In Russia, a government decree came into force, which included drugs based on pregabalin, tapentadol and tropicamide in the list of potent and toxic substances, the circulation of which is regulated by the Criminal Code. All three drugs are included in the list of vital and essential drugs (VED).
Previously, drugs with these active ingredients were included in the list of medicines for medical use, which are subject to subject-quantitative accounting. Pharmacies were required to sell them strictly according to prescription, otherwise they faced administrative liability.
Question and answer Which drugs are included in the list of potent substances?
Now the sale of drugs based on pregabalin, tapentadol and tropicamide without a prescription faces criminal liability under Art. 234 of the Criminal Code of the Russian Federation (“Illegal trafficking of potent or toxic substances for the purpose of sale”). Punishment threatens not only sellers, but also citizens for the illegal manufacture, processing, acquisition, storage or illegal sale of these drugs. Maximum liability under Art. 234 is imprisonment for up to 8 years and a fine of up to 200 thousand rubles.
The Ministry of Health said that the tightening of penalties for dispensing drugs based on pregabalin, tapentadol and tropicamide without a prescription is due to the fact that they are often abused by drug addicts.
What are medications containing tropicamide used for?
The active ingredient tropicamide is used in eye drops. They are prescribed for spasms in the muscles responsible for focusing vision - when a person with poor vision who does not use glasses strains the eye muscles too much to see something.
Most often, such drugs are used to examine the fundus. Tropicamide drops temporarily dilate the patient's pupil, allowing the doctor to perform the procedure. This effect lasts for 4-6 hours, after which the pupil returns to its original size. In addition, drugs with tropicamide can be used in ophthalmology in the treatment of inflammatory processes, as well as in surgery, before and after ophthalmic operations.
During the action of the drug, tropicamide blocks the receptors of the iris of the eye. Therefore, doctors advise patients to refrain from driving a car and activities that require increased concentration and speed of psychomotor reactions for several hours. In addition, drops with this active substance are not recommended for use by people with glaucoma, increased intraocular pressure and eye hypersensitivity.
Palexia
| The above information on the use of this drug is presented for informational purposes only and is intended for specialists. For more complete information, please refer to the manufacturer's instructions included in the package. Before starting to use any drug, it is recommended to consult a doctor. |
Trade name of the drug: Palexia
International nonproprietary name: Tapentadol
Dosage form: Long-acting film-coated tablets
Active ingredient: Tapentadol
Pharmacotherapeutic group: Analgesic narcotic
Pharmacological properties:
Tapentadol is a powerful analgesic that is an opioid μ-receptor agonist and a norepinephrine reuptake inhibitor. Tapentadol directly has an analgesic effect without the participation of pharmacologically active metabolites.
Tapentadol has demonstrated effectiveness in pain of nociceptive, neuropathic, visceral origin and in pain caused by the inflammatory process. During clinical studies of the drug for back pain, cancer and non-cancer pain, the analgesic effectiveness of tapentadol was confirmed.
Effect on the cardiovascular system: with careful study of the QT interval, no effects from taking therapeutic or exceeding therapeutic doses of tapentadol on the QT interval were established. Tapentadol had no significant effects on other ECG parameters (heart rate, PR interval, QRS complex, T and U wave morphology).
Pharmacokinetics
Suction
The average absolute bioavailability of tapentadol after oral administration of a single dose on an empty stomach in extended-release film-coated tablets is approximately 32% due to extensive first-pass metabolism. Cmax of tapentadol in blood plasma is observed between 3 and 6 hours after oral administration of extended-release film-coated tablets.
A dose-proportional increase in AUC (the most significant parameter for extended-release dosage forms) was observed after oral administration of extended-release tablets within the therapeutic dose range.
Long-term oral administration of tapentadol twice daily at doses of 86 mg and 172 mg extended-release tablets showed an accumulation coefficient of approximately 1.5, which was mainly determined by the dosing interval and T1/2 of tapentadol. Css of tapentadol in blood plasma is achieved on the second day after the start of oral administration of long-acting film-coated tablets.
Food influence
The AUC and Cmax of tapentadol increased by 8% and 18%, respectively, when oral extended-release tablets were administered after a high-fat, high-calorie meal. The time to reach Cmax is delayed by 1.5 hours when eating high-calorie foods. This was considered clinically insignificant. The drug Palexia can be taken orally both before and after meals.
Distribution
Plasma protein binding is low and does not exceed 20%. Tapentadol has a large Vd. After intravenous administration of tapentadol, Vd in the terminal elimination phase is 540 ± 98 l.
Metabolism
Tapentadol undergoes extensive metabolism. About 97% of the compound is metabolized. The main route of metabolism of tapentadol is conjugation with glucuronic acid. After oral administration, approximately 70% of the dose is excreted in the urine in the form of conjugated forms (55% glucuronide and 15% tapentadol sulfate). Uridine diphosphate glucuronyl transferase (UGT) is the main enzyme involved in the process of glucuronidation (mainly isoenzymes UGT1A6, UGT1A9 and UGT2B7). A total of 3% of tapentadol is excreted unchanged in urine. Tapentadol is also metabolized to N-desmethyltapentadol (13%) by the CYP2C9 and CYP2C19 isoenzymes and to hydroxytapentadol (2%) by the CYP2D6 isoenzyme, which are further conjugated. For this reason, the metabolism of tapentadol, mediated through the cytochrome P450 isoenzyme system, is of less importance compared to glucuronidation.
