nor the patient knows what each of the subjects is drinking - medicine or a “dummy”.
Nootropic drugs have been little studied, and studies of their effectiveness are inadequate. Either there are too few people, or the criteria are unclear. For example, they estimate the number of test points only after treatment - they apparently forgot before treatment. The American FDA, in principle, does not consider nootropics to be drugs - in the USA they are sold as dietary supplements.
“Everyone knows that nootropics are drugs without proven effectiveness. But they continue to be used, says Varvara Khaletskaya. — There are statistics, there are international protocols that help the doctor. But at the same time, each doctor’s personal experience remains with a wide range: from “they are useless” to “they are effective in many patients.”
The fact is that there is a rare exception: piracetam improves cognitive function in people with severe dementia, according to an assessment of 19 high-quality studies. But with a traumatic brain injury or mild dementia, piracetam will no longer help. Moreover, it is useless for healthy people who want to follow the path of Eddie Morra from the film “Dark Areas” and become a megabrain. Therefore, if biohacking experiments with Mexidol seem to be effective, it is only due to self-persuasion.
The incidence of chronic cerebrovascular accident is determined to be 70-100 cases per 1000 population [8], and impaired cognitive function is recognized as one of the most common manifestations of cerebrovascular disease. According to population studies, the initial manifestations of this disorder are detected in 24.4% of the urban population of elderly and senile age (60 years and older), and among elderly patients observed in a psychoneurological clinic - in 18.7% [1]. During a comprehensive examination of elderly patients at a territorial clinic, these disorders were found in 30.8% [6]. Mild cognitive impairment (MCI) as part of vascular psychoorganic syndrome in 24.5% of cases is the reason for contacting a gerontopsychiatrist at a general somatic clinic, and in another 36.2% of cases it is diagnosed as a comorbid disorder in patients of a gerontopsychiatric office [6 ].
MCI[] syndrome is characterized by a borderline disorder of memory and cognitive functions, the degree of manifestation of which does not allow a diagnosis of dementia of cerebrovascular or other origins, including Alzheimer's disease (AD) [2].
The prevalence of MCI syndrome in old age is extremely high. Among the Moscow population over 60 years of age, this figure is about 18% [4]. Similar figures (19%) are given by O. Lopez et al. [15]. As has been shown by domestic researchers [9], 40% of people with an established diagnosis of MCI are diagnosed with AD or dementia of another origin within 4 years.
In recent years, evidence has been obtained of the heterogeneity of the MCI syndrome, and therefore various clinical variants of the syndrome have been identified (amnestic, non-amnestic and variant with multiple cognitive impairment), which have a different prognosis in terms of the likelihood of transition to different nosological types of dementia (AD, vascular or frontal dementia). temporal dementia, dementia with Lewy bodies, etc.).
A high risk of worsening cerebral vascular disease, including an increased risk of cerebrovascular accidents, as well as the risk of developing dementia even without stroke, is most often associated with MCI syndrome with multiple cognitive impairment [5, 15].
In this regard, the tasks of treating MCI of vascular origin in elderly and senile patients have become the most pressing in geriatric practice and constitute the daily content of the activities of both neurologists and psychiatrists, as well as general practitioners [12, 14]. Treatment of the initial manifestations of cognitive decline is one of the most important tasks of complex therapy, including the prevention of dementia in the elderly.
Current treatments for initial cognitive decline of vascular origin include improving blood rheology, improving the delivery and use of oxygen and glucose in cerebral structures; reduction of neurotransmitter deficiency.
Actovegin, used for the treatment and prevention of hypoxic and ischemic disorders of organs and tissues, belongs to the group of drugs without direct vasodilating effects. The drug acts as a neurometabolic stimulant, increasing the energy supply of nerve cells by increasing the consumption and utilization of oxygen and glucose, which leads to improved brain function.
Actovegin is a highly purified hemodialysate obtained by ultrafiltration from the blood of young bulls under the age of 6 months. The drug contains exclusively physiological components with high biological activity - organic low-molecular compounds: amino acids, oligopeptides, nucleosides; intermediate products of carbohydrate and fat metabolism: oligosaccharides and glycolipids. The molecular weights of the organic compounds that make up Actovegin do not exceed 5000 daltons. The technology for obtaining hemodialysate excludes the presence of protein and other components with antigenic and pyrogenic properties. Experimental and clinical studies have proven that Actovegin does not contain additional impurities of blood components.
