Anonymously
Around the clock
Attention! The material contains information about substances, the use of which can cause serious harm to your health!
Pharmacy drug or medicinal product? These are the kinds of debates that are constantly going on about certain drugs that are widely used in the treatment of certain diseases, but at the same time are successfully used by drug addicts to get a high. First you need to figure out what “Lyrics” is.
- Lyrica tablets - what is it, effect, active ingredient
- What does the drug Lyrica look like, photo
- Lyrica action, instructions
- Ways to use Lyrica
- Drug effect
- Pregabalin
- Symptoms of drug use - how to understand that a person is on Lyrica
- Eyes are the main feature
- Side effects from Lyrica
- How does it affect potency?
- How addiction is formed
- Is it possible to die from Lyrica?
- Alcohol compatibility
- Lyrica Test
- Medical therapy
We will select an individual treatment plan
Free consultation 8-800-200-27-23
Lyrica tablets - what is it, effect, active ingredient
The drug was originally prescribed as a medicine to treat epilepsy. It has an anticonvulsant effect, giving the same effect as antidepressants. Widely used in addiction medicine to relieve withdrawal symptoms. Alas, Lyrica pills for getting high will quickly lead a person to an impressive list of side effects. Since 2012, the drug has been sold only by prescription precisely because of the increased number of Lyrica drug addicts.
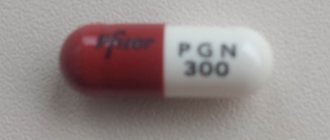
What does the drug Lyrica look like (photo)
The medicine is an oblong gelatin capsule of red and white color.
Photo of Lyrica tablets
The price of these tablets is relatively low, so the drug “lyra” has gained even more popularity among pharmacy drug addicts.
Lyrica action, instructions
The product contains pregabalin - this active substance affects opioid receptors in the human brain. As a result, pain is reduced and there is an anticonvulsant effect. The medicine has proven itself in the treatment of generalized anxiety symptoms. Analogues of the drug contain substances similar in action, for example, Algerica, Gabana.
Lyrica's instructions indicate doses for the treatment of certain diseases - from 150 to 600 mg per day. In addition, withdrawal from the drug should be gradual - the dose is reduced daily. After stopping the medication, reactions such as nausea, depression, excessive sweating, chills and lack of appetite are possible.
HOW TO HELP A DRUG ADDICT IF HE DOESN'T WANT TO BE TREATED
Ways to use Lyrica
The harm from lyrics is further aggravated by the method of administration. Drug addicts practice several methods of use:
- together with alcohol, which greatly accelerates the destruction of the liver and kidneys;
- standard oral administration without dosage control and diet causes disruption of the gastrointestinal tract;
- Some drug addicts believe that if the drug is inhaled, the rush will increase. Perhaps such an effect is present, but at the same time the respiratory tract is affected, and the risk of spasms increases;
- Parenteral administration (intravenously) is dangerous due to the occurrence of sepsis, transmission of HIV and hepatitis, and the likelihood of blood clots increases many times over.
Even short-term use of the medicine (including under the supervision of a doctor) can be addictive.
Drug effect
The effect of the drug "Lyra" is similar to the effect of heroin - a person feels euphoria, relaxation, and bliss. Some people experience a surge of strength and extraordinary love for everyone around them.
Fig.: Preparing the lyrics
Pregabalin
This substance is a synthetic substitute, a synthetic analogue of gamma-aminobutyric acid. Absorption is quite fast, which is what drug addicts take advantage of. In addition, pregabalin is not detected by standard tests; it can only be detected by chemical and toxicological analysis of human biomaterial.
General information
Pregabalin (or Lyrica) has clear therapeutic potential. The drug has proven itself as an effective remedy for relieving neuropathic pain. Lyrica is a synthetic analogue of a non-proteinogenic amino acid, which is the main inhibitory neurotransmitter in the central nervous system.
Therefore, the drug is also effective for the treatment of epilepsy and relief of seizures of various origins. In narcology, pregabalin is prescribed for alcohol withdrawal and opium withdrawal.
Pregabalin reduces the intensity of neuropathic pain. Therapeutic doses, even with a long course, do not cause an increase in tolerance to the drug.
Pregabalin in the treatment of pain syndromes / I. A. Strokov, V. A. Golovacheva, P. Ya. Brand - Medical advice. – 2013. – 69 – 73 p. [Electronic resource].
Recreational use of the drug is addictive. Because the drug has a stimulating effect on opiate receptors. Since 2010, the drug has been included in the list of potent drugs with narcotic potential. Dispensed from pharmacies only with a prescription.