None of the tapentadol metabolites have an analgesic effect.
Removal
Tapentadol and its metabolites are excreted almost completely (99%) by the kidneys. The total clearance after intravenous administration is 1530±177 ml/min. The final T1/2 after taking tapentadol orally in extended-release film-coated tablets averages 5-6 hours.
Pharmacokinetics in special clinical situations
Elderly patients. The AUC of tapentadol is similar in elderly (65-78 years) and middle-aged patients (19-43 years), with the average Cmax being 16% lower in elderly patients than in middle-aged patients.
Renal dysfunction. The AUC and Cmax of tapentadol are comparable in patients with varying degrees of renal function (from normal to severely impaired). Conversely, with increasing severity of renal failure, an increase in the AUC of tapentadol-O-glucuronide was observed. In patients with mild, moderate and severe renal impairment, tapentadol-O-glucuronide AUC increased by 1.5, 2.5 and 5.5 times compared with patients with normal renal function, respectively.
Liver dysfunction. In patients with hepatic impairment, oral tapentadol was characterized by higher AUC and serum concentrations compared to patients with normal hepatic function. The tapentadol pharmacokinetic ratios for the groups of patients with mild and moderate hepatic impairment when compared with the group of patients with normal liver function were 1.7 and 4.2, respectively, for AUC; 1.4 and 2.5 respectively for Cmax; and 1.2 and 1.4 respectively for T1/2. The rate of formation of tapentadol-O-glucuronide is lower in patients with more severe liver dysfunction.
Pharmacokinetic interaction
Tapentadol is mainly metabolized through phase 2 (glucuronidation), and only a small amount is metabolized through phase 1 oxidative processes. Because glucuronidation is a high capacity, low affinity system, any clinically significant interaction associated with glucuronidation is unlikely. This was confirmed by the experience of simultaneous use of tapentadol with naproxen and probenecid; an increase in the AUC of tapentadol by 17% and 57%, respectively, was observed. When used simultaneously with paracetamol and acetylsalicylic acid, no changes in the pharmacokinetic parameters of tapentadol were observed.
A study of the possible effect of metoclopramide and omeprazole on the absorption of tapentadol did not reveal a clinically significant effect on the concentration of tapentadol in the blood plasma.
Tapentadol is not an inducer or inhibitor of cytochrome P450 isoenzymes. Therefore, clinically significant interactions mediated through the cytochrome P450 isoenzyme system are unlikely.
The binding of tapentadol to plasma proteins is low (approximately 20%). For this reason, the likelihood of a pharmacokinetic interaction due to displacement from plasma proteins is low.
Indications for use:
- chronic pain syndrome of moderate and severe severity.
The drug is used only for pain of moderate and severe intensity, requiring the prescription of opioid analgesics.
Contraindications:
- hypersensitivity to tapentadol or any of the excipients included in the drug;
- in situations where opioid μ-receptor agonists are contraindicated, i.e. in patients with significant respiratory depression (if observation is impossible or in the absence of resuscitation equipment), as well as in patients with exacerbation or severe bronchial asthma or hypercapnia;
- presence or suspicion of paralytic intestinal obstruction;
- acute intoxication with alcohol, hypnotics, centrally acting analgesics and psychotropic drugs;
- in patients receiving MAO inhibitors or who have taken them within the last 14 days;
- severe renal failure;
- severe liver failure;
— age up to 18 years;
- lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
Carefully
- with an increased risk of misuse or abuse of the drug;
- in case of respiratory dysfunction;
— in patients with traumatic brain injury and depression of consciousness;
- in patients with a history of seizures or any conditions that increase the risk of developing seizures;
- in patients with moderate liver failure;
- in patients with pathology of the biliary tract and acute pancreatitis;
- in patients with low blood pressure.
It is recommended to gradually reduce the dose of Palexia before complete discontinuation.
Caution is required when using Palexia concomitantly with serotonergic drugs.
Use during pregnancy and breastfeeding
Data on the use of tapentadol during pregnancy are limited. Animal studies have not demonstrated teratogenicity associated with tapentadol. However, at doses exceeding the upper therapeutic limit, embryonic development delay and embryotoxicity (CNS effects associated with agonism to opioid μ-receptors) were detected. An effect on the postnatal development of the offspring was detected when tapentadol was administered in doses that did not cause adverse events in pregnant females.
The use of the drug Palexia during pregnancy is permissible if the potential benefit to the mother outweighs the potential risk to the fetus.
The effect of tapentadol when used during labor is unknown. The use of tapentadol during labor and immediately before childbirth is not recommended. Due to tapentadol's affinity for opioid μ receptors, neonates whose mothers have taken tapentadol should be closely monitored for the possibility of respiratory depression.
Information on the excretion of tapentadol into breast milk is limited. Physicochemical and pharmacodynamic/toxicological data for tapentadol indicate excretion in breast milk, so the risk of exposure to the breast-fed infant cannot be excluded. The drug Palexia should not be prescribed during breastfeeding.
Use for liver dysfunction
No dose adjustment is required in patients with mild hepatic impairment. Caution must be exercised when prescribing Palexia to patients with moderately severe liver failure. Treatment of such patients should begin with 50 mg of tapentadol in extended-release film-coated tablets, no more than once a day. Further therapy should be aimed at maintaining the analgesic effect with an acceptable level of tolerability. There is no experience of use in patients with severe liver dysfunction, therefore use in this group of patients is contraindicated.