The therapeutic effectiveness of Actovegin is due to a wide range of substances included in its composition: amino acids, oligopeptides (insulin-like action), nucleosides, electrolytes (potassium, sodium, phosphorus, magnesium, calcium, copper) and microelements, as well as intermediate metabolic products (oligosaccharides, glycolipids).
Numerous studies have shown that Actovegin, by improving the absorption of oxygen and glucose by nerve cells, has an activating effect on metabolic processes in the brain. When glucose consumption increases, oxygen consumption increases accordingly. These processes lead to the acceleration of ATP synthesis in the brain, stimulation of cellular metabolism, and improvement of blood supply to ischemic brain tissue, which provides a clear therapeutic effect for cerebrovascular accidents.
The supply of large amounts of oxygen causes activation of aerobic oxidation, which in turn increases the energy potential of the cell. Actovegin improves energy exchange in the vascular endothelium, which leads to the release of endogenous substances with vasodilating properties - prostacyclin and nitric oxide - and improved perfusion of all tissues and a decrease in peripheral resistance. In conditions of tissue hypoxia caused by impaired microcirculation, Actovegin promotes the restoration of the capillary network due to newly formed vessels. By improving oxygen delivery and reducing the severity of ischemic tissue damage, Actovegin promotes the protein-synthesizing function of cells.
The effect of Actovegin is most pronounced under conditions of intracellular oxygen deficiency, in particular due to hypoxia or hypoperfusion, and the antihypoxic effect of Actovegin extends not only to neuronal, but also to glial structures. The effect of Actovegin begins to manifest itself no later than 30 minutes (10-30 minutes) after parenteral administration and reaches a maximum after an average of 3 hours (2-6 hours).
Due to the fact that Actovegin improves microcirculation and has an activating effect on metabolic processes in the brain, it seems reasonable to study its effectiveness in elderly patients with cognitive impairment of vascular origin. Although Actovegin has been known for about 40 years as a classic neurometabolic drug, its attitude towards nootropic properties has fluctuated from doubts to evidence-based statements. A number of controlled studies [6, 7, 9, 12, 15, 17, 19] have shown the effectiveness of Actovegin in cognitive disorders of varying severity, including dementia of vascular and Alzheimer's origin [7, 9, 12]. Most studies show the benefits of parenteral administration of Actovegin by intravenous infusion of 250 ml (2000 mg) in a course of at least 10 infusions; however, a faster onset of effects on cognitive impairment is indicated. Reduction or leveling of memory and attention disorders, an increase in the pace of mental processes are recorded in more than half of the patients. There are no data on the results of another method of parenteral administration of Actovegin - intramuscular, which is much more convenient for widespread use in outpatient practice.
The purpose of this work is to study the effectiveness and safety of intramuscular use of Actovegin in elderly patients with mild cognitive decline syndrome of cerebrovascular origin.
Material and methods
The study was conducted as an open, uncontrolled study in a group of patients with MCI syndrome of vascular origin, under the supervision of employees of the Department of Alzheimer's Disease and Associated Disorders of the Department of Geriatric Psychiatry of the Scientific Center for Mental Health of the Russian Academy of Medical Sciences.
Inclusion criteria
patients in the study: women (postmenopausal) and men aged 50 to 85 years;
MMSE score ≥26 points; compliance with the operational criteria for the diagnosis of mild cognitive decline syndrome (MCI) (patient complaints of memory loss, confirmed by an informant - usually a family member, and objectively detected signs of mild cognitive dysfunction; score 0.5 on the CDR scale; no basis for a diagnosis of dementia; preservation of daily activities , although slight deterioration in complex and instrumental types of daily and/or professional activities is possible); Hacinski scale score >4 points; obtaining written informed consent from the patient. Exclusion criteria
: diagnosis of dementia according to DSM-IV, ICD-10 criteria; other organic diseases of the nervous system, congenital and/or acquired metabolic encephalopathies, toxic and drug encephalopathies, Parkinson's disease, stroke, epilepsy, infectious diseases, demyelinating and hereditary degenerative diseases of the central nervous system); neoplastic and/or traumatic brain injury; systemic diseases; severe organ pathology: malignant extracerebral, HIV infection, diabetes mellitus in the stage of decompensation or other endocrine diseases; alcoholism and/or drug dependence; drug or other intoxication; depression with a score >18 on the Hamilton Depression Scale; systolic pressure level >180 mm Hg, diastolic >95 mm Hg; deficiency of folic acid and/or vitamin B12; hypothyroidism; treatment with procognitive agents for 4 weeks before or during the study.
