pharmachologic effect
Hypoglycemic agent - glucagon-like polypeptide receptor agonist.
Dulaglutide is a long-acting glucagon-like peptide-1 (GLP-1) receptor agonist. Its molecule consists of two identical chains linked by disulfide bonds, each containing a modified human GLP-1 analog covalently linked to the heavy chain (Fc) fragment of modified human immunoglobulin G4 (IgG4) via a small polypeptide chain. The GLP-1 analog portion of dulaglutide is approximately 90% homologous to native human GLP-1. The half-life (t1/2) of native human GLP-1 due to cleavage by dipeptidyl peptidase-4 (DPP-4) and renal clearance is 1.5-2 minutes. Unlike native GLP-1, dulaglutide is resistant to degradation by DPP-4 and is large in size, which slows absorption and reduces renal clearance. These structural features provide a soluble form and a half-life of 4.7 days, making the drug suitable for subcutaneous administration once a week. In addition, the dulaglutide molecule was designed to reduce the Fc receptor-mediated immune response and reduce its immunogenic potential.
The hypoglycemic effect of dulaglutide is due to several mechanisms of action of GLP-1. With increased glucose concentrations, dulaglutide increases the content of intracellular cyclic adenosine monophosphate (cAMP) in the beta cells of the pancreas, which leads to increased insulin secretion. Dulaglutide suppresses excess glucagon secretion in patients with type 2 diabetes mellitus, which leads to decreased glucose output by the liver. In addition, dulaglutide slows the rate of gastric emptying.
Effect of liraglutide on body weight of patients with T2DM
Various studies have shown that liraglutide leads to a significant reduction in body weight, both as monotherapy and as part of combination therapy, compared with glitazones and insulin glargine, which traditionally cause weight gain (Fig. 12).
Weight loss occurred in the first 16 weeks of treatment and was maintained at the achieved level throughout the year of treatment. The decrease in weight was more pronounced the higher the initial body mass index (from 2 to 7 kg per year). Body weight loss occurred mainly due to visceral fat, which was confirmed by both a decrease in waist circumference (-3-3.6 cm) and a study of body composition using computed tomography.
Treatment with liraglutide in a comparative study with sitagliptin was also accompanied by a more significant decrease in body weight: -3.38 kg and -2.86 kg for dosages, respectively, of 1.8 mg and 1.2 mg, compared with -0.96 kg for sitagliptin.
The high effectiveness of liraglutide in reducing body weight suggests the possibility of its use in the future for the treatment of obesity (the drug is currently registered only for the treatment of T2DM).
Indications for use
Trulicity is indicated in adult patients with type 2 diabetes mellitus to improve glycemic control in the form of:
- monotherapy
If diet and exercise do not provide the necessary glycemic control in patients for whom the use of metformin is not indicated due to intolerance or contraindications.
- combination therapy
In combination with other hypoglycemic drugs, including insulin, if these drugs, together with diet and exercise, do not provide the necessary glycemic control.
Antihyperglycemic effect of liraglutide
Studies have shown that liraglutide was more effective than other drugs in reducing HbA1c levels in all series of trials. At the same time, the maximum decrease in HbA1c during monotherapy was 1.6% compared to the initial value.
- In monotherapy, liraglutide at a dose of 1.8 mg per day demonstrated significantly greater efficacy than at a dose of 1.2 mg per day (HbA1c levels decreased by 1.6 and 1.2%, respectively), and significantly greater efficacy than glimepiride monotherapy in dose of 8 mg per day (HbA1c decreased by 0.9%) over 52 weeks of treatment (Fig. 10).
- After 1 year of treatment, the number of patients achieving treatment goals (HbA1 < 7%) was significantly higher among those taking liraglutide at both doses (58% and 62% at doses of 1.2 mg and 1.8 mg, respectively) compared with glimepiride at a dose of 8 mg (31%).
- In all of these LEAD studies, liraglutide provided rapid and sustained reductions in fasting hyperglycemia, greater than glimepiride and rosiglatizone and comparable to insulin glargine.
- When compared with the GLP-1 mimetic exenatide, liraglutide was significantly more effective in reducing HbA1c levels (by 1.1% versus 0.8%) and fasting hyperglycemia. However, hyperglycemia after breakfast and dinner was better reduced when taking exenatide due to its twice-daily administration.