Use for renal impairment
No dosage adjustment is required in patients with mild or moderate renal impairment. There is no experience of use in patients with severe renal impairment, therefore the use of the drug in this group of patients is contraindicated.
Use in children
Palexia is contraindicated for use in patients under 18 years of age due to insufficient data on efficacy and safety.
Use in elderly patients
In general, recommended doses for elderly patients with normal hepatic and renal function are the same as for middle-aged patients with normal renal and hepatic function. Because elderly patients are more likely to have decreased renal and hepatic function, care should be taken when selecting dosages and not exceeding recommended dosages.
Interaction with other drugs:
Concomitant use of tapentadol with benzodiazepines, barbiturates and opioids (analgesics, antitussives and withdrawal agents) may increase the risk of respiratory depression. Drugs that depress the activity of the central nervous system (benzodiazepines, antipsychotics, histamine H1 receptor blockers, opioids, alcohol) may enhance the sedative effect of tapentadol and depression of the central nervous system. If a combination of tapentadol and drugs that cause respiratory or central nervous system depression is necessary, consider reducing the dose of the drugs.
Opioid receptor agonists-antagonists. Caution should be exercised when tapentadol is used concomitantly with μ-opioid agonists (eg, pentazocine, nalbuphine) or partial μ-opioid agonists (eg, buprenorphine). The need to increase the dose of the μ-opioid agonist has been noted when used concomitantly with buprenorphine, and careful monitoring for adverse effects such as respiratory depression is necessary in these circumstances.
There are isolated reports of the development of serotonin syndrome coinciding with the simultaneous use of tapentadol and serotonergic drugs, for example, selective serotonin reuptake inhibitors (SSRIs). Possible symptoms of serotonin syndrome include, for example: confusion, agitation, fever, sweating, ataxia, hyperreflexia, myoclonus and diarrhea. Discontinuation of serotonergic medications usually resulted in rapid resolution of symptoms. Therapy is determined by the nature and severity of symptoms.
Since the main route of metabolism of tapentadol is conjugation with glucuronic acid involving the isoenzymes UGT1A6, UGT1A9 and UGT2B7, simultaneous use with potent inhibitors of these isoenzymes (such as ketoconazole, fluconazole, meclofenamic acid) may increase the systemic exposure of tapentadol.
Patients being treated with tapentadol should be careful when starting and stopping concomitant use of potent liver enzyme inducers (e.g., rifampicin, phenobarbital, St. John's wort), as this may result in a corresponding decrease in effectiveness or risk of side effects.
Tapentadol is contraindicated in patients receiving MAO inhibitors or who have taken them in the last 14 days, because it is possible to increase the content of norepinephrine, which can cause side effects from the cardiovascular system, such as a hypertensive crisis.
Directions for use and dosage:
As with the treatment of other analgesics with a central mechanism of action, the dose of the drug should be selected individually in accordance with the severity of the pain syndrome, previous therapy and the ability to monitor the patient. The drug Palexia in extended-release film-coated tablets should be taken twice a day, approximately every 12 hours, regardless of meals. The tablet must be taken orally with a sufficient amount of liquid, without chewing, breaking or dissolving.
Start of treatment
Patients not taking narcotic analgesics: therapy should begin with a dose of 50 mg 2 times a day.
Patients taking narcotic analgesics: when switching from other narcotic analgesics to Palexia and choosing the initial dose, the characteristics of the previously prescribed drug, the frequency of its use and the average daily dose should be taken into account.
Dose selection and maintenance therapy
After starting treatment, under close medical supervision, the dose should be adjusted individually until adequate pain relief is achieved with a minimum of side effects. Current experience shows that a tapentadol dose titration regimen of 50 mg 2 times a day every 3 days is sufficient in most patients to achieve adequate pain control.
A daily dose of tapentadol exceeding 500 mg in extended-release film-coated tablets has not been prescribed, so the drug is not recommended for use in such doses.
Completion of treatment
If you immediately stop taking tapentadol, withdrawal syndrome may develop. It is recommended to gradually reduce the dose of the drug before complete discontinuation in order to prevent the development of withdrawal syndrome.
Adults with chronic diseases
No dose adjustment is required in patients with mild to moderate renal impairment. There is no experience of use in patients with severe renal impairment, therefore the use of the drug in this group of patients is contraindicated.
No dose adjustment is required in patients with mild hepatic impairment. Caution must be exercised when prescribing Palexia to patients with moderately severe liver failure. Treatment of such patients with tapentadol in the form of extended-release film-coated tablets should begin with a dose of 50 mg no more than 1 time/day. Further therapy should be aimed at maintaining the analgesic effect with an acceptable level of tolerability. There is no experience of use in patients with severe liver dysfunction, therefore use in this group of patients is contraindicated.
In general, recommended doses for elderly patients (65 years and older) with normal hepatic and renal function are the same as for middle-aged patients with normal renal and hepatic function. Because elderly patients are more likely to have decreased renal and hepatic function, care should be taken when selecting dosages and not exceeding recommended dosages.
Palexia is contraindicated for use in children under 18 years of age due to insufficient data on efficacy and safety.
Special instructions:
Possible abuse of the drug
There is a potential risk of abuse of Palexia. This should be taken into account when prescribing the drug in situations where there is a risk of misuse, abuse of the drug, or transfer of the drug to others.
All patients treated with μ-opioid agonist drugs should be closely monitored for drug abuse and dependence.