Symptoms of drug use - how to understand that a person is on Lyrica
How to recognize a person who uses this drug for a high? Most often you will notice empty Lyrica packs in the trash can or pockets. At the same time, the drug addict believes that he will not be exposed, because this is medicine. This is a complete lie - the drug is not sold without a doctor’s prescription, and for this there must be serious indications for use. Other signs include:
- absent-mindedness, the addict periodically completely “disconnects” from the world around him”;
- a person may stagger, he cannot control his body even when walking normally;
- frequent mood swings from laughter to deep depression, and all this alternates;
- heavy sweating with a strong unpleasant odor;
- slurred speech.
Eyes are the main feature
The most important sign of drug intoxication is the eyes. When using Lyrica, you can see dilated pupils that do not react to light, your eyes do not focus and constantly run around.
Sometimes the opposite effect is observed - the eyes become glassy and practically do not move even when communicating. Anyone who has ever seen a drug addict will understand what it looks like. There is a possibility of severe redness of the whites of the eyes.
Fig.: Eyes of a drug addict under the lyrics
History of creation
Pregabalin was created by American medicinal chemist R. Silverman. The drug was developed as an alternative to Gabapentin, but with a more powerful therapeutic effect. After approval for use by the European Union, the drug was produced by Pfizer under the brand name Lyrica.
The drug was freely available. Since it was believed that the drug has a low narcotic potential when used for other purposes. Until 2008, no cases of recreational use were recorded. The first case of drug overdose was recorded in Sweden. Since the end of 2009, there has been a steady increase in the use of the drug to achieve drug intoxication.
In Russia, the drug was also available over-the-counter from pharmacies. Drug addicts used it to relieve symptoms of opium withdrawal. But the addiction formed earlier led to persistent dependence on Lyrics. Using the drug in overdose led to an increase in the narcotic effect of other psychostimulants.
Dependence on Lyrica develops in a fairly short time, since in order to achieve drug intoxication it is necessary to constantly increase the dose.
After cases of fatal overdose were recorded, over-the-counter dispensing from pharmacies was prohibited by law. After research, it was found that pregabalin in high doses has a toxic effect. Long-term use causes degenerative changes in the central nervous system.
Side effects from Lyrica
Like any other drug, Lyrica has an impressive list of side effects: tremors of the limbs, nausea, vomiting, insomnia, increased sweating, hallucinations, dry mucous membranes, bloating, lack of sexual desire and erection. Due to frequent diarrhea, it is possible to wash out all useful substances from the body, in particular calcium, which threatens osteoporosis.
Memory lapses, so common to many drug addicts, are also relevant when taking Lyrica. A person may not remember what happened an hour or a day ago.
How does it affect potency?
As mentioned above, the drug almost completely eliminates libido. At the same time, problems with potency may not be solved even after stopping taking Lyrica. There are known cases of infertility.
How addiction is formed
The addiction to the drug forms unnoticed by the user - the first doses only bring a feeling of high. Next, the body begins to adapt to the active substance and requires increasingly larger dosages to return to the original sensations. Often, an increase in the amount of Lyrica can cause a sharp change in mood and causeless aggression even towards close people. There are known cases of suicide under the influence of the drug.
Find out treatment recommendations without leaving home for free
To select a treatment plan, you just need to leave a request, we will contact you to select the time and specialist you need
Submit your application
Is it possible to die from Lyrica?
This medicine, at an adequate dosage prescribed by a doctor for the treatment of certain diseases, is not capable of causing death. But drug addicts most often combine Lyrica with other drugs or alcohol, and also do not control the number of pills. In this case, an overdose occurs and the corresponding phenomena are vomiting, diarrhea, confusion and coma.
If a drug addict has heart or kidney problems (and almost 80 percent of drug users have them), then death from an overdose is also possible. It is worth noting that such cases occur when taking Lyrica for a sufficiently long time. The lethal dose of a drug is individual for everyone, it all depends on the duration of use and the condition of the body as a whole.
DOTOXIFICATION
Indications and contraindications for use
Doctors prescribe medication in the following cases:
- Epilepsy, seizures
- Neuropathic pain sensations
- Pain in muscles and joints
- In combination with other medications, it is prescribed to treat panic attacks.
The substance is contraindicated:
- In case of drug intolerance
- Persons under the age of majority
- Hereditary diseases
With caution, the pharmaceutical drug is prescribed to people who have a diseased liver or kidneys.
Alcohol compatibility
Drug addicts often combine alcohol and Lyrica. This is done to enhance the effect. Such a tandem is doubly dangerous:
- alcohol reduces the breakdown and release of pregabalin, which can result in severe intoxication of the body;
- the combination of medication and alcohol can cause powerful disturbances of consciousness and hallucinations.
Everything also depends on the concentration and strength of alcoholic beverages, as well as on the dosage of the medicine. In large quantities, this combination can cause mental disorder.
The principle of action of pregabalin as a drug
According to doctors, drug addicts taking pregabalin experience euphoria, relaxation, a surge of strength, self-confidence, liberation, and numbness in the body.