- Mild hypoglycemia also occurred less frequently in patients receiving liraglutide compared with patients receiving exenatide (1.93 with liraglutide versus 2.60 events per patient per year with exenatide).
The Lancet in 2010 published the results of the first international multicenter 26-week randomized, open-label study of liraglutide compared with sitagliptin in combination with metformin in patients with type 2 diabetes.
- Liraglutide provided significantly greater reductions in HbA1c, fasting plasma glucose (FPG) and body weight compared with sitagliptin (Januvia) with similar or higher overall treatment satisfaction.
- Using liraglutide at a dose of 1.8 mg and 1.2 mg, 54.6 and 43.4% of patients, respectively, achieved treatment goals, and in the sitagliptin 100 mg group - 22.4% of patients (Fig. 11).
Key results comparing liraglutide and sitagliptin therapy in terms of hypoglycemic effect are as follows:
- The drug liraglutide provided a greater reduction in HbA1c levels (-1.50% and -1.24% at dosages of 1.8 mg and 1.2 mg, respectively) compared to sitagliptin (-0.90%).
- The mean reduction in fasting plasma glucose was significantly greater in the liraglutide-treated group.
- The study also assessed patient satisfaction with treatment using the Diabetes Treatment Satisfaction Questionnaire (DTSQ), which is used in many diabetes drug trials: The increase in overall treatment satisfaction was greater with liraglutide 1.8 mg than with liraglutide 1.8 mg. during therapy with sitagliptin.
- There were no differences in perceived comfort of treatment (oral versus injectable route).
Directions for use and doses
Trulicity should be administered subcutaneously to the abdomen, thigh or shoulder. The drug cannot be administered intravenously or intramuscularly.
The drug can be administered at any time of the day, regardless of food intake.
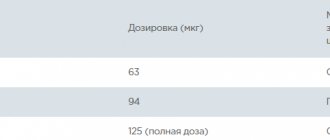
- Monotherapy: the recommended dose is 0.75 mg once a week.
- Combination therapy: the recommended dose is 1.5 mg once a week.
In patients aged 75 years and older, the recommended starting dose of the drug is 0.75 mg once a week.
When dulaglutide is added to current therapy with metformin and/or pioglitazone, metformin and/or pioglitazone can be continued at the same dose. When dulaglutide is added to ongoing sulfonylurea or prandial insulin therapy, a dose reduction of the sulfonylurea or prandial insulin may be necessary to reduce the risk of hypoglycemia.
Additionally, glycemic control is not required to adjust the dose of dulaglutide. Additional glycemic control may be required to adjust the dose of sulfonylureas or prandial insulin.
- Missing a dose
If a dose of Trulicity is missed, it should be administered as soon as possible if at least 3 days (72 hours) remain before the next scheduled dose. If less than 3 days (72 hours) remain before the next scheduled dose, skip the drug and administer the next dose as scheduled. In each case, patients can resume the usual regimen of drug administration once a week.
The day of drug administration can be changed if necessary, provided that the last dose was administered at least 3 days (72 hours) ago.
Efficacy of liraglutide in clinical studies
The phase III liraglutide research program “Study of the Effect and Action of Liraglutide in Diabetes (LEAD™)” included about 6,500 patients from 41 countries, including Russia. Among them, approximately 4,445 patients received liraglutide. The goal of the program was to determine the indications for the use of liraglutide for the treatment of T2DM in monotherapy and in combination with traditional glucose-lowering drugs. The LEAD program compared the efficacy and safety of liraglutide with sulfonylureas, glitazones, insulin glargine, and exenatide. (Fig. 9).
The effects of liraglutide compared with sitagliptin in combination with metformin in patients with T2DM were assessed in an international, multicenter, 26-week, randomized, open-label, parallel-group study.
- The dynamics of HbAlc reduction in these studies averaged -1.6%. Two years of liraglutide monotherapy (1.8 and 1.2 mg) demonstrated significant and sustained improvements in glycemic control (-1.1 and -0.9%, respectively, compared with -0.6% on glimepiride) and body weight ( -2.7 kg and -2.1 kg compared with + 1.1 kg on glimepiride) against the background of a low risk of hypoglycemia (6 times less often) compared with motor therapy with glimepiride.
- The maximum reduction in HbA1c when adding liraglutide to metformin monotherapy was 2.74% in the subgroup of patients with an initial HbA1c level >9.5%.