Respiratory depression
At high doses and in patients with hypersensitivity to μ-opioid agonists, tapentadol may cause dose-dependent respiratory depression. For this reason, Palexia should be administered with caution to patients with respiratory dysfunction. The use of non-opioid agonist analgesics should be considered, and Palexia should only be used in these patients under close medical supervision and in the lowest effective doses. Respiratory depression should be treated as for respiratory depression with any other μ-opioid agonist.
Traumatic brain injury and increased intracranial pressure
As with other drugs - agonists of opioid μ-receptors, tapentadol should not be prescribed to patients who may be particularly sensitive to the pathophysiological reactions that develop with an increase in the partial pressure of carbon dioxide in the intracranial vessels and brain tissue, for example, with increased intracranial pressure, depression consciousness or coma. Analgesics with affinity for opioid μ receptors may mask the clinical manifestations of traumatic brain injury. Palexia should be used with caution in patients with traumatic brain injury and brain tumors.
Convulsions
There have been no systematic studies of tapentadol in patients with seizures. However, like other analgesics with an affinity for μ-opioid receptors, Palexia should be administered with caution to patients with a history of seizures or any conditions that place the patient at risk of developing seizures.
Liver failure
In patients with mild and moderate hepatic impairment, a 2-fold and 4.5-fold increase in systemic exposure was detected, respectively, compared to patients with normal liver function. Palexia should be used with caution in patients with moderate hepatic impairment. The drug Palexia has not been studied in patients with severe liver dysfunction and is therefore contraindicated for use in this group of patients.
Use for pathology of the pancreas and bile ducts
Drugs with affinity for opioid μ receptors can cause spasm of the sphincter of Oddi. Palexia should be used with caution in patients with biliary tract pathology and acute pancreatitis.
Withdrawal syndrome
If you immediately stop taking tapentadol, withdrawal syndrome may develop. The following symptoms may occur: anxiety, increased sweating, insomnia, chills, pain, nausea, tremors, diarrhea, upper respiratory symptoms, piloerection and, rarely, hallucinations. In order to prevent withdrawal syndrome, it is recommended to gradually reduce the dose of the drug before complete withdrawal.
Decreased blood pressure
The drug Palexia can cause a significant decrease in blood pressure, especially in patients with hypovolemia or taking drugs simultaneously with tapentadol that reduce peripheral vascular tone (for example, phenothiazine derivatives, anesthetics).
Serotonin syndrome
There are reports of the development of life-threatening serotonin syndrome with the simultaneous use of tapentadol, even in therapeutic doses, with serotonergic drugs: selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors, tricyclic antidepressants, triptans, drugs that affect serotonergic transmission in the central nervous system (eg, mirtazapine, trazodone and tramadol), and drugs that interfere with serotonin metabolism (eg, MAO inhibitors). Possible symptoms of serotonin syndrome may include, for example: confusion, agitation, coma, tachycardia, fever, incoordination, nausea, vomiting and diarrhea.
Tapentadol should be used with caution in patients with adrenocortical insufficiency (eg, Addison's disease), in patients with delirium tremens, toxic psychosis, in patients with myxedema and hypothyroidism, as well as in prostatic hypertrophy and urethral strictures.
Impact on the ability to drive vehicles and machinery
Like other drugs - agonists of opioid μ-receptors, Palexia can negatively affect the ability to drive vehicles and operate complex mechanisms, because has an effect on the central nervous system. This effect is especially often possible at the beginning of treatment, with any changes in the dose of the drug, or when taken simultaneously with tranquilizers or alcohol. Patients should refrain from driving and engaging in potentially hazardous activities.
Side effects:
Approximately 60% of patients taking Palexia extended-release film-coated tablets experienced adverse reactions, mostly of mild or moderate intensity. The most common of these were gastrointestinal and central nervous system disorders (nausea, dizziness, constipation, headache and drowsiness).
The table shows the adverse reactions of the drug Palexia identified during its use. Determination of the categories of frequency of adverse reactions: very often (≥1/10), often (≥1/100, <1/10), uncommon (≥1/1,000, <1/100), rarely (≥1/10,000, <1/1,000), very rare (<1/10,000).
Very common (≥1/10) Common (≥1/100 to <1/10) Uncommon (≥1/1,000 to <1/100) Rare (≥1/10,000 to <1/1,000) From the side of the immune system, hypersensitivity* From the side of metabolism, loss of appetite, loss of body weight. Mental disorders, sleep disturbances, anxiety, depressed mood, increased excitability, restlessness, unusual dreams, disturbances of perception, disorientation in place and time, psychomotor agitation, confusion, euphoria, drug dependence, pathological thinking. From the nervous system, dizziness, headache. pain drowsiness involuntary muscle contractions tremor attention disorders paresthesia hypoesthesia imbalance sedation fainting memory impairment cognitive impairment depression of consciousness dysarthria coordination problems pre-syncope convulsions Visual impairment visual impairment Cardiovascular system hot flashes increased heart rate decreased heart rate palpitations decreased blood pressure Side effects respiratory system shortness of breath respiratory depression From the digestive system nausea constipation vomiting diarrhea dyspepsia abdominal discomfort impaired evacuation of stomach contents From the skin and subcutaneous tissues itching hyperhidrosis rash urticaria From the urinary system pollakiuria difficulty urinating From the reproductive system and mammary gland Sexual dysfunction General reactions fatigue dryness mucous membranes (mouth, eyes and throat) asthenia sensation of changes in body temperature swelling withdrawal symptoms irritability unusual sensations feeling intoxicated feeling relaxed
* Rare cases of angioedema, anaphylaxis and anaphylactic shock have been reported during post-marketing use of the drug.