At the end of the run-in period, which lasted up to 7 days, patients were prescribed Actovegin at a dose of 200 mg (5 ml) intramuscularly, and treatment continued for 28 days.
Concomitant therapy was allowed to use short-acting benzodiazepine drugs and drugs aimed at treating somatic pathology if therapy with them began 1 month before the present study and continued throughout the study in stable doses.
The assessment of the patients' condition during treatment using scales was carried out on fixed days: day 0 (before the start of therapy), day 14 of the study, day 28 of the study (end of the treatment course), day 56 (follow-up period).
Before and during the study, the following methods of examining patients were used: objective clinical examination, ECG, laboratory blood and urine tests.
In accordance with the recommendations of S. Kanowski [14], the effectiveness of a nootropic drug should be assessed in three areas: psychopathologically (assessment of clinical symptoms); psychometrically (testing); by behavior (self-esteem and assessment by others, taking into account age characteristics).
The following scales and tests were used to assess the state of cognitive functions and daily activity of patients: CGI (Clinical Global Impression Scale), MMSE, Speech Performance Test, Frontal Dysfunction Scale, Clock Drawing Test, Boston Naming Test, Mattis Dementia Scale, 10 Word Memory Test , Hamilton Depression Scale. The safety of the drug was assessed using an adverse event rating scale.
The study included 30 patients, 7 men and 23 women aged from 53 to 84 years (average 71.2±8 years), who were undergoing inpatient or outpatient treatment.
The age of the patients at the onset of the disease ranged from 52 to 81 years (average 67.8±7.9 years). The duration of the disease in all cases (with the exception of one) coincided with the duration of the psychopathological state that was the indication for the prescription of Actovegin, and ranged from 1 year to 7 years (on average 3.3 years).
All patients with sufficiently long duration of disorders that met the criteria for MCI syndrome had no signs of obvious progression of cognitive impairment. In all cases, the score on the General Deterioration Scale - GDS (Global Deterioration Scale) corresponded to point 3, which reflects the most initial manifestations of the disease [18]. The assessment of cognitive status according to the Clinical Dementia Rating - CDR (Clinical Dementia Rating) in all cases did not exceed 0.5 points, which excluded or made the diagnosis of dementia doubtful due to the mild degree of the disorder. According to the Clinical Global Impression - Severity (CGI-S) scale, the severity of the patients’ condition was classified as “borderline disorder” in 10 patients, and in the remaining 20 observations - as “mild illness”.
In 3 cases, mild cognitive impairment was combined with comorbid depression of mild severity (14-16 points on the Hamilton Depression Scale - HAM-D). Another 12 patients had individual depressive symptoms (5-13 points on HAM-D) , the totality of which did not meet the criteria for depressive syndrome, and their manifestations coincided with somatic complaints or overlapped with asthenic symptoms.The average group total score before the start of treatment with Actovegin according to HAM-D was 9.1.
The psychopathological history, along with mild cognitive decline and pseudoneurasthenic disorders, in 5 patients revealed time-bound episodes of psychopathological disorders that occurred 2-3 years before inclusion in the present study. One patient had experienced delirium in the past, another developed depression after an acute cerebrovascular accident (ACVA), and another 3 patients had previously reported psychogenic depressive reactions.
Determination of the neurological history revealed that 9 patients had previously suffered strokes - in 5 cases in the form of transient ischemic attacks (TIA), the remaining 4 patients suffered ischemic strokes (in one of these cases - again). The Hacinski scale score at the beginning of the study ranged from 4 to 10 points (average 6 points). The neurological diagnosis of all patients included in the study was formulated as stage 1-2 dyscirculatory encephalopathy [10].