Sometimes the opposite effect of the drug was observed: irritability, insomnia, disorientation, decreased libido.
The drug affects the same areas of the brain as tranquilizers. Increases endurance and activity. Sometimes they drink pregabalin and alcohol: the latter enhances the effect of the drug.
Drug addicts often use Lyrica to relieve withdrawal symptoms - withdrawal symptoms, hangovers. Therefore, addiction can develop against the background of alcoholism.
Lyrica Test
It was already mentioned above that this drug is not detected by standard urine and blood tests. These tests are designed to detect marijuana, heroin, cocaine and other drugs. It is possible to conduct a chemical and toxicological examination. However, the medicine does not belong to the list of narcotic substances.
What is it used for?
Pregabalin is an anticonvulsant and antiepileptic drug and is considered one of the most effective anticonvulsant drugs on the pharmaceutical market.
The antiepileptic effect after taking the medication begins very quickly, in addition, the pharmaceutical agent actively affects the patient’s psyche. Due to these effects, pregabalin is more popular than other alternative drugs.
The use of pregabalin helps eliminate pain and sensitivity. Taking the medication on an empty stomach increases its effectiveness.
What else is included in pregabalin (Lyrica)
- Gelatin
- Magnesium chloride
- Lactose disaccharide
- Hydrogenated starch hydrolysate
- Titanium dioxide
- Various types of dyes
Medical therapy
Treatment for a drug addict taking Lyrica is virtually no different from therapy for a heroin and other drug user. It can be roughly divided into two stages:
- removing the drug from the body, cleansing it, replenishing the lack of fluid;
- further therapy, including withdrawal symptoms, drug treatment, and psychological rehabilitation.
After the drug is removed from the body and withdrawal symptoms are eliminated, it is important to conduct a comprehensive examination. This will allow you to understand what you need to pay attention to. Most often, drug addicts suffer from liver, kidneys and heart.
DRUG ADDICTION TREATMENT IN MOSCOW
The most difficult stage is not physiological, but psychological - the drug can be easily removed from the blood, but it is very difficult to remove it from consciousness. Psychotherapy is mandatory for all patients. Sessions with a specialist or in a group will help to cope with a person’s internal problems, which often lead to drugs.
Leave a request for a free consultation with a specialist
We will contact you as soon as possible
- — Anonymous
- - For free
- — Around the clock
Another difficulty is returning to normal life, because outside the clinic the likelihood of buying a drug is at every turn. It is best to continue psychotherapy sessions for an addicted person regularly throughout life. They are also necessary for family and friends - often parents, husbands, wives, brothers or sisters become codependent and do not know how to behave correctly.
Article verified by an expert
Barinov Alexander Mikhailovich
More than 10 years of experience working with alcohol and drug addicts.
Similar articles:
Certificate from a narcologist: types, validity period and methods of obtaining
Drug Speed: symptoms and consequences of use
How long do drug cravings last?
Laughing gas. Effects of taking nitrous oxide
What to do if an addict does not want treatment?
to ““Lyrics - a drug or a medicine?””
- Yaroslav:
November 20, 2021 at 09:21
The drug Lyrica is nothing more than a medicine used to combat pain and cramps. To be precise, Pregabalin, also known as Lyrica, is an antiepileptic drug. It is a strong pain reliever.
Answer
- Lyubov Uspenskaya:
November 27, 2021 at 06:30
The pregabalin molecule, being an analogue of GABA, binds to the additional subunit (?2?) of voltage-gated calcium channels in the central nervous system, which contributes to the manifestation of analgesic and anticonvulsant effects. A decrease in seizure frequency begins within the first week.
Answer
- Yana:
December 23, 2021 at 01:56 pm
I just can’t understand how you manage to write such interesting notes.
Answer
- Vladimir:
January 28, 2021 at 02:39 pm
An indispensable remedy for neuropathy. The only thing that helps relieve severe pain.
Answer
- Boris:
February 8, 2021 at 16:03
Tell me, how does the analgesic effect of Lyrica manifest itself - immediately after ingestion or after a course of administration?
Answer
- Elena:
May 8, 2021 at 08:39 pm
Lyrica is not a therapeutic drug, but a symptomatic one. Helps very well with neuropathic pain. The pain goes away, but the pathology remains, REMAINS. A herniated disc can only be cured surgically; other types of supposed treatment involve eliminating pain for a short period of time. Personally, two 75 mg capsules twice a day are enough for me. In the morning and in the evening. For a drug addict, this dosage is “a drop in the bucket.” They can always find this drug in a pharmacy without a prescription, 300 mg capsules. Two per appointment. But people with pain syndrome may not even get a prescription. Pharmacists find errors in the prescription every time. They take away the recipe, and you’re left with “butter.” Corruption is all around. At the doctor, at the pharmacist. I didn't even know what was written in my medical history. You'll never know what prescription you've been given. There is one dosage in the medical history, and another in the prescription. And the discharge date doesn’t match. I’m HORROR!