When taking the drug Palexia orally in long-acting film-coated tablets for up to 1 year, cases of mild withdrawal syndrome were observed with abrupt interruption of therapy; their severity was classified as mild. However, physicians should consider the possibility of withdrawal syndrome and provide necessary treatment if it occurs.
The risk of suicidal thoughts is higher in patients suffering from chronic pain. In addition, drugs with a pronounced effect on the monoaminergic system increase the risk of suicidal behavior in patients suffering from depression, especially at the beginning of treatment. Clinical studies and post-marketing experience with tapentadol have shown no evidence of an increased risk. If any side effects indicated in the instructions occur, or other side effects not listed in the instructions are noticed, tell your doctor.
Overdose:
Data on overdose are very limited.
Symptoms: one should expect the symptoms inherent in all drugs that have a central analgesic effect and are characterized by an affinity for opioid μ-receptors - miosis, vomiting, collapse, depression of consciousness up to coma, convulsions and respiratory depression with the possibility of stopping it.
Treatment: Treatment of overdose should focus on eliminating symptoms of μ-opioid receptor stimulation. If tapentadol overdose is suspected, the focus should be on establishing the airway and administering controlled or monitored ventilation. Full opioid receptor antagonists, such as naloxone, are specific antidotes for respiratory depression associated with narcotic analgesic overdose. Respiratory depression following overdose may exceed the duration of action of the opioid receptor antagonist. Prescribing an opioid receptor antagonist does not replace continuous monitoring of the condition of the respiratory tract, monitoring of respiratory and circulatory disorders that have developed as a result of an overdose of narcotic analgesics. If the response to opioid receptor antagonists is insufficient or short-lived, additional administration of an opioid receptor antagonist may be possible.
Gastrointestinal cleansing may be performed to remove unabsorbed tapentadol. The use of activated charcoal or gastric lavage can be performed within 2 hours after ingestion. Before cleansing the gastrointestinal tract, it is necessary to secure the respiratory tract.
Storage conditions:
The drug should be stored out of the reach of children at a temperature not exceeding 30°C. Shelf life: 3 years.
Conditions for dispensing from pharmacies: By prescription.
Manufacturer: GRUNENTHAL GmbH, Germany (4032129036925, 4032129036970, 4032129082113, 4011548022733)
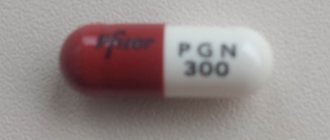
Who is prescribed medications with pregabalin?
Pregabalin-based medications are classified as antiepileptic and anti-anxiety drugs. They have analgesic and anticonvulsant effects and are usually available in capsule form.
Medicines containing pregabalin are used as adjunctive therapy for epilepsy: they reduce the frequency of seizures. The drug is also prescribed for the treatment of generalized anxiety disorder (a mental disorder characterized by general, persistent anxiety). In addition, pregabalin helps relieve neuropathic pain that occurs in the presence of pathological processes in the peripheral and central nervous system, as well as fibromyalgia syndromes, a disease that is accompanied by chronic, predominantly symmetrical pain throughout the body.
Article on the topic
Death in the medicine cabinet. What common medications are extremely dangerous?
Preparations containing pregabalin are not used to treat children and adolescents under 17 years of age. Restrictions also apply to patients with renal and chronic heart failure.
Tapentadol is included in the PCU list
From August 26, 2021, by order of the Russian Ministry of Health dated July 27, 2018 N 471n, Tapentadol was included in the list of medicines subject to subject-quantitative accounting.
Tapentadol is an opioid narcotic analgesic, but is not included in the List of Narcotic Drugs and Psychotropic Substances. The instructions for the drug note that there is a potential risk of abuse of tapentadol. This should be taken into account when prescribing it in situations where there is a risk of misuse, abuse or transfer to others. All patients treated are subject to close monitoring for tapentadol abuse and dependence.
From August 26, 2021:
- all actions with tapentadol must be recorded in a special subject-quantitative register in accordance with Order of the Ministry of Health of Russia dated June 17, 2013 N 378n;
— tapentadol must be stored in wooden or metal locked cabinets in accordance with the requirements of Order of the Ministry of Health and Social Development of Russia dated August 23, 2010 N 706n;
— tapentadol must be prescribed on prescription forms, form N 148-1/u-88, in accordance with the requirements of Order of the Ministry of Health of Russia dated December 20, 2012 N 1175n.
Prescriptions for a medicinal product under the international nonproprietary name Tapentadol, issued on prescription forms of form N 107-1/u before August 26, 2021, are valid until their expiration date.
It should be noted that failure to comply with the rules for subject-quantitative accounting of medicinal products is a violation of licensing requirements when carrying out medical activities - see paragraphs. “c_1” clause 5 of the Regulations on licensing of medical activities.
Tapentadol (and with it Pregabalin and Tropicamide) is also planned to be included in the list of potent substances approved by Decree of the Government of the Russian Federation of December 29, 2007 N 964, which will make it possible to bring those responsible for the illegal distribution of these drugs to criminal liability under Article 234 of the Criminal Code of the Russian Federation.
Dear readers, if you liked the review, do not forget to like and subscribe to new articles and reviews, and share with colleagues!
