This information will help you learn how to give yourself a subcutaneous injection (shot) using a prefilled syringe. A subcutaneous injection is an injection that is given under the skin. A pre-filled syringe is a syringe that is sold with medication already inside.
Your healthcare provider will show you how to give the injection yourself. You can use the information in this resource as a reminder when you give the injection at home.
to come back to the beginning
Intravenous
The needle is inserted directly into the lumen of the vein. Medicines immediately penetrate the bloodstream and have an effect. In terms of technique, this is one of the most difficult types of injections, since you need to get into a blood vessel without piercing it through. In addition, no infection or air bubbles should enter the vein. Intravenous injections are made using a syringe or transfusion systems. Slow infusion through droppers with a catheter allows you to prolong the effect of the drug for several hours and evenly distribute its intake, which is very convenient in the treatment of bedridden patients.
Intravenous injections are done in most cases when it is necessary to quickly release the drug into the blood and begin its action. This is an indispensable first aid tool. But it should be borne in mind that intravascular administration has a greater number of possible complications than subcutaneous and intramuscular administration. Thromboembolism, infection, hematomas in the puncture area, burns and inflammation of the vein walls, etc. occur. Performing intravascular infusions for people without medical education is prohibited.
Order of conduct
Before administering a drug, you should definitely check your sensitivity to this medication. The manipulation is carried out in a procedural environment, maintaining sterility. Treat the surface of your hands with alcohol using two cotton balls.
The skin is pre-treated twice in the injection area. To do this, use sterile beads with alcohol. First, a large area of skin around is captured. Then it is treated only at the puncture site. Injections are performed as follows:
- Intradermal administration. Take half a milliliter of the drug from the ampoule with a long needle. Then change the regular needle to a thin one. Check its patency. For injection, use the middle third of the patient's forearm, its inner surface. Hold the needle with the cut side up. It is inserted at an acute angle parallel to the skin. Then the end of the needle is inserted into the tissue to hide the gap. After this, 0.1 ml of solution is injected. A papule forms, which resolves after forty minutes. The needle is removed and the skin is not treated after the injection.
- Subcutaneous. With your left hand, collect the skin into a fold. Right, hold the syringe at an acute angle. Then the needle is inserted to a depth of approximately 2/3 of its length. The cut is directed upward. The drug is administered. A cotton swab with alcohol is applied to the puncture site. With a sharp movement, remove the needle from the tissue. Massage the injection site with a cotton ball and alcohol for better distribution.
- Intramuscular. Determine the exact injection site on the buttock. The injection is made into the upper-outer sector at an angle of 90° to the surface. With the left hand, the soft tissues are firmly fixed. With the right hand, insert the needle perpendicular to the surface to a depth of six centimeters. Slowly introduce the solution. Remove the needle with a quick movement, applying a cotton ball with alcohol to it. The injection site is lightly massaged.
After administering medications, it is necessary to monitor the injection sites. The formation of infiltrates and suppurations should be avoided.
Intramuscular
Inserting a needle into the thickness of the muscles is an intramuscular injection. The muscles are well supplied with blood and lymph, so the bioavailability of the administered substances is high. The effect of drugs administered in this way occurs much more slowly than with intravenous infusion; usually the effect becomes noticeable after 30-45 minutes. A drug injected into a muscle is kept there for some time in the form of a kind of depot, from where it gradually enters the blood and has an effect on the body.
Intramuscular injections are used in cases where immediate action is not needed, but a daily or multi-hour dose of the drug must be administered so that it is slowly absorbed (for example, the administration of antibiotics). In terms of technique, injections into the muscle are the simplest, but if the technique is incorrect, complications are also possible: getting into large vessels, nerve trunks, infection.
What are intradermal, subcutaneous, and intramuscular injections used for?
Injection is a method of introducing medications into body tissues in the form of solutions using syringes and hollow needles. Recently, another method of injecting drugs has been used - high-pressure injection using needle-free devices. There are several types of injections:
- Intradermal. When placing them, the needle is inserted into the thickness of the skin to a slight depth at an acute angle. The solution, penetrating into the tissue, forms a round elevation - a “lemon peel”. The following sites are used for intradermal injection: the middle and upper third of the anterior outer area of the shoulder, the middle and upper third of the anterior outer area of the thigh. Less commonly used are the lateral area of the anterior abdominal wall, the area around the navel, and the subscapular area.