Answer
- Dmitriy:
September 26, 2021 at 10:02 pm
To everyone who will read this article after they have been prescribed Lyrica or Convalis. Yes, the drugs are quite powerful and have consequences. Unfortunately, the neurologist prescribes only a course of complex treatment. hepabeptin, Lyrica, injections, vitamins B1 and B6, etc. Amitriptyline goes there too. None of the above will relieve pain immediately. The pain is relieved by a set of measures and course. Those. when you come in with severe pain, there is a 99% chance you will come out without a short-term solution. They will tell you to hold on, the pain will go away in a month (or maybe in 6). See for yourself in the direction of distracting ointments. Perhaps they will prescribe a Versatis patch, it is expensive, and if the pain is severe(!), the reduction does not justify the price. Moreover, after the patch there is a 12-hour break and it will hurt. Strong painkillers (or God forbid tramadols, etc.) are generally when things are really bad. Look towards oflomelid (if the damage is not severe) or gevkamen (this one remarkably relieves pain, costs 50 rubles), but not a single doctor talks about it. Also be sure to consult a dermatologist and neurologist. Don't take my comment as a ready-made solution.
Answer
- oksana:
September 27, 2021 at 11:20 am
Thank you for the recommendations for users, but it is worth remembering that this cannot in any way replace going to the doctor and making a diagnosis. Everything is individual. Health to everyone!
Answer
Dmitriy:
September 27, 2021 at 10:42 pm
Oksana, of course, this is exactly what is written at the end of my comment. What has been written applies specifically to those who have already received a neurological diagnosis. pain in fact (I was stunned that they were prescribed something like lyric) and is trying to figure out how to reduce it (the pain). In my case, none of the 6 doctors gave an answer on what to do right then and there. I’ll add one more thing on my own behalf. If opportunities allow, take expensive analogues from imp. manufacturers. Yes, the substance is the same, but the purity and method of delivery can be completely different. I won’t give specifics, lest they be considered advertising, but in my case the difference was strong. At the same time, it is simply impossible to buy them in a pharmacy near your home, no.
Answer
- Vladimir:
September 30, 2021 at 09:31 pm
For some reason, everyone is silent about Cymbalta. For example, my doctor prescribed Lyrica and Cymbalta to drink at the same time. I have polyneuropathy. The pain is partially relieved. The doctor said that Lyrica should be added per capsule. I tried to add it, but at the same time my head and temples were compressed on the sides. I didn't drink the second one. I don’t know how long to take it. Everyone around, both doctors and people, say we need to get away from this nasty thing. As much as we are doctors, we have in common so many different opinions. One
Answer
Pregabalin in the treatment of pain syndromes
STROKOV I.A.
., Doctor of Medical Sciences, Professor,
GOLOVACHEVA V.A.
,
BRAND P.Y.
, Candidate of Medical Sciences,
Department of Nervous Diseases of the First Moscow State Medical University named after. I.M. Sechenova Neuropathic pain is caused by primary damage or disease of the somatosensory system.
Neuropathic pain is based on pathological activation of pain pathways, which may be associated with damage to the nervous system at the level of peripheral nerves, plexuses and dorsal roots (peripheral neuropathic pain) or the spinal cord and brain (central neuropathic pain). Neuropathic pain reduces the quality of life of patients, their social adaptation and ability to work, and in many cases the pain is difficult to treat. The prevalence of neuropathic pain in the population is 6 - 8% and it is associated with chronic pain syndromes, female gender, older age of patients, frequent visits to medical care and a low level of social status, which can be considered as risk factors. According to the Russian EPIC study, out of 85,923 patients who consulted neurologists, 33,664 patients (39%) had complaints of pain. According to the results of testing using the DN4 questionnaire, neuropathic pain was detected in 15,301 patients (17.8%) [1]. The prevalence of neuropathic pain among all patients who consulted neurologists in Spain was significantly lower and amounted to only 3.88% [2]. The reasons for the formation of neuropathic pain in the EPIC study were similar to most foreign studies, i.e. in most cases (91.74%) the cause was peripheral neuropathic pain. Back pain dominated in terms of frequency (50.58%), and pain in DPN was traditionally in second place (10.64%). The problem of diagnosing and treating neuropathic pain is one of the most important in modern medicine.