For legal assistance, you can contact medical lawyer Vadim Sergeevich Berezinsky in the professional community VKontakte https://vk.com/medicinskijyurist .
What is the medicine tapentadol?
Tapentadol is a powerful opioid analgesic used for acute and chronic pain of moderate to severe intensity. Preparations with this active substance are usually produced in the form of tablets and are used for nociceptive pain (occurs in response to irritation of pain receptors), neuropathic (appears due to pathological excitation of neurons in the peripheral or central nervous system), visceral (caused by increased pressure in the stomach cavity and intestines when they are stretched or contracted) in nature, as well as due to pain caused by the inflammatory process. In addition, medications based on tapentadol are used for postoperative, orthopedic, cancer pain, back pain, and chronic pain due to osteoarthritis.
Tapentadol is not used to treat patients under 18 years of age. It is also contraindicated in cases of exacerbation or severe bronchial asthma, paralytic ileus, acute alcohol intoxication, severe renal or liver failure. It should not be used together with hypnotics, centrally acting analgesics and psychotropic drugs.
Introduction
Osteoarthritis (OA) is one of the most common causes of chronic pain, along with low back pain and headaches.
The number of patients suffering from OA is constantly increasing due to the aging population and the increasing prevalence of obesity. Pain caused by the severity of OA not only leads to patient disability and deterioration in quality of life, but also reduces its duration, being a significant predictor of the risk of death [1]. Patients with OA use various painkillers and methods, among which nonsteroidal anti-inflammatory drugs (NSAIDs) remain the undoubted leader. However, despite the treatment, from 27 to 61% of patients continue to experience chronic pain (CP) and are not satisfied with therapy [2].
Features of pain syndrome in osteoarthritis
The main cause of pain in OA is considered to be inflammatory and degenerative changes in the joint and periarticular tissues. However, examination and observation of patients with OA in some cases indicate that the intensity of pain does not always correlate with destructive changes [3] and surgical treatment often does not relieve the patient of pain. Up to 44% of patients after adequately performed knee replacement and up to 27% of hip replacement continue to experience pain [4].
These facts can be explained by the fact that the pain syndrome in OA can be mixed, including signs of nociceptive pain and pain due to central sensitization (CS) [5].
Central nervous system is defined as an increase in nerve signals in the central nervous system, which provides hypersensitivity to pain - in other words, it is the hyperexcitability of central nociceptors, as a result of which their excitation threshold decreases and they themselves begin to generate pain impulses, becoming a source of pain [6, 7]. For the first time, CS during the formation of CB was described by C. Woolf in 1983 [8]. Long-term inflammation in the joint leads to hypersensitivity of peripheral afferent neurons, i.e. peripheral sensitization is formed [9]. With ongoing peripheral sensitization, neuroplastic changes occur in the central nervous system and CS occurs, which is the main mechanism of the pathogenesis of chronic pain syndrome [3, 10].
The CS is accompanied by the following phenomena: a progressive increase in neuronal activity (wind-up phenomenon), in which neurons become more susceptible to repeated stimuli; increased sensitivity to pain in intact tissues located far from the damaged area (secondary hyperalgesia); an increase in the amplitude and duration of the neural response; a decrease in the excitation threshold when normally non-painful stimuli activate nociceptors (allodynia) [11, 12].
A classic example of CS is fibromyalgia, a disease in which there is neither inflammation nor damage to the joints [13], but the cause is dysfunction of the pain system. According to recent studies, CS phenomena can occur not only in fibromyalgia, but also in migraine, neck pain, pelvic pain, chronic fatigue syndrome, etc., as well as in rheumatic diseases [14–17].
As a result of chronic inflammation in the joint and its destruction, peripheral pain receptors are excited and pain impulses are transmitted along the peripheral nerves to the dorsal horns of the spinal cord. They are under the control of analgesic (antinociceptive) systems, the activity of which is aimed at modulating pain. Under conditions of continued excitation, in this case inflammation in the joint, and weakness of antinociceptive systems, CS occurs.
Compared with nociceptive CP, patients with CD report more intense pain, a greater impact on quality of life, more severe impairment of functional activity, depression and anxiety [18].
The causes of CS have not yet been established, but genetic and environmental factors can be discussed. If a patient has CS, then the clinical picture may show a rapid transition to CB and an insufficient response to treatment [19, 20].
CS in spinal and supraspinal pain neurons alters the clinical characteristics of pain syndrome. Neuropathic symptoms appear (burning, tingling, numbness, electric shocks, etc.), which, unlike neuropathic pain itself, are localized in anatomically illogical areas, i.e. Topically do not correspond to any lesion of the somatosensory nervous system. In OA, CS according to the Pain DETECT questionnaire occurs in 28–30% of patients [21–24], and up to 34% of patients use neuropathic characteristics of pain when describing their complaints [25].
The presence of CS in patients with OA is confirmed by a significantly lower pressure pain threshold compared to the healthy control group.
In a study by M. Imamura et al. [26] to determine the state of the nervous system in 62 women with knee OA, pressure pain thresholds in the muscles, ligaments, tendons and skin of the lower limb were assessed. It was shown that all patients with OA had significantly lower pressure pain thresholds. This decrease was correlated with high pain intensity, low quality of life, low functional activity and disability.