According to the study results, while taking liraglutide, 52-65% of patients achieve HbA1c levels <7% with a minimal risk of hypoglycemia. Liraglutide also causes rapid and sustained weight loss, a clinically significant reduction in systolic blood pressure, and an improvement in β-cell function.
Liraglutide: achieving comprehensive diabetes treatment goals
- Liraglutide has an effect similar to human GLP-1: against the background of hyperglycemia, it stimulates insulin secretion and suppresses glucagon secretion, and at normal or low glycemia these effects are not observed. This mechanism helps prevent the development of hypoglycemic conditions.
- Liraglutide also improves β-cell function, slows gastric emptying and reduces postprandial hyperglycemia, accelerates satiety, and has beneficial cardiovascular effects.
- The use of the drug liraglutide leads to a significant reduction in body weight both in monotherapy and as part of combination therapy. Weight loss occurs in the first weeks of treatment and is maintained at the achieved level throughout the year of treatment. The higher the initial body mass index, the more pronounced the weight loss. Body weight loss occurs mainly due to visceral fat.
- A meta-analysis of these studies showed that the addition of liraglutide injections to previous antihyperglycemic therapy resulted in a reduction in HbA1c levels by 1.26-1.36%, thus setting the average HbA1c endpoint at 6.96-7.05%. At the same time, the proportion of patients who achieved the target HbA1c level <7% during combination therapy with liraglutide was 71% (Fig. 14).
- A meta-analysis of LEAD studies showed the following advantages of liraglutide in comparison with representatives of all classes of hypoglycemic drugs: the odds ratio of achieving control of HbAlc and body weight without hypoglycemia for liraglutide is 2.0 - 10.3 times higher than in patients receiving comparator drugs. All results are statistically significant.
- Thus, with the use of the drug liraglutide, the percentage of patients who manage to achieve control of HbA1c, body weight and SBP is higher than with therapy with any comparison drugs (Fig. 15).
Sources:
- Ametov AS First GLP-1 analog liraglutide: the result of clinical trails on efficacy / AS Ametov, LL Kamynina // Diabetes Mellit. – 2011. – T. – No. 4 – 39 p.
- Shestakova M.V. LIRAGLUTIDE POSSIBILITIES OF AN INTEGRATIVE THERAPEUTIC APPROACH IN THE THERAPY OF TYPE 2 DM / Shestakova M.V. // Diabetes mellitus – 2009. – No. 5.
Effect of liraglutide on the cardiovascular system
A number of studies have shown that liraglutide “inherited” from GLP-1 not only the glucose-lowering effect, but also cardioprotective properties. The studies noted a significant decrease in systolic blood pressure, which was observed approximately 2 weeks from the start of treatment and reached a maximum of -6.6 mm Hg. Art. at a dose of 1.2 mg and -5.5 mmHg. Art. at a dose of 1.8 mg (Fig. 13).
The antihypertensive effect of the drug is probably associated with a vasodilatory effect due to stimulation of the production of endothelial nitric oxide synthase (NOS). A hypothesis has also been put forward about the natriuretic or diuretic effect of the drug.
In phase II clinical studies, the highest dose reduced levels of three cardiovascular risk biomarkers (triglycerides, plasminogen activator inhibitor-1, and B-type natriuretic peptide), supporting a direct cardioprotective effect of liraglutide.
Effect of liraglutide on β-cell mass and function
To date, the only way to assess the functional activity of beta cells in vivo is the HOMA-B homeostasis model assessment model: using a special formula, the ratio of fasting glucose and plasma insulin levels is calculated.
According to a series of studies, the use of liraglutide was accompanied by a significant increase in HOMA-B by 40-71%, as well as a change in the proinsulin/insulin ratio, which may indirectly reflect the drug’s ability to restore the functional activity of pancreatic beta cells.
- Improvement in β-cell function, as assessed by the HOMA-B index, was significantly greater with liraglutide at both doses compared with placebo and rosiglitazone and comparable to that with glimepiride.
- Liraglutide at a dose of 1.8 mg once caused a significantly greater increase in the HOMA-B index (by 32%) compared with exenatide at a dose of 10 mcg twice a day (by 3%).
- In a 26-week, randomized, open-label study of liraglutide versus sitagliptin in combination with metformin in patients with type 2 diabetes, improvement in β-cell function as measured by HOMA-B was significantly greater with liraglutide at both doses compared with sitagliptin.