- Subcutaneous. They are placed by puncturing the skin about 15 millimeters deep. The rapid effect of the drug with this type of parenteral administration is explained by the fact that there are many blood vessels in the subcutaneous fat layer. Medicines here are quickly absorbed and do not cause any harm to the subcutaneous tissue. Up to two liters of liquid can be injected under the skin. The most convenient areas of the human body for subcutaneous injections are considered to be: the outer surface of the shoulder, the subscapular area, the anterior outer area of the thigh, and the anterolateral area of the abdomen. When carrying out manipulations, the location of large vessels and nerves should be avoided.
- Intramuscular. During this manipulation, a puncture is most often made in the area of the upper outer quadrant of the gluteal region. Somewhat less frequently, the area of the outer surface of the thigh or the posterolateral surface of the shoulder is used. The volume of injected solution with a standard intramuscular injection does not exceed six milliliters.
- Intravenous. The drugs are administered into superficially located and inactive ulnar and radial veins. Less commonly, puncture of venous vessels is performed in the dorsum of the hand.
The injections are carried out by specially trained medical personnel. The manipulation is carried out in a procedural setting on an outpatient basis or in a hospital in compliance with the principles of asepsis and antisepsis.
Subcutaneous
For hypodermic injections, the needle is inserted to a depth of no more than 15 mm. The drug enters the layer of subcutaneous fat. Small amounts of drugs (up to 2 ml) can be administered in this way. Before the injection, the skin is gathered into a fold, then a needle is inserted into this fold at an angle of 45 and the liquid is slowly released. The optimal places to perform it are the space under the shoulder blades, the anterior side of the thigh, the outer part of the shoulder, the lower part of the armpit, that is, all places where it is easy to make a skin fold.
Subcutaneous injections are used in cases where there is no immediate need for the onset of action of the drug, but it is desirable to bypass the gastrointestinal tract. In addition, there are medications that are destroyed in the gastrointestinal tract or are poorly absorbed in it. Subcutaneous injections are simple in technique, and in case of an error they give even fewer complications than intramuscular ones. Therefore, subcutaneous injections are allowed for people without medical education. Possible complications include infection and hematoma at the injection site. Subcutaneous administration is often used for vaccination.
Indications
By injection, those medications are administered that are not absorbed in the intestinal wall, cause local irritation, or quickly disintegrate under the influence of enzymes of the digestive tract.
Intradermal administration is used for allergy tests, as well as specific diagnostic reactions - Mantoux, Pirquet, etc. Subcutaneous injections are used when it is necessary to ensure prolonged absorption and effect of the drug (insulin, heparin, vaccines).
Intradermal
Introducing drugs into the skin is not so simple technically and requires some skill. A thin needle should penetrate only under the upper stratum corneum, but not into the subcutaneous fat. A sign that the injection has been performed correctly is a light-colored bump with the drug that appears on the skin after injection. After some time it resolves.
Intradermal administration of drugs is most often used in cosmetology to normalize the condition of the skin, as well as when testing for allergens and specific immune reactions (Mantoux test, Schick reaction, etc.). Some types of local anesthesia are also administered this way. As a rule, they are done on the outer surface of the shoulder and forearm. It is prohibited for non-specialists (people without medical training) to perform such injections.
How to Store Prefilled Syringes
How you store prefilled syringes depends on the type of medicine in them. Most medications are stored at room temperature, but some should be kept in the refrigerator. Your healthcare provider will tell you how to store your syringes. Do not store prefilled syringes in the freezer or leave them in the sun.
Check one of the boxes below so you don't forget how to store your syringes.
- Store prefilled syringes at room temperature.
- Store prefilled syringes in the refrigerator.
If you have questions about storing or carrying prefilled syringes while traveling, contact your healthcare provider.
What to do if the medicine is frozen
If the medicine inside the syringe is frozen, place it near the front of the refrigerator or on a shelf in the refrigerator door to thaw. Do not use the medicine if it has been frozen more than once. Call your healthcare provider for further instructions.
to come back to the beginning
Rules for injections to prevent complications
Almost all complications can be prevented by maintaining sterility and avoiding air bubbles in the liquid. After opening, you must not touch the needle; the injection site must be treated with cotton wool and alcohol. Use only sterile preparations from ampoules.