In another work, L. Arendt-Nielsen et al. [27] assessed CV by measuring pressure pain thresholds (at the joint and at a distant point) in 48 women with knee OA and 24 healthy women. Significantly lower pressure pain thresholds were found in patients with OA both in the joint area and at a distant point. An inverse correlation was shown between pain intensity values and average pressure pain thresholds at a distant point.
Pathogenetic therapy is most effective in the treatment of CB. By providing an anti-inflammatory effect in the area of the affected joint, NSAIDs can reduce nociceptive impulses. However, their use is associated with a high risk of developing adverse events from both the gastrointestinal tract and the cardiovascular system. Thus, patients with severe concomitant pathology require selection of pain therapy taking into account their medical history. Nociceptive impulses from the periphery play an important role in the clinical picture of CB, however, pharmacological agents of peripheral action are not able to reduce CV. Only centrally acting drugs can affect the processes involved in CS, therefore, along with traditional therapy, patients with signs of CS should be prescribed complex treatment, which also includes centrally acting drugs.
Opioid analgesic tapentadol PR
A new potent centrally acting analgesic, tapentadol PR, which has a dual mechanism of action, binds to mu-opioid receptors and also inhibits norepinephrine (NA) reuptake [28].
Mu receptors, the most studied type of opioid receptor, are located in the nervous system, as well as in the gastrointestinal tract and other tissues. Among the functions they regulate, nociception, breathing, memory, learning, secretion of neurohormones, intestinal contractile activity, etc. should be noted. When opioid receptors are activated, voltage-gated ion calcium channels in presynaptic neurons are closed and the release of excitatory mediators, such as glutamate, is reduced, and the activation of potassium channels in postsynaptic neurons leads to membrane hyperpolarization, which reduces the sensitivity of neurons to excitatory neurotransmitters and thus reduces the transmission of pain impulses [29].
NA is a key neurotransmitter in descending antinociceptive pathways. By inhibiting the reuptake of NA after its release at synapses, tapentadol increases the level of this neurotransmitter by activating α2 receptors. This increased receptor activation leads to suppression of pain transmission through second-order neurons. Inhibition of NA reuptake complements the effects of tapentadol on mu-opioid receptors and enhances its analgesic efficacy [30, 31].
Tapentadol is fundamentally different from its predecessor tramadol: the molecule is an active substance, tapentadol has no active metabolites, the main mechanism of metabolism is glucuronidation, tapentadol is 50 times weaker than morphine (tramadol is 6000 times weaker), the drug blocks the reuptake of NA, but not serotonin [32 , 33].
Tapentadol is prescribed to patients with severe to very severe pain. The dose is selected individually in accordance with the severity of the pain syndrome, previous therapy (lack of effect from NSAIDs) and the possibility of monitoring the patient. Tapentadol PR (extended release) should be taken twice daily with or without food. The tablet must be taken orally with a sufficient amount of liquid without chewing, breaking or dissolving. Patients who have not previously taken narcotic analgesics begin therapy with a dose of 50 mg 2 times a day, followed by titration if necessary. Current experience suggests that a tapentadol dose titration regimen of 100 mg per day every 3 days is sufficient for most patients to achieve adequate pain control [34].
The effectiveness of tapentadol was studied in patients with painful diabetic polyneuropathy [35]. The study involved 588 patients with polyneuropathy who were dissatisfied with previous pain therapy with opioid or non-opioid analgesics for 3 months, with persistent pain intensity of at least 5 points on the 11-point NRS (Numeric Rating Scale for pain). All patients received tapentadol for 3 weeks with the optimal individual dose titrated to 100–250 mg per day. Those patients who experienced a decrease in pain intensity of at least 1 point (n=395) were further divided into two groups. One group of patients received placebo, the second received an optimal fixed dose of tapentadol for 12 weeks.
The effectiveness of tapentadol has also been studied in the treatment of the neuropathic component of pain in patients with chronic back pain in combination with the anticonvulsant pregabalin. Monotherapy with tapentadol 500 mg/day (n=152) was compared with combination therapy with pregabalin 300 mg/day and tapentadol 300 mg/day (n=136). A significant decrease in neuropathic pain scores was observed in both groups. Secondary assessment of the effectiveness of treatment using the SF-12 and EQ-5D scales revealed similar positive dynamics both with tapentadol monotherapy and with tapentadol/pregabalin combination therapy. However, cases of nausea and drowsiness were observed significantly more often in patients on combination therapy [36].
Use of tapentadol PR for osteoarthritis
The effectiveness of tapentadol PR in the treatment of patients with OA has been assessed in several studies (see table).
In a randomized, double-blind, placebo-controlled, multicenter study, M. Afilalo et al. [37] evaluated the comparative effectiveness of tapentadol PR, oxycodone, and placebo in patients with OA over a 3-week titration period followed by a 12-week treatment and observation period. 1030 patients with chronic knee pain due to OA were randomized to receive tapentadol 100–250 mg twice daily, oxycodone 20–50 mg twice daily, or placebo. There was a significantly higher percentage of patients in the tapentadol group achieving a ≥50% reduction in pain intensity (32.0% [110/344]) compared with placebo (24.3% [82/337]; p=0.027). while in the oxycodone group this percentage was significantly lower (17.3% [59/342]; p=0.023). Undesirable side effects from the gastrointestinal tract were noted in 26.1% of patients in the placebo group, 43.0% during tapentadol therapy and in 67.3% of patients receiving oxycodone.