The condition of the patients before starting treatment with Actovegin was characterized by a complex of symptoms of varying nature and varying degrees of severity. Common to all was a combination of signs of mild cognitive decline and asthenic (pseudoneurasthenic) disorders expressed to varying degrees and extent.
The reason for seeking medical help was primarily complaints of forgetfulness and various manifestations of asthenia. Manifestations of forgetfulness were described by patients as difficulties in memorizing or recalling, loss of natural ease in choosing words, “as if something had stopped.” Patients complained of absent-mindedness, slowed intelligence, admitted that it was “not easy for them to collect their thoughts” and remember recent intentions, especially when attention was distracted, but, as the patients noted, they could subsequently spontaneously remember what was necessary. Most patients, with rare exceptions, complained of frequent or constant headaches, sometimes only in one half of the head, but more often without clear localization, or heaviness in the head, described painful sensations in the head in the form of “tightening with a hoop” or “pressure on the eyes, on your ears." In addition, many patients complained of constant “ringing” in the ears, noise, and “hum” in the head.
The next most common complaints were unsteady balance, unsteadiness when walking, or a feeling that “the ground is falling away from under your feet.” In addition, patients noted the rapid onset of fatigue after light exertion, even after eating, making the bed, fatigue and decreased performance, weakness with a desire to lie down. The deterioration of general well-being was accompanied by sleep disturbances, difficulty falling asleep, a decrease in the depth and duration of sleep, abundant vivid dreams of sometimes frightening content or tiresomely changing meaningless content, in some observations with hypnagogic visual illusions of perception. Morning awakening was characterized by difficulties in the transition from sleep to wakefulness, and a lack of feeling of rest after sleep. Some patients complained of daytime sleepiness and drowsiness that interfered with their usual activities.
Patients noticed the appearance of tearful touchiness or heightened sensitivity to ordinary impressions from what they saw or heard. Mood instability was characterized by the ease of reactions of irritation and impatience; patients often noticed an increase in these manifestations after a restless night with frequent awakenings. A tendency toward a pessimistic assessment of everyday phenomena and life events could be combined with an influx of unaccountable anxiety and worry. The content of anxious fears often determined the appearance of forgetfulness and concentration on the disease as a whole or individual disorders.
In the mental state, manifestations of bradyphrenia were revealed with a slow pace of thinking and speech, difficulties concentrating attention, its instability and exhaustion, which was clearly revealed during testing and was manifested by difficulties in maintaining an activity program, distractibility, forgetting a task, and a slow pace of completion. At the same time, the patients willingly underwent the testing procedure, and when they noticed their mistakes or when shortcomings were pointed out, they lamented or sadly ironized about the weakening of memory or intelligence. Initial manifestations of difficulties in naming the proposed objects or images were compensated for by replacing or describing their purpose, while a minimal sound prompt quickly led to the desired result. Hesitations and pauses when choosing words, slowness of speech were combined with thoroughness and excessive detail, getting bogged down in details or with repeated repetition of what has already been said. Emotional lability was manifested by episodes of tearful weakness against the background of a predominantly complacent background of mood or the emergence of anxiety against the background of low mood.
Basic clinical and demographic data regarding the examined patients are presented in Table. 1
.
Magnetic resonance imaging (MRI) of the brain in the vast majority of patients revealed: expansion of the subarachnoid spaces - in 25 (83.3%) patients out of 30 and enlargement of the cerebral ventricles - in 26 (86.7%) patients. In 18 (60%) patients, post-ischemic foci of small volume located periventricularly were found: single up to 1.5 cm in diameter in 7 (23.3%) patients or multiple small ones in 11 (36.7%) patients. Leukoaraiosis was noted in 19 (63.3%) cases. In general, according to MRI data, signs of dyscirculatory encephalopathy were confirmed in almost all patients.
In the patients included in the study, the polymorphism of the apolipoprotein (ApoE) genotype was determined using a blood test. In two thirds of the observations, patients had the ApoE4(-) genotype with the following distribution of &egr;2 and &egr;3 alleles: 3.3, 3.2, 2.3 (51.9, 3.7 and 11.1%, respectively). 7 patients (25.9%) had the ApoE4(+) genotype, including 3.4, 4.4 and 2.4 (25.9, 3.7 and 3.7%, respectively). Various types of somatic pathology were identified in the patients included in the study (Table 2)
.