Air bubbles from the liquid must be carefully removed because when they enter the blood, they cause the formation of a blood clot. This complication is especially dangerous with intra-arterial injections, and slightly less so with intravenous injections.
In our clinic, injections are performed by qualified specialists, come and perform the procedures without the risk of complications!
CLINIC PRICES OUR CLINIC DOCTORS MAKE AN APPOINTMENT ASK QUESTIONS PERMANENT DISCOUNTS PROMOTIONS THIS MONTH
When should you contact your healthcare provider?
Call your healthcare provider if you have the following symptoms:
- Blood does not stop flowing from the injection site.
- You have very severe pain.
- You injected the medicine into the wrong place.
- You have a fever of 100.4°F (38°C) or higher.
- You have signs of an allergic reaction, such as swelling, redness, itching, or a rash.
- You cannot use the syringe because the medicine has expired, the medicine has foamed, changed color, become cloudy, or has crystals in it.
- You cannot use the syringe because you touched something with the needle before injecting.
- You cannot use a pre-filled syringe with Lovenox because there is no air bubble in it.
- You are having difficulty administering the injection.
to come back to the beginning
UZ "Mogilev City Emergency Hospital"
Insulin is administered subcutaneously. Insulin can be administered using:
- insulin syringes;
- syringe pens;
- injection port (iPort);
- insulin pump.
In the Republic of Belarus, insulin is most often administered using insulin syringes.
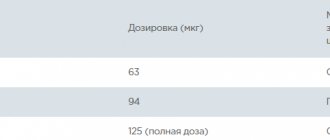
Volumes of insulin syringes: 0.3 ml, 0.5 ml and 1 ml. The syringe is marked with divisions and numbers. The numbers indicate the number of units (from 10 to 100 units). In the picture there is a syringe with a volume of 1 ml, 1 ml contains 100 units, one small division corresponds to 2 units of insulin.
The syringe must match the insulin concentration. Now almost all insulins have a concentration of 100 U/ml and they correspond to syringes 0.1 ml - 10 IU (1 ml syringe marked 100 IU; 0.5 ml - 50 IU; 0.3 ml - 30 IU). But earlier insulin was produced with a concentration of 40 units/ml and there were corresponding syringes for it (40 units - 1 ml). If you draw insulin with a concentration of 100 U/ml into such a syringe, the dose will be exceeded by 2.5 times. In our country, such syringes are currently not produced.
In addition, the insulin analog Toujeo contains 300 units per ml. Toujeo is administered with a syringe pen. But if you suddenly need to inject Tujeo with a syringe and dial up the dose with an insulin syringe of 100 units/ml, then the dialed dose will be 3 times more than the required dose.
The length of the needle in an insulin syringe is from 6 to 13 mm. The needle thickness is indicated by the letter “G” (G31 – G26). The higher the number, the thinner the needle (i.e. a G31 needle will be thinner than a G26).
The choice of the optimal length and thickness of the needle depends on the individual parameters of the body and is selected experimentally.
Syringe pens
A syringe pen is a device into which insulin is inserted in special bottles called cartridges. The required dose of insulin is set and administered as an injection (shot), just like with a syringe. The needles in pens are removable and must be changed after each insulin injection. The needles are universal and fit all syringe pens. After injecting insulin, the needle must be removed. Do not store the pen with the needle screwed on. Insulin may leak from the needle and air may enter the cartridge.
Needles come in lengths from 4 to 12 mm and thicknesses G32 - G29. Just like an insulin syringe, the higher the number, the thinner the needle.
Syringe pens are disposable and reusable.
For example, Lantus is available in the form of a disposable pen (Lantus SoloStar) and in cartridges for a reusable pen (Lantus Penfill).
A disposable pen contains 300 units of insulin (1 ml - 100 units, 3 ml in one pen). When the insulin runs out, the pen is thrown away. Reusable syringe pens contain insulin in replaceable cartridges. One cartridge (except Tujeo) also contains 300 IU of insulin (1 ml - 100 IU, 1 cartridge - 3 ml). In Tujeo, 1 ml contains 300 units.
In the Republic of Belarus, insulin in cartridges is prescribed only to certain categories of patients specified in the order of the Ministry of Health (children, pregnant women, etc.).
Pens are also available electronic and mechanical. The pens also differ in the step at which insulin can be injected (0.1 units; 0.5 units; 1 unit).