In clinical practice, diagnosing the neuropathic nature of pain is often difficult. The experience of pain is always subjective, it cannot be accurately measured, and there are no absolute criteria to distinguish neuropathic pain. Judging the pathophysiological mechanisms underlying the pain syndrome can only be tentative, based on the characteristics of pain, data from a neurological examination and the results of a neurophysiological study. Moreover, the identification of clinical signs and changes in electrophysiological parameters showing a pathological change in the state of the nociceptive system does not reliably prove the presence of neuropathic pain. Neuropathic pain may occur immediately after damage to the somatosensory system, such as in acute small fiber neuropathy, or may develop years or even decades after the injury or disease onset. The neuropathic nature of pain can be diagnosed if a dysfunction of the somatosensory system is confirmed in the presence of: 1) spontaneous sensory symptoms; 2) the results of a clinical examination identifying symptoms of damage to the nervous system: positive neuropathic symptoms (stimulus-dependent pain) and negative neuropathic symptoms (neurological deficit); 3) data from neurophysiological studies (EMG, quantitative sensory testing, somatosensory evoked potentials). In this case, the choice of research methods is determined by the results of a neurological examination.
Neurological symptoms make it possible to determine the presence, extent and localization of damage to the nervous system. To diagnose the phenomenon of neuropathic pain, the doctor is primarily interested in the state of the sensory system. It is clear that, depending on the peripheral or central localization of the pathological process, a study of the general neurological status, including the motor and autonomic systems, is of great importance for diagnosis; in this case, negative symptoms will include, for example, a decrease in reflexes, muscle strength, the presence of muscle atrophy, dryness and discoloration of the skin. When identifying damage to the sensory system, to diagnose neuropathic pain, they focus on the state of sensitivity associated with the activation of thin, weakly myelinated Aδ- (cold stimulus and blunt needle prick) and thin, unmyelinated C-fibers (painful and thermal stimuli). It should be remembered that neuropathic pain usually occurs in the area of decreased or lack of sensitivity, that is, the area of pain and sensitivity disorders in these cases coincides. In recent years, epidemiological studies to study the prevalence of pain are based on the use of special questionnaires that make it possible to determine the nature of pain with a high degree of accuracy [3,4]. Neuropathic pain occurs in a wide range of diseases of the peripheral and central nervous systems (Table 1, Table 2), and in terms of prevalence, peripheral neuropathic pain is far ahead of central neuropathic pain.
Treatment of neuropathic pain is based on modern ideas about the pathophysiological mechanisms of its development [5]. Pharmacological interventions are used aimed at reducing peripheral afferentation, which supports changes in the excitability of nociceptive structures of the spinal cord and brain, drugs that reduce the excitability of nociceptive neurons, and drugs that enhance supraspinal descending inhibitory antinociceptive effects. In severe cases, administration of pharmacological drugs close to the central receptors (intradural) is used. It is possible to use electrical stimulation of peripheral nerves, primarily proprioceptive fibers, to enhance the inhibitory effects on the excitability of nociceptive neurons of the spinal cord, and acupuncture. Surgical treatment for cases refractory to pharmacotherapy may include the use of implanted electrodes in the brain or spinal cord, nerve release or decompression, chemical destruction, or nerve transection. Table 3 presents European recommendations for the treatment of neuropathic pain, based on an analysis of the Cochrane Database of Controlled Trials, for the period from 1966 to 2006 [6]. These recommendations were developed by a group of experts on neuropathic pain, led by the French neurologist N. Attal, and discussed at several specialized symposia. When drawing up domestic recommendations for the treatment of neuropathic pain, special attention was paid to the analysis of European recommendations [7].
The most widely used drug for treating neuropathic pain is pregabalin (trade name Lyrica). The drug reduces the intensity of pain in most types of central and peripheral neuropathic pain. Suffice it to say that pregabalin is registered in the USA and Russia as a drug for the treatment of all types of neuropathic pain.
Pregabalin is close in chemical structure to GABA and has anticonvulsant, anti-anxiety and analgesic effects. The effect of pregabalin is not realized through conversion to GABA or interaction with GABA receptors. Compared to gabapentin, pregabalin is more rapidly absorbed and has higher bioavailability (90% versus 60%) [8]. Food intake does not affect the bioavailability of the drug. Important advantages of pregabalin compared to gabapentin are a clear linear dependence of the drug concentration in the blood within the therapeutic window (75-600 mg), a lower daily dose, faster titration of the drug, and fewer side effects [9].
Studies have shown that pregabalin significantly reduces the intensity of neuropathic pain during the first three days of taking the drug. Long-term studies (15 months) of the use of pregabalin for neuropathic pain showed that it retains its analgesic effect throughout the entire period of use without developing tolerance to the drug. The excellent analgesic effect of pregabalin is confirmed by the improvement in sleep indicators in patients,
mood and quality of life. It should be noted that there is no evidence on the method of discontinuing the drug, although most researchers, based on personal experience, recommend its gradual withdrawal. The main mechanism of action of pregabalin, like gabapentin, is binding to the α2-δ protein of presynaptic voltage-dependent calcium channels, which leads to a decrease in the flow of calcium into the neuron and a decrease in the level of its excitability, a decrease in the release of neurotransmitters such as glutamate, dopamine and a specific algogen substance R. This mechanism works both at the spinal level and in the structures of the brain. It should be noted that pregabalin has six times greater affinity for α2-δ protein compared to gabapentin [10,11].