80% of patients suffered from arterial hypertension. More than half of the patients were diagnosed with coronary heart disease; in one third of these cases, disturbances in cardiac conduction and rhythm were noted.
results
Clinical positive dynamics in the process of treatment with Actovegin was expressed in a decrease in complaints, patients about “gained strength.” The feeling of dizziness, according to them, occurred noticeably less frequently, the unsteadiness of gait and instability of balance disappeared. In a number of cases, a decrease in the painful sensation of noise in the head or ears was also noted. Patients also noted improved night sleep, decreased fatigue, and increased activity and performance. The improvement in mood was accompanied by a decrease in the level of anxiety and de-actualization of overvalued fears (according to the patients, “it was as if they were wearing a filter”). While forgetfulness remained, patients showed a lesser tendency to fixate on these manifestations.
It was noteworthy that already from the 2nd week of treatment in patients whose condition before the start of therapy showed signs of subdepression or individual depressive symptoms, the general background of mood improved, and this positive dynamics persisted until the end of the course administration of Actovegin and even a month after its ending.
Along with a decrease in complaints, a reduction in asthenic disorders, restoration or increase in emotional stability, disturbances in cognitive functioning experienced significant positive dynamics. First of all, this relates to improving concentration and reducing inhibition. The acceleration of the pace of mental activity was manifested in faster answers to questions and an improvement in the pace of activity when completing test tasks. In some cases, there was a clear decrease in the torpidity of thinking and the manifestations of bradyphrenia in general. Activity and initiative in conversation and communication increased, and daily activities were restored to the required extent. The manifestations of speech difficulties decreased, hesitations and pauses disappeared in spontaneous speech, and patients coped with naming faster and better. Dysmnestic disorders noticeably decreased in their severity, which was reflected in an increase in the volume of memorization or in a greater ease of reproducing consolidated information. It is important to note that this effect turned out to be quite stable and persisted a month after completion of Actovegin administration, when patients did not receive any other treatment other than maintenance therapy for somatic diseases.
Changes in the condition of patients during therapy and during the follow-up period are shown in the figure.
.
Figure 1. Effectiveness of Actovegin therapy according to the CGI scale. 1 - minimal deterioration, 2 - no improvement, 3 - minimal improvement, 4 - moderate improvement, 5 - marked improvement. An improvement in the general clinical condition in the studied group of patients by the 14th day of therapy was noted in 96.7% of cases, including minimal improvement in 73.4% of patients and moderate improvement in 23.3% (see figure)
. In 1 patient, by the 14th day of treatment, the condition slightly worsened. By the time the course of therapy was completed (28 days), the overall frequency of improvement of varying degrees of severity remained the same (96.7%), however, moderate improvement was found in 66.7% of patients, pronounced improvement was achieved in 13.3% of patients, and only in 16.7% of patients showed minimal improvement. In 1 patient the condition did not change. 28 days after the end of the course of treatment, i.e. on day 56, the rate of improvement of varying severity was 100%. Moderate improvement was observed in 76.7% of patients, pronounced improvement was found in 13.3% of cases, minimal improvement in 10% of cases.
There was a statistically significant improvement on the MMSE scale ( p
<0.01) cognitive functions at each stage of the course of therapy: before treatment - 26.8±1.3 points, after 14 days - 28.0±1.3 points, after 28 days - 28.5±1.0 points and on the 56th day - 28.6±1.2 points.
Compared with the period before treatment, all indicators reached a degree of statistical significance ( p
<0.01). Moreover, by the 56th day of the study (28 days after completion of the course of treatment), the total score on the scale turned out to be even higher than the score at the end of the course of therapy.
There was a statistically significant increase in the number of words named within 1 minute (starting with the letter “k”): on the 14th day - 14.2±3.9; on the 28th day - 14.7±3.9 and on the 56th day - 15.5±2.5 compared to the period before treatment - 11.3±3.9 ( p
<0,01).
There was a significant improvement on the frontal dysfunction scale ( p
<0.01) was noted in the “Conceptualization” and “Sound Associations” tests - by the 14th and 28th days of the treatment course, as well as by the 56th day of the study, i.e.
28 days after the end of Actovegin administration (Table 3)
.