Each insulin has its own syringe pen!
You can learn more about syringe pens on the website www.test-poloska.ru.
Injection port
The purpose of the port is to reduce the number of injections. When using it, 1 puncture is performed when installing the iport itself (a cannula is inserted under the skin with a special device), and then an insulin injection is made not under the skin, but into the rubber membrane of the iport. The injection port is set for 72 hours or 75 injections. The iport cannula comes in 6 and 9 mm sizes (for children – 6 mm, for adults – 9 mm). Short and long insulin cannot be injected into the iport at the same time. The difference between injections should be at least 60 minutes. Moreover, first you need to inject short-acting insulin and only after 60 minutes long-acting insulin can be injected into the airport. After long-acting insulin is injected into the iport, short-acting insulin can be injected into it no earlier than 3 hours later. Therefore, short-acting insulin is often administered intravenously, and long-acting insulin is usually administered by injection.
Injections into the iport membrane can be performed with syringes and pens. But the needles must be at least 6 mm.
Recommended sites for insulin injection
Insulin can be injected into the area of the anterior outer surface of the thighs, buttocks, outer surface of the shoulders, and abdomen. In the abdominal area, insulin is not injected around the navel area (2 cm in diameter), in the midline of the abdomen, from the ribs down, 2 cm must be injected.
Depending on where the insulin is injected, the action time of the genetically engineered insulin differs (this does not apply to analogues). The fastest action of insulin occurs when injected into the stomach, so short-acting insulin is injected into the stomach. Long-acting insulin is injected into the thighs and buttocks.
It is advisable to inject insulin into the shoulders only if someone else is doing the injection.
Insulin will be absorbed faster under conditions of increased blood circulation (after a bath, hot shower, massage of the injection site, physical activity). Insulin slows down the action of cooling, vasospasm, dehydration.
Insulin cannot be injected into the same place; insulin injection sites must be alternated (left-right thigh or shoulder, left-right half of the abdomen), the distance between insulin injections must be at least 2 cm. Insulin is not injected into the area of scars, stretch marks ( stretch marks).
It is necessary to regularly inspect and palpate the injection sites. If the injection technique is incorrect (multiple injections in one place, injection of cold insulin, repeated use of needles, etc.), seals (“bumps”) can form at the sites of insulin injection - hypertrophic lipodystrophy. Less commonly, thinning of the subcutaneous fat (“depression”) may occur at the sites where insulin is administered—atrophic lipodystrophy. Insulin should not be injected into areas of lipodystrophy! If insulin is injected into areas of lipodystrophy, it will have no effect, and insulin can accumulate there and act unpredictably. Sensitivity is lost in areas of lipodystrophy, so patients often inject insulin there because it “doesn’t hurt” there. You can't do that.
Insulin injection technique
If you are administering extended-release NPH insulin (“cloudy” long-acting insulin), then before use it must be mixed by rolling it between your palms at least 10 times (do not shake the bottle).
If insulin is injected with a syringe, then you need to draw air into the syringe according to the number of units of insulin (if you inject 10 units of insulin, you need to draw 10 units of air). Then inject the collected air from the syringe into the insulin vial and draw the required amount of insulin. Remove air bubbles from the syringe (needle up, tap the syringe), release excess air and 0.5-1 units of insulin from the syringe.
If insulin is administered with a syringe pen, then you need to dial and release 0.5-1 units of insulin, while holding the pen with the needle up.
Injections are performed on a clean area of skin with clean hands. If you follow the rules of personal hygiene and take a shower every day, there is no need to disinfect your skin before each injection.
It is necessary to form a skin fold (muscles should not be grasped into the fold, only the skin should be grasped). Insulin injections should be administered into subcutaneous fat and not intradermally or intramuscularly. The fold should be taken with two fingers, and not with the whole hand (so as not to catch the muscles).
The needle is inserted, depending on the thickness of the subcutaneous fat, inserted at a right angle or at an angle of 450 into the base of the fold, with the needle cut upward.
After inserting the needle, you must gently press the plunger of the syringe or syringe pen (grasp the syringe pen with 4 fingers, press with your thumb), inject insulin and hold the syringe under the skin for at least 10 seconds (count to 20). The higher the dose, the longer you need to hold the needle. After this, take out the needle (don’t let go of the fold!), wait a little (count to 3) and release the fold.