The half-life of the drug is 5.5-6.7 hours, depending on the dose used. Pregabalin does not bind to plasma proteins, is not metabolized by the liver and is excreted unchanged in the urine. Elimination through the kidneys forces the use of lower daily doses of the drug in patients with renal pathology. Pregabalin does not interact with other drugs and can be used in various combinations, for example with tricyclic antidepressants. Pregabalin is usually well tolerated by patients, but temporary dose-dependent side effects such as dizziness and drowsiness are possible (22-29% of patients). It is extremely rare to experience dry mouth, difficulty concentrating, weight gain, blurred vision, and peripheral edema in the legs.
The most studied is the analgesic effect of pregabalin in painful diabetic polyneuropathy. Patients with diabetes may develop various forms of painful diabetic neuropathy, which differ in the localization of pain, the severity of the occurrence and the nature of the pain, although in all cases the pain is neuropathic. The classic variant of peripheral neuropathic pain is the pain syndrome associated with diabetic distal symmetrical sensorimotor polyneuropathy. Epidemiological studies conducted in the USA have shown that neuropathic pain occurs with diabetic polyneuropathy more often than with all polyneuropathies of other etiologies combined. According to the Russian EPIC study, neuropathic pain in diabetic polyneuropathy is second only to back pain in prevalence [3].
Diabetic polyneuropathy (DPN) is observed in approximately 50% of patients with diabetes, while neuropathic pain is observed in 11-24% of patients with polyneuropathy, which depends on the duration of diabetes and polyneuropathy, as well as the type of diabetes. Already at the first description of a patient with DPN in 1798. The English doctor J. Rollo identified pain and paresthesia as the main symptoms. Clinical manifestations, frequency, severity and duration of pain syndrome in DPN are extremely diverse, they are united by a common feature - the neuropathic nature of pain. Among patients suffering from diabetes, chronic pain occurs in 25% of cases, while in the population the prevalence of chronic pain syndromes is about 15%, and the difference is formed to a greater extent due to neuropathic pain [12].
Neuropathic pain in DPN is represented by two main components: spontaneous (stimulus-independent) and evoked (stimulus-dependent) pain. Spontaneous pain can be constant (burning pain) or occur paroxysmally with pain lasting from seconds to hours (shooting pain). Spontaneous pain is caused by the ectopic activity of nociceptive C-fibers as a result of the appearance on them under pathological conditions of a large number of sodium channels and a change in the excitability of pain receptors, leading to their activation under low-threshold stimuli, which is not observed under normal conditions. It is also possible that excitation is transferred from one fiber to another - the phenomenon of ephaptic excitation. Thus, pain afferentation increases, further leading to changes in the excitability of nociceptive neurons of the dorsal root ganglion and dorsal horn. The processes of disruption of the functional state of dorsal horn neurons associated with the mechanisms of ambient, pre- and postsynaptic inhibition, deafferentation, as well as the mechanisms of central sensitization with damage to peripheral nerves are described in detail in reviews by foreign and domestic authors [3,13,14]. Nociceptive signals from dorsal horn neurons travel to the thalamus opticum and then to the somatosensory cortex, where pain is perceived. It has been shown that in patients with painful DPN, in contrast to patients with diabetes mellitus without pain, there is a change in metabolism in the thalamus [15]. Neurons of central sensory structures can also change their excitability with the formation of the phenomenon of sensitization. All central structures for the conduction and perception of pain have close connections with descending inhibitory and activating pathways. The main inhibitory (antinociceptive) influences are associated with descending pathways from the periaqueductal gray matter and the rostro-ventral parts of the medulla oblongata to the dorsal horn. These descending inhibitory influences are realized through the norepinephrine and serotonin neurotransmitter systems.