Scores on the tests “Simple choice reaction” and “Complicated choice reaction” reached a statistically significant value by the time the treatment course was completed ( p
<0.01). There was no improvement in the total score on the Dynamic Praxis test.
The clock drawing test score improved statistically significantly ( p
<0.01) at each stage of the course of therapy and after completion of treatment: before treatment - 8.3±1.8; 14th day - 9.1±1.6; 28th day - 9.3±1.5; 56th - 9.6±1.1.
According to the Boston Naming Test, the total group number of independent correct answers statistically significantly improved ( p
<0.01) at each stage of the course of therapy and after completion of treatment: before treatment - 42.7±6.8; on the 14th day - 46.2±5.6; on the 28th day - 49.1±5.1; on the 56th day - 49.5±5.4.
According to the Mattis Dementia Scale in the “Similarities” and “Memory” tests, there was a statistically significant improvement ( p
<0.01) was noted on the 14th and 28th days of treatment, as well as after 4 weeks of follow-up
(Table 4)
.
There was no improvement in total scores on the “Reciprocal Coordination” and “Graphomotor Test” tests.
According to the 10-word memorization test, there was a statistically significant improvement in total scores during 1, 2, and 3 attempts to memorize words ( p
<0.01) was noted on the 14th and 28th days of the course of treatment, as well as on the 28th day of follow-up
(Table 5)
.
A statistically significant improvement in the total assessment of delayed word recall was achieved by the 28th day of therapy.
The statistically significant level of its improvement remained after 4 weeks of follow-up observation, although the degree of improvement in the total assessment decreased somewhat. According to the HAM-D scale, a statistically significant improvement in the total group score is M±SD ( p
<0.01) was noted by the 14th day - 5.8±3.2 points and the 28th day - 3.9±3.1 points of the course of treatment, as well as by the 28th day of follow-up - 3.9 ±3.7 points compared to the period before treatment - 8.8±4.5.
There were no adverse events during treatment with Actovegin during the study.
Discussion
The incidence of mild cognitive impairment, not reaching the level of dementia, is extremely high among elderly patients in general somatic institutions. However, there is a certain paradox in the clinical thinking of internists, when a diagnosis of cerebrovascular disease is easily made, often only on the basis of so-called “vascular” complaints and nonspecific neurological symptoms, while complaints of elderly patients about forgetfulness or statements of dysmnestic disorders are regarded as age-related characteristics of cognitive status. Accordingly, medical prescriptions are limited to the prescription of antihypertensive therapy, less often in combination with antiplatelet agents and vasodilators, and the correction of cognitive impairment is considered an optional measure, sometimes left to the discretion of patients.
Assessing the condition of patients urgently requires the study of cognitive functions, especially since complaints of elderly people about weakened memory, impaired ability to concentrate, decreased productivity, and fatigue are often the leading ones when visiting a doctor and determine the search for help.
In the genesis of cognitive impairment, a predominant role is given to ischemic brain lesions, both focal and diffuse, with special importance attached to subcortical lesions. One of the main pathogenetic factors is arterial hypertension (AH) and vascular lipohyalinosis. In these conditions, when there is a decrease in blood pressure or circadian blood pressure fluctuations, heart failure, or inadequate antihypertensive therapy, hypoperfusion occurs in the areas of the terminal circulation (deep structures). A marker of the presence of chronic ischemia is leukoaraiosis as a neuroimaging sign of demyelination, gliosis, and expansion of perivascular spaces.
The leading role in the pathogenesis of cognitive disorders of vascular origin is played by damage to the deep parts of the white matter and basal ganglia, which leads to disruption of connections between the frontal lobes and subcortical structures (disconnection phenomenon).
The results of an open, uncontrolled study of the effectiveness of a course of treatment with Actovegin with daily intramuscular administration of the drug at a dose of 200 mg demonstrated a significant improvement in the condition of the vast majority of patients with MCI syndrome of vascular origin. There was a significant improvement in group average indicators in almost all tests used to assess cognitive dysfunction. It should be noted that the drug in the studied dosage form has an undoubted effect on improving concentration, accelerating the pace of mental activity and memory processes.