Insulin storage
The insulin supply should be stored in the refrigerator at a temperature of 2 to 80C. Insulin should not be frozen! If insulin has been frozen, it cannot be used. On an airplane, insulin cannot be checked in as luggage. he might freeze there.
The bottle from which insulin is administered can be stored at room temperature (up to 250C) for up to 4 weeks. Avoid exposing insulin to direct sunlight.
If insulin is removed from the refrigerator, it should be at room temperature for at least 1 hour.
When traveling or on the beach, insulin reserves should be stored in special thermal cases for storing insulin. Also, thermal covers should be used at negative ambient temperatures. When the ambient temperature is below freezing, insulin should be transported by placing it close to the body and not in a bag.
Do not use insulin if color changes, flakes or sediment appear.
Insulin pump
An insulin pump is a device that delivers continuous subcutaneous infusion of insulin. In this case, ultra-fast insulin is administered at a given rate as basal insulin and additional insulin boluses are administered for food.
In this case, you can change the rate of basal insulin administration hourly (effective for dawn syndrome), use different boluses of short-term insulin (effective for compensating for different meals). The pump does not replace glucose monitoring (monitoring is one expense, the pump is another). You also need to understand that the pump is not an artificial pancreas; the decision on the administered doses of insulin is made not by the pump, but by the patient. When using a pump, you must be able to accurately count carbohydrates and know your coefficients. It makes sense to install a pump when there is an understanding of diabetes compensation. In the absence of knowledge, the pump itself will not solve the compensation problem.
There are wired and wireless pumps. In wireless pumps (Omnipod), insulin is located in special devices (pods) that are installed on the body. Insulin supply is controlled via a special remote control. The price of one pod is $20-25, one pod is set for 72 hours, a minimum of 10 pods are needed for a month. The price of the remote control is about $600.
With corded pumps, the insulin is stored in a special reservoir in the pump. The pump is fixed on clothing, a cannula (Teflon or steel) is installed subcutaneously on the body, and insulin is supplied from the pump to the cannula through a special catheter. The reservoir, cannula and catheter must be changed every 3 days.
In the Republic of Belarus, wired pumps are certified, which are sold by the company Zarga, on whose website you can find the current prices.
The main problems that arise when using a pump:
- high cost (pumps can be installed free of charge for children and pregnant women, infusion sets are purchased by patients at their own expense, insulin is free);
- discomfort when wearing, need to be removed during water procedures (showering, bathing);
- the cannulas are bent, as a result of which insulin stops entering the body.
Instructions for subcutaneous injections
You will need:
- a clean cloth napkin;
- packaging with the drug in a syringe and alcohol wipes;
- two sterile dry cotton balls (one of them is a spare).
Check your doctor's prescription before giving the injection. Make sure that the drug you purchased or received is appropriate. Focus on the international nonproprietary name - INN. Check whether the drug has expired or whether the syringe is damaged. The solution in it must be the color stated in the instructions and not contain foreign particles or suspensions [1,2].
How to give injections [1,2]:
- Wash your hands with warm water and soap.
- Prepare everything you need in advance. Place a clean cloth on the table, lay out the package with the drug, remove the syringe and alcohol wipes from it. Before using the syringe with the drug, keep it at room temperature for the time specified in the instructions for use. Place two dry cotton balls. Find a comfortable, relaxed position.
- Select the injection site according to the instructions for medical use of the drug prescribed for you. Carefully read the recommended injection sites and inject the drug only into the indicated areas.
- Wipe the selected injection site with one or two wipes. Let the skin dry and discard the tissues.
- Take the syringe with the injection needle and carefully remove the protective cap without touching the needle.
- Form and maintain a skin fold according to the instructions in the instructions for use. Without touching the skin with your fingers, quickly and firmly insert the needle into the fold at a right angle, holding the syringe like a pen. Slowly pressing the plunger, inject the solution until the syringe is completely empty.
- Remove the needle with a vertical movement without tilting it to the sides. Release the skin fold. Apply a dry, sterile cotton ball to the injection site.
- After the procedure, the syringe must be disposed of.
Try to choose a new injection site each time and do not inject the drug into painful areas.
Do not rub or massage the injection site.
Manufacturers include special short needles for subcutaneous injections with kits for injections of PMTRS, so the drug is administered at a right angle [3].