In clinical studies, pregabalin has been shown to be highly effective in treating neuropathic pain caused by diabetic peripheral nerve damage. Already in the first randomized, double-blind, placebo-controlled studies of the effectiveness of pregabalin for painful DPN, conducted at the beginning of the century, it was noted that, compared with placebo, the drug significantly reduced pain [16,17,18]. In a randomized, double-blind, placebo-controlled study in 146 patients with painful DPN, a significant reduction in the intensity of neuropathic pain was obtained within the first week of the study, which was maintained over the next 8 weeks of taking the drug. A graded visual analogue Likert scale was used as the main criterion in the study. Significant improvements in sleep and social abilities of patients were also noted [17]. Another study on 81 patients showed that when other pharmacological drugs were ineffective for painful diabetic polyneuropathy, pregabalin at a dose of 150-600 mg was significantly effective [19]. In a randomized, double-blind, placebo-controlled study, Japanese experts in 2011 studied the effectiveness of doses of 300 mg and 600 mg of pregabalin compared with placebo in 317 patients with painful DPN [20]. The duration of treatment was 14 weeks, a significant decrease in pain (p<0.05) with both doses of the drug was noted already from the first week of treatment. By the end of the study, a reduction in pain by 50% or more was observed when taking 300 mg of pregabalin in 29.1% of patients, when taking 600 mg of the drug in 35.6% of patients, and when using placebo in 21.5% of patients. In addition to a reduction in pain in the groups receiving pregabalin, there was also an improvement in sleep, a decrease in numbness and paresthesia.
The study, published in 2013, analyzed the results of 11 randomized, double-blind, placebo-controlled trials of the effectiveness of pregabalin in painful DPN and postherpetic neuralgia. Using original statistical analysis techniques, the authors came to the conclusion that the improvement in the quality of life of patients treated with pregabalin is associated not only with a decrease in pain, but there is also a direct effect of pregabalin on the quality of life, possibly associated with the anxiolytic effect of the drug [21]. European and world recommendations for the treatment of neuropathic pain emphasize the fact of the high effectiveness of pregabalin (Lyrica) in the treatment of neuropathic pain syndromes, including DPN, and classify it as a first-line therapy with evidence of effectiveness A [22,23]. When drawing up domestic recommendations for the treatment of neuropathic pain, special attention was also paid to pregabalin [7]. Pregabalin has shown its effectiveness not only in chronic neuropathic pain syndromes, but also in acute pain, such as post-operative pain. Typically, non-steroidal anti-inflammatory drugs, local anesthetics, small doses of ketamine, and less commonly opioids are used to treat postoperative pain. Pregabalin reduces the sensitization of dorsal ganglion neurons, which is detected in experimental models of acute pain of postoperative pain and plays a role in the chronicity of pain syndrome [24,25]. Due to this effect, pregabalin reduces the intensity of postoperative pain syndrome. In this situation, the anxiolytic component of the effect of pregabalin also plays a certain role. More than 10 randomized controlled studies have been conducted showing the ability of pregabalin to reduce the severity of acute and chronic postoperative pain.
A double-blind, randomized study of the effectiveness of pregabalin (50 and 300 mg), ibuprofen (400 mg) and placebo in the postoperative period found that there was a significant difference in the ability of drugs and placebo to reduce pain intensity. The duration of effect of 300 mg pregabalin was significantly longer than that of ibuprofen [26].
A randomized controlled trial compared the ability of diazepam (10 mg) and pregabalin (150, 300 and 600 mg) in the preoperative period (laposcopic hysterectomy) and pregabalin in the same doses and placebo in the postoperative period to reduce pain. It has been shown that the use of 600 mg of pregabalin significantly reduces the need for opioid use [27].
Pregabalin has shown its effectiveness in randomized controlled trials for a wide range of pain syndromes: fibromyalgia [28], after spinal surgery [29], post-stroke pain [30], pain due to spinal injury [31], and abdominal pain due to chronic pancreatitis [32].
The ability of pregabalin to reduce the excitability of neurons in the dorsal ganglion, dorsal horn, thalamus and cortical neurons, a wide range of pain syndromes in which the drug has shown its ability to reduce the intensity of pain, improve sleep and quality of life make it a universal drug for the treatment of neuropathic pain syndromes of various localizations and etiologies .
Literature.
1. N.N. Yakhno, M.L. Kukushkin, O.S. Davydov et al. Results of the Russian epidemiological study of the prevalence of neuropathic pain (EPIC Study). Treatment of neuropathic pain // Consilium medicum. Neurology 2008; 2:64-70. 2. Montero HJ, Guttierez-Rivas E, Fernandez J et al. Epidemiological study of prevalence incidence and neuropathic pain characterization in neurology unit. PREVADOL study // Neurologia 2005; 20: 385-389. 3. Yakhno N.N., Kukushkin M.L., Davydov O.S. and others. Results of a Russian epidemiological study of the prevalence of neuropathic pain, its causes and characteristics in a population of outpatients who consulted a neurologist // Pain 2008; 3: 24-32. 4. Danilov A.B., Davydov O.S. Neuropathic pain // Iz-vo Borges, Moscow 2007: 32-55. 5. Kukushkin M., L., Khitrov N.K. General pathology of pain // M. 2004: 144 pages. 6. Attal N., Cruccu G., Haanpaa M. et al. EFNS guidelines on pharmacological treatment of neuropathic pain // Eur J Neurol 2006; 13: 1153-1169. 7. Guidelines for the diagnosis and treatment of neuropathic pain. Edited by Academician of the Russian Academy of Medical Sciences N.N. Yakhno // Moscow, RAMS Publishing House 2008: 32 p. 8. Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice // Epilepsia 2004; 45: 13-8. 9. Freynhagen R., Strojek K., Griesing T. et al. Efficacy of pregabalin in neuropathic pain evaluated in 12-week, randomized, double-blind, multicenter, placebo-controlled trial of fble- and fixed-dose regimen // Pain 2005; 115:254-263. 10. Belliotti T., Capiris T., Ekhato I. et al. Structure-activity relationships of pregabalin and analogues that target the α(2)-δ protein // J Med Chem 2005; 48:2294–2307. 11. Dones D., Sorkin L. Systemic gabapentin and S(+)-3-isobutil-γ-aminobutiric acid block secondary hyperalgesia // Brain Res 1998; 810:93-99. 12. Chan AW, MacFarlane IA, Bowsher DR et al. Chronic pain in patients with diabetes mellitus: comparison with non-diabetic population // Pain Clinic 1990; 3: 147-159. 13. Novikov A.V., Solokha O.A. Neuropathic pain: Review based on materials from the journal “The Lancet” (May-June 1999) // Neurological Journal 2000; 1:56-61. 14. Besson J. The neurobiology of pain // Lancet 1999; 353: 1610-1615. 15. Sorensen L, Siddall PJ, Trenell MI et al. Differences in metabolites in pain-processing brain regions in patients with diabetes and painful neuropathy // Diabetes Care 2008; 31: 980-981. 16. Lesser H., Sharma U., LaMoreaux L. et al. Pregabaline relieves symptom of painful diabetic neuropathy: a randomized controlled trial // Neurology 2004; 63:2104–2110. 17. Rosenstock J, Tuchman M, LaMoreaux L et al. Pregabaline for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial // Pain 2004; 110:628-638. 18. Richter RW, Portenoy R, Sharma et al. Relief of diabetic painful peripheral neuropathy with pregabalin: a randomized, placebo-controlled trial // J Pain 2005; 6:253-260. 19. Stacey BR, Dworkin RH, Murphy K. et al. Pregabalin in the treatment of refractory neuropathic pain: results of a 15-month open-label trial // Pain Med – 2008 Mar 11. 20. Satoh J., Yagihashi S., Baba M. et al. Efficacy and safety of pregabalin for treatment of neuropathic pain associated with diabetic peripheral neuropathy: a 14 week, randomized, double-blind. placebo-controlled trial // Diabet Med 2011; 28(1): 109-116. 21. Vinic A., Emir B., Cheung R. et al. Relationship between pain relief and improvements in patient function/ quality of life in patients with painful diabetic peripheral neuropathy o postherpetic neuralgia treated with pregabalin // Clin Ther 2013; 1. 22. Attal N., Cruccu G., Baron R. et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision // Eur J Neurol, 2010, 17(9), 1113-88. 23. Bril V., England J., Franklin GM et al. Evidence-based guideline: Treatment of painful diabetic neuropathy // Neurology 2011; 76(20): 1758-1765. 24. Aasvang E., Kehlet H. Chronic postoperative pain/ The case of inguinal herniorrhaphy // Br J Anaesth 2005; 95: 69-76. 25. Rowbotham D/J/ Gabapentin: a new drug for postoperative pain? Br J Anaesth 2006; 96: 152-155. 26. Hill C., Balkenohl M., Thomas D. et al. Pregabalin in patients with postoperative dental pain // Eur J Pain 2001; 5:119-124. 27. Jokela R., Ahonen J., Tallgren M. et al. A randomized controlled trial of perioperative administration of pregabalin for pain after laparoscopic hysterectomy // Pain 2008; 134: 106-112. 28. Pauer L, Atkinson G, Murphy TK et al. Long-term maintenance of response across multiple fibromyalgia symptom domains in a randomized withdrawal study of pregabalin // Clin J Pain 2012; 28(7):609-614. 29. Ozgencil E., Yalcin S., Tuna H. et al. Perioperative administration of gabapentin 1200 mg day-1 and pregabalin 300 mg day-1 for pain following lumbar laminectomy and discectomy: a randomized, double-blinded, placebo-controlled study // Singapore Med J 2011; 52(12): 883-889. 30. Kim JS, Bashford G, Murphy TK et al. Safety and efficacy of pregabalin in patients with central post-stroke pain // Pain 2011; 152(5): 1018-1023. 31. Cardenas DD, Nieshoff EC, Suda K. et al. A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury // Neurology 2013; 80(6): 533-539. 32. Bouwense SAW, Olesen SS, Drewes AM et al. Effects of pregabalin on central sensitization in patients with chronic pancreatitis in a randomized, controlled trial // PLoS One, 2012 7(8): e42096.