The data obtained correspond to the indications given in the literature on the improvement of cognitive functions in cerebrovascular insufficiency under the influence of treatment with Actovegin [6, 7, 10, 17]. Although it is not possible to reasonably judge the antidepressant properties of the drug, one cannot ignore the fact that during treatment with Actovegin there was a decrease in the severity or disappearance of depressive symptoms, especially since none of the patients received antidepressant therapy during the period of treatment with Actovegin. A decrease in the severity of affective disorders as a result of treatment with Actovegin was previously noted in a study by Kuntz (2004), where depressive disorders were detected in 53.3% of patients with MCI.
Of particular interest is the fact that the positive therapeutic effect continued to increase after the end of the Actovegin therapy course, which indicates not only the persistence of the improvement, but also its possible impact on the mobilization of compensatory mechanisms.
[]MCI syndrome in a number of works by domestic neurologists [3] is called moderate cognitive disorder (MCI).
New aspects of the use of Actovegin: from mechanisms of action to clinical effects
The results of studies evaluating the effect of the drug Actovegin on the functional activity of the microvascular endothelium, in particular the functional state of the microvascular smooth muscle apparatus, are presented. Due to its endothelial protective properties, Actovegin can be used to correct endothelial dysfunction in neurological, therapeutic, endocrinological and surgical patients.
Currently, the universality of the mechanisms of cell damage under various types of pathological influences has been proven. The final link in inflammation, ischemia, and stress is a violation of redox reactions, metabolism and energy supply to cells [1]. Today, neuroprotection, neuroplasticity and neurogenesis are considered fundamental neurobiological processes that participate in the implementation of endogenous protective activity, resist pathophysiological damaging mechanisms and stimulate endogenous recovery [2].
The classical concept of neuroprotection involves suppression of individual pathophysiological mechanisms of damage when using an appropriate drug [3]. Impaired transport and utilization of glucose is one of the leading pathogenetic mechanisms of cell apoptosis. The action of various drugs is aimed at enhancing the delivery of glucose into cells, inhibiting the oxidation of long-chain fatty acids in mitochondria and indirectly enhancing the oxidation of glucose. This leads to an increase in the synthesis of adenosine triphosphate and the neutralization of oxygen radicals, the production of which increases under ischemic conditions [4].
Today, one of the best approaches to neuroprotection is the use of pleiotropic drugs. Pleiotropic action involves a simultaneous modulating effect on various damaging pathological mechanisms (hypoxia, oxidative stress, excitotoxicity, inflammation, apoptosis and many others) [3]. The drug of biological origin Actovegin has these properties.
Actovegin is a highly purified, protein-free derivative of calf blood, obtained by ultrafiltration and consisting of more than 200 biological substances. The molecular weight of the organic compounds that make up the drug does not exceed 5000 daltons [5]. The main components of Actovegin are amino acids, biogenic amines and polyamines, sphingolipids, hexoses, eicosanoids, succinate, choline, vitamins, adenosine monophosphate, inositol phosphooligosaccharides, as well as macroelements (magnesium, sodium, calcium, phosphorus) and neuroactive microelements (silicon, copper). The macro- and microelements that make up Actovegin are part of neuropeptides, enzymes and amino acids, and therefore are recognized and absorbed by neurons much better than macro- and microelements that enter the body in the form of salts.
The metabolic effect of Acto-vegin consists primarily of enhancing the utilization of oxygen and the transfer of glucose into cell mitochondria. Various experimental models have shown that Actovegin, by influencing oxidative phosphorylation in mitochondria, increases oxygen production by cells by almost 40% [6, 7]. In addition, Actovegin is able to enhance the transport of glucose into the cell. It was found that the active fraction of the drug, including inositol phosphooligosaccharides, activates the transport of glucose into the cell through the activation of transport proteins (GLUT1, GLUT4), without involving insulin receptors. This is of great clinical importance, for example, in type 2 diabetes mellitus against the background of insulin resistance [8].
Actovegin has a neuroprotective effect and, in particular, has a pronounced antioxidant effect. According to in vitro data, Actovegin improves metabolism in cells, increases the number of neuronal synapses, reduces the level of markers of apoptosis induction (caspase 3) and the formation of reactive oxygen species in cells. These effects are dose-dependent [9, 10]. Similar results were obtained in recent experimental work.