I. Steigerwald et al. [38] studied the effectiveness and tolerability of tapentadol PR in 195 patients with severe chronic bronchitis in OA, which was previously treated with various NSAIDs. The observation period included a 5-week tapentadol titration period (50–250 mg twice daily) followed by 7 weeks of therapy. The dynamics of pain intensity from the initial level was -3.4±2.10 (p<0.0001). Adverse events were detected in 38.5% of patients.
In a comparative randomized controlled open study, M. Banerjee et al. [39] patients with OA received tapentadol PR (100 mg twice daily; n=108) or etoricoxib (30 mg twice daily; n=110) for 12 weeks. Sustained improvement was noted in the form of a decrease in pain intensity on the visual analogue scale and the WOMAC index in both groups. However, at the end of the study, more patients in the tapentadol group reported a satisfactory response (p=0.036). Adverse events in the group with an opioid analgesic were observed less frequently than with NSAIDs (37.03 versus 49.09%). A. Serrie et al. also conducted a randomized trial to evaluate the efficacy and safety of tapentadol PR (100–250 mg twice daily) and oxycodone (20–50 mg twice daily) in patients with OA compared with placebo. The study, which included 990 patients, found that neither tapentadol nor oxycodone resulted in a significant reduction in pain intensity compared with placebo after 3 weeks of titration and 12 weeks of treatment. However, the overall health of patients receiving tapentadol was better than that of patients receiving oxycodone; the percentage of patients completing the study in the tapentadol group was higher than in the oxycodone group (56 vs. 42.5%). Tapentadol also demonstrated a better tolerability profile: there was a lower incidence of constipation (17.9 vs. 35%) and a combination of nausea/vomiting (23.8 vs. 46.8%) [40].
A pooled analysis of two randomized, double-blind, placebo-controlled trials by B. Lange et al. suggested that tapentadol PR is superior to oxycodone in providing pain relief and improving overall health in patients with CB and moderate-to-severe OA. Both studies consisted of a 3-week titration and 12-week treatment; Patients were randomized to tapentadol PR (100–250 mg twice daily), oxycodone CR (20–50 mg twice daily), or placebo. Treatment with tapentadol resulted in a greater reduction in mean pain intensity compared with oxycodone after both 12 weeks of treatment (mean difference -0.41 [95% CI: -0.65 to -0.16]; p=0.001) and during the maintenance period (-0.35 [95% CI: -0.58 to -0.12]; p=0.003). The general condition of patients in the tapentadol group according to the SF-36 scale and the EQ-5D quality of life index was also significantly higher than in the oxycodone group (p<0.001). Treatment with tapentadol was associated with fewer adverse side effects (vomiting, constipation, nausea, drowsiness, and itching) and fewer treatment discontinuations (42.2 vs. 64% for oxycodone) [41].
Tapentadol PR is also used for pain relief after joint replacement. C. Hartrick et al. assessed the effectiveness and tolerability of tapentadol and oxycodone in 659 patients with knee OA who required surgical treatment. A significant reduction in pain intensity compared to placebo on days 2, 5 and 10 after surgery was observed when taking tapentadol at a dose of 50 or 75 mg/day and oxycodone at a dose of 10 mg/day. The incidence of gastrointestinal complications was significantly lower in subjects taking tapentadol at both dosages compared with oxycodone. The rate of treatment discontinuation during therapy with tapentadol at a dose of 50 mg was 18%, at a dose of 75 mg - 26%, in the oxycodone group - 35 versus 10% in the placebo group [42].
L. Panella et al. compared the analgesic effect and tolerability of tapentadol PR 50–150 mg 2 times a day with paracetamol at a dose of 1000 mg/day in patients in the rehabilitation period after knee replacement with pain intensity >6 points according to NRS. A more rapid increase in range of motion, improved sleep quality, and a decrease in pain intensity have been shown during opioid analgesic therapy [43].
An important aspect of choosing an opioid analgesic is not only the severity of the analgesic effect, but also its tolerability. It is known that when using drugs in this group, adverse events often occur due to the effect on mu-opioid receptors, which are widely represented in various organs and tissues. Among them are gastrointestinal (nausea, constipation), cardiovascular (arterial hypertension), pulmonary (respiratory depression), endocrine (decreased potency) and mental effects, undesirable effects on driving, as well as the risk of abuse. The dual mechanism of action of tapentadol significantly reduces the risk of adverse events, because the drug's impact on mu-opioid prescriptions is 40% lower than that of other opioids. Thus, a pronounced analgesic effect and good tolerability are important advantages of the drug among other opioid analgesics.
The risk of drug dependence is also a significant factor limiting the use of opioid analgesics in patients with chronic pain syndrome. In 2012, the incidence of abuse was studied when treating patients with tapentadol PR, oxycodone, hydrocodone and tramadol, showing the most rare development of dependence when using the first of them [44, 45].
Conclusion
OA is a widespread disease among older people. Effective pain control is critical in improving patients' quality of life. The choice of effective therapy for pain in OA should be determined by both the intensity of the pain and its pathogenesis, i.e. the drug must act on both the nociceptive mechanism and the central nervous system.
The dual action mechanism of tapentadol allows its use as a pathogenetic therapy for severe pain in patients with OA. Good tolerability and high efficiency make it possible to recommend tapentadol PR to elderly patients for the conservative treatment of OA in the presence of contraindications or insufficient effectiveness of NSAIDs, as well as for the treatment of postoperative pain in patients who have undergone joint replacement, and as part of rehabilitation.