MM. Yurinskaya et al. (2014) found that the use of Actovegin leads to a decrease in apoptosis of human neuroblastoma cells induced by hydrogen peroxide and suppression of intracellular signaling pathways involved in the mechanism of cell death [11].
L.G. Khaspekov et al. (2014) [12], studying the protective effect of Actovegin in a model of glutamate toxicity, found that the drug at a dose of 1 mg/ml has a neuroprotective effect, expressed in a decrease in cell death and most likely associated with the action of glutamate in rat cerebellar neurons.
Actovegin also demonstrated a neuroprotective effect in severe neuropathy in a model of streptozotocin-induced diabetes in rats. According to A. Dieckmann et al. (2011), Actovegin significantly improved conductivity in sensory nerve fibers and reduced the activity of poly-ADP-ribose polymerase, a nuclear enzyme whose excessive activation can trigger cell death processes in conditions such as cerebrovascular diseases and diabetic polyneuropathy [13].
In a study by S. Mielin et al. (2014) on a model of total cerebral ischemia in rats with occlusion of four main arteries of the brain, Actovegin contributed to better survival of neurons in the CA1 zone of the hippocampus compared to placebo [14]. This observation was accompanied by a large number of surviving individuals in the Actovegin group and significantly better results in the Morris water maze test.
In addition to Actovegin’s ability to improve cellular metabolism and have a neuroprotective effect, a number of studies have noted the drug’s effect on the microvascular endothelium.
In a pilot study by A.A. Fedorovich on 28 healthy volunteers, it was revealed that Actovegin has a direct endothelial protective effect at the level of the microvascular bed [15]. The obtained results were subsequently confirmed in a population of patients with obliterating diseases of the arteries of the lower extremities, as well as with arterial hypertension.
According to the results of another study, intravenous infusions of Actovegin improved microcirculation parameters due to the endothelial protective effect and had a positive effect on the course of the disease. Patients receiving the drug were able to walk longer distances without pain [16].
The effectiveness of the drug was assessed in patients with arterial hypertension and moderate vascular cognitive impairment. Despite adequate lipid-lowering and antihypertensive therapy with the achievement of target blood pressure levels, cognitive disorders persisted in the comparison group (decrease in voluntary attention indicators), while in the Actovegin group it was possible to level out the cognitive deficit. In addition, during Actovegin therapy, a significant increase in the number of functioning capillaries at rest was noted, that is, a decrease in the elements of functional rarefaction of the microvasculature observed in patients with arterial hypertension [17].
V.V. Zakharov and V.B. Sosnin assessed the therapeutic effect of Actovegin on cognitive functions in patients with type 2 diabetes mellitus [18]. The patients were divided into two subgroups: the first - with the presence of concomitant arterial hypertension, signs of coronary heart disease and hemodynamically significant stenosis of the carotid arteries, the second - with the absence of the above pathology. After a three-month course of therapy, the greatest dynamics in indicators of concentration, short-term memory, visual-motor coordination and regulation of mental activity were observed in the group of patients in whom diabetes was combined with other clinically significant cardiovascular risk factors. Cognitive impairment in this category of patients, along with other factors, is based on tissue hypoxia caused by micro- and macrovascular damage. It is likely that Actovegin may have an additional positive effect in vascular cognitive disorders associated with damage to small vessels by improving microcirculatory parameters.
Thus, based on a number of experimental and clinical data, we can conclude that Actovegin, having many positive effects (antihypoxic, metabolic, neuroprotective and endothelial protective), is one of the promising drugs for the correction of hypoxic-ischemic damage, endothelial dysfunction, and microcirculatory disorders. Actovegin can be recommended as the drug of first choice for neurological and therapeutic patients: with acute or chronic cerebral ischemia and concomitant cardiovascular diseases, diabetes mellitus complicated by diabetic polyneuropathy, moderate and severe cognitive impairment in persons who have suffered a stroke. Therapeutic regimens used for the use of Actovegin in chronic ischemic conditions: 10–20 ml (400–800 mg) per 200 ml of saline intravenously in a course of seven to ten days, then one or two tablets (200–400 mg) three times a day within one to two months. In the presence of mnestic-intellectual disorders in elderly people - up to 12 weeks, two to three tablets three times a day. Repeat courses after six to